Supplemental Digital Content is available in the text
Keywords: levodopa challenge test, nonmotor symptoms, Parkinson disease, respiratory dysfunction
Abstract
Introduction:
Parkinson disease is associated with various nonmotor symptoms, including rare respiratory dysfunction events. However, patients with Parkinson disease often have comorbid medical problems, such as respiratory distress, and differentiating nonmotor symptoms can be difficult.
Case presentation:
A 78-year-old male presented with repetitive shortness of breath. He was diagnosed with Parkinson disease and chronic obstructive pulmonary disease (COPD) several years prior. His symptoms were ambiguous between acute COPD exacerbation and levodopa-related nonmotor symptoms of Parkinson disease. To clarify the underlying cause, we performed the levodopa challenge test. After the patient complained of dyspnea following levodopa administration, levodopa-induced respiratory dysfunction was diagnosed. After adjusting antiparkinson medication, the patient's respiratory symptoms gradually improved.
Conclusion:
Respiratory dysfunction as a nonmotor symptom of Parkinson disease can be caused by levodopa medication. To determine whether the symptoms are induced by levodopa, the levodopa challenge test may be useful in clarifying symptoms related to antiparkinson medication.
1. Introduction
Parkinson disease is the second most common degenerative disease. It was recently shown to be associated with various nonmotor symptoms, such as mood disorders, gastrointestinal symptoms, and sleep disturbances, in addition to the motor symptoms typical of Parkinson disease.[1] Respiratory dysfunction, including shortness of breath and stridor, are also often observed in patients.[2] Various nonmotor symptoms may be associated with the progression of Parkinson disease or with administration of antiparkinsonian drugs.[1,3] Some nonmotor symptoms of Parkinson disease may be due to the effects of antiparkinson medication, which can be determined using the levodopa challenge test.[4] Parkinson disease is common in older patients who often have comorbid medical problems. Therefore, differentiating nonmotor symptoms from other medical issues can be difficult. Herein, we present an instructive case report of a patient with Parkinson disease and chronic obstructive pulmonary disease (COPD) who complained of shortness of breath and was effectively treated after the levodopa challenge test.
2. Case report
A 78-year-old male presented with shortness of breath. The patient was diagnosed with Parkinson disease and started taking antiparkinson medication 10 years prior. He was also diagnosed with COPD 5 years before and was undergoing inhalation therapy. He was referred to our tertiary medical center due to repeated difficulty breathing for 6 months. At an initial visit, his symptoms were considered to be indicative of acute COPD exacerbation, and the patient was treated with antibiotics and oral steroids. However, there was no significant improvement in respiratory symptoms after treatment, and the patient was referred to the neurology department to evaluate possible neurologic causes of his dyspnea. Following the neurology consult, he still complained of shortness of breath with stridor that usually worsened in the afternoon. When respiratory symptoms were present, oxygen saturation monitoring showed that levels were maintained within normal limits. Emphysematous changes were observed on X-ray and chest computed tomography (Fig. 1), and there was no significant difference from previous imaging findings.
Figure 1.
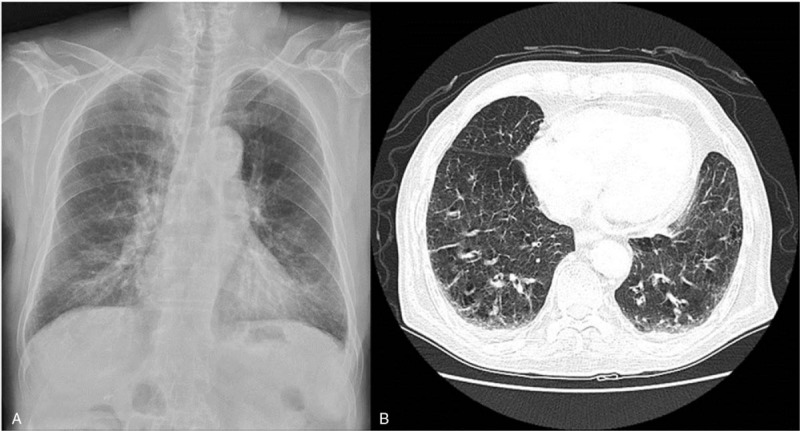
Chest X-ray (A) and chest computed tomography (B) showed scattered centrilobular lucencies involving both lungs.
The patient complained of general weakness and fatigue, but focal weakness was not observed on neurological examination. He had bradykinesia and rigidity in both extremities. He also had a gait problem, with short strides and subtle imbalances, but could walk independently while taking medication. Postural instability was not severe and tremor was not observed. His daily levodopa dose was 900 mg. The patient took antiparkinson medication 3 times a day at 7 am, 1 pm, and 7 pm. There were some variations, but he usually suffered from shortness of breath around 2 pm. When he had respiratory symptoms, arterial blood gas analysis showed pH 7.474, partial pressure of oxygen (PO2) 108.3 mm Hg, partial pressure of carbon dioxide (PCO2) 32.5 mm Hg, and oxygen saturation of 99%, indicating no carbon dioxide retention. Inhaled ventolin therapy showed partial improvement, but dyspnea and wheezing were sustained. Dyskinetic movement of the patient's neck and trunk was also observed. In order to distinguish the nonmotor symptoms of Parkinson disease due to wearing off, we used short-acting levodopa, but did not observe significant improvement. Because the patient had been treated for COPD for a long time, the cause of dyspnea was not clear. To confirm whether symptoms were related to levodopa, we performed a levodopa challenge test to induce a medication off state. As a result, unified Parkinson Disease Rating Scale motor scale improved from 37 points to 29 points, and 27.58% response to levodopa was confirmed. Video images taken before and after the test in the medication off state showed no dyspnea and a stable breathing rate at about 22 times per minute. After 150% of the usual levodopa dose was administered, the respiration rate increased to 38 breaths per minute and the patient complained of severe dyspnea, as shown on the supplemental video. We confirmed that he was experiencing levodopa-induced respiratory symptoms. Levodopa dose was gradually decreased and a catechol-O-methyltransferase inhibitor was added to control respiratory and Parkinson symptoms. After a few days, the respiratory symptoms improved without deterioration of motor symptoms. During follow-up 6 months after discharge, the patient complained of intermittent mild respiratory distress. However, the symptoms were transient and there were no dyspnea events that required hospital admission. Overall, symptoms remained significantly improved.
To report this instructive case, informed consent was obtained from the patient for publication and accompanying images and video.
3. Discussion
Although respiratory symptoms are not a common complication of Parkinson disease, they have been reported with disease progression as a result of upper airway obstruction, restrictive respiratory dysfunction, abnormal central control of ventilation, and drug-related dysfunction.[2] The mechanism of these symptoms in Parkinson disease is not yet clear. However, in most cases, symptoms are related to disease progression or wearing off of medication such that symptoms are relieved with levodopa dose titration.[5,6] Levodopa leading to poor respiratory function has not been widely reported.[7] Parkinson disease is often accompanied by various chronic medical problems given that the prevalence increases with age. In particular, respiratory problems are common medical conditions in elderly populations and are also the most common cause of death in Parkinson patients.[8] Therefore, the boundary between the underlying cause and nonmotor symptoms of Parkinson disease is ambiguous in older patients. In patients with COPD and refractory dyspnea, as described in the present case, clinicians generally focus on acute medical care and appropriate treatment may be overlooked. Even if clinicians suspect that symptoms are caused by Parkinson disease, it is often difficult to determine whether they are drug on or off symptoms. We performed a levodopa challenge test to clarify this ambiguous case.
The levodopa challenge test is used primarily to assess the patient's dopamine responsiveness or to evaluate indications for deep brain stimulation.[9] Fundamentally, the test is performed to evaluate the efficacy of levodopa drugs and can clearly identify drug on or off symptoms. As a result, levodopa-induced respiratory symptoms were confirmed with the dopamine challenge test in this case of rare respiratory dysfunction. Not all nonmotor symptoms of Parkinson disease are responsive to levodopa, and the levodopa challenge test is limited primarily because it assesses the acute response of the drug. Therefore, it is necessary to evaluate the usefulness of the levodopa challenge test for various nonmotor symptoms as well as respiratory dysfunction in various cases. Nevertheless, the levodopa challenge test is an excellent method to intuitively demonstrate and exclude other factors that affect drug response. We suggest that levodopa challenge test may be a useful tool for clarifying the symptoms related to antiparkinson medication.
Author contributions
Conceptualization: Pan-Woo Ko.
Data curation: Pan-Woo Ko.
Writing – original draft: Pan-Woo Ko.
Writing – review & editing: Kyunghun Kang, Ho-Won Lee.
Pan-Woo Ko orcid: 0000-0002-5520-2211.
Supplementary Material
Footnotes
Abbreviations: COPD = chronic obstructive pulmonary disease, PCO2 = partial pressure of carbon dioxide, pH = pouvoir hydrogene, PO2 = partial pressure of oxygen.
The authors have nothing to disclose and no conflicts of interest.
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI16C2210).
Supplemental Digital Content is available for this article.
References
- [1].Poewe W. Non-motor symptoms in Parkinson's disease. Eur J Neurol 2008;15suppl 1:14–20. [DOI] [PubMed] [Google Scholar]
- [2].Torsney KM, Forsyth D. Respiratory dysfunction in Parkinson's disease. J Royal Coll Phys Edin 2017;47:35–9. [DOI] [PubMed] [Google Scholar]
- [3].Park A, Stacy M. Non-motor symptoms in Parkinson's disease. J Neurol 2009;256suppl 3:293–8. [DOI] [PubMed] [Google Scholar]
- [4].Fabbri M, Coelho M, Guedes LC, et al. Response of non-motor symptoms to levodopa in late-stage Parkinson's disease: results of a levodopa challenge test. Parkinson Relat Disord 2017;39:37–43. [DOI] [PubMed] [Google Scholar]
- [5].Hovestadt A, Bogaard JM, Meerwaldt JD, et al. Pulmonary function in Parkinson's disease. J Neurol Neurosurg Psychiatry 1989;52:329–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Herer B, Arnulf I, Housset B. Effects of levodopa on pulmonary function in Parkinson's disease. Chest 2001;119:387–93. [DOI] [PubMed] [Google Scholar]
- [7].De Keyser J, Vincken W. L-dopa-induced respiratory disturbance in Parkinson's disease suppressed by tiapride. Neurology 1985;35:235–7. [DOI] [PubMed] [Google Scholar]
- [8].Beyer MK, Herlofson K, Arsland D, et al. Causes of death in a community-based study of Parkinson's disease. Acta Neurol Scand 2001;103:7–11. [DOI] [PubMed] [Google Scholar]
- [9].Rodriguez RL, Fernandez HH, Haq I, et al. Pearls in patient selection for deep brain stimulation. Neurologist 2007;13:253–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


