Abstract
Guidelines for patients with subarachnoid hemorrhage (SAH) management and several grading systems or prognostic indices have been used not only to improve the quality of care but to predict also the outcome of these patients. Among them, the gold standards Fisher radiological grading scale, Hunt-Hess and the World Federation of Neurological Surgeons (WFNS) are the most employed. The objective of this study is to compare the predictive values of simplified acute physiology score (SAPS) 3, sequential organ failure assessment (SOFA), and Glasgow Coma Scale (GCS) in the outcome of patients with aneurysmal SAH.
Fifty-one SAH patients (33% males and 67% females; mean age of 54.1 ± 10.3 years) admitted to the intensive care units (ICU) in the post-operative phase were retrospectively studied. The patients were divided into survivors (n=37) and nonsurvivors (n = 14). SAPS 3, Fischer scale, WFNS, SOFA, and GCS were recorded on ICU admission (day 1 – D1), and 72-hours (day 3 – D3) SOFA, and GCS. The capability of each index SAPS 3, SOFA, and GCS (D1 and D3) to predict mortality was analyzed by receiver operating characteristic (ROC) curves. The area under the ROC curve (AUC) and the respective confidence interval (CI) were used to measure the index accuracy. The level of significance was set at P < .05.
The mean SAPS 3, SOFA, and GCS on D1 were 13.5 ± 12.7, 3.1 ± 2.4, and 13.7 ± 2.8 for survivors and 32.5 ± 28.0, 5.6 ± 4.9, and 13.5 ± 1.9 for nonsurvivors, respectively. The AUC and 95% CI for SAPS 3, SOFA, and GCS on D1 were 0.735 (0.592–0.848), 0.623 (0.476–0.754), 0.565 (0.419–0.703), respectively. The AUC and 95% CI for SOFA and GCS on D3 were 0.768 (0.629–0.875) and 0.708 (0.563–0.826), respectively. The overall mortality was 37.8%.
Even though SAPS 3 and Fischer scale predicted mortality better on admission (D1), both indices SOFA and GCS performed similarly to predict outcome in SAH patients on D3.
Keywords: Glasgow Coma Scale, ICU setting, outcome, SAPS 3, SOFA
1. Introduction
The treatment provided within an intensive care unit (ICU) should not be restricted to knowledge about procedures, technology and clinical protocols. Safety, cost-effectiveness and outcome of the critically ill patient must also be assessed since they impact on the demand for financial resources.[1] Guidelines for subarachnoid hemorrhage (SAH) management[2] and several grading systems or prognostic indices have been used not only to improve the quality of care but to predict also the outcome of these patients. Among them the gold standards Fisher radiological grading scale (Grade 0 to 4),[3] Hunt–Hess (Grade 1 –5)[4] and the World Federation of Neurological Surgeons (WFNS) (Grade 1–5) which includes the Glasgow Coma Scale (GCS) combined with presence or absence of focal deficits[5] are the score systems most employed. However, some other prognostic indices have been used such as acute physiology and chronic health evaluation (APACHE) and Simplified Acute Physiology Score (SAPS) to predict outcome in patients with SAH.[6–8] These scores are more extensive, because of the use of multiple physiological variables from different organic systems and the GCS in their score calculation. On the other hand, the GCS is critical in the neurological patients with acute brain disorders, including SAH, this scale measurement loss its accuracy on day 1 (D1) when the patient is sedated, for example, the day after the surgical procedure. The objective of this study is to compare the predictive values of SAPS 3, Sequential Organ Failure Assessment (SOFA) and GCS on D1 and D3 (SOFA and GCS) in the outcome of patients with SAH.
2. Material and methods
This retrospective study was conducted in a general 20-bed adult ICU of Sao Francisco Hospital, Ribeirao Preto, Sao Paulo, Brazil. This tertiary ICU admits critically ill adults such as clinical cases or surgical patients (SAH after surgical clipping or endovascular aneurysm obliteration) in early postoperative period. The study protocol was approved by the Research Ethics Committee of Clinics Hospital of Ribeirao Preto Medical School, University of Sao Paulo (Protocol 7076/2016). Patients with SAH admitted to ICU between 2011 and 2016 were analyzed. Data concerning the diagnosis upon ICU arrival, comorbidities, demographic profile, Hunt-Hess and Fischer radiological grading scales were documented. Prognostic indexes such as SAPS 3,[9,10] SOFA[11] and Glasgow Coma Score (GCS) were recorded. Data for calculation of the prognostic indexes were collected during the first 24 hours (D1) and 72 hours (D3) after patient admission. Therefore, SAPS 3, SOFA and GCS were recorded on ICU admission (day 1 – D1), and SOFA and GCS 72-hours after admission (day 3 – D3). The calibration of prognostic indices was provided by manufacter's software of data bank (Epimed Solutions, Rio de Janeiro, Brazil). The SAPS 3 calibration customized equation for South America was built to improve the performance of the score and it was based upon the comparison between predicted probabilities and observed results are the basis of Hosmer–Lemeshow goodness of fit test for logistic regression.
3. Statistical analysis
Comparison of demographic and clinical data of the patients (survivors and non-survivors) was accomplished by employing the 2-sample Wilcoxon rank-sum (Mann–Whitney) test for quantitative variables and Fisher exact for qualitative variables. Variables are expressed as mean ± standard deviation. The physiologic parameters on day 1 (D1) and day 3 (D3) of patients survivors and nonsurvivors were analysed as the median and range (minimum and maximum values). The capability of each index SAPS 3, SOFA, and GCS (D1 and D3) to predict mortality was analyzed by receiver operating characteristic (ROC) curve. The area under the ROC curve (AUC) and the respective confidence interval (CI) were used as a measure of the overall index accuracy. Comparison among these curves was tested as proposed by DeLong et al.[12] The significance level was set at P < .05. ROC curves analyses were performed using the software MedCalc v. 14 (Ostend, Belgium).
4. Results
Fifty-one SAH patients (33% males and 67% females; mean age of 54.1 ± 10.3 years) admitted to the ICU of a tertiary care Hospital in the immediate postoperative period were retrospectively studied. Demographic data and incidence of complications by comparison of groups of patients designated survivors (n = 37) and nonsurvivors (n = 14) are reported in Table 1. The overall mortality was 37.8%. Physiologic parameters and the components used in SOFA score calculation on day 1 (D1) and day 3 (D3) of patients are provided in Table 2. The mean SAPS 3, SOFA, and GCS on D1 were 13.5 ± 12.7, 3.1 ± 2.4, and 13.7 ± 2.8 for survivors and 32.5 ± 28.0, 5.6 ± 4.9, and 13.5 ± 1.9 for nonsurvivors, respectively. The mean SOFA and GCS on D3 were 3.6 ± 3.2 and 11.9 ± 4.8 for survivors and 8.1 ± 4.0 and 8.1 ± 5.2 for nonsurvivors, respectively. The AUC for SAPS 3, SOFA, and GCS and the respective CI data between survivors and nonsurvivors are summarized in Table 3. In the general population of the study (n = 51) the AUC and 95% CI for SAPS 3, SOFA, and GCS on D1 were 0.735 (0.592–0.848), 0.623 (0.476–0.754), 0.565 (0.419–0.703), respectively. The AUC and 95% CI for SOFA and GCS on D3 were 0.768 (0.629–0.875) and 0.708 (0.563–0.826), respectively. The pairwise comparison between indices (SOFA and GCS) on D3 did not show statistical significance (P = .06). The comparisons of ROC curves for these indices are depicted in Figure 1 (D1) and Figure 2 (D3). The means of SOFA and GCS (Table 3) demonstrated that the former above 8 predicted 78.5% of deaths, whereas the latter below 8 predicted 50%. Fischer (Grade 3 and 4), WFNS (grade 4 and 5) and Hunt–Hess (grade 4 and 5) predicted mortality in 85.7%, 50%, and 50% of cases, respectively.
Table 1.
Demographic and clinical characteristics of patients survivors and nonsurvivors of subarachnoid hemorrhage.
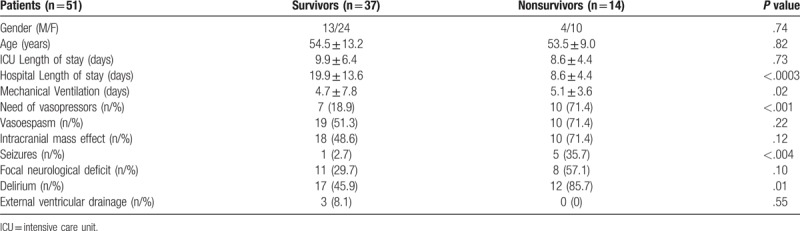
Table 2.
Physiologic parameters on day 1 (D1) and day 3 (D3) of patients survivors (n = 37) and nonsurvivors (n = 14) of subarachnoid hemorrhage.
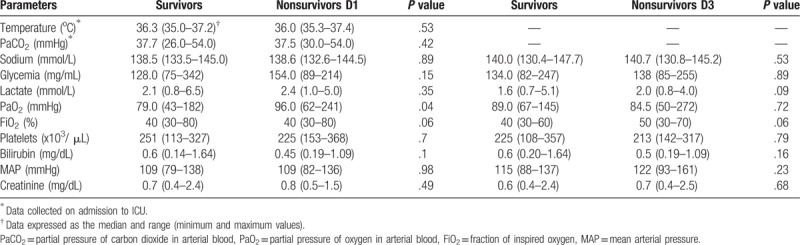
Table 3.
Values for different indices SAPS 3, SOFA and GCS scores on D1 and D3 (SOFA and GCS) and area under the receiver operating characteristic curve (AUC) with respectives 95% confidence interval (CI) of patients survivors and nonsurvivors of SAH.

Figure 1.
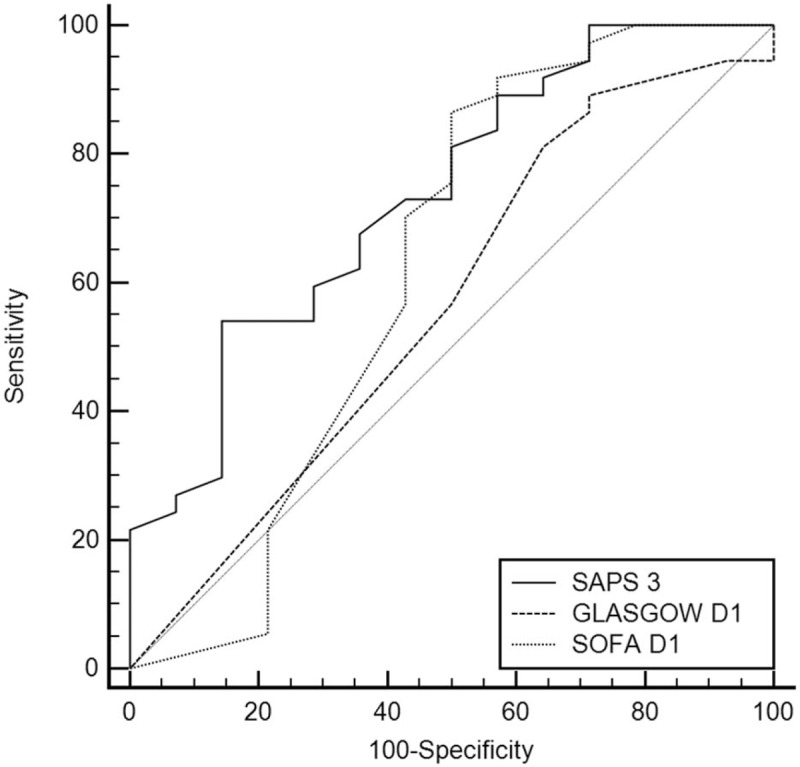
Comparison of ROC curves of SAPS 3, Glasgow Come Score and SOFA on D1. ROC = receiver-operating characteristic, SAPS 3 = Simplified Acute Physiology Score, SOFA = Sequential Organ Failure Assessment.
Figure 2.
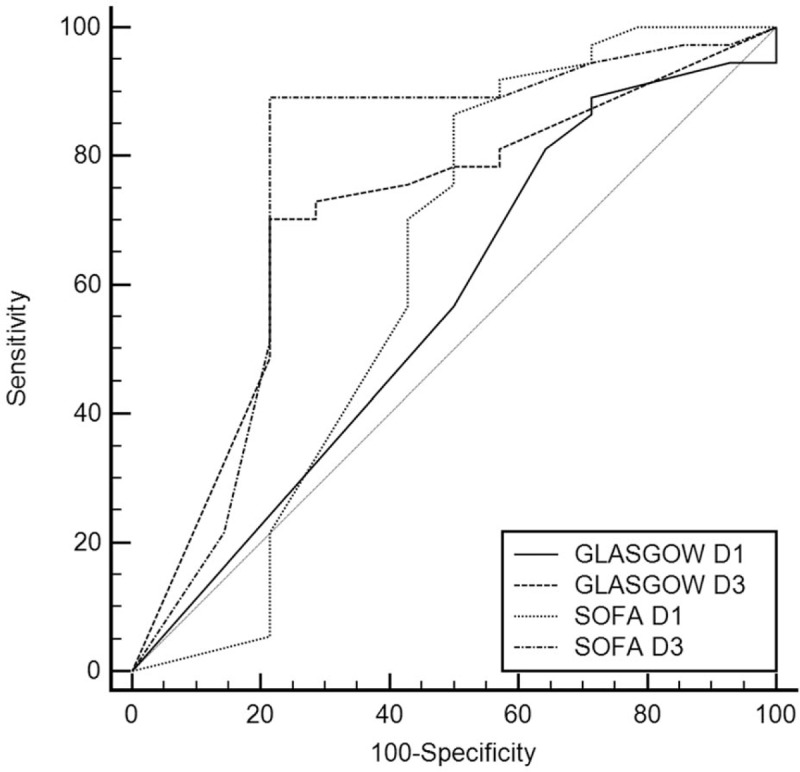
Comparison of ROC curves of GCS and SOFA on D1 and D3. GCS = Glasgow Coma Scale, ROC = receiver-operating characteristic, SOFA = Sequential Organ Failure Assessment.
5. Discussion
SAH without preceding trauma is caused by a rupture of an intracranial aneurysm in 80% of cases, followed by vascular malformations and vasculitis.[13] In USA 5% to 10% of strokes are SAH.[14] Thus, 50% of survivors, that potentially affect young adult patients, will present a poor quality of life in long-term.[15] The incidence of SAH varies worldwide. Shea et al[16] estimated 14.5 cases per 100,000 hospitalizations per year in USA. The mortality is about 50%. Vasospasm[17] and prolonged cerebral ischemia after surgery are the major causes of the high mortality observed.
Prognostic indices have been used in the past decades in patients with SAH. Among the several index employed in this clinical condition, literature reports the use of APACHE II, SAPS II, GCS, and WFNS scale. In this context, Ting et al[18] compared the predictive power of APACHE II, SAPS II, and GCS in the outcome of 154 patients with SAH. The mortality was 31.1%. These authors found an AUC of 0.846, 0.872, and 0.866 for APACHE II, SAPS II, and GCS, respectively. Furthermore, these authors concluded that the GCS is 1 of the most reliable evaluation index used to assess the level of consciousness in neurosurgical patients, especially in SAH, and therefore all other indices indices incorporate the GCS in their final score calculation. In addition, Zali et al[8] showed in 93 patients with trauma head injury associated with systemic trauma that the GCS remains, for its simplicity and effectiveness, the easiest score for brain injury. However, it seems, theoretically, that other scores such as APACHE, SAPS, and SOFA could predict better the outcome than GCS alone, since these indices include several physiologic parameters in their equations. SOFA score, for example, includes variables such as partial pressure of oxygen in arterial blood (PaO2)/FiO2 ratio (mmHg), blood platelets count (x103/μL), bilirubin (mg/dL), cardiovascular hypotension (with or without vasoactive drugs), blood creatinine (mg/dL) and GCS scale.
Indeed, the patients admitted to the ICU after SAH already have a high mortality rate, which can be incremented by pre-existing comorbidities and the involvement of other organs and systems. Some authors[19,20] have demonstrated that variables, such as hypoxemia, electrolyte (hyper/hyponatremia)[21] and acid-base imbalances, hyperglycemia and hemodynamic instability could play an independent role as predictors of mortality in SAH patients. For these reasons, after the surgical procedure of the ruptured aneurysm, these critical patients can develop several medical complications and should necessarily be placed at an ICU, with a trained staff in neurocritical care.[22] On the other hand, although the GCS is critical in the neurological patients with acute brain disorders, including SAH, this scale measurement loss its accuracy when the patient is sedated, for example, the day after de surgical procedure. Several factors have been associated with poor outcome of patients with SAH.[23–27] Rivero-Rodríguez et al[28] evaluated care-related demographic, clinical and imaging factors associated with poor prognosis in a retrospective cohort of 334 patients with SAH. The logistic regression analysis (odds ratio) showed an increased risk for some conditions, such as age > 65 years old (OR = 3.51), female sex (OR = 2.51), systolic hypertension > 60 mmHg (OR = 4.82), hyperglycemia at admission (OR = 3.93), rebleeding (OR = 16.5), vasospasm (OR = 19.0), cerebral ischemia (OR = 3.82), Fisher CT grade scale (OR = 5.18), WFNS grade 4–5 (OR = 2.09), among others factors. More recently, Galea et al[29] have found similar results in a prospective multicenter study in UK and Ireland in 3,341 patients with SAH. 68.5% were female presenting a grade I and II of WFNS (70%). These authors showed that the independent predictors of poor prognosis were age (OR = 1.04), WFNS grade (OR = 2.06), delayed cerebral ischemia (OR = 2.21), need for cerebrospinal fluid diversion (OR = 3.25) and preoperative bleeding (OR = 7.41). Park et al[6] studied retrospectively the predictive power of APACHE II and SAPS II of 672 patients admitted to a neurosurgical ICU. These authors showed that SAPS II had a significant role in predicting mortality in SAH patients. Similarly, Schuiling et al[5] observed in a cohort of 148 patients with SAH that SAPS II and WFNS scores were strong prognosticators of outcome.
Our data showed that both SOFA and GCS alone were able to predict mortality of patients with SAH since the AUC of ROC curves were similar for these indices (Table 3). We emphasize that scores such as APACHE II,[30] SAPS 3, Fischer, Hunt–Hess and WFNS are preferably performed at admission or at least within 24 hours after admission. Conversely, only SOFA and GCS can be recorded at admission and, on a daily basis, throughout the ICU stay. Thus, it should be considered the simplicity of SOFA. This score has only 6 variables, whereas APACHE II and SAPS 3 have 14 and 20 variables, respectively.
The currently available predictive systems were conceived for analysis of the severity and approximate calculation of mortality in a case mix of patients admitted to the ICU. Likewise, no prognostic index in use nowadays is able to predict mortality with 100% sensitivity and specificity in a group of patients. Moreover, these indexes are not accurate to predict individual mortality. For individuals, it is not recommended that intensivists rely only on the index and its equation for calculation of death risk.
5.1. Study limitations
This study has some limitations, such as the limited number of patients that may compromise the statistical findings and conclusions. Thus, it is a study carried out in a single center, which limits the extent of the results to other populations. Finally, the protocol design was observational and retrospective. However, through this study, we would like to deliver a message to the anesthesiologists, intensivists, and neurosurgeons, about the possible use of SOFA as prognostic index to explore not only neurological impairment used in the traditional approach but also possible organ dysfunction of patients with SAH during the ICU stay.
6. Conclusions
Prognostic systems can be helpful to predict in-hospital mortality, nevertheless, the best score system is yet to be developed. The present study gives some insight into this issue. Our data suggest that even though SAPS 3 and Fischer scale predicted outcome better on admission, SOFA and GCS were both effective indices to predict mortality in patients with SAH when performed on D3. However, because of the limited number of patients included in this study, further studies preferably multicentric with a larger cohort will be needed to corroborate these findings.
Acknowledgments
We are thankful to the Fundação de Amparo ao Ensino, Pesquisa e Assistência (FAEPA) of Clinics Hospital, Ribeirão Preto Medical School, University of São Paulo, Brazil for financial support. This study received no grant from any funding agency.
Author contributions
Conceptualization: Edson Antonio Nicolini.
Data curation: Edson Antonio Nicolini, Roosevelt Santos Nunes.
Formal analysis: Mayra Gonçalves Menegueti, Marcus Antonio Feres.
Investigation: Roosevelt Santos Nunes.
Methodology: João Paulo Uvera Ferreira.
Project administration: Anibal Basile-Filho.
Software: Silas Lucena de Lima.
Supervision: Anibal Basile-Filho.
Validation: Mayra Gonçalves Menegueti.
Visualization: Alessandra Fabiane Lago.
Writing – original draft: Anibal Basile-Filho.
Writing – review & editing: Alessandra Fabiane Lago.
Footnotes
Abbreviations: APACHE = acute physiology and chronic health evaluation, AUC = area under the ROC curve, CI = confidence interval, GCS = Glasgow Coma Scale, ICUs = intensive care units, ROC = receiver operating characteristic, SAH = subarachnoid hemorrhage, SAPS 3 = simplified acute physiology score, SOFA = sequential organ failure assessment.
The authors have no conflicts of interest to disclose.
References
- [1].Basile-Filho A, Menegueti MG, Auxiliadora-Martins M, et al. Why the surgical patients are so critical in their intensive care unit arrival. Acta Cir Bras 2013;28suppl 1:48–53. [DOI] [PubMed] [Google Scholar]
- [2].Connolly ES, Jr, Rabinstein AA, Carhuapoma JR, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American Stroke Association; American Heart Association Stroke Council; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Clinical Cardiology. Stroke 2012;43:1711–37. [DOI] [PubMed] [Google Scholar]
- [3].Fisher CM, Kistler JP, Davis JM. Relation of cerebral vasospasm to subarachnoid hemorrhage visualized by computerized tomographic scanning. Neurosurgery 1980;6:1–9. [DOI] [PubMed] [Google Scholar]
- [4].Hunt WE, Hess RM. Surgical risk as related to time of intervention in the repair of intracranial aneurysms. J Neurosurg 1968;28:14–20. [DOI] [PubMed] [Google Scholar]
- [5].Drake CG, Hunt WE, Sano K, et al. Report of world federation of neurological surgeons committee on a universal subarachnoid hemorrhage grading scale. J Neurosurg 1988;68:985–6. [DOI] [PubMed] [Google Scholar]
- [6].Schuiling WJ, de Weerd AW, Dennesen PJ, et al. The simplified acute physiology score to predict outcome in patients with subarachnoid hemorrhage. Neurosurgery 2005;57:230–6. [DOI] [PubMed] [Google Scholar]
- [7].Park SK, Chun HJ, Kim DW, et al. Acute physiology and chronic health evaluation ii and simplified acute physiology score ii in predicting hospital mortality of neurosurgical intensive care unit patients. J Korean Med Sci 2009;24:420–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zali AR, Seddighi AS, Seddighi A, et al. Comparison of the acute physiology and chronic health evaluation score (APACHE) II with GCS in predicting hospital mortality of neurosurgical intensive care unit patients. Glob J Health Sci 2012;4:179–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Metnitz PG, Moreno RP, Almeida E, et al. SAPS 3 Investigators. From evaluation of the patient to evaluation of the intensive care unit. Part 1: Objectives, methods and cohort description. Intensive Care Med 2005;31:1336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Moreno RP, Metnitz PG, Almeida E, et al. SAPS 3 Investigators. From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med 2005;31:1345–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Vincent JL, Moreno R, Takala J, et al. The SOFA. (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. on behalf of the working group on sepsis-related problems of european society of intensive care medicine. Intensive Care Med 1996;22:707–10. [DOI] [PubMed] [Google Scholar]
- [12].DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837–45. [PubMed] [Google Scholar]
- [13].Lawton MT, Vates GE. Subarachnoid hemorrhage. N Engl J Med 2017;377:257–66. [DOI] [PubMed] [Google Scholar]
- [14].Rincon F, Rossenwasser RH, Dumont A. The epidemiology of admissions of nontraumatic subarachnoid hemorrhage in the United States. Neurosurgery 2013;73:217–22. [DOI] [PubMed] [Google Scholar]
- [15].Taufique Z, May T, Meyers E, et al. Predictors of poor quality of life 1 year after subarachnoid hemorrhage. Neurosurgery 2016;78:256–64. [DOI] [PubMed] [Google Scholar]
- [16].Shea AM, Reed SD, Curtis LH, et al. Characteristics of nontraumatic subarachnoid hemorrhage in the United States in 2003. Neurosurgery 2007;61:1131–7. [DOI] [PubMed] [Google Scholar]
- [17].Macdonald RL, Pluta RM, Zhang JH. Cerebral vasospasm after subarachnoid hemorrhage: the emerging revolution. Nat Clin Pract Neurol 2007;3:256–63. [DOI] [PubMed] [Google Scholar]
- [18].Nieuwkamp DJ, Setz LE, Algra A, et al. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol 2009;8:635–42. [DOI] [PubMed] [Google Scholar]
- [19].Ting HW, Chen MS, Hsieh YC, et al. Good mortality prediction by Glasgow Coma Scale for neurosurgical patients. J Chin Med Assoc 2010;73:139–43. [DOI] [PubMed] [Google Scholar]
- [20].Gruber A, Reinprecht A, Illievich UM, et al. Extracerebral organ dysfunction and neurologic outcome after aneurysmal subarachnoid hemorrhage. Crit Care Med 1999;27:504–14. [DOI] [PubMed] [Google Scholar]
- [21].Claassen J, Vu A, Kreiter KT, et al. Effect of acute physiologic derangements on outcome after subarachnoid hemorrhage. Crit Care Med 2004;32:832–8. [DOI] [PubMed] [Google Scholar]
- [22].Qureshi AI, Suri MF, Sung GY, et al. Prognostic significance of hypernatremia and hyponatremia among patients with aneurysmal subarachnoid hemorrhage. Neurosurgery 2002;50:749–55. [DOI] [PubMed] [Google Scholar]
- [23].Samuels O, Webb A, Culler S, et al. Impact of a dedicated neurocritical care team in treating patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care 2011;14:334–40. [DOI] [PubMed] [Google Scholar]
- [24].Frontera JA, Fernandez A, Claassen J, et al. Hyperglycemia after SAH: predictors, associated complications, and impact on outcome. Stroke 2006;37:199–203. [DOI] [PubMed] [Google Scholar]
- [25].Rosengart AJ, Schultheiss KE, Tolentino J. Macdonald RL prognostic factors for outcome in patients with aneurysmal subarachnoid hemorrhage. Stroke 2007;38:2315–21. [DOI] [PubMed] [Google Scholar]
- [26].Langham J, Reeves BC, Lindsay KW, et al. Browne JP; steering group for national study of subarachnoid haemorrhage. variation in outcome after subarachnoid hemorrhage: a study of neurosurgical units in UK and Ireland. Stroke 2009;40:111–8. [DOI] [PubMed] [Google Scholar]
- [27].Kurtz P, Claassen J, Helbok R, et al. Systemic glucose variability predicts cerebral metabolic distress and mortality after subarachnoid hemorrhage: a retrospective observational study. Crit Care 2014;18:R89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rivero Rodríguez D, Scherle Matamoros C, Fernández Cúe L, et al. Factors associated with poor outcome for aneurysmal subarachnoid haemorrhage in a series of 334 patients. Neurologia 2017;32:15–21. [DOI] [PubMed] [Google Scholar]
- [29].Galea JP, Dulhanty L, Patel HC. UK and ireland subarachnoid hemorrhage database collaborators. predictors of outcome in aneurysmal subarachnoid hemorrhage patients: observations from a multicenter data set. Stroke 2017;48:2958–63. [DOI] [PubMed] [Google Scholar]
- [30].Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818–29. [PubMed] [Google Scholar]


