Abstract
The aim of this study was to illuminate risks factors of residual lesions, and recurrence of the high-grade cervical intraepithelial lesions (HSIL) patients with positive margin who underwent cervical conization.
A retrospective cohort study of 218 patients with positive margin after conization, including cold knife conization (CKC) and loop electrosurgical excisional procedure (LEEP), and follow-up from 2013 through 2016. The diagnosis of residual disease and recurrence were established and confirmed by biopsy. We evaluate the correlations among residual rate, recurrence rate, and clinical parameters, such as age, menopausal status, gravity, parity, glandular involvement, thinprep cytologic test (TCT), and human papillomavirus (HPV) results. We also detect the difference between CKC and LEEP.
There was statistical difference between the positive margin rate of CKC group and LEEP regarding the surgery methods (5.8% and 12.09% separately, P < .001). Residual disease was found in 53.66% cases where 41 patients received second surgery after conization. Besides, age (P = .027), menopausal status (P = .006), and HPV infection (P = 0.018) were significantly associated with residual lesion. Among 177 cases with histopathologic follow-up, 15.91% women relapsed from 4 to 27 months. As for recurrence we found it was more frequent with HPV infection and glandular involvement (P < .001). TCT was also an independent factor in patients with recurrence of lesion. No evidence shows difference between CKC and LEEP for recurrence rate (P = .918).
The factors related to rate of residual lesion were age, menopausal status, and HPV infection. HPV infection, TCT, and glandular involvement were associated with HSIL recurrence. LEEP was as effective as CKC with regard to recurrence rate. Further large-scale studies are needed to confirm our findings.
Keywords: cold knife conization, high-grade cervical intraepithelial lesions, loop electrosurgical excisional procedure, positive margin, recurrence, residual lesion
1. Introduction
The incidence of cervical cancer, one of the most common gynecological tumors, has been continuously increasing in recent decades. Cervical intraepithelial neoplasia (CIN) is a precursor of cervical cancer. Untreated high grade CIN significantly increases the risk of invasive cancer. Accurate and standardized treatment of cervical lesions, especially high-grade cervical intraepithelial lesions (HSIL), is considered as the most important method to prevent cervical cancer. Conization currently is one of the main treatments of cervical precancerous lesions, which plays both diagnostic and therapeutic roles CIN.[1] It can remove as well as clarify the extent of cervical lesions. Both the dual roles have a great value. Cold knife conization (CKC) and loop electrosurgical excisional procedure (LEEP) are the most common strategy.[2] However, there are still around 15% of patients relapse or residual after surgery.[3] Recurrence and progression are the most worried problems caused by residual lesion.[4] Evidence indicates that margin involvement, histopathological CIN grade, glandular involvement, persistent human papillomavirus (HPV) infection, age, and immunosuppression are predictive factors associated with CIN residual and recurrence rate.[5–10] Positive margin is always regarded as a high risk factor for residual lesion and recurrence.[4] However, the best way for follow-up treatment in these patients is inconsistent. There are 3 management options: thinprep cytologic test (TCT), HPV, and colposcopic in close follow-up; repeat conization and hysterectomy.[11,12]
Many researchers have figured out few difference of effect between CKC and LEEP,[13] and LEEP appears to be as equally effective as CKC to some degree. However, no analysis focusing on the positive margin patients has been published up to date. The purpose of this study is to compare the residue, recurrence rate of LEEP, CKC in the treatment of HSIL patients with positive margins. The study is also to investigate the relevant factors for residual disease according to demographic data and various pathologic parameters.
2. Methods
2.1. Case selection
Case inclusion criteria: patients with positive margin, who had been diagnosed as HSIL by biopsy, including CIN II–III.
Case exclusion criteria: patients with complications, such as endometrial carcinoma; cervical cancer including microinvasion; patients who were lost contact; and information incomplete, such as lacking of correlation among cytology, biopsy, colposcopic findings, and losing reports of postoperational text in follow-up.
A total of 218 patients who had been diagnosed as HSIL, including CIN II–III, underwent cervical conization at the Department of Obstetrics and Gynecology, Qilu Hospital of Shandong University from January 2013 to December 2016, were diagnosed by “three-step” method, cytology-colposcopy-histology,[14] and the biopsy-proved HSIL before the surgery. Age, gravidity, and parity of patients and the operation process were recorded. A total of 77 patients received CKC and 139 received LEEP depends on the fertility requirements, age, lesion, and patients’ choice.
2.2. Treatment method
Iodine smears the cervix before excision to determine the scope of surgery. Excise along the 0.5 cm outside of the noncoloring area from the lesion. As for LEEP, the surgical procedures were performed under colposcopic guidance. A suture was placed of the cone specimen for mark and then the specimen was fixed with 10% neutral formalin and embedded in paraffin for the pathologic examination. All specimens were processed with a standardized method. The paraffin-blocked slides were observed by 2 trained independent pathologists to prove the histological diagnosis and pathological grade without knowledge of the patients’ condition. If the pathological findings were inconsistent with multiple results, colposcopy, biopsy, and the pathologic exam, in 1 patient, the highest level of lesions were regarded as the final result. A total of 41 patients with positive margins, reported by postoperative pathological, received secondary surgery, such as hysterectomy, LEEP, and CKC, within 3 months after the first operation. Based on the archived data several variables were assessed, including age, gravidity, parity, results of cytology, and cervical biopsy, histopathologic results of cone specimen (surgical margin and glandular involvement), and histopathologic signs of HPV.
2.3. Follow-up after treatment
All the after-cone patients were reviewed regularly in our outpatient clinic department or local hospital. Long-term follow-up was provided by reviewing hospital records, but also by collecting data directly from the reports of patients. TCT, HPV examination, and colposcopy were examined at each after-surgery visit. When atypical cells (atypical squamous cells, highly indicates the existence of high grade-cervical lesions [ASC-US] or higher) were detected and/or HPV positive, a colposcopy-directed punch biopsy was recommended, which was regarded as the golden standard. And these samples were examined by experienced pathologists. The follow-up deadline was November 2017, and mean follow-up period was 20 months, the range of 11 to 56 months, in our study period.
2.4. Criteria for positive margins, residual lesions, and recurrent lesions
Women who had 2 or more consecutive negative postoperative biopsies were considered as being free of residual lesions, irrespective of the results of the HPV or TCT test in our study. If HSIL lesions were found in the resection margin, including ectocervical margin, endocervical margin, or both, of about 100 μm or less, it would be regarded as the positive margin. If HSIL lesions were diagnosed in women who underwent secondary surgery within 3 months, we assumed that it was a residual lesion. If HSIL was diagnosed in 3 months later after surgery, it was regarded as a recurrent lesion, which needs to be proved by the colposcopy-directed punch biopsy or postoperation pathology. CIN1 was not considered as residual or recurrence in this study. All procedures were approved by the Ethics Committee of Shandong University [2018 (054)].
2.5. Statistical analysis
Statistical analysis was performed using IBM SPSS for Windows (version 22.0). χ2 test was used to compare the positive margins rate, residual, and recurrence between CKC group and LEEP group. Association of gravidity, parity and HPV infection in residual lesion and gravidity, parity TCT, and glandular involvement in recurrence were estimated using χ2 test. Fisher test was used to analyze the rest values which were <5. The survival curves were compared using log-rank. For all statistical tests, the differences were considered statistically significant when P-values were <.05.
3. Results
3.1. Clinical presentation
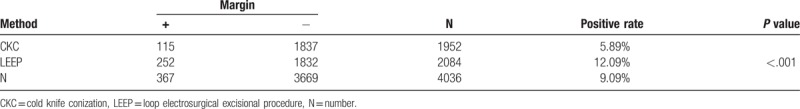
A total of 4036 patients who were diagnosed as HSIL by biopsy, received conization treatments in Qilu Hospital during the study period. A total of 1952 patients received CKC treatment (meaning scope of operations was 2.55 × 2.85 cm), therein, 115 patients were reported as positive margins in their postoperative pathological report. Meanwhile, in 2084 patients who received LEEP (meaning scope of operations was 1.55 × 1.60 cm), 252 patients were diagnosed as positive margins. The positive margin rate of CKC group and LEEP group were 5.8% and 12.09% separately, and there was statistical difference between CKC group and LEEP regarding the surgery methods (P < .001) (Table 1).
Table 1.
Comparison of positive margins rate between CKC group and LEEP group.
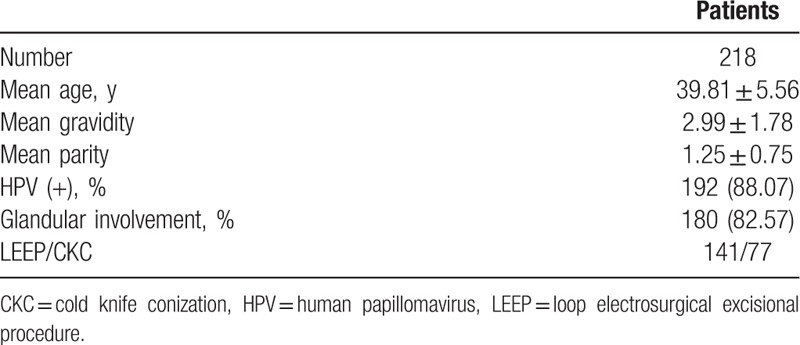
Overall, 367 patients were diagnosed as positive margins during the study period. In the final diagnosis, there were 31 cases of cervical cancer or microinvasive carcinoma, 97 cases of lost contact or information incomplete (lacking of correlation among cytology, biopsy, and colposcopic findings and losing information about postoperational text in follow-up). All of them were excluded from the study. The remaining 218 women with positive margins were enrolled in our study and evaluated for statistical analysis. The characteristics of this group are shown in Table 2. The mean age was 39.86 (±5.56) years old, ranged from 23 to 64. The mean gravity was 2.99 (±1.78) and the mean parity was 1.24 (±0.75). A total of 192 (88.07%) women were HPV infected, and 180 (82.57%) women were glandular involvement.
Table 2.
The characteristics of patients with positive margin.
3.2. Association between residual disease and clinicopathological factors
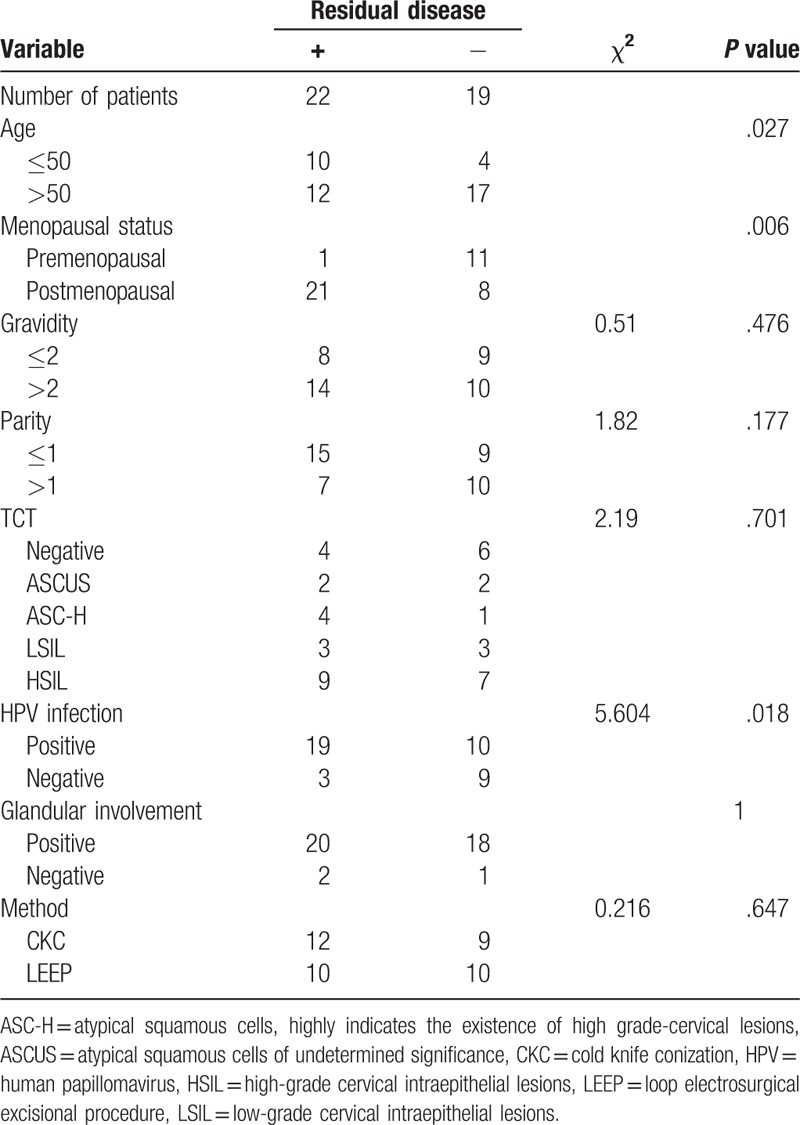
A total of 41 patients underwent secondary operation within 3 month, and of them, 32 cases received hysterectomy, 9 cases chose repeat conizations (5 cases in LEEP and 4 cases in CKC). Residual lesions were found in the specimens obtaining from hysterectomy or repeated conization of 22 of the 41 patients (53.66%) and clinicopathological factors are summarized in Table 3. There were less predictive value for residual lesion regarding gravidity (P = .476), parity (P = .177), TCT (P = .701), and glandular involvement (P = 1). Other parameters such as age (P = 0.027), menopause status (P = .006), and HPV infection (P = .018) were significant factors for residual disease. No statistical difference between rates of residual lesions regarding the surgery methods (P = .647) was found. None of the 41 patients were found recurrence during the follow-up time.
Table 3.
Association between clinicopathological factors and residual lesion.
3.3. Clinical characteristics of recurrent patients with positive margin
The follow-up deadline was November 31, 2017, and 177 patients were followed regularly during our study period, mean follow-up time was 20 months, ranging from 11 to 56 months. Nine (18.07%) of 56 cases in CKC group with positive margins were reported as recurrence by colposcopy-directed biopsy, compared to 19 (15.70%) of 121 cases following LEEP group with positive margins and there was no big difference between 2 groups (P = .918, Table 4). The first recurrence took place in the fourth month among the compromised margin patients, and the mean time of recurrent time was 9.5 months. Eleven cases of the 27 patients with HSIL recurrent lesions received hysterectomy; 13 cases choose relatively conservative management including repeat CKC and LEEP. One case of whom were diagnosed as residual lesions again and received hysterectomy during follow-up visits. Three patients chose to follow up closely even though they were reported as recurrent lesions by colposcopy-directed biopsy. HPV turning negative from positive was observed in most of the patients who had received the hysterectomy, but only 1 patient with persistent HPV infection was diagnosed as vaginal intraepithelial neoplasia.
Table 4.
Recurrence between CKC and LEEP.
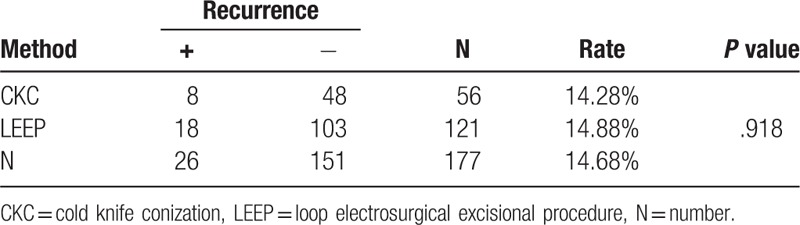
A total of 177 patients were followed regularly during this period. Recurrence cervical lesions were identified in 26 (14.68%) totally. No squamous cell carcinoma or adenocarcinoma was diagnosed during the follow-up period. The characteristics of the recurrence patients are summarized in Table 5.
Table 5.
The characteristics of the recurrence patients with positive margins.
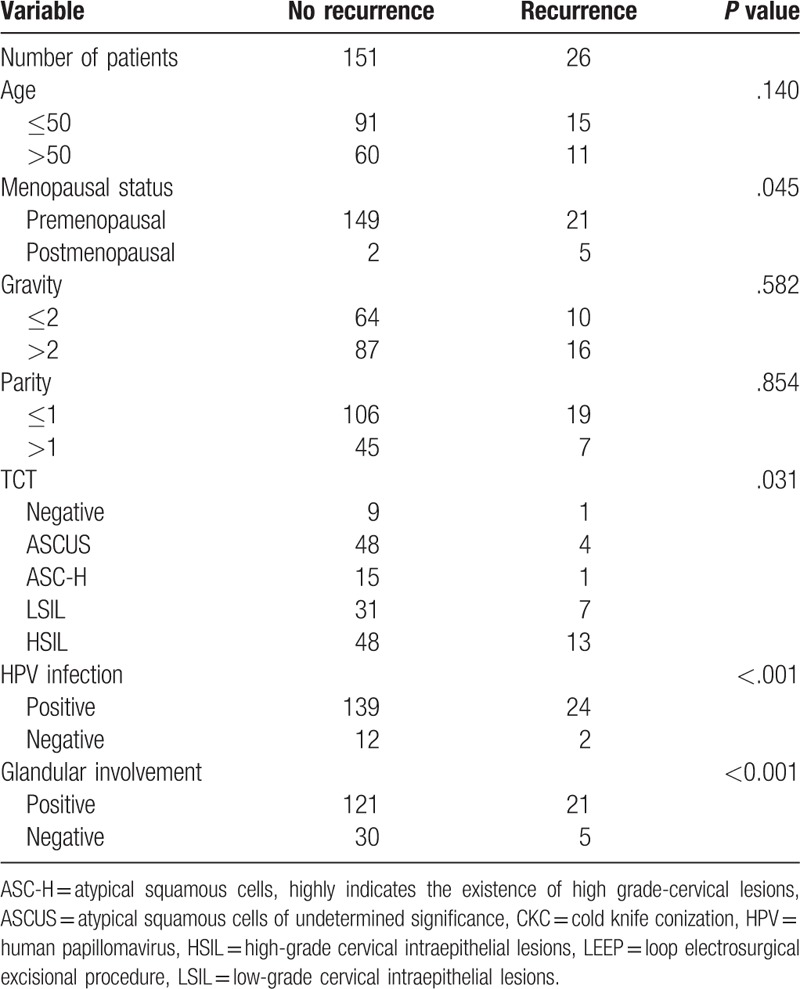
There was no significant difference for the recurrence of CIN in women with positive margins older than 50 years (P = .140). Moreover, there were no statistical difference between the 2 groups regarding the number of gravity (P = .419) and parity (P = .765). Recurrence of CIN was observed in 92.31% of HPV-infected women with positive margins compared to 7.69% of HPV-noninfected women with positive margins (P < .001, Fig. 1). Glandular involvement was correlated with 80.77% of cases with positive margins, while recurrence without glandular involvement was observed only in 18.23% of patients with positive margins (P < .001, Fig. 2). A higher frequency of recurrent of lesions was found when HSIL shown in TCT results (P = .031). Menopausal status and TCT results were also associated with recurrence in patients with positive margins (P = .045 and P = .031, respectively).
Figure 1.
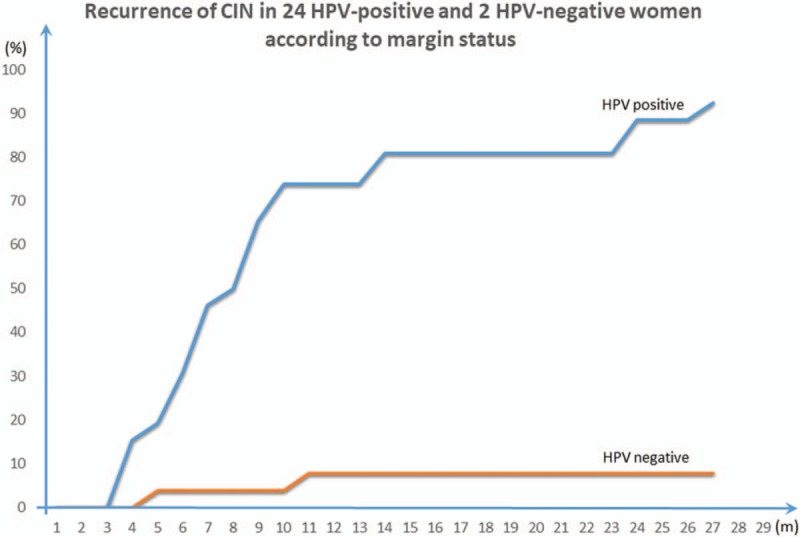
Recurrence of CIN in 24 HPV-positive and 2 HPV-negative women according to margin status.
Figure 2.
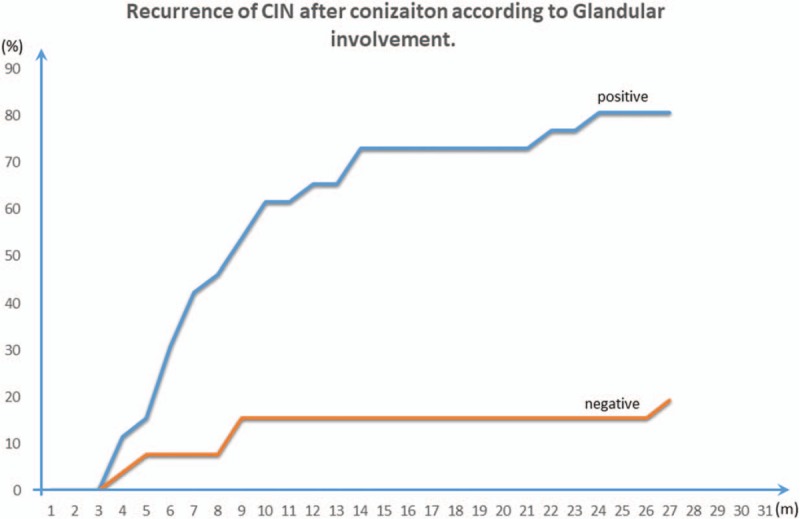
Recurrence of CIN after conization according to Glandular involvement.
4. Discussion
Active and effective treatment of HSIL is the significant approach to control the occurrence and development of cervical cancer. Cervical conization is the standardized treatment for HSIL, especially for cervical cancer occurred on an increasing number of young women recent years. For young patients, it is better to receive conservative treatments which help them to retain their reproductive function. However, previous studies observed that residual lesions and recurrence may obviously occur following both procedures.[10] Identification of risk factors may guide therapeutic decisions in following treatment steps. The positive margins after cervical conization are generally considered to be a risk factor for the recurrence or persistence of CIN currently.[4] When positive margin exists, there are 3 management options: TCT, HPV, and colposcopic in close follow-up; repeat conization (including CKC and LEEP again); and hysterectomy.[11,12] The choice making is mainly influenced by the patients’ demand for fertility, age, compliance of follow-up, and the probability of residual disease. The probability of residual lesions and recurrent lesions is a focus of attention for patients and doctors. Our research was focusing on the group of patients with positive margin after cervical conization and aimed to find out the related factors of residual disease as well as the recurrence and figured out a better way to treat HSIL by comparing the difference between LEEP and CKC.
4.1. Factors related to residue lesions
The total residual rate in this research was 53.66%, which was consistent with the result found by Sankasem et al.[15,16] In Sankasem et al's result, the factor “age” was identified as the predictive factor of residual disease.[17,18] Fortunately, based on data we had, our study came to the almost identical conclusion. High rate of residual lesion after cervical conization may be associated with the multicenter pathopoiesis of cervical lesions, except the cervical squamous column junction where was most easily affected, other parts can be infected simultaneously or successively. We chose 50 years old as a cut off age, which also indicated that high frequency of residual disease was found in patients who were postmenopausal. It applied that the higher incidence of incomplete excision in elder patients, which may be relative to increasing surgical difficulties by atrophy of the genital tract as well as deep inversion of the transformation zone. Besides, we also found in our study that HPV-infected females have higher residual rate than noninfected women (P = .092), which was consistent with previous reports that HPV was the risk factor of postoperative residual disease.[18] However, gravidity and parity were not found to be predictive of residual disease in our study, coinciding with the research of Moore et al, which identified a correlation between parity and residual diseases.[19] Moreover, TCT examination and residual lesions had no significant correlation, suggesting that TCT examination cannot be a prediction signal for residual lesions after conizations. In addition, glandular involvement (P = 1) may be only a causative factor for CIN. Therefore, appropriate excision range and special individual treatment are important for people who were relatively older patients. According to our study, for these female patients with HSIL and over 50, due to high HPV positive, we recommend a second operation, especially for these with follow-up difficulties. At the same time, patients’ fertility requirements should be considered. Others should be under regular follow-up for long period, including the cervical cytology and HPV and colposcopy examination, biopsy or secondary LEEP, which may help to find residual or recurrence of cervical lesions timely. More accurate prediction of postcone residual disease before the execution of hysterectomy by various predictive factors should be emphasized and more diagnostic tools should be further investigated.
4.2. Factors associated with recurrence
A total of 177 patients with positive margins chose to follow-up after first surgery during our study period. Overall recurrence rate was 14.68% in our study. Our results supported the findings of all previous series that CIN was hard to cure. van Hamont's study found that 80.3% recurrence of cervical conization occurred within 24 months after surgery.[20] A total of 96% of the lesions recurrences within 24 months in our study, consistent with the findings of van Hamont et al. Close and regular follow-up is necessary for patients with positive margins in order to find recurrence in time
Age, gravity, and parity were not significantly different for the recurrence of CIN between groups in our study, and this finding was supported by Alonso et al,[6] while other articles show that age, lesion grade, and margin involvement were significant predictors of HPV persistence and CIN recurrence after the treatment.[21] We found that HPV-infected women were significantly more likely to recurrent than HPV noninfected women (P < .001). It has been confirmed that high-risk HPV persistent infection was the critical cause of cervical cancer. In the study of 162 patients with HPVs positive, the infection rate was as high as 92%. Further study discovered that HPV infection and disease recurrence were closely correlated (P < .001). The presence glandular involvement (P < .001) in female was significantly different between groups, in accordance with what had been reported elsewhere.[5] The possible reason may be that the degree of cell proliferation than the latter caused by involvement of the gland. In the present study, different grades of TCT results were related to the recurrence condition. HSIL were regarded as a high risk factor for recurrence. TCT test can be a prediction signal for recurrence in patients with positive margins, while cannot infer the residual lesions after conization. Recurrence occurred more often in premenopausal female (P = .045), which were contrast to our beginning thoughts.
4.3. Comparison between CKC and LEEP
Cervical conization, including LEEP and CKC, is the main procedure. Due to the low cost, less bleeding during operation, and the low incidence of postoperative cervical insufficiency, LEEP is becoming more and more popular in surgical method chosen not only in domestic but also in foreign countries.[11] Besides, the relationship between conization and postoperative margins and residual lesions remains controversial. For example, a previous review reported that the prevalence of residual and recurrent disease after incomplete LEEP did not differ significantly compared with the results after knife-cone biopsy,[22] no significant difference were found in residual and recurrence rate regarding the choice of treatment in our study. However, the positive margin rate of CKC group and LEEP group were 5.8% and 12.09%, respectively (P = .918). We assumed that there were several reasons those cause the difference between 2 methods. First, the average massive and depth in LEEP is smaller compared to CKC, which might cause incomplete removal of lesion in LEEP. And the massive of lesion also affect the choice of treatment. Second, patients with high-grade lesion were tended to receive CKC rather than LEEP. The degree of disease could lead to discrepancy. Third, the results might be influenced by the burning margin because the high frequency electrotome was performed in LEEP, affecting the accuracy and reliability of the conclusion.
4.4. Limitations
There were still some limitations in our research. Firstly, the sample size was not big enough and the loss to follow-up due to many patients refuse to give the information. For a more accurate evaluation, increasing the numbers in the future study may be necessary. Secondly, different measures were performed on the secondary surgery of postconization, the residual rate probably may be influenced by the choice of methods. Due to a small number of samples, further researches were needed to prove our ideas. Thirdly, the HPV genotype and virus amount were not investigated in our study because different professors or hospitals chose different ways, which was hard to control. Many reports indicate that the genotype of HPV, especially high risk HPV, such as HPV16 and 18, may cause higher recurrence rate.[10] And it would be better to study more genotypes to confirm our result. The possible factor for positive margin was not included in our study, which will be the next goal for our team.
In conclusion, age, menopausal status, and glandular involvement were tightly linked to the residual disease. TCT, HPV infection, and glandular involvement were predictive factors for recurrence. No statistical difference was found between LEEP and CKC regarding to recurrence rate. Further large-scale studies are needed to confirm our findings.
Author contributions
Conceptualization: Jun-yu Chen.
Data curation: Jun-yu Chen, Zhi-ling Wang.
Formal analysis: Jun-yu Chen.
Software: Zhao-yang Wang.
Writing – original draft: Jun-yu Chen, Zhi-ling Wang.
Writing – review and editing: Xing-sheng Yang.
Footnotes
Abbreviations: CIN = cervical intraepithelial neoplasia, CKC = cold knife conization, HPV = human papillomavirus, HSIL = high-grade cervical intraepithelial lesions, LEEP = loop electrosurgical excisional procedure, TCT = thinprep cytologic test, VAIN = vaginal intraepithelial neoplasia.
J-yC and Z-lW contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kyrgiou M, Tsoumpou I, Vrekoussis T, et al. The up-to-date evidence on colposcopy practice and treatment of cervical intraepithelial neoplasia: the Cochrane colposcopy & cervical cytopathology collaborative group (C5 group) approach. Cancer Treat Rev 2006;32:516–23. [DOI] [PubMed] [Google Scholar]
- [2].Sadler L, Saftlas A, Wang W, et al. Treatment for cervical intraepithelial neoplasia and risk of preterm delivery. JAMA 2004;291:2100–6. [DOI] [PubMed] [Google Scholar]
- [3].Kocken M, Helmerhorst TJ, Berkhof J, et al. Risk of recurrent high-grade cervical intraepithelial neoplasia after successful treatment: a long-term multi-cohort study. Lancet Oncol 2011;12:441–50. [DOI] [PubMed] [Google Scholar]
- [4].Wright TC, Jr, Cox JT, Massad LS, et al. 2001 Consensus guidelines for the management of women with cervical intraepithelial neoplasia. J Low Genital Tract Dis 2003;7:154–67. [DOI] [PubMed] [Google Scholar]
- [5].Lima MI, Tafuri A, Araujo AC, et al. Cervical intraepithelial neoplasia recurrence after conization in HIV-positive and HIV-negative women. Int J Gynaecol Obstet 2009;104:100–4. [DOI] [PubMed] [Google Scholar]
- [6].Alonso I, Torne A, Puig-Tintore LM, et al. Pre- and post-conization high-risk HPV testing predicts residual/recurrent disease in patients treated for CIN 2-3. Gynecol Oncol 2006;103:631–6. [DOI] [PubMed] [Google Scholar]
- [7].Fogle RH, Spann CO, Easley KA, et al. Predictors of cervical dysplasia after the loop electrosurgical excision procedure in an inner-city population. J Reprod Med 2004;49:481–6. [PubMed] [Google Scholar]
- [8].Heard I, Potard V, Foulot H, et al. High rate of recurrence of cervical intraepithelial neoplasia after surgery in HIV-positive women. J Acquir Immune Defic Syndr 2005;39:412–8. [DOI] [PubMed] [Google Scholar]
- [9].Prato B, Ghelardi A, Gadducci A, et al. Correlation of recurrence rates and times with posttreatment human papillomavirus status in patients treated with loop electrosurgical excision procedure conization for cervical squamous intraepithelial lesions. Int J Gynecol Cancer 2008;18:90–4. [DOI] [PubMed] [Google Scholar]
- [10].Park JY, Kim DY, Kim JH, et al. Human papillomavirus test after conization in predicting residual disease in subsequent hysterectomy specimens. Obstet Gynecol 2009;114:87–92. [DOI] [PubMed] [Google Scholar]
- [11].Lapaquette TK, Dinh TV, Hannigan EV, et al. Management of patients with positive margins after cervical conization. Obstet Gynecol 1993;82:440–3. [PubMed] [Google Scholar]
- [12].Watson AJ, Tuffnell DJ, Lowe JW, et al. The incomplete cone biopsy: a comparison of conservative and surgical management. Eur J Obstet Gynecol Reprod Biol 1993;51:119–23. [DOI] [PubMed] [Google Scholar]
- [13].Jiang YM, Chen CX, Li L. Meta-analysis of cold-knife conization versus loop electrosurgical excision procedure for cervical intraepithelial neoplasia. Onco Targets Ther 2016;9:3907–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Coccia PF, Pappo AS, Beaupin L, et al. Adolescent and Young Adult Oncology, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2018;16:66–97. [DOI] [PubMed] [Google Scholar]
- [15].Cardoza-Favarato G, Fadare O. High-grade squamous intraepithelial lesion (CIN 2 and 3) excised with negative margins by loop electrosurgical excision procedure: the significance of CIN 1 at the margins of excision. Hum Pathol 2007;38:781–6. [DOI] [PubMed] [Google Scholar]
- [16].Sankasem A, Thavaramara T, Manusirivithaya S, et al. Tumor persistence in high grade squamous intraepithelial lesion patients with positive surgical margin post loop electrosurgical excision procedure. J Med Assoc Thai 2006;89:934–40. [PubMed] [Google Scholar]
- [17].Kalogirou D, Antoniou G, Karakitsos P, et al. Predictive factors used to justify hysterectomy after loop conization: increasing age and severity of disease. Eur J Gynaecol Oncol 1997;18:113–6. [PubMed] [Google Scholar]
- [18].Park JY, Lee SM, Yoo CW, et al. Risk factors predicting residual disease in subsequent hysterectomy following conization for cervical intraepithelial neoplasia (CIN) III and microinvasive cervical cancer. Gynecol Oncol 2007;107:39–44. [DOI] [PubMed] [Google Scholar]
- [19].Moore BC, Higgins RV, Laurent SL, et al. Predictive factors from cold knife conization for residual cervical intraepithelial neoplasia in subsequent hysterectomy. Am J Obstet Gynecol 1995;173:361–6. discussion 366–368. [DOI] [PubMed] [Google Scholar]
- [20].van Hamont D, van Ham MA, Struik-van der Zanden PH, et al. Long-term follow-up after large-loop excision of the transformation zone: evaluation of 22 years treatment of high-grade cervical intraepithelial neoplasia. Int J Gynecol Cancer 2006;16:615–9. [DOI] [PubMed] [Google Scholar]
- [21].Costa S, De Simone P, Venturoli S, et al. Factors predicting human papillomavirus clearance in cervical intraepithelial neoplasia lesions treated by conization. Gynecol Oncol 2003;90:358–65. [DOI] [PubMed] [Google Scholar]
- [22].Ghaem-Maghami S, Sagi S, Majeed G, et al. Incomplete excision of cervical intraepithelial neoplasia and risk of treatment failure: a meta-analysis. Lancet Oncol 2007;8:985–93. [DOI] [PubMed] [Google Scholar]


