Abstract
Objective
To determine the dose response to weight loss on clinical and mechanistic outcomes in overweight and obese adults with knee osteoarthritis.
Methods
This is a secondary analysis of the diet-only (D) and diet plus exercise (D+E) groups in the Intensive Diet and Exercise for Arthritis (IDEA) randomized controlled clinical trial. Participants were 240 overweight and obese older community-dwelling adults with pain and radiographic knee OA. Participants were divided into 4 groups according to weight loss achieved over an 18-month period; less than 5% (<5% group), between 5 and 10% (≥5% group), between 10 and 20% (≥ 10% group), and greater than 20% (≥20% group).
Results
There were significant dose responses to weight loss for pain (p = 0.01), function (p = 0.0006), 6-minute walk distance (p < 0.0001), physical (p = 0.0004) and mental (p = 0.03) health- related quality of life (HRQL), knee joint compressive force (p < 0.0001), and IL-6 (p = 0.002). Greater weight loss resulted in superior clinical and mechanstic outcomes with the highest weight loss group (≥20% group) distinguishing itself on all measures compared to the <5% and ≥5% groups; the ≥20% group had 25% less pain and better function than the ≥ 10% group, and significantly (p = 0.006) better physical HRQL.
Discussion
Long-term weight loss between 10–19.9% of baseline body weight has substantial clinical and mechanistic benefits compared to less weight loss; the value of an additional 10% weight loss includes significantly improved physical HRQL, and a clinically important reduction in pain and improvement in function.
Obesity is a health issue worldwide and a major and modifiable risk factor for many of the over 250 million people afflicted with knee osteoarthritis (OA) [1–4]. Previous weight loss studies in overweight and obese adults with knee OA conducted in highly controlled [5] and community-based environments [6] found similar significant responses; 10% weight loss resulted in less pain, better function, improved health-related quality of life (HRQL), reduced knee joint loads, and lower inflammation than in groups that did not lose weight or lost less than 10%. These data are consistent with the NIH recommendation for overweight and obese adults to lose 10% of baseline weight as an initial goal [7]. Moreover, recent observational data from the Osteoarthritis Initiative (OAI) indicates that greater weight loss is associated with less cartilage degradation [8].
Most randomized controlled weight loss trials in older overweight and obese adults with knee OA report between 5 and 10% weight reduction after 1 to 2 years [5, 9, 10]. Data from the National Weight Control Registry indicate that some patients lose and maintain more than twice that weight loss [9, 11–15]. However, whether weight loss of this magnitude can be achieved non-surgically under randomized clinical trial conditions and whether there is any benefit beyond what has been shown with 10% weight loss in a knee OA population is unknown.
Achieving significant weight loss without regain is difficult. The body acts in starvation mode, increasing feelings of hunger. It suppresses satiety, slows metabolic rate, and attempts to defend higher body weights [16]. Therefore, to justify the effort needed by patients to achieve a more substantial intentional weight loss than what is proven effective in randomized clinical trials the outcomes should be significantly better with minimal adverse side effects [5, 6, 10]. We performed a secondary analysis of our IDEA weight loss groups (diet and diet plus exercise) to determine if participants who lost twice the 10% group average had significantly better clinical and mechanistic outcomes at 18-month follow-up. We hypothesized that participants who lost ≥ 20% of baseline body weight would have significantly reduced pain, knee joint loads, and systemic inflammation, and improved function and health related quality of life compared to participants who lost <5%, between 5 and 9.9%, and between 10 and 19.9% of their baseline body weight.
MATERIALS AND METHODS
Study Design
Intensive Diet and Exercise for Arthritis (IDEA) was a single-blind, single-center, 18-month, randomized controlled trial conducted at Wake Forest University and Wake Forest School of Medicine between July 2006 and April 2011. Participants were randomized into one of three groups: Diet + Exercise (D+E), Diet (D), or Exercise (E). Data from the D and D+E groups were used for this dose-response analysis. Trial design and rationale, and the primary outcomes of the trial are detailed elsewhere [5, 17]. The study was approved by the Human Subjects Committee of Wake Forest Health Sciences. Informed consent was obtained verbally and in writing from all participants.
Study Sample
The sample consisted of ambulatory, community-dwelling persons age ≥ 55 years with: (1) Kellgren-Lawrence (KL) grade 2 or 3 (mild or moderate) radiographic tibiofemoral OA or tibiofemoral plus patellofemoral OA of one or both knees [18], (2) pain on most days due to knee OA, (3) 27 kg·m−2 ≤ Body Mass Index (BMI) ≤ 41 kg·m−2, and (4) a sedentary lifestyle (< 30 min·wk−1 of formal exercise for the past 6 months). Participants maintained and adjusted their usual medications as needed with their physician’s consent.
D+E and D participants were classified into weight loss categories based on percent loss in body weight at 18 months according to the following categories: less than 5% (<5% group), between 5 and 9.9% (≥5% group), between 10 and 19.9% (≥ 10% group), and 20% and greater (≥20% group). The ≥5% and ≥ 10% weight loss categories reflect the weight loss goals achieved in ADAPT [9] and IDEA [5], respectively; the ≥20% was twice the weight loss in IDEA and the ≤5% group was considered not achieving a significant weight loss compared to the healthy lifestyle control group in ADAPT.
Interventions
The D group received the dietary weight loss intervention, and the D+E group received both diet and exercise interventions.
Intensive weight loss intervention
The goal of this intervention was a mean group loss of at least 10% of baseline weight, with a desired range between 10% and 15%. The diet was based on partial meal replacements, including up to 2 meal-replacement shakes per day (Lean Shake®, provided by General Nutrition Centers, Inc., Pittsburgh, PA.). For the third meal, participants followed a weekly menu plan with recipes that were 500–750 kcals, low in fat, and high in vegetables. Daily caloric intake was adjusted according to the rate of weight change between intervention visits.
The initial diet plan provided an energy-intake deficit of 800–1000 kcals·d−1 as predicted by energy expenditure (estimated resting metabolism × 1.2 activity factor) with at least 1100 kcals for women and 1200 kcals for men. The calorie distribution goal was 15–20% from protein, < 30% from fat, and 45–60% from carbohydrates, consistent with the Dietary Reference Intakes for Energy and Macronutrients [19] and successful weight-loss programs [20]. As follow-up progressed, fewer meal replacements were consumed. Body weight was monitored weekly or biweekly during nutrition education and behavioral sessions that were developed within a social cognitive theoretical framework: from months 1–6, one individual session and 3 group sessions per month, and from months 7–18, biweekly group sessions and an individual session every 2 months [21, 22]. A more detailed discussion of the dietary intervention can be found elsewhere [5, 23]. A loss of >20% body weight after 6 months or >30% after 12 months triggered a weight-related safety alert.
Exercise Intervention
The exercise intervention was conducted for 1 hour 3 d·wk−1 for 18 months and was supervised by trained interventionists, most who held American College of Sports Medicine certification. The program consisted of aerobic walking (15 min), strength training (20 min), a second aerobic phase (15 min), and cool-down (10 min).
Measurements and Procedures
All participants were tested at baseline, 6-month follow-up (FU6), and FU18. An initial symptom-limited, maximum exercise stress test excluded anyone with severe manifestations of coronary heart disease. The Modified Mini-Mental State Exam (3MSE) screened for cognitive deficiencies [24]. Knee osteoarthritis is an active disease process with joint destruction driven by both biomechanical and pro-inflammatory factors [25]. We used bone-on-bone knee joint compressive forces and IL-6 as the primary biomechanical and inflammatory outcomes.
Knee Joint Load
Bone-on-bone peak tibiofemoral (knee) compressive force (N) was the primary measure of knee joint loading. Detailed description of instruments and calculation of knee joint compressive force can be found elsewhere [26].
Plasma IL-6
Blood samples were collected in the early morning after a 10-hour fast at baseline, FU6, and FU18. The 6- and 18-month samples were collected at least 24 hours after the last acute bout of exercise training (D+E group) and sampling was postponed (1–2 weeks after recovery from symptoms) in the event of an acute respiratory, urinary tract, or other infection. All blood was collected, processed, divided into aliquots, and stored at −80°C until analysis.
The inflammation measure was plasma IL-6 pg·ml−1. All samples were measured in duplicate using enzyme-linked immunosorbent assays (Quantikine® ELISA kits R&D Systems, Minneapolis, MN) with the average used for data analyses.
Pain
The Western Ontario McMasters Universities Osteoarthritis Index (WOMAC) pain subscale was used to measure self-reported pain [27, 28]. Participants indicate on a scale from 0 (none) to 4 (extreme) the degree of pain experienced performing daily living activities in the last 48 hours due to knee OA. Total scores for the 5 items range from 0–20; higher scores indicate greater pain.
Function
Individual scores on the 17 items of the WOMAC self-reported function subscale were added to generate a summary score ranging from 0 to 68; higher scores indicate poorer function.
Mobility
6-minute walk distance (m) was our measure of mobility.
Weight, height, BMI
Weight, height, and BMI were obtained using standard techniques.
Health-related quality of life (HRQL)
SF-36 was used to measure HRQL using two broad summary scores: physical and mental health, scaled from 0 (worst) to 100 (best) [29].
Body composition and bone mineral density (BMD)
Whole body lean mass (kg) and fat mass (kg) and BMD (g·cm−2) were measured at baseline and FU18 by dual x-ray absorptiometry using a fan-beam scanner (Delphi A™, Hologic, Waltham, MA) and the manufacturer’s recommendations for patient positioning, scanning, and analysis.
X-ray
We used bilateral, posterioranterior, weight-bearing knee x-rays to identify tibiofemoral OA and sunrise views to identify patellofemoral OA. To visualize the tibiofemoral joint, we used a positioning device to flex knees 15 degrees, with the beam centered on the joint space. Kellgren-Lawrence (K-L) grade (0–4) was used to quantify severity of tibiofemoral OA [18].
Physical activity scale for the elderly (PASE)
This scale was used to assess self-reported daily physical activity during a seven day period prior to baseline and follow-up testing [30, 31].
Statistical Analysis
Baseline characteristics of the participants overall and by weight loss categories were summarized using means and standard deviations for continuous variables and frequencies and percentages for categorical variables. Tests for heterogeneity of weight loss group characteristics at baseline were performed using one way ANOVA for continuous variables and Chi-square tests for categorical variables. Outcomes were modeled using a mixed linear model using 6 and 18 month follow-up data, with main effects of weight loss category, visit code, and weight loss category by visit interaction, adjusted for baseline BMI, gender, treatment assignment (D or D+E), and baseline values of the outcome. Substitution of baseline body weight for baseline BMI as a covariate did not alter the outcomes (data not shown).Tests of the outcomes at 18 months were performed using contrast statements, and p<0.05 was considered significant for the main weight loss category effect. Significant pairwise comparisons were noted at a conservative Bonferroni-adjusted significance level of 0.0125. All analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC).
RESULTS
Table 1 shows the baseline characteristics of the weight loss groups. There were no significant baseline differences in age, BMI, or weight between the groups. The majority of participants were female and white.
Table 1.
Characteristics of participants at baseline.
| Baseline Characteristic |
All (n=240) |
<5% (n= 74) |
≥5% (n=59) |
≥10% (n=76) |
≥20% (n= 31) |
P |
|---|---|---|---|---|---|---|
|
| ||||||
| Age (yrs) | 65.8 | 65.4 | 66.1 | 66.0 | 65.9 | 0.91 |
| 6.0 | 6.4 | 5.4 | 6.2 | 6.1 | ||
|
| ||||||
| BMI (kg·m−2) | 33.4 | 33.1 | 33.8 | 33.1 | 34.3 | 0.39 |
| 3.8 | 4.0 | 3.5 | 3.9 | 3.4 | ||
|
| ||||||
| Weight (kg) | 92.4 | 90.7 | 94.0 | 91.8 | 94.6 | 0.47 |
| 14.7 | 13.6 | 12.6 | 15.9 | 17.5 | ||
|
| ||||||
| Female, No. % | 173 | 55 | 42 | 55 | 21 | 0.92 |
| 72.1 | 74.3 | 72.1 | 74.3 | 72.1 | ||
|
| ||||||
| White, No. % | 204 | 54 | 51 | 70 | 29 | 0.004 |
| 85.0 | 73.0 | 86.4 | 92.1 | 93.5 | ||
Weight Loss and Body Composition
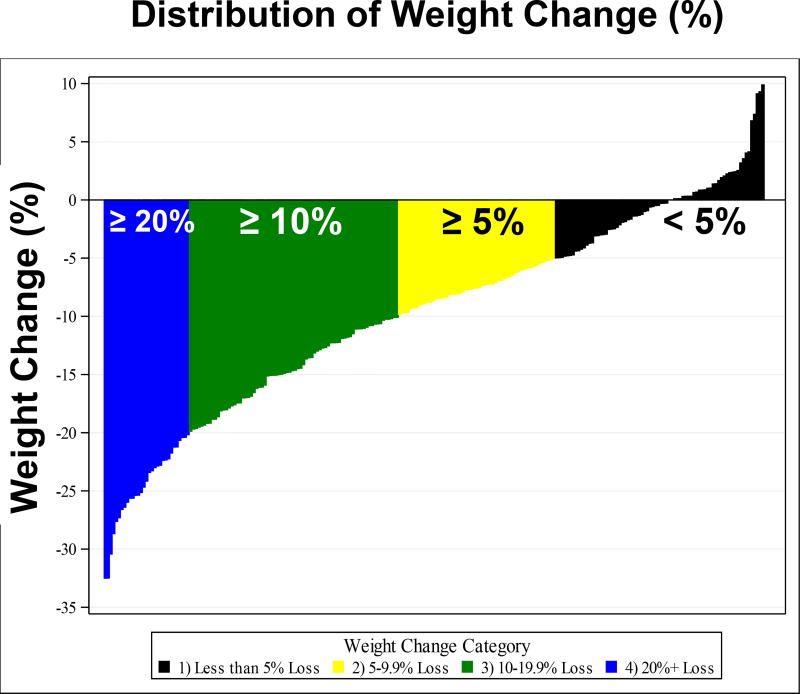
The mean percent weight change from lowest to highest weight loss group was 0.2% (n = 74), 7.4% (n = 59), 14.5% (n = 76), and 24.6% (n = 31), respectively. Total body fat increased in the <5% group by 0.44 kg and decreased by 3.29 kg, 7.97 kg, and 14.44 kg for the ≥5%, ≥10%, and ≥20% weight loss groups, respectively. These changes in body composition resulted in alterations in BMI of +0.1, −2.4, −4.7 and −8.1 kg·m−2. Figure 1 shows the distribution of weight loss across all categories and participants.
Figure 1.
The distribution of weight change by weight loss group.
Weight, BMI, and total hip and femoral neck bone mineral density at 18-month follow-up adjusted for visit, gender, treatment arm, and baseline values, and lean and fat mass adjusted for gender, treatment arm, and baseline values, all exhibited significant dose responses (Table 2).
Table 2.
Mean (95% CI) dose response to weight loss for body composition at 18-month follow-up.
| Variable | <5% (n= 74) |
≥5% (n=59) |
≥10% (n=76) |
≥20% (n= 31) |
P |
|---|---|---|---|---|---|
|
| |||||
| †Weight Loss, kg(%) | 0.15 | 6.95 | 13.37 | 23.23 | <0.0001 |
| (0.2) | (7.4) | (14.5) | (24.6) | ||
|
| |||||
| †Weight (kg) | 93.5 | 88.5 | 83.9 | 78.3 | <0.0001 |
| 91.8,95.3 | 86.8,90.1 | 82.2,85.6 | 76.3,80.3 | ||
|
| |||||
| †BMI (kg/m2) | 32.7 | 30.9 | 29.2 | 27.3 | <0.0001 |
| 32.2,33.3 | 30.4,31.4 | 28.6,29.7 | 26.6,27.9 | ||
|
| |||||
| ‡Total Body Fat (kg) | 36.2 | 32.8 | 27.8 | 21.9 | <0.0001 |
| 35.3,37.1 | 31.9,33.8 | 27.0,28.6 | 20.7,23.0 | ||
|
| |||||
| ‡Total Body Lean (kg) | 53.3 | 52.1 | 50.2 | 48.1 | <0.0001 |
| 52.7,54.0 | 51.4,52.7 | 49.6,50.8 | 47.3,48.9 | ||
|
| |||||
| #Total Hip BMD (g·cm−2) | 0.97 | 0.95 | 0.95 | 0.92 | <0.0001 |
| 0.96,0.98 | 0.95,0.96 | 0.94,0.95 | 0.91,0.93 | ||
|
| |||||
| #Femoral Neck BMD (g·cm−2) | 0.79 | 0.79 | 0.78 | 0.78 | 0.013 |
| 0.79,0.80 | 0.78,0.80 | 0.78,0.79 | 0.77,0.79 | ||
Adjusted for visit, gender, treatment group.
Adjusted for gender, treatment group, and baseline values.
Adjusted for visit, gender, treatment group, baseline BMI, baseline values.
Dose Response to Weight Loss
Clinical Outcomes
There was a significant (p = 0.012) dose response in WOMAC pain levels; pairwise comparisons at FU18 revealed the ≥20% group had significantly less pain than the <5% (p = 0.0046) and ≥5% (p = 0.0027) groups. There was a similar significant dose response (p = 0.0006) to weight loss in WOMAC function; the ≥20% group had better function compared to the <5% (p = 0.0002) and ≥5% groups (p = 0.0006). The ≥10% group also had better function than the <5% group (p = 0.0123); there was no significant difference in pain or function between the ≥10% and ≥20% groups (Tables 3, 4).
Table 3.
Mean (95% CI) dose response to weight loss for outcome measures at 18-month follow-up. Adjusted for visit, gender, treatment group, baseline BMI, change in PASE scale, and baseline value of outcome.
| Variable | <5% (n= 74) |
≥5% (n=59) |
≥10% (n=76) |
≥20% (n= 31) |
P |
|---|---|---|---|---|---|
|
| |||||
| IL-6 (pg/mL) | 2.84 | 2.52 | 2.65 | 2.27 | 0.017* |
| 2.41,3.26 | 2.10,2.94 | 2.26,3.04 | 1.70,2.83 | ||
|
| |||||
| Knee Compressive Force (N) | 2750 | 2611 | 2444 | 2200 | <0.0001 |
| 2619,2880 | 2473,2749 | 2321,2567 | 2019,2381 | ||
|
| |||||
| WOMAC Pain (0–20) | 4.46 | 4.60 | 3.71 | 2.79 | 0.006 |
| 3.81,5.11 | 3.92,5.28 | 3.09,4.34 | 1.87,3.71 | ||
|
| |||||
| WOMAC Function (0–68) | 17.13 | 16.73 | 13.57 | 10.84 | 0.0005 |
| 15.15,19.11 | 14.70,18.76 | 11.67,15.47 | 8.07,13.61 | ||
|
| |||||
| 6 Minute Walk Distance (m) | 508 | 522 | 542 | 559 | <0.0001 |
| 496,520 | 510,534 | 530,553 | 543,576 | ||
|
| |||||
| SF-36 Physical (0–100) | 42.5 | 43.2 | 44.3 | 48.1 | 0.001 |
| 40.8,44.2 | 41.5,45.0 | 42.8,45.9 | 45.8,50.4 | ||
|
| |||||
| SF36 Mental (0–100) | 55.4 | 54.6 | 57.5 | 58.1 | 0.02 |
| 53.7,57.0 | 52.9,56.3 | 56.0,59.1 | 55.8,60.4 | ||
|
| |||||
| **PASE | 140 | 165 | 134 | 129 | 0.083 |
| 120,160 | 143,188 | 115,152 | 104,154 | ||
Significance based on log transformed data (not shown)
Not adjusted for change in PASE
Table 4.
Mean (95% CI) pairwise between group comparisons at 18-month follow-up. Adjusted for visit, gender, treatment group, baseline BMI, change in PASE scale, baseline values of outcome.
| Variable | <5% vs ≥20% | ≥5% vs ≥20% | ≥10% vs ≥20% | <5%vs≥10% | ≥5% vs ≥10% | <5%vs≥5% |
|---|---|---|---|---|---|---|
|
| ||||||
| IL-6 (pg/mL) | 0.57*† | 0.25# | 0.38 | 0.18 | −0.13 | 0.32 |
| −0.13,1.27 | −0.44,0.95 | −0.28,1.05 | −0.37,0.74 | −0.68,0.42 | −0.26,0.90 | |
|
| ||||||
| Knee Compressive Force (N) | 550† | 411† | 244# | 306† | 168 | 139 |
| 332,768 | 191,632 | 35,453 | 135,478 | −7,343 | −40,317 | |
|
| ||||||
| WOMAC Pain | 1.68† | 1.81† | 0.93 | 0.75 | 0.89# | −0.14 |
| 0.57,2.78 | 0.69,2.93 | −0.14,1.99 | −0.12,1.62 | 0.01,1.77 | −1.03,0.76 | |
|
| ||||||
| WOMAC Function | 6.29† | 5.89† | 2.73 | 3.56† | 3.16# | 0.40 |
| 2.96,9.62 | 2.58,9.20 | −0.39,5.85 | 0.98,6.13 | 0.63,5.69 | −2.19,2.99 | |
|
| ||||||
| 6 Minute Walk Distance (m) | −51† | −37† | −17 | −34† | −20† | −14 |
| −71,−31 | −57,−17 | −36,1 | −49,−18 | −35,−4 | −30,1 | |
|
| ||||||
| SF-36 Physical | −5.59† | −4.85† | −3.75† | −1.84 | −1.10 | −0.74 |
| −8.40,−2.78 | −7.66,−2.04 | −6.40,−1.10 | −4.02,0.33 | −3.26,1.06 | −2.96,1.48 | |
|
| ||||||
| SF36 Mental | −2.68 | −3.48# | −0.54 | −2.15 | −2.94† | 0.79 |
| −5.46,0.10 | −6.28,−0.67 | −3.22,2.14 | −4.33,0.03 | −5.13,−0.74 | −1.46,3.04 | |
Significance based on log transformed data (not shown)
p≤0.0125;
p≤0.05
Six-minute walk distance (p < 0.0001) was significantly impacted by the amount of weight loss (Table 3). Both the ≥20% and ≥10% groups walked significantly farther than the two lowest weight loss groups (≥20% vs. <5%, p < 0.00001; ≥20% vs. ≥5%, p = 0.0001; ≥10% vs. <5%, p = 0.0001; ≥10% vs. ≥5%, p = 0.0046) (Table 4).
Both the physical (p = 0.0004) and mental (p = 0.03) subscales of the SF-36 were affected by the amount of weight loss (Table 3). The ≥20% group significantly improved physical HRQL compared to the three lower weight loss categories (≥20% vs. <5%, p < 0.0001; ≥20% vs. ≥5%, p = 0.0008; ≥20% vs. ≥10%, p = 0.003). Improvement in mental HRQL was similar between the weight loss groups (Table 4). There was no significant does response in the PASE activity scale (p = 0.083).
Mechanistic Outcomes
IL-6, our primary inflammatory outcome, was significantly different among the weight loss groups (p = 0.002) (Table 3). The two highest weight loss groups had decreased IL-6 levels compared to the lowest weight loss group (≥20% vs. <5%, p = 0.0003; ≥10% vs. <5%, p = 0.0095).
Bone-on-bone knee joint compressive forces showed a distinct weight loss dose response (p < 0.0001). Compressive forces in the ≥20% group were attenuated by 252 N (57 lbs.), 400 N (90 lbs.), and 533 N (120 lbs.) compared to the ≥10% (p = 0.0165), ≥5% (p = 0.0004), and the <5% (p <0.0001) groups, respectively. The ≥10% group also demonstrated lower compressive forces than the <5% group (p = 0.0007) (Table 4).
DISCUSSION
Moderate (5%) to intensive (10%) weight loss in older, overweight and obese adults with knee OA has positive effects on clinical and mechanistic outcomes, with a clear dose-response effect [5, 6, 9, 10]. Our participants who reached their weight loss goal of 10% and expressed a desire to continue to lose weight were monitored by the study team to ensure additional weight loss was achieved safely. Consequently, 13% of the participants in the weight loss groups safely lost more than 20% of their baseline body weight. Two participants triggered weight-related safety alerts by losing greater than 20% of their baseline weight in 6 months or greater than 30% in 12 months. In these two cases the study physician contacted the participants and questioned them on clinical symptoms that would indicate safety or health issues. Additionally, intervention staff continued to monitor weight loss, physical activity, and dietary behaviors to look for indications of disordered eating and excessive levels of exercise.
Significant pairwise differences between the adjacent ≥10% and ≥20% groups was limited to improvement in physical health related quality of life, due in part to the small sample size in the more extreme weight loss group (i.e., possible Type II error). However, the strong trend for pain (p = 0.012) and function (p = 0.0006) (see Table 2) across weight loss groups combined with a clinically important 25% mean reduction in pain and improvement in function when moving from 10% to 20% weight loss argues that there may be additional clinical value with the greater weight loss. Hence, while our results and clinical trial data (4, 5) support the NIH recommendation of an initial weight loss of 10% for overweight and obese adults with knee OA (6, 24), the added benefit of substantially greater weight loss, achieved safely and without pharmacologic or surgical intervention, is an intriguing possibility that warrants further study.
Pairwise comparisons between the <5% and ≥5% groups revealed little statistical difference. This is surprising considering the D+E group in our ADAPT trial, with a 5.7% reduction in body weight, was statistically and clinically better in function, mobility, and pain after an 18-month intervention than a healthy lifestyle control group that lost 1.2% of their weight [9]. This suggests that participating in long-term diet or diet plus exercise interventions provides some clinical benefit regardless of weight loss success. Interestingly, mortality risk eight years post-intervention in ADAPT participants randomized to the D and D+E groups, irrespective of the amount of weight loss achieved, was statistically lower than in participants randomized to non-weight loss groups [32].
Significant weight loss in older adults could exacerbate bone loss and increase the risk of hip fracture [33]; however, obesity increases the loads on lower extremity bones and therefore is somewhat protective for this population. Nevertheless, we documented total hip and femoral neck BMD at baseline and 18-month follow-up. Data from NHANES III defined osteopenia for men and women as between 0.56 to 0.74 g·cm−2 for the femoral neck, and between 0.64 to 0.82 g·cm−2 for total hip BMD [34]. There was a significant dose response to weight loss in BMD; however, mean values at FU18 remained above osteopenic threshold levels for all weight loss categories. We suggest that the significant reduction in pain, inflammation, and knee joint loads combined with significant improvements in function, mobility, and HRQL outweighs the slight reduction in BMD that accompanies a weight loss of ≥10% or ≥20% of baseline body weight.
Brownell [16] summarized effectively the biological factors that work against achieving and maintaining significant weight loss: the body acts in starvation mode, increases feelings of hunger, suppresses satiety, slows metabolic rate, and attempts at all costs to defend higher body weights. However, it is possible to achieve and maintain significant weight loss [13]. Previous work indicates that habits that distinguish successful from unsuccessful weight loss include maintaining a low calorie, low-fat diet, high levels of physical activity, frequent weighing, and routinely eating breakfast [13]. Enhanced self-efficacy and the ability to tolerate feelings of hunger are psychological characteristics that also appear to help achieve and maintain weight loss [35]. Whether particular psychological characteristics differentiated the 13% of the diet groups that were able to achieve greater than 20% weight loss, and whether these characteristics improve the ability to resist weight regain is unknown. Finally, our study was limited by its observational design and small sample size in the ≥20% group. Group assignment was not random, rather it was based on weight loss achieved in a previous randomized clinical trial in which the goal was to lose at least 10% of baseline weight.
In summary, relatively large differences in intentional, non-pharmacologic, non-surgical weight loss produce large and beneficial differences in health outcomes. Both ≥10% and ≥20% weight loss have substantial clinical and mechanistic benefits compared to less weight loss. We suggest that standard of care for older, overweight and obese adults with knee OA should include, at minimum, a 10% weight loss using the techniques developed in previous successful weight loss trials such as IDEA and Osteoarthritis Healthy Weight for Life. An additional 10% weight loss has the added benefit of significantly improved physical health related quality of life, and a clinically important reduction in pain and improvement in function.
SIGNIFICANCE AND INNOVATIONS.
Relatively large differences in intentional, non-pharmacologic, non-surgical weight loss produce large and beneficial differences in clinical and mechanistic outcomes.
The significant dose response to weight loss in pain, inflammation, knee joint loads, function, mobility, and health related quality of life outweighs the slight reduction in bone mineral density that accompanies a weight loss of ≥10% or ≥20% of baseline body weight.
Standard of care for older, overweight and obese adults with knee OA should include, at minimum, a 10% weight loss.
Losing 20% compared to 10% of baseline body weight for overweight and obese adults with knee OA has the added benefit of a significantly improved physical health-related quality of life, and a 25% reduction in pain and improvement in function.
Acknowledgments
We would like to thank the IDEA research staff and the IDEA participants for their important contributions.
Role of the Sponsor: The sponsors had no role in the design and conduct of the study; in the collection, analysis, and interpretation of data; in the preparation of the manuscript; or in the review or approval of the manuscript.
Funding/Support: Support for this study was provided by grants from the National Institutes of Health: R01 AR052528-01 from NIAMS, P30 AG21332 from NIA, M01-RR00211 from NCRR, and General Nutrition Centers, Inc.
FE is CEO of Chondrometrics GmbH; he has provided consulting services to EMD Serono, Bioclinica/Synarc, Samumed, Abbvie and Servier, has prepared educational sessions for Medtronic, and has received research support from Pfizer, Eli Lilly, Merck Serono, Novartis, Stryker, Abbvie, Kolon, Synarc, Ampio, BICL, Orthotrophix and Tissuegene.
AG is President of BICL, LLC. He is consultant to Pfizer, GE, OrthoTrophix, TissueGene, Sanofi, MerckSerono and AstraZeneca.
DJH is a consultant for Flexion, Tissuegene and Merck Serono.
Footnotes
Trial Registration: NCT00381290
Competing Interests
All other authors declare that they have no competing interests.
Authors’ Contributions
SPM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. He also conceived the study, participated in its design and coordination, carried out the gait analysis, and drafted the manuscript. AR help draft the manuscript and presented these data as part of her undergraduate honor’s thesis. DPB was responsible for the statistical analyses and helped draft the manuscript. SLM participated in study design, and coordinated patient compliance and adherence protocols. GDM participated in study design, and designed the nutrition intervention. BJN participated in study design and coordination and was responsible for IL-6 measurements. PD participated in study design, and helped coordinate the gait analysis and the measurement of knee compressive forces. ML carried out the participant evaluation of GXT results, and made decisions regarding inclusion/exclusion based on medical tests and medical history. DJH participated in study design and coordination. FE participated in study design and coordination. RFL participated in study design, addressed participant’s issues related to exercise adherence due to joint symptoms, coordinated x-ray readings, and assisted in the analysis of IL-6. All authors read and made comments on previous drafts of the manuscript, and approved the final manuscript.
References
- 1.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States--no statistically significant change since 2003–2004. NCHS data brief. 2007;(1):1–8. [PubMed] [Google Scholar]
- 2.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States, 2005–2008. NCHS data brief. 2010;(50):1–8. [PubMed] [Google Scholar]
- 3.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18(1):24–33. doi: 10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 4.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, Devita P, Beavers DP, Hunter DJ, Lyles MF, Eckstein F, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–1273. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atukorala I, Makovey J, Lawler L, Messier SP, Bennell K, Hunter DJ. Is There a Dose-Response Relationship Between Weight Loss and Symptom Improvement in Persons With Knee Osteoarthritis? Arthritis care & research. 2016;68(8):1106–1114. doi: 10.1002/acr.22805. [DOI] [PubMed] [Google Scholar]
- 7.Health NIo, Institute NHLaB. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. 1998 [PubMed] [Google Scholar]
- 8.Gersing AS, Solka M, Joseph GB, Schwaiger BJ, Heilmeier U, Feuerriegel G, Nevitt MC, McCulloch CE, Link TM. Progression of cartilage degeneration and clinical symptoms in obese and overweight individuals is dependent on the amount of weight loss: 48-month data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2016;24(7):1126–1134. doi: 10.1016/j.joca.2016.01.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, Ettinger WH, Jr, Pahor M, Williamson JD. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50(5):1501–1510. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 10.Aaboe J, Bliddal H, Messier SP, Alkjaer T, Henriksen M. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthritis Cartilage. 2011;19(7):822–828. doi: 10.1016/j.joca.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 11.Rejeski WJ, Mihalko SL, Ambrosius WT, Bearon LB, McClelland JW. Weight Loss and Self-Regulatory Eating Efficacy in Older Adults: The Cooperative Lifestyle Intervention Program. J Gerontol B Psychol Sci Soc Sci. 2011 doi: 10.1093/geronb/gbq104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Runhaar J, van Middelkoop M, Reijman M, Willemsen S, Oei EH, Vroegindeweij D, van Osch G, Koes B, Bierma-Zeinstra SM. Prevention of Knee Osteoarthritis in Overweight Females: The First Preventive Randomized Controlled Trial in Osteoarthritis. The American journal of medicine. 2015 doi: 10.1016/j.amjmed.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 14.Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care. 1998;21(3):350–359. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- 15.Wing RR. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med. 2010;170(17):1566–1575. doi: 10.1001/archinternmed.2010.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brownell KD. The humbling experience of treating obesity: Should we persist or desist? Behav Res Ther. 2010;48(8):717–719. doi: 10.1016/j.brat.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 17.Messier SP, Legault C, Mihalko S, Miller GD, Loeser RF, Devita P, Lyles M, Eckstein F, Hunter DJ, Williamson JD, et al. The Intensive Diet and Exercise for Arthritis (IDEA) trial: design and rationale. BMC Musculoskelet Disord. 2009;10:93. doi: 10.1186/1471-2474-10-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Academies IoMotN. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients) National Academy Press. 2002 doi: 10.1016/s0002-8223(02)90346-9. [DOI] [PubMed] [Google Scholar]
- 20.Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA. 2003;289(14):1799–1804. doi: 10.1001/jama.289.14.1799. [DOI] [PubMed] [Google Scholar]
- 21.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-Efficacy: The Exercise of Control. New York: W H Freeman and Co; 1997. [Google Scholar]
- 23.Miller GD, Beavers DP, Hamm D, Mihalko SL, Messier SP. Nutrient Intake During Diet-Induced Weight Loss and Exercise Interventions in a Randomized Trial in Older Overweight and Obese Adults. The journal of nutrition, health & aging. 2017;21(10):1216–1224. doi: 10.1007/s12603-017-0892-5. [DOI] [PubMed] [Google Scholar]
- 24.Folstein MF, Folstein SE, McHugh PR. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 25.Griffin TM, Guilak F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc Sport Sci Rev. 2005;33(4):195–200. doi: 10.1097/00003677-200510000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Messier SP, Legault C, Loeser RF, VanArsdale SJ, Davis C, Ettinger WH, Devita P. Does high weight loss in older adults with knee osteoarthritis affect bone-on-bone joint loads and muscle forces during walking? Osteoarthritis and Cartilage. 2011;19:272–280. doi: 10.1016/j.joca.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt L. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes following total hip or knee arthroplasty in osteoarthritis. Journal of Orthopaedic Rheumatology. 1988;1:95–108. [PubMed] [Google Scholar]
- 28.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 29.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 30.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 31.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 32.Shea MK, Houston DK, Nicklas BJ, Messier SP, Davis CC, Miller ME, Harris TB, Kitzman DW, Kennedy K, Kritchevsky SB. The effect of randomization to weight loss on total mortality in older overweight and obese adults: the ADAPT Study. J Gerontol A Biol Sci Med Sci. 2010;65(5):519–525. doi: 10.1093/gerona/glp217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Langlois JA, Mussolino ME, Visser M, Looker AC, Harris T, Madans J. Weight loss from maximum body weight among middle-aged and older white women and the risk of hip fracture: the NHANES I epidemiologic follow-up study. Osteoporos Int. 2001;12(9):763–768. doi: 10.1007/s001980170053. [DOI] [PubMed] [Google Scholar]
- 34.Looker AC, Melton LJ, 3rd, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005–2006 compared with NHANES III. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2010;25(1):64–71. doi: 10.1359/jbmr.090706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Buren DJ, Sinton MM. Psychological aspects of weight loss and weight maintenance. Journal of the American Dietetic Association. 2009;109(12):1994–1996. doi: 10.1016/j.jada.2009.09.010. [DOI] [PubMed] [Google Scholar]