Abstract
Objective:
To identify factors associated with prolonged maternal breast milk (BM) provision in very low birth weight (VLBW) infants.
Study design:
This was a cohort study of VLBW infants who initially received maternal BM and were born at one of 197 neonatal intensive care units managed by the Pediatrix Medical Group from 2010 to 2012. We used multivariable logistic regression to identify demographic, clinical, and maternal factors associated with provision of maternal BM on day of life (DOL) 30 and at discharge.
Results:
Median gestational age (GA) for all infants was 28 weeks (25th, 75th percentiles: 26, 30), and median maternal age was 28 years (23, 33). Of 8806 infants, 6261 (71%) received maternal BM on DOL 30, and 4003/8097 (49%) received maternal BM at discharge to home. Predictors of maternal BM provision at DOL 30 included increased maternal age, white maternal race, absence of history of necrotizing enterocolitis or late-onset sepsis, higher household income, lower education level, lack of donor breast milk exposure, and lower GA.
Conclusions:
Our results suggest that maternal-infant demographic and clinical factors and household neighborhood socioeconomic characteristics were associated with provision of maternal BM at 30 postnatal days to VLBW infants. Identification of these factors allows providers to anticipate mothers’ needs and develop tailored interventions designed to improve rates of prolonged maternal BM provision and infant outcomes.
Keywords: human milk, VLBW, duration, neonatal, mother’s own milk
Very low birth weight (VLBW, <1500 g birth weight) infants often do not receive maternal breast milk (BM) despite its known benefits over infant formula or pasteurized donor human milk.1–3 These benefits include lowered risks of sepsis, necrotizing enterocolitis (NEC), retinopathy of prematurity, and bronchopulmonary dysplasia, as well as improved neurodevelopmental outcomes.4–15 This information, along with improvements in neonatal intensive care unit (NICU)-specific interventions, have resulted in increased rates of lactation initiation, and most mothers of VLBW infants make the decision to provide maternal BM soon after delivering a VLBW infant.16–19 Despite this, VLBW infants are less likely than their normal birth weight counterparts to receive maternal BM at hospital discharge.1,2 Although the amount of maternal BM received during critical exposure periods in the NICU hospitalization has been linked to the reduction in the abovementioned morbidities, little is known about provision of maternal BM in the NICU aside from initiation and discharge rates.20 Of particular interest is the first 30 days post-birth, as VLBW infants transition from intrauterine to extrauterine nutrition and are at the greatest risk for morbidities that are potentially preventable with high-dose maternal BM feedings. Furthermore, there is evidence of a 3-fold increase in the number of mothers choosing not to provide maternal BM after 30 days of age compared with earlier in the NICU hospitalization.21
Previous work has identified associations between provision of maternal BM in the NICU and infant characteristics (eg, gestational age [GA] or birth weight), maternal characteristics (e.g., maternal age or maternal race), and environmental factors (e.g., site of care, social support, or access to breastfeeding education).22–26 However, many of these studies failed to distinguish between VLBW and term infants and vary with respect to the duration of maternal BM provision during the hospitalization, such as initiation or maintenance to hospital discharge.27,28
Leveraging a large, multi-center, electronic health record-derived database, the purpose of this study was to identify factors that predicted prolonged provision of maternal BM among VLBW infants initially exposed to maternal BM. For this report, we examined which of these factors predicted continued provision of maternal BM through 30 days of age and to discharge.
Methods
We conducted a prospective cohort study of electronic health records from 197 NICUs managed by the Pediatrix Medical Group in the United States from January 1, 2010 – December 31, 2012. The Pediatrix Medical Group Clinical Data Warehouse includes data on multiple aspects of care obtained from admission notes, daily progress notes, and discharge summaries and includes maternal history, demographic data, medications, laboratory results, diagnoses, and procedures.29 Infants were eligible for inclusion based on the following criteria: birth weight <1500 g; receipt of maternal BM at any time prior to 30 days of life (DOL); NICU discharge between 2010 and 2012, with availability of maternal address linking to census block group-specific geospatial data; inborn; and alive on DOL 30. Infants who were discharged or transferred prior to DOL 30 and those missing data on BM provision on DOL 30 were excluded. Variables considered as potentially associated with prolonged provision of maternal BM included donor BM intake, GA, sex, 5-minute Apgar score, NEC diagnosis prior to DOL 30, late-onset sepsis from DOL 4–29, cesarean delivery, maternal race, maternal age, and utilization of prenatal care. Additionally, we used each mother’s home address to identify her corresponding U.S. census block, which was then linked to block group-specific geospatial data, including annual income, educational attainment, presence of single-female households, and straight-line distance to the nearest NICU. This study was approved by the Duke University Institutional Review Board with a waiver of written informed consent.
Definitions
Provision of maternal BM at DOL 30 was defined as receipt of maternal BM by any enteral route on DOL 30. Infants receiving nothing by mouth on DOL 30 were included if they received maternal BM on the first day of resumed enteral feeding after DOL 30. Provision of maternal BM at discharge was defined as receipt of maternal BM by any enteral route on the day of or the day before discharge home. We defined donor BM provision as receipt of breast milk originating from a human milk bank at any point prior to DOL 30. NEC diagnoses were obtained from the medical record, defined according to the attending neonatologist, and included medical or surgical NEC. Late-onset sepsis was defined as a positive bacterial culture for blood or cerebrospinal fluid from DOL 4–29, including probable and definite episodes due to coagulase-negative Staphylococcus but excluding other organisms likely to be contaminants.30
Statistical Analyses
Descriptive statistics (medians, 25th and 75th percentiles, counts, and percentages) were used to summarize data. We performed unadjusted analyses between groups, using the Wilcoxon rank-sum test for continuous variables and the chi-square test for categorical variables where appropriate. The primary outcome was provision of maternal BM at DOL 30. We used multivariable logistic regression to evaluate the association of all demographic, clinical, and maternal variables with provision of maternal BM at DOL 30. We also examined provision of maternal BM by site among those that discharged at least 20 infants during the study period. We divided sites into quartiles according to the percentage of infants who received maternal BM at DOL 30 and reported site characteristics by quartile, including volume of infants, GA, and percentage of infants receiving donor BM. As a secondary analysis among infants who were discharged home, we used multivariable logistic regression to evaluate the association of the same covariates with provision of maternal BM at discharge. P values <.05 were considered statistically significant. Analyses were conducted using Stata 15.1 software (StataCorp LLC, College Station, TX).
Results
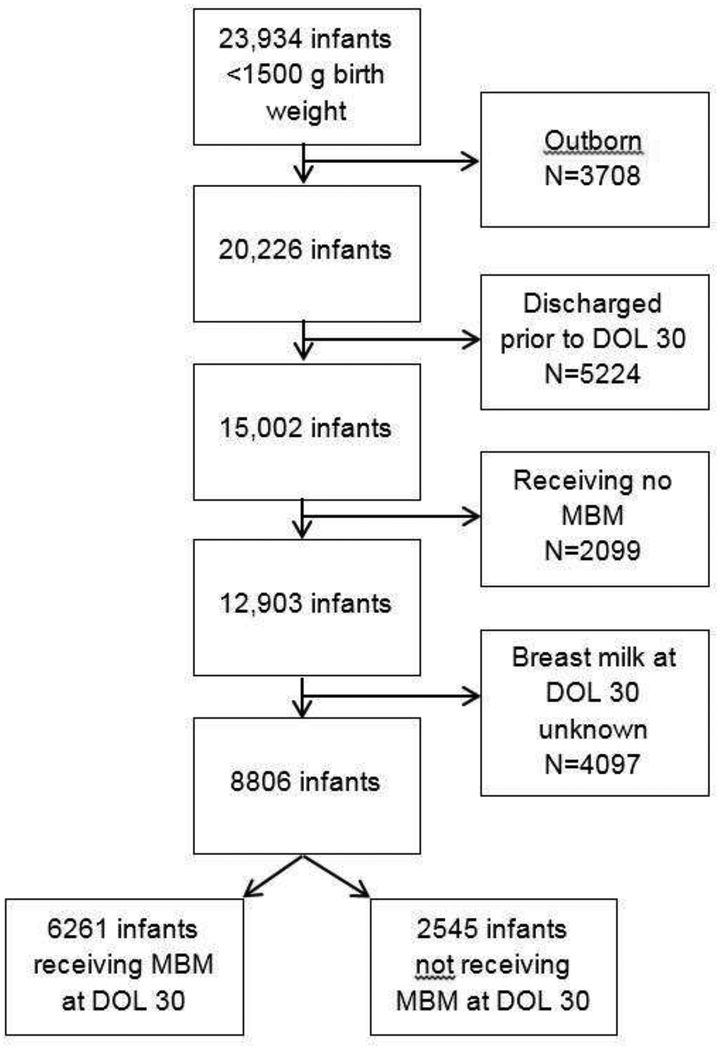
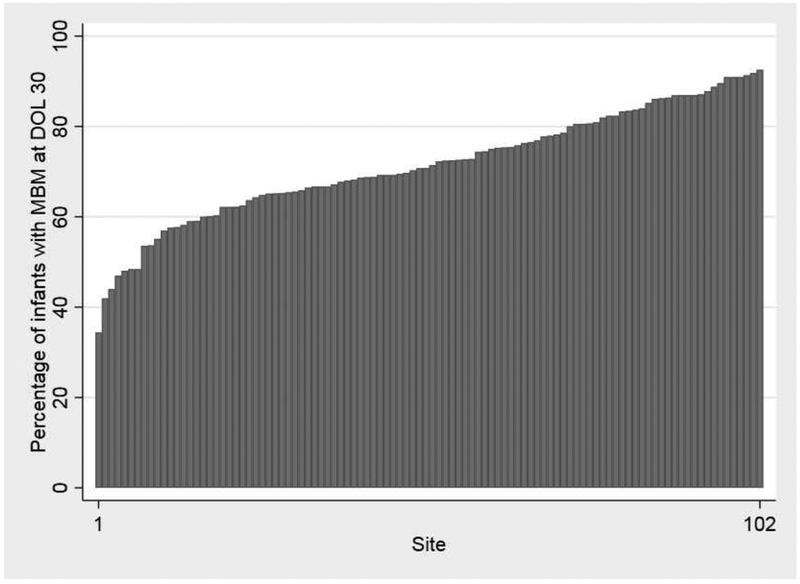
A total of 8806 infants were included in the analysis (Figure 1). The median GA was 28 (25th, 75th percentiles: 26, 30) weeks, and the median birth weight was 1070 (840, 1280) g. The median maternal age was 28 (23, 33) years. A total of 6261 (71%) infants received maternal BM on DOL 30 (Table 1). Among the 102 sites discharging ≥20 infants during the study period, the median percentage of infants receiving maternal BM at DOL 30 was 71% (65%, 81%). We observed significant variability across sites in the proportion of infants receiving maternal BM at DOL 30, with 7 (7%) sites reporting <50% of infants and 6 (6%) sites reporting ≥90% of infants receiving maternal BM at 30 days of age, respectively (Figure 2). There were few noticeable trends in unit volume, GA, and provision of donor BM according to the proportion of infants receiving maternal BM at DOL 30 at each site (Table 2). Of the 102 sites discharging ≥20 infants during the study period, 95/102 (93%) sites provided donor BM for at least 1 infant.
Figure 1.
Study flow diagram
DOL, day of life; maternal BM, maternal breast milk
Table 1.
Demographics and clinical characteristics by exposure to Maternal BM at DOL 30.
| Maternal BM at DOL 30 N=6261 (71%) |
No Maternal BM at DOL 30 N=2545 (29%) |
P-value | |
|---|---|---|---|
| Gestational age (weeks) | <0.001 | ||
| <26 | 1057 (17) | 362 (14) | |
| 26–28 | 2400 (38) | 929 (37) | |
| 29–32 | 2665 (43) | 1198 (47) | |
| >32 | 138 (2) | 56 (2) | |
| Male sex | 3169 (51) | 1269 (50) | 0.53 |
| 5-min. Apgar score | 0.40 | ||
| 0–3 | 238 (4) | 108 (4) | |
| 4–6 | 945 (15) | 403 (16) | |
| 7–10 | 4960 (81) | 1987 (80) | |
| Maternal race | <0.001 | ||
| White | 3036 (50) | 935 (38) | |
| Black | 1586 (26) | 1067 (43) | |
| Hispanic | 1011 (17) | 374 (15) | |
| Other | 393 (7) | 95 (4) | |
| Cesarean delivery | 4744 (77) | 1926 (76) | 0.60 |
| Maternal age (years) | <0.001 | ||
| ≤19 | 503 (8) | 358 (14) | |
| 20–29 | 2972 (48) | 1286 (51) | |
| 30–39 | 2509 (40) | 771 (30) | |
| ≥40 | 260 (4) | 118 (5) | |
| Prenatal care | 5939 (95) | 2414 (95) | 0.99 |
| Distance to NICU (miles) | <0.001 | ||
| <10 | 2599 (42) | 1192 (47) | |
| ≥10 and <20 | 1613 (26) | 544 (21) | |
| ≥20 | 2043 (33) | 799 (32) | |
| Less than high school education or GED* (%) | <0.001 | ||
| <10 | 2550 (41) | 706 (28) | |
| ≥10 and <30 | 2699 (43) | 1231 (48) | |
| ≥30 | 1011 (16) | 608 (24) | |
| Median household income* ($) | <0.001 | ||
| <30,000 | 967 (15) | 641 (25) | |
| 30,000–59,999 | 3247 (52) | 1352 (53) | |
| ≥60,000 | 2045 (33) | 548 (22) | |
| Single female household* (%) | <0.001 | ||
| <10 | 1487 (24) | 407 (16) | |
| ≥10 and <30 | 3156 (50) | 1169 (46) | |
| ≥30 | 1617 (26) | 967 (38) | |
| Necrotizing enterocolitis | 190 (3) | 127 (5) | <0.001 |
| Late-onset sepsis | 395 (6) | 187 (7) | 0.08 |
| Donor breast milk | 1611 (26) | 900 (35) | <0.001 |
Data presented as n (%).
Percentages or medians refer to individuals living in the maternal census tract. DOL, day of life; GED, general equivalency diploma; MBM, maternal breast milk; NICU, neonatal intensive care unit.
Figure 2.
Maternal breast milk provision at DOL 30 by site*
DOL, day of life; maternal BM, maternal breast milk
*Sites discharging <20 infants in the time period were excluded
Table 2.
Characteristics of sites by quartile of percentage of infants receiving maternal BM at DOL 30.
| Quartile 1 N=1894 |
Quartile 2 N=2263 |
Quartile 3 N=2473 |
Quartile 4 N=1515 |
|
|---|---|---|---|---|
| Infants receiving Maternal BM at DOL 30, n (%) | 1095 (58) | 1539 (68) | 1889 (76) | 1320 (87) |
| Infants admitted, median (25th, 75th percentile) | 57 (32, 96) | 59 (33, 134) | 85 (38, 108) | 46 (33, 69) |
| Gestational age (weeks), n (%) | ||||
| <26 | 306 (16) | 404 (18) | 416 (17) | 222 (15) |
| 26–28 | 747 (39) | 865 (38) | 943 (38) | 569 (38) |
| 29–32 | 807 (42) | 941 (42) | 1061 (43) | 691 (46) |
| >32 | 33 (2) | 53 (2) | 53 (2) | 33 (2) |
| Donor breast milk, n (%) | 537 (28) | 708 (31) | 698 (28) | 358 (24) |
On adjusted analysis, women 20–29 years of age (odds ratio [OR] 1.54, 95% confidence interval [CI] 1.31–1.82, p=0.001) and 30–39 years of age (OR 1.90, 95% CI 1.59–2.27, p<0.001) were more likely to provide maternal BM, compared with women <20 years of age (Table 3). Black race was associated with less provision of maternal BM on DOL 30 than white race (OR 0.58, 95% CI 0.51–0.66, p<0.001). Provision of maternal BM on DOL 30 did not differ between Hispanic and “other” race/ethnicity and white race.
Table 3.
Odds Ratios, 95% Confidence Intervals, and P-values for prolonged maternal BM provision.
| MBM on day of life 30 | MBM at discharge | |||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Gestational age (weeks) | ||||
| <26 | Reference | Reference | ||
| 26–28 | 0.79 (0.68–0.93) | 0.004 | 1.32 (1.12–1.55) | 0.001 |
| 29–32 | 0.60 (0.51–0.71) | <0.001 | 2.10 (1.78–2.48) | <0.001 |
| >32 | 0.61 (0.42–0.88) | 0.008 | 2.66 (1.82–3.88) | <0.001 |
| Male sex | 1.04 (0.94–1.15) | 0.50 | 1.10 (0.99–1.21) | 0.07 |
| 5-min. Apgar score | ||||
| 0–3 | Reference | Reference | ||
| 4–6 | 1.17 (0.89–1.55) | 0.27 | 1.37 (1.00–1.86) | 0.05 |
| 7–10 | 1.26 (0.97–1.63) | 0.08 | 1.77 (1.33–2.36) | <0.001 |
| Maternal race | ||||
| White | Reference | Reference | ||
| Black | 0.58 (0.51–0.66) | <0.001 | 0.52 (0.46–0.60) | <0.001 |
| Hispanic | 1.05 (0.89–1.24) | 0.57 | 0.99 (0.84–1.16) | 0.87 |
| Other | 1.24 (0.96–1.61) | 0.10 | 1.37 (1.08–1.73) | 0.01 |
| Cesarean delivery | 0.89 (0.79–1.01) | 0.07 | 0.83 (0.74–0.94) | 0.003 |
| Maternal age (years) | ||||
| <20 | Reference | Reference | ||
| 20–29 | 1.54 (1.31–1.82) | <0.001 | 2.40 (1.98–2.91) | <0.001 |
| 30–39 | 1.90 (1.59–2.27) | <0.001 | 3.91 (3.20–4.78) | <0.001 |
| ≥40 | 1.14 (0.85–1.52) | 0.38 | 2.72 (2.00–3.69) | <0.001 |
| Prenatal care | 0.97 (0.76–1.24) | 0.79 | 0.96 (0.75–1.22) | 0.71 |
| Distance to NICU (miles) | ||||
| <10 | Reference | Reference | ||
| ≥10 and <20 | 1.12 (0.98–1.28) | 0.11 | 1.01 (0.88–1.14) | 0.93 |
| ≥20 | 0.95 (0.84–1.08) | 0.46 | 0.91 (0.80–1.03) | 0.13 |
| Less than high school education or GED* (%) | ||||
| <10 | Reference | Reference | ||
| ≥10 and <30 | 0.78 (0.69–0.89) | <0.001 | 0.73 (0.64–0.83) | <0.001 |
| ≥30 | 0.69 (0.58–0.83) | <0.001 | 0.63 (0.52–0.75) | <0.001 |
| Median household income* ($) | ||||
| <30,000 | Reference | Reference | ||
| 30,000–59,999 | 1.28 (1.10–1.48) | 0.001 | 1.40 (1.20–1.64) | <0.001 |
| ≥60,000 | 1.37 (1.11–1.68) | 0.003 | 1.54 (1.26–1.89) | <0.001 |
| Single female household* (%) | ||||
| <10 | Reference | Reference | ||
| ≥10 and <30 | 0.92 (0.80–1.07) | 0.27 | 1.00 (0.88–1.15) | 0.98 |
| ≥30 | 0.80 (0.67–0.96) | 0.02 | 0.82 (0.69–0.98) | 0.03 |
| Necrotizing enterocolitis | 0.67 (0.52–0.86) | 0.002 | 0.66 (0.49–0.88) | 0.005 |
| Late-onset sepsis | 0.81 (0.66–0.99) | 0.04 | 0.75 (0.60–0.94) | 0.01 |
| Donor breast milk provision | 0.60 (0.53–0.67) | <0.001 | 0.69 (0.61–0.78) | <0.001 |
Percentages and medians refer to individuals living in maternal census tract. CI, confidence interval; GED, general equivalency diploma; MBM, maternal breast milk; NICU, neonatal intensive care unit; OR, odds ratio.
Compared with infants born at <26 weeks’ gestation, those born at 26–28 weeks’ gestation (OR 0.79, 95% CI 0.68–0.93, p=0.004), 29–32 weeks’ gestation (OR 0.60, 95% CI 0.51–0.71, p<0.001), and >32 weeks’ gestation (OR 0.61, 95% CI 0.42–0.88, p=0.008) were less likely to receive maternal BM at 30 days of age. Infants receiving any donor BM prior to DOL 30 were less likely to receive maternal BM on DOL 30 than those not exposed to donor BM (OR 0.60, 95% CI 0.53–0.67, p<0.001). Infants with a history of NEC (OR 0.67, 95% CI 0.52–0.86, p=0.002) or late-onset sepsis (OR 0.81, 95% CI 0.66–0.99, p=0.04) were less likely to receive maternal BM on DOL 30. Compared with mothers residing in areas with a median income of <$30,000, those residing in areas with median incomes of $30,000-$59,999 (OR 1.28, 95% CI 1.10–1.48, p=0.001) and >$60,000 (OR 1.37, 95% CI 1.11–1.68, p=0.003) were more likely to provide maternal BM through to DOL 30. Mothers residing in areas in which ≥30% of households were led by a single female individual were less likely to provide maternal BM through to discharge (OR 0.80, 95% CI 0.67–0.96, p=0.02). Mothers residing in areas in which ≥30% of individuals did not have a high school education or a general equivalency diploma (GED) were less likely to provide maternal BM through to DOL 30 (OR 0.69, 95% CI 0.58–0.83, p<0.001).
A total of 8097 infants were discharged home, and 4003/8097 (49%) were receiving maternal BM at discharge (Table 4; available at www.jpeds.com). Covariates that were predictive of maternal BM provision at DOL 30 were similar to those that were predictive of maternal BM provision at discharge (Table 3). In contrast to our findings at DOL 30, however, those born at 26–28 weeks’ gestation (OR 1.32, 95% CI 1.12–1.55, p=0.001), 29–32 weeks’ gestation (OR 2.10, 95% CI 1.78–2.48, p<0.001), and >32 weeks’ gestation (OR 2.66, 95% CI 1.82–3.88, p<0.001) were more likely to receive maternal BM at discharge than infants born at <26 weeks’ gestation. In addition, higher Apgar scores were associated with increased likelihood of receiving maternal BM at discharge (Table 4: online).
Table 4.
Demographics and clinical characteristics by exposure to maternal BM at discharge.
| Maternal BM at Discharge N=4003 (49) |
No Maternal BM at Discharge N=4094 (51) |
P-value | |
|---|---|---|---|
| Gestational age (weeks) | <0.001 | ||
| <26 | 400 (10) | 727 (18) | |
| 26–28 | 1362 (34) | 1698 (41) | |
| 29–32 | 2127 (53) | 1602 (39) | |
| >32 | 113 (3) | 67 (2) | |
| Male sex | 2033 (51) | 2018 (49) | 0.18 |
| 5-min. Apgar score | <0.001 | ||
| 0–3 | 97 (2) | 189 (5) | |
| 4–6 | 453 (12) | 697 (17) | |
| 7–10 | 3384 (86) | 3117 (78) | |
| Maternal race | <0.001 | ||
| White | 2098 (54) | 1557 (39) | |
| Black | 812 (21) | 1601 (41) | |
| Hispanic | 651 (17) | 650 (16) | |
| Other | 307 (8) | 141 (4) | |
| Cesarean delivery | 3089 (78) | 3055 (75) | 0.003 |
| Maternal age (years) | <0.001 | ||
| ≤19 | 189 (5) | 603 (15) | |
| 20–29 | 1761 (44) | 2145 (53) | |
| 30–39 | 1856 (47) | 1177 (29) | |
| ≥40 | 185 (5) | 154 (4) | |
| Prenatal care | 3812 (95) | 3865 (94) | 0.10 |
| Distance to NICU (miles) | 0.001 | ||
| <10 | 1664 (42) | 1838 (45) | |
| ≥10 and <20 | 1045 (26) | 934 (23) | |
| ≥20 | 1290 (32) | 1312 (32) | |
| Less than high school education or GED* (%) | <0.001 | ||
| <10 | 1839 (46) | 1176 (29) | |
| ≥10 and <30 | 1640 (41) | 1950 (48) | |
| ≥30 | 524 (13) | 968 (24) | |
| Median household income* ($) | <0.001 | ||
| <30,000 | 488 (12) | 980 (24) | |
| 30,000–59,999 | 2021 (51) | 2222 (54) | |
| ≥60,000 | 1493 (37) | 888 (22) | |
| Single female household* (%) | <0.001 | ||
| <10 | 1047 (26) | 714 (18) | |
| ≥10 and <30 | 2089 (52) | 1907 (47) | |
| ≥30 | 867 (22) | 1471 (36) | |
| Necrotizing enterocolitis | 87 (2) | 163 (4) | <0.001 |
| Late-onset sepsis | 176 (4) | 304 (7) | <0.001 |
| Donor breast milk provision | 1024 (26) | 1282 (31) | <0.001 |
Data presented as n (%).
Percentages or medians refer to individuals living in the maternal census tract. GED, general equivalency diploma; MBM, maternal breast milk; NICU, neonatal intensive care unit.
Discussion
We studied factors predicting continued maternal BM provision in VLBW infants through to DOL 30 and identified the following significant variables: increased maternal age, white maternal race, absence of history of NEC or late-onset sepsis, higher household income, lower education level, lack of donor breast milk exposure, and lower GA. Consistent with a study performed at Pediatrix NICUs in 1999–2000, we found that provision of maternal BM varied substantially among sites.25 The variability in maternal BM provision among sites supports the notion that there are modifiable factors that can be influenced by interventions to increase maternal BM provision. Our findings can inform such targeted interventions to decrease barriers to continued maternal BM provision in this population of infants, who remain less likely to receive maternal BM at 6 months of age than term counterparts despite the World Health Organization’s recommendation of exclusive breast milk feedings for all infants during the first 6 months of life.31 These interventions are increasingly important, as ingestion of maternal BM in premature infants has previously been shown to have dose-dependent positive effects on post-NICU hospital readmissions as well as neurodevelopmental outcomes.14,15 Understanding which factors predict sustained maternal BM provision can inform structured support programs specifically tailored to the demographics of the individual NICU.
Whereas previous studies have focused largely on breastfeeding rates in the NICU or at NICU discharge, we chose to examine maternal BM provision at DOL 30 in order to identify factors uniquely predictive of continued provision of maternal BM among mothers who initiated lactation. Furthermore, we speculate that the 30-day time point might serve as an appropriate marker for measuring maternal commitment to continued maternal BM provision or direct breastfeeding. In addition, many infants have achieved a substantial volume of milk intake by DOL 30. Among infants who received any maternal BM, we observed that 71% received maternal BM at DOL 30 and 49% at discharge, lower than the 60% maternal BM provision rate at NICU discharge observed by Brownell et al.2 The Brownell study involved a single-center cohort of infants cared for at a NICU with a well-established lactation program; we were unable to quantify the degree of lactation support in the NICUs in our study. These results may prove useful in the development of educational programs aimed at encouraging breast milk provision up to and post-discharge. Lactation counseling for mothers of VLBW infants is often aimed at easing mothers’ anxiety about their children’s health and promoting lactation initiation. In contrast, efforts to promote continued maternal BM provision in the NICU should involve the entire NICU team and perhaps emphasize achievable short-term goals, such as initiation of pumping in the first postnatal hours, enhancing skin-to-skin contact, production and provision of colostrum to NICU infants, and optimizing postpartum and NICU staff support of mothers’ efforts on sustained lactation up to DOL 30.32 Acknowledging the challenges and designing interventions to support mothers with lower incomes (e.g., facilitating the search for and purchasing of pumps) may also improve rates of 30-day provision of maternal BM.33
Consistent with previously published findings, we found that maternal race, maternal age, education level, married status, and median household income in the census block wherea family lives are associated with maternal BM provision in VLBW infants at both DOL 30 and discharge. A 2011 retrospective study concluded that black mothers, mothers of lower socioeconomic status, and younger mothers had less success in continuing maternal BM provision at discharge from the NICU.24 Although this study did not specifically examine maternal BM provision on DOL 30, similarities between the contributing factors support our conclusion that race, maternal age, and income are important predictors of longer-term maternal BM provision in VLBW infants. Some or all of these factors also may be correlated with more direct barriers to prolonged maternal BM provision, such as limited access to prenatal care, NICU-specific breastfeeding education and equipment (such as hospital-grade electric breast pumps), postpartum support, and resources required to provide maternal BM to a non-breast feeding preterm infant. A 2011 report by the Centers for Disease Control and Prevention cited several racial disparities in access to maternity care practices known to support breastfeeding.34 Racial differences in maternal BM provision rates might also reflect cultural influences on breastfeeding experiences, knowledge, and perception.21,35–37
Interestingly, extreme prematurity (GA <26 weeks) was associated with increased likelihood of maternal BM provision at DOL 30, but decreased likelihood of maternal BM provision at discharge. This finding agrees with results of previous studies. For instance, a 2003 retrospective study of 42,891 NICU infants determined that infants of older GA were more likely to receive maternal BM at discharge.25 However, this older study included term infants in addition to preterm infants. Compared with late preterm and term infants, very preterm infants may be at higher risk for absence of maternal BM exposure at discharge given their longer length of hospital stay. Another study has documented findings similar to our results at DOL 30; Colaizy et al demonstrated an increased likelihood of providing maternal BM for at least 4 weeks in infants with a GA of <32 weeks compared with more mature infants admitted to the NICU.18 We propose 2 possible explanations for our finding that the least mature infants in our study had an increased likelihood for maternal BM at DOL 30. First, because their children were at risk for a number of complications, mothers of the least-mature infants may have received stronger counseling and greater support for providing maternal BM from their NICU caregivers, including more targeted provision of pumps and other time-related resources, thus increasing the likelihood of maternal BM provision. It is also possible that smaller and less mature infants required lower volumes of milk than larger infants, leading to a longer length of time that a stored maternal BM supply was available for use.
A history of NEC or late-onset sepsis in the first 30 days of life was associated with decreased likelihood of maternal BM provision. Critical illness in the NICU can be a significant maternal stressor, which has been associated previously with decreased breast milk provision.38 Additionally, infants without maternal BM receipt at DOL 30 may have lacked the protective effect of maternal BM in earlier weeks, possibly leading to an increased risk of NEC and late-onset sepsis.8,39
We also found that receipt of donor BM prior to DOL 30 is associated with decreased likelihood of maternal BM provision at DOL 30 and at discharge. This observation is consistent with the notion that infants receiving donor BM in the first few weeks of life (potentially indicating a problem with maternal BM supply) are likely to continue receiving donor BM at DOL 30. Although several previous studies have disagreed with our findings and have shown that donor BM does not reduce rates of maternal BM provision, another has suggested that maternal BM provision, particularly in low-income black women, can be negatively impacted by donor BM programs.40,41 In addition, because donor BM use can occur because of maternal complications of pregnancy or pre-existing conditions that preclude sufficient maternal BM provision, there is a need for NICU-specific lactation care by personnel who can diagnose and manage these complications. Although donor BM has been shown to have advantages over formula,42 the advantages of maternal BM over both donor BM and formula have been well-described in the literature.43
Consistent with a previous single-center study,22 geographic distance to the nearest NICU was not a significant predictor of maternal BM provision at DOL 30. We had hypothesized that increased distance between the home and the NICU would increase mother-infant separation and therefore represent a barrier to consistent and prolonged provision of maternal BM. We had also hypothesized that mothers living far away from a NICU might have less access to prenatal care and less exposure to breastfeeding-promotion programs. Although we excluded outborn infants from our sample to control for the fact that many infants born at smaller centers are transferred to larger centers, 32% of mothers in our study lived ≥20 miles from the NICU. We did not observe a significant difference in maternal BM provision by these mothers at DOL 30 or discharge. It is possible that other factors not available in our dataset, such as access to private or public transportation, could have an impact on maternal BM provision.
Strengths of our study include the large number of included infants and the diverse patient population. We were able to show a substantial variation in maternal BM provision among a large number of included study sites. Our study was limited by a lack of information describing the existence of NICU-specific, evidence-based lactation support programs and the number of lactation specialists available. We also could not determine whether breast pumps were provided for mothers or whether mothers were exposed to medications or had medical diagnoses that may have affected maternal BM supply. An additional limitation of this study is the use of maternal BM feedings at DOL 30 to represent mothers’ continued provision of maternal BM. It is possible that we may have overestimated the maternal BM provision rate by including infants who continued to receive stored frozen maternal BM from earlier in the NICU hospitalization. We were also unable to quantify the volume of maternal BM received, which prevented us from examining what factors affect the establishment of a full milk supply, and the use of fortifiers, which may have affected the volume of maternal BM required. Furthermore, the variables of maternal education, household income, and single female household were all based on census data (referring to the block group in which with the mother’s home address is located and U.S. census data for that location). Of course, a mother’s personal demographics may not always match the demographics of her surrounding region. However, insight by providers into the socioeconomic demographics of a community may be important for them to implement the most innovative, cost-effective strategies to promote sustained maternal BM provision.
Going forward, significant work remains to elucidate barriers to mothers’ ability to provide maternal BM for their VLBW infants. A survey-based, prospective study gathering and aggregating data derived from maternal motivation surveys in addition to providers’ attitudes and available NICU resources may provide additional insight into mothers’ reasons for providing maternal BM to their VLBW infants. In addition, the variation in maternal BM provision among sites in our study indicate that some NICUs excel at acquiring and feeding human milk but others do not. In-depth studies of individual centers are needed to determine differences in NICU-specific, evidence-based lactation care.
Acknowledgments
R.G. receives research support from the National Institutes of Health (NIH) (HHSN 275201000003I, HHSN 272201300017I), and from the Food and Drug Administration (HHSF223201610082C). D.B. received support from the NIH (4 R25 HD076475–04). A.P. received support from the NIH (R03HD081412). P.S. received support from the NIH (1 R21 HD080606 01A1, 1R18AE000028–01, DHHS). The other authors declare no conflicts of interest.
Acronyms and Abbreviations:
- CI
confidence interval
- DOL
day of life
- GA
gestational age
- BM
breast milk
- NEC
necrotizing enterocolitis
- NICU
neonatal intensive care unit
- OR
odds ratio
- VLBW
very low birth weight
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Nutrition, Physical Activity and Obesity: Data, Trends and Maps. Available at: https://www.cdc.gov/nccdphp/dnpao/data-trends-maps/index.html. Accessed July 1, 2015.
- 2.Brownell EA, Lussier MM, Hagadorn JI, McGrath JM, Marinelli KA, Herson VC. Independent predictors of human milk receipt at neonatal intensive care unit discharge. Am J Perinatol. 2014;31:891–898. [DOI] [PubMed] [Google Scholar]
- 3.Meier P, Patel A, Esquerra-Zwiers A. Donor Human Milk Update: Evidence, Mechanisms, and Priorities for Research and Practice. J Pediatr. 2017;180:15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel AL, Johnson TJ, Engstrom JL, Fogg LF, Jegier BJ, Bigger HR, et al. Impact of early human milk on sepsis and health-care costs in very low birth weight infants. J Perinatol. 2013;33:514–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson TJ, Patel AL, Bigger HR, Engstrom JL, Meier PP. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology. 2015;107:271–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel AL, Johnson TJ, Robin B, Bigger HR, Buchanan A, Christian E, et al. Influence of own mother’s milk on bronchopulmonary dysplasia and costs. Arch Dis Child Fetal Neonatal Ed. 2017;102:F256–F261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eidelman AI. Breastfeeding and the use of human milk: an analysis of the American Academy of Pediatrics 2012 Breastfeeding Policy Statement. Breastfeed Med. 2012;7:323–324. [DOI] [PubMed] [Google Scholar]
- 8.Hylander MA, Strobino DM, Dhanireddy R. Human milk feedings and infection among very low birth weight infants. Pediatrics. 1998;102:E38. [DOI] [PubMed] [Google Scholar]
- 9.Hylander MA, Strobino DM, Pezzullo JC, Dhanireddy R. Association of human milk feedings with a reduction in retinopathy of prematurity among very low birthweight infants. J Perinatol. 2001;21:356–362. [DOI] [PubMed] [Google Scholar]
- 10.Mamemoto K, Kubota M, Nagai A, Takahashi Y, Kamamoto T, Minowa H, et al. Factors associated with exclusive breastfeeding in low birth weight infants at NICU discharge and the start of complementary feeding. Asia Pac J Clin Nutr. 2013;22:270–275. [DOI] [PubMed] [Google Scholar]
- 11.Corpeleijn WE, Kouwenhoven SM, Paap MC, van Vliet I, Scheerder I, Muizer Y, et al. Intake of own mother’s milk during the first days of life is associated with decreased morbidity and mortality in very low birth weight infants during the first 60 days of life. Neonatology. 2012;102:276–281. [DOI] [PubMed] [Google Scholar]
- 12.Meinzen-Derr J, Poindexter B, Wrage L, Morrow AL, Stoll B, Donovan EF. Role of human milk in extremely low birth weight infants’ risk of necrotizing enterocolitis or death. J Perinatol. 2009;29:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sisk PM, Lovelady CA, Dillard RG, Gruber KJ, O’Shea TM. Early human milk feeding is associated with a lower risk of necrotizing enterocolitis in very low birth weight infants. J Perinatol. 2007;27:428–433. [DOI] [PubMed] [Google Scholar]
- 14.Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Higgins RD, Langer JC, et al. Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics. 2007;120:e953–e959. [DOI] [PubMed] [Google Scholar]
- 15.Vohr BR, Poindexter BB, Dusick AM, McKinley LT, Wright LL, Langer JC, et al. Beneficial effects of breast milk in the neonatal intensive care unit on the developmental outcome of extremely low birth weight infants at 18 months of age. Pediatrics. 2006;118:e115–e123. [DOI] [PubMed] [Google Scholar]
- 16.Bixby C, Baker-Fox C, Deming C, Dhar V, Steele C. A Multidisciplinary Quality Improvement Approach Increases Breastmilk Availability at Discharge from the Neonatal Intensive Care Unit for the Very-Low-Birth-Weight Infant. Breastfeed Med. 2016;11:75–79. [DOI] [PubMed] [Google Scholar]
- 17.Sisk PM, Lovelady CA, Dillard RG, Gruber KJ. Lactation counseling for mothers of very low birth weight infants: effect on maternal anxiety and infant intake of human milk. Pediatrics. 2006;117:e67–e75. [DOI] [PubMed] [Google Scholar]
- 18.Colaizy TT, Morriss FH. Positive effect of NICU admission on breastfeeding of preterm US infants in 2000 to 2003. J Perinatol. 2008;28:505–510. [DOI] [PubMed] [Google Scholar]
- 19.Colaizy TT, Saftlas AF, Morriss FH Jr. Maternal intention to breast-feed and breast-feeding outcomes in term and preterm infants: Pregnancy Risk Assessment Monitoring System (PRAMS), 2000–2003. Public Health Nutr. 2012;15:702–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bigger HR, Fogg LJ, Patel A, Johnson T, Engstrom JL, Meier PP. Quality indicators for human milk use in very low-birthweight infants: are we measuring what we should be measuring? J Perinatol. 2014;34:287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoban R, Bigger H, Patel AL, Rossman B, Fogg LF, Meier P. Goals for Human Milk Feeding in Mothers of Very Low Birth Weight Infants: How Do Goals Change and Are They Achieved During the NICU Hospitalization? Breastfeed Med. 2015;10:305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Riley B, Schoeny M, Rogers L, Asiodu IV, Bigger HR, Meier PP, et al. Barriers to Human Milk Feeding at Discharge of Very Low-Birthweight Infants: Evaluation of Neighborhood Structural Factors. Breastfeed Med. 2016;11:335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meier PP, Patel AL, Bigger HR, Rossman B, Engstrom JL. Supporting breastfeeding in the neonatal intensive care unit: Rush Mother’s Milk Club as a case study of evidence-based care. Pediatr Clin North Am. 2013;60:209–226. [DOI] [PubMed] [Google Scholar]
- 24.Pineda RG. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed Med. 2011;6:15–19. [DOI] [PubMed] [Google Scholar]
- 25.Powers NG, Bloom B, Peabody J, Clark R. Site of care influences breastmilk feedings at NICU discharge. J Perinatol. 2003;23:10–13. [DOI] [PubMed] [Google Scholar]
- 26.Sisk P, Quandt S, Parson N, Tucker J. Breast milk expression and maintenance in mothers of very low birth weight infants: supports and barriers. J Hum Lact. 2010;26:368–375. [DOI] [PubMed] [Google Scholar]
- 27.Davanzo R, Monasta L, Ronfani L, Brovedani P, Demarini S. Breastfeeding at NICU discharge: a multicenter Italian study. J Hum Lact. 2013;29:374–380. [DOI] [PubMed] [Google Scholar]
- 28.Davanzo R, Ronfani L, Brovedani P, Demarini S. Breast feeding very-low-birthweight infants at discharge: a multicentre study using WHO definitions. Paediatr Perinat Epidemiol. 2009;23:591–596. [DOI] [PubMed] [Google Scholar]
- 29.Spitzer AR, Ellsbury DL, Handler D, Clark RH. The Pediatrix BabySteps Data Warehouse and the Pediatrix QualitySteps improvement project system--tools for “meaningful use” in continuous quality improvement. Clin Perinatol. 2010;37:49–70. [DOI] [PubMed] [Google Scholar]
- 30.Hornik CP, Fort P, Clark RH, Watt K, Benjamin DK Jr., Smith PB, et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev. 2012;88 Suppl 2:S69–S74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The World Health Organization’s infant feeding recommendation. Available at: http://www.who.int/nutrition/topics/infantfeeding_recommendation/en. Accessed July 1, 2015.
- 32.Meier PP, Johnson TJ, Patel AL, Rossman B. Evidence-Based Methods That Promote Human Milk Feeding of Preterm Infants: An Expert Review. Clin Perinatol. 2017;44:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chamberlain LB, McMahon M, Philipp BL, Merewood A. Breast pump access in the inner city: a hospital-based initiative to provide breast pumps for low-income women. J Hum Lact. 2006;22:94–98. [DOI] [PubMed] [Google Scholar]
- 34.Lind JN, Perrine CG, Li R, Scanlon KS, Grummer-Strawn LM. Racial disparities in access to maternity care practices that support breastfeeding - United States, 2011. MMWR Morb Mortal Wkly Rep. 2014;63:725–728. [PMC free article] [PubMed] [Google Scholar]
- 35.Street DJ, Lewallen LP. The influence of culture on breast-feeding decisions by African American and white women. J Perinat Neonatal Nurs. 2013;27:43–51. [DOI] [PubMed] [Google Scholar]
- 36.Fleurant E, Schoeny M, Hoban R, Asiodu IV, Riley B, Meier PP, et al. Barriers to Human Milk Feeding at Discharge of Very-Low-Birth-Weight Infants: Maternal Goal Setting as a Key Social Factor. Breastfeed Med. 2017;12:20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Anstey EH, Chen J, Elam-Evans LD, Perrine CG. Racial and Geographic Differences in Breastfeeding - United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2017;66:723–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Purdy IB, Singh N, Le C, Bell C, Whiteside C, Collins M. Biophysiologic and social stress relationships with breast milk feeding pre- and post-discharge from the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2012;41:347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lucas A, Cole TJ. Breast milk and neonatal necrotising enterocolitis. Lancet. 1990;336:1519–1523. [DOI] [PubMed] [Google Scholar]
- 40.Meier P, Patel A, Esquerra-Zwiers A. Donor Human Milk Update: Evidence, Mechanisms, and Priorities for Research and Practice. J Pediatr. 2017;180:15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams T, Nair H, Simpson J, Embleton N. Use of Donor Human Milk and Maternal Breastfeeding Rates: A Systematic Review. J Hum Lact. 2016;32:212–220. [DOI] [PubMed] [Google Scholar]
- 42.Quigley M, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database Syst Rev. 2014:CD002971. [DOI] [PubMed] [Google Scholar]
- 43.Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010;50:85–91. [DOI] [PubMed] [Google Scholar]