Abstract
Injury to the proximal tibiofibular joint can lead to lateral knee pain and instability owing to chronic rupture of the posterior tibiofibular ligament. The condition is often missed, and the true incidence is unknown. A variety of surgical treatments have been proposed over the last decades. Methods such as arthrodesis and fibular head resection have largely been replaced with various reconstruction techniques using autografts. The purpose of this report is to describe our method for treatment of proximal tibiofibular joint instability by dynamic internal fixation with a suture button.
Injury to the proximal tibiofibular joint (PTFJ) is a rare but recognized injury and can cause significant disability and symptoms. Typically, the injury occurs during external rotation of the leg with the foot in plantar flexion and the knees bent. The stress is directed through the fibula and causes the fibular head to sublux laterally. In some cases, there is no history of trauma, and the condition might be bilateral, especially in patients with general joint laxity.1
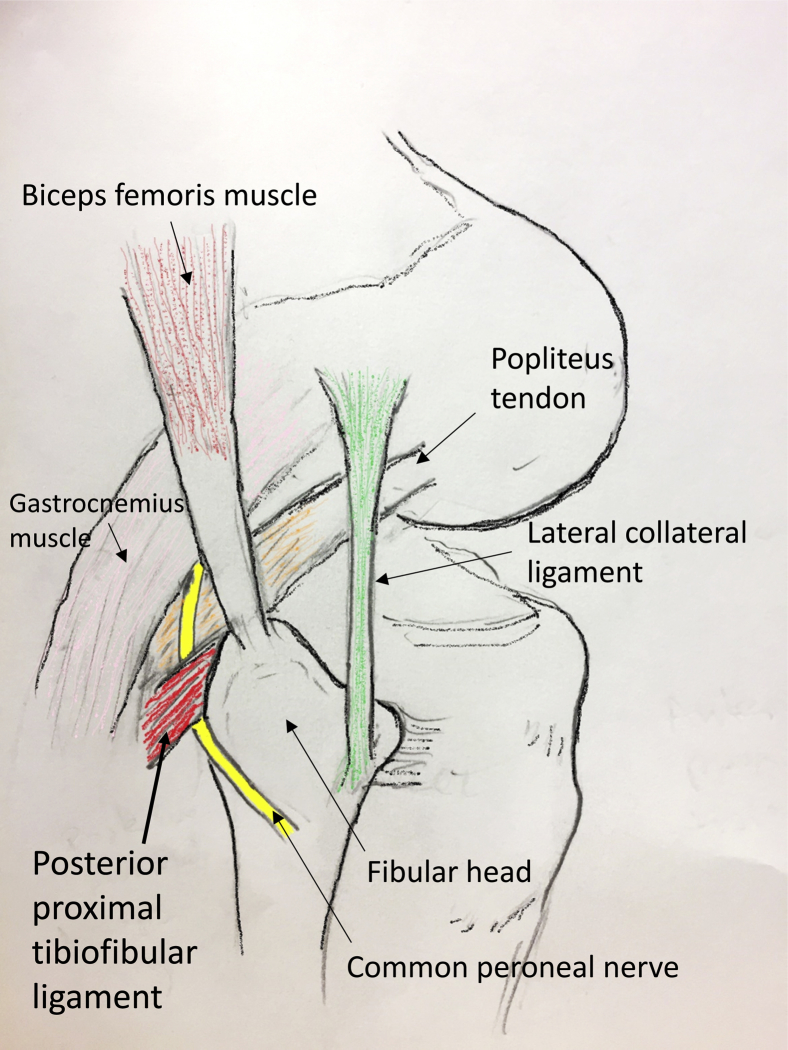
Most often, it is the posterior proximal tibiofibular ligament that is ruptured. This ligament is a relatively thin structure, compared with the more rigid anterior ligaments that are augmented by the biceps femoris tendon (BFT; Fig 1).2 The lateral collateral ligament (LCL) and the BFT are not involved, and the injury is often missed initially. There may be little or minimal swelling, and weight bearing is often possible. The patient will often experience pain, especially during squatting. Neurologic symptoms may be present owing to irritation of the common peroneal nerve (CPN), which winds around the fibular head. Radiological diagnosis can be difficult, but a thorough clinical examination will often be sufficient to make the diagnosis. An anterolateral subluxation maneuver of the fibular head will confirm the diagnosis. In chronic cases the instability is obvious, especially in deep flexion (squatting). Comparison with the contralateral knee is useful, as there is great variation in the physiological laxity of the PTFJ. Magnetic resonance imaging scans are also useful to exclude or confirm concurrent knee injuries.
Fig 1.
Lateral view of the right knee. Instability is caused by rupture of the posterior proximal tibiofibular ligament. The common peroneal nerve winds around the fibular head and must be protected during surgery.
The optimal surgical treatment for chronic instability of the PTFJ is not known. The purpose of this article is to describe our treatment for PTFJ instability by internal fixation with a dynamic suture button (TightRope; Arthrex, Naples, FL; Video 1)
Surgical Technique
Patient Positioning
The patient is placed in the supine position, with both legs draped free. Manipulation under anesthesia is performed to confirm the diagnosis, and the degree of instability is compared with the contralateral knee. We use a proximally placed tourniquet inflated to 250 mm HG. A single dose of intravenous prophylactic antibiotics is administrated according to current institutional guidelines.
Direct Suture of the Proximal Tibiofibular Ligament
The BFT and LCL are palpated in flexion and outlined with a sterile marking pen (Fig 2). A slightly curved lateral incision over the fibular head is made. Careful dissection to the posterior aspect of the joint is carried out. The CPN is visualized and protected (Fig 3). The posterior capsule is identified with the insertion of the BFT and the LCL (Fig 4). Just below these structures, the posterior proximal tibiofibular ligament is inspected. The ligament is mobilized if necessary and repaired using a slowly resorbable suture of appropriate size. The capsule is also repaired.
Fig 2.
Skin marking of the right knee. The femoral head and the course of the common peroneal nerve are outlined.
Fig 3.
Lateral approach to the proximal tibiofibular joint, right knee. The common peroneal nerve is visualized and protected with a holding suture.
Fig 4.
Lateral approach to the proximal tibiofibular joint, right knee. Careful dissection to inspect the posterior structures of the joint. The common peroneal nerve is visualized and protected with a holding suture. The lateral collateral ligament is localized with a pean forceps.
Internal Bracing
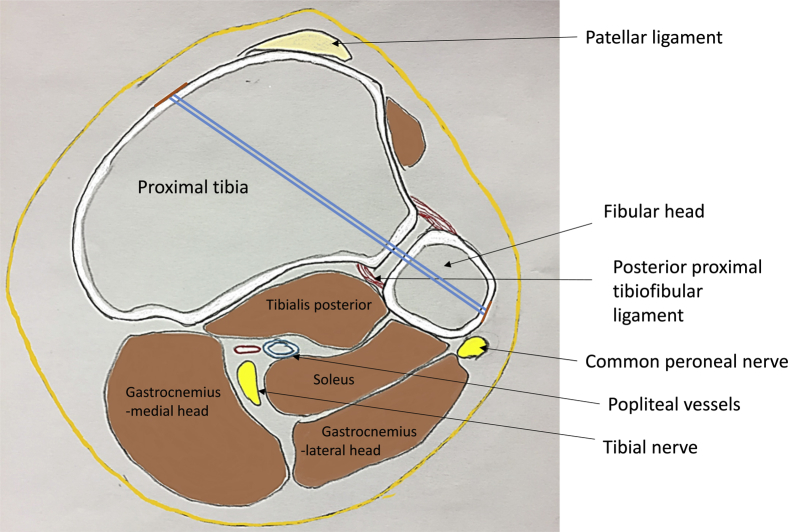
Internal bracing is performed with a knotless suture button (TightRope syndesmosis implant; Arthrex). While protecting the CPN, sharp dissection to the fibular head is performed (Fig 2). The drill sleeve is applied to the fibular head, avoiding the insertion of the LCL and the BFT (Fig 5, Table 1). The drill guide is directed in a posteroanterior direction toward the anteromedial aspect of the proximal tibia, making sure to avoid the pes anserinus complex on the medial side (Fig 6). The drill is advanced through all 4 cortices. The TightRope needle is then passed through to the anteromedial aspect of the tibia, until it exits the skin medially. The implant is pulled through, flipping the medial button on the outside of the anteromedial cortex. The implant is pulled back laterally to ensure that the medial button is engaged against the cortex. The TightRope is subsequently tightened by pulling and spreading the sutures until the lateral button reaches the fibular head. Tightening is gradually tested by manipulation of the proximal fibula, until appropriate stability is achieved. Comparison with the contralateral knee is useful to determine adequate tightness. The BFT, LCL, and nerve are inspected, and the wound is closed in layers as per usual (Figs 7 and 8). An elastic bandage is applied from the foot to the midthigh.
Fig 5.
Lateral view of the right knee. The drill is directed in a posteroanterior direction. Safe application of the drill is performed by protecting the common peroneal nerve and placing the drill sleeve directly on the femoral head, to avoid soft tissue injury.
Table 1.
Pearls and Pitfalls of Internal Fixation of the Proximal Tibiofibular Joint With a Suture Button
| Stage | Pearls | Pitfalls |
|---|---|---|
| Incision | Use a marking pen to outline the femoral head. | If the incision is too anterior, it is difficult to obtain adequate direction of the drill. |
| Dissection | Identify and protect the common peroneal nerve. | A bursa is often present and should be removed. |
| Drilling | Place the drill sleeve directly on bone, to avoid soft tissue injury. | Be aware of the biceps femoris tendon and the peroneal nerve. |
| Tightening of the suture button | Compare laxity with contralateral knee. | Make sure the medial button is flipped by pulling the implant laterally. |
Fig 6.
Axial view of the proximal tibia, right knee. The drill guide is directed in a posteroanterior direction through the fibular head toward the anteromedial aspect of the proximal tibia, making sure to avoid the pes anserinus complex on the medial side. The drill is advanced through all 4 cortices.
Fig 7.
Closing the wound, right knee. The wound is closed in layers, using subcutaneous absorbable sutures.
Fig 8.
Inspection of the surgical scar, 5 weeks after internal fixation of the proximal tibiofibular joint of the right knee.
Rehabilitation Protocol
The postoperative care is divided into 4 phases:
Phase 1: The first 2 weeks. Protected weight bearing with crutches is permitted. The focus is to regain contact with the quadriceps muscle and let the wound heal. Range of motion exercises to achieve full extension are recommended. Flexion is limited to 70°.
Phase 2: Two to 4 weeks postoperatively. Weight bearing is gradually permitted, supported by crutches if necessary, as well as cycling with low resistance, permitting full range of motion. Muscle resistance exercises but avoiding biceps femoris activation in flexion are also recommended.
Phase 3: Four to 8 weeks postoperatively. Full weight bearing is permitted as well as strengthening exercises, including the biceps femoris, mainly through hip extension. Swimming and cycling with moderate restriction and running, toward the end of the period, are permitted.
Phase 4: After 8 weeks. Return to full strength training, treadmill running, explosive running exercises, direction changes. Return to sport is individualized according to symptoms and type of sport. In our experience, full return to competitive sport takes 3 to 5 months (Table 1).
Discussion
The purpose of this article is to describe a method of treating instability of the PTFJ with open direct repair of the posterior ligament structures and internal fixation with a dynamic suture button.
Previously, instability of the PTFJ was treated with arthrodesis or resection of the fibular head. However, late complications such as instability and pain of the ankle and knee joints have made these options less popular.3 As knee ligament reconstruction surgery has developed, various techniques to reconstruct the ligaments with autografts have been described. Reconstruction using the BFT was advocated by Giachino,4 whereas Shapiro et al.5 described reconstruction using the iliotibial band. Reconstruction of the anterior and the posterior ligamentous structures with hamstring grafts was described by Kobbe et al.6 and Morrison et al.7 Others have demonstrated that reconstruction of the anterior structures is not necessary.8, 9 The latest suggestion is to use a semitendinous graft to reconstruct the posterior ligament only.9
Stabilization without reconstruction is not new and has been described with the use of temporary screw fixation.10 The producers of the TightRope have advocated a combined reconstruction with 2 diverging TightRope implants and an additional screw fixation. However, this construct is in our opinion too rigid and can lead to screw loosening or breakage. A recently published cadaver study indicates that repair with a bicortical suspension device restores PTFJ motion.11 We therefore hypothesized that stabilization of the PTFJ by internal bracing without screw fixation (and the need of screw removal) is possible. We are proposing that direct repair and internal bracing are sufficient to treat instability of the PTFJ. This is a less invasive operation compared with reconstruction and avoids graft harvest. It is simple to perform and permits early rehabilitation. Furthermore, more formal reconstruction with a hamstring graft is still possible if instability reoccurs later.
There are some limitations to this procedure (Table 2). In chronic cases, the ligament and posterior capsule may not be repairable. If these structures do not heal, the stability will depend on the implant alone, and failure is likely. In gross instability, the use of 2 implants might be necessary.12 The main risk is affection of the CPN, which may lead to transient or chronic drop foot. The insertion of the BFT on the fibular head may also be injured during drilling and must be protected during surgery.
Table 2.
Advantages and Disadvantages of Internal Fixation of the Proximal Tibiofibular Joint With a Suture Button
| Advantages | Disadvantages |
|---|---|
| No need for graft harvest. | Posterior ligament and capsule might not be repairable in chronic cases. |
| Enables early rehabilitation and same season return to sport. | Implant failure if soft tissue structures do not heal. |
| No need for implant removal. | Formal reconstruction with hamstring graft necessary as salvage procedure in failed cases. |
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Surgical technique demonstration of internal stabilization of the proximal tibiofibular joint in a right knee, using a dynamic suture button (TightRope). The patient is placed in the supine position with the leg draped free. Manipulation under anesthesia is performed to confirm the diagnosis. The fibular head and the common peroneal nerve (CPN) are outlined with a sterile marking pen. A slightly curved lateral incision over the fibular head is made. Careful dissection to the posterior aspect of the joint is carried out. The CPN is visualized and protected. The posterior capsule and the lateral collateral ligament are identified. Internal bracing is performed with a knotless suture button. While protecting the CPN, sharp dissection to the fibular head is performed. The drill sleeve is applied to the fibular head, avoiding the insertion of the lateral collateral ligament and the biceps femoris tendon. The drill guide is directed in a posteroanterior direction toward the anteromedial aspect of the proximal tibia, making sure to avoid the pes anserinus complex on the medial side. The drill is advanced through all 4 cortices. The TightRope needle is then passed through to the anteromedial aspect of the tibia, until it exits the skin medially. The implant is pulled through, flipping the medial button on the outside of the anteromedial cortex. The implant is then pulled back laterally to ensure that the medial button is engaged against the cortex. The TightRope is subsequently tightened by pulling and spreading the sutures until the lateral button reaches the fibular head. Tightening is gradually tested by manipulation of the proximal fibula, until appropriate stability is achieved. Comparison with the contralateral knee is useful to determine adequate tightness. The wound is closed in layers as per usual.
References
- 1.Sekiya J.K., Kuhn J.E. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg. 2003;11:120–128. doi: 10.5435/00124635-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Espregueira-Mendes J.D., da Silva M.V. Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2006;14:241–249. doi: 10.1007/s00167-005-0684-z. [DOI] [PubMed] [Google Scholar]
- 3.Halbrecht J.L., Jackson D.W. Recurrent dislocation of the proximal tibiofibular joint. Orthop Rev. 1991;20:957–960. [PubMed] [Google Scholar]
- 4.Giachino A.A. Recurrent dislocations of the proximal tibiofibular joint. Report of two cases. J Bone Joint Surg Am. 1986;68:1104–1106. [PubMed] [Google Scholar]
- 5.Shapiro G.S., Fanton G.S., Dillingham M.F. Reconstruction for recurrent dislocation of the proximal tibiofibular joint. A new technique. Orthop Rev. 1993;22:1229–1232. [PubMed] [Google Scholar]
- 6.Kobbe P., Flohe S., Wellmann M., Russe K. Stabilization of chronic proximal tibiofibular joint instability with a semitendinosus graft. Acta Orthop Belg. 2010;76:830–833. [PubMed] [Google Scholar]
- 7.Morrison T.D., Shaer J.A., Little J.E. Bilateral, atraumatic, proximal tibiofibular joint instability. Orthopedics. 2011;34:133. doi: 10.3928/01477447-20101221-28. [DOI] [PubMed] [Google Scholar]
- 8.Ogden J.A. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg Am. 1974;56:145–154. [PubMed] [Google Scholar]
- 9.Warner B.T., Moulton S.G., Cram T.R., LaPrade R.F. Anatomic reconstruction of the proximal tibiofibular joint. Arthrosc Tech. 2016;5:e207–e210. doi: 10.1016/j.eats.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van den Bekerom M.P., Weir A., van der Flier R.E. Surgical stabilisation of the proximal tibiofibular joint using temporary fixation: A technical note. Acta Orthop Belg. 2004;70:604–608. [PubMed] [Google Scholar]
- 11.Pessoa P., Alves-da-Silva T., Guerra-Pinto F. Repair with bicortical suspension device restores proximal tibiofibular joint motion. Knee Surg Sports Traumatol Arthrosc. 2018 doi: 10.1007/s00167-018-5061-9. [DOI] [PubMed] [Google Scholar]
- 12.McNamara W.J., Matson A.P., Mickelson D.T., Moorman C.T., 3rd Surgical management of proximal tibiofibular joint instability using an adjustable loop, cortical fixation device. Arthrosc Tech. 2018;7:e271–e277. doi: 10.1016/j.eats.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique demonstration of internal stabilization of the proximal tibiofibular joint in a right knee, using a dynamic suture button (TightRope). The patient is placed in the supine position with the leg draped free. Manipulation under anesthesia is performed to confirm the diagnosis. The fibular head and the common peroneal nerve (CPN) are outlined with a sterile marking pen. A slightly curved lateral incision over the fibular head is made. Careful dissection to the posterior aspect of the joint is carried out. The CPN is visualized and protected. The posterior capsule and the lateral collateral ligament are identified. Internal bracing is performed with a knotless suture button. While protecting the CPN, sharp dissection to the fibular head is performed. The drill sleeve is applied to the fibular head, avoiding the insertion of the lateral collateral ligament and the biceps femoris tendon. The drill guide is directed in a posteroanterior direction toward the anteromedial aspect of the proximal tibia, making sure to avoid the pes anserinus complex on the medial side. The drill is advanced through all 4 cortices. The TightRope needle is then passed through to the anteromedial aspect of the tibia, until it exits the skin medially. The implant is pulled through, flipping the medial button on the outside of the anteromedial cortex. The implant is then pulled back laterally to ensure that the medial button is engaged against the cortex. The TightRope is subsequently tightened by pulling and spreading the sutures until the lateral button reaches the fibular head. Tightening is gradually tested by manipulation of the proximal fibula, until appropriate stability is achieved. Comparison with the contralateral knee is useful to determine adequate tightness. The wound is closed in layers as per usual.