Abstract
Objective:
To assess feasibility in engaging stressed, low-income parents with obesity in a novel mindfulness-based parent stress intervention to decrease risk of early childhood obesity.
Study eesign:
An 8-week mindfulness-based parent stress group intervention (Parenting Mindfully for Health) plus Nutrition and physical activity counseling (PMH+N) was developed for parents with obesity to prevent obesity in their at-risk 2–5 year-olds. PMH+N was compared with Control group intervention (C+N) and improvement in parenting was assessed pre/postintervention using the laboratory-based Toy Wait Task (TWT). Additionally, nutrition, physical activity, and stress were all assessed using a multi-method approach.
Results:
After establishing feasibility in 20 parent-child dyads (Phase 1), 42 dyads were randomized to PMH+N versus C+N (Phase 2). PMH+N vs. C+N demonstrated significantly higher group attendance (P < .015), improvements in parental involvement (p<0.05), and decreased parental emotional eating ratings (p<0.011). Furthermore, C+N, but not PMH+N was associated with significant increases in child BMI-percentile during treatment (p<0.03) when accounting for TWT pre/post changes in parenting scores.
Conclusions:
These findings suggest that a mindfulness-based parent stress intervention to decrease childhood obesity risk is feasible, needs further testing of therapeutic mechanisms in larger samples, and may be a potential way to attenuate risk for childhood obesity.
Trial registration:
Keywords: Childhood Obesity, MBSR, Stress Reduction, Parent Stress
Obesity is particularly common in low-income ethnic-minority children(5) and in those with parents who are obese(6). Low-income families report higher levels of adversity and stress overall(7), and parental stress is associated with overeating, decreased physical activity(8), and increased weight in both parents and children(9, 10).
Chronic stress may alter brain reward and motivation circuits that are critical for making healthful decisions(11), thereby affecting food preference and choices(12). Highly stressed parents are more likely to engage in negative and less warm parenting(10). Parenting that is low in involvement and warmth and highly punitive is associated with risk for obesity in youth(13).
The preschool population is an ideal subgroup to target in prevention programs, particularly parent programs that may improve food and activity choices offered to young children at home. Additionally, this population may especially benefit from an intervention directed toward the parent because parents regulate food and activity choices for their young children. Mindfulness interventions may help parents reduce their own stress, to better tolerate normative preschooler behaviors (eg, high emotional arousal, bids for autonomy) without over-reactivity, be more “present” in child interactions, and more accepting and compassionate towards children’s wants and needs(17).
The main goal of this study was to assess feasibility in engaging stressed, low-income parents with obesity in a novel mindfulness and stress-reduction intervention to decrease risk of early childhood obesity. We developed a Parenting Mindfully for Health plus Nutrition and physical activity counseling (PMH+N) intervention using well-established behavioral and mindfulness strategies adapted from Mindfulness-Based Stress Reduction (MBSR)(18), to reduce parent stress and improve parenting and lifestyle choices to prevent obesity in their at-risk 2–5 year-old children. We randomized parent-child dyads to PMH+N or contact Control intervention plus.Nutrition and physical activity (C+N) and hypothesized that PMH+N compared with C+N would improve parenting, decrease parent stress, increase healthy eating and physical activity, and decrease obesity risk in the children.
Methods
Parent-preschooler dyads of low-income families ($25,00–34,999/year for family of 4)(20) were recruited from the local community during the period of 8/2014 to 2/2015. The potential participating parents were advised that the study purpose was to learn about parent stress, family nutrition and health behaviors and that they had been invited to participate in this research study because they have a child between the ages of 2–5 years and they reported being stressed and had an interest in learning about a healthy nutrition and lifestyle and stress management. Pre-treatment intake assessment visits included clinical interviews, self-report questionnaires, anthropometric measures, and the TWT. Low income parents were included in the sample if they had a child in the 2–5 age group, were obese, reported high levels of perceived stress as assessed by the Perceived Stress Scale(21) (score great than 25), were able to read or write, and were excluded if they self-reported a current medical or psychiatric illness with a need for acute medical care and pharmacologic intervention for psychotic or acute psychiatric symptoms (suicidal/homicidal ideations), or if the target child had mental retardation or pervasive developmental disorder. Individuals with self reported past or current depression and anxiety disorders or those in treatment for these illnesses were not excluded. In addition, those with active, untreated, alcohol or substance use disorder as per self-report of current drug use and positive drug testing by urine toxicology were excluded. The study was approved by the Yale IRB and registered on clinicaltrials.gov (NCT01974102). Informed consent was obtained from all subjects at study enrollment. All study visits were conducted at the Yale Stress Center located in New Haven, CT.
Demographic data on parent and child, including age, race, and parent education level, was assessed with parent-report forms (Table 1). Parent and child height was measured with a stadiometer. For parents, BMI was calculated from weight and height. For children, weight and height was plotted on CDC growth charts to determine the BMI-for-age and sex percentile scores.
Table 1.
Demographics, weight measures, and parent stress measures in the total sample (Phase 1 and 2) and in Phase 2.
| Demographics | Phase 1 & 2 | Phase 2 | ||||
|---|---|---|---|---|---|---|
| All | Total Randomized |
Control+N Group | PMH+N Group | |||
| N | 62 dyads | 42 | 22 | 20 | ||
| Parents | Age (yrs) | 31.7 (6.5) | 31 (6.6) | 31.6 (6.9) | 30.2 (6.3) | |
| Sex | Female | 61 (98%) | 41 (98%) | 21 (95%) | 20 (100%) | |
| Race | White | 23 (37%) | 16 (38%) | 10 (45%) | 6 (30%) | |
| Non-white | 39 (63%) | 26 (62%) | 12 (55%) | 14 (70%) | ||
| Education (yrs) | 13.6 (2.2) | 13.9 (2.4) | 13.7 (2.4) | 14.1 (2.4) | ||
| Weight (lbs) | 211.3 (53.5) | 209.5 (47.7) | 204.2 (51.3) | 215.2 (44) | ||
| BMI (kg/m2) | 35.8 (8.1) | 35.9 (7.6) | 34.6 (7.6) | 37.3 (7.5) | ||
| Children | Age (mos) | 44.9 (13.8) | 43.7 (14) | 43.4 (14.3) | 44.1 (13.9) | |
| Sex | Female | 36 (58%) | 24 (57%) | 12 (55%) | 12 (60%) | |
| Race | White | 18 (29%) | 14 (33%) | 9 (41%) | 5 (25%) | |
| Non-white | 44 (71%) | 28 (67%) | 13 (59%) | 15 (75%) | ||
| BMI percentiles | 68 (27) | 67 (27) | 62 (25) | 72 (29) | ||
| Parent Stress | PSS | 26.0 (8.14) | 26.8 (7.85) | 28.1 (8.74) | 25.5 (6.89) | |
| PSI | 73.5 (18.61) | 73.8 (19.73) | 73.2 (24.42) | 74.5 (14.19) | ||
Standard deviation (SD); N varies between 57–62 per availability of data for each measure; PSS, Perceived Stress Scale; PSI, Parenting Stress Inventory; BMI, Body Mass Index.
To assess subjective stress levels, parents completed the Perceived Stress Scale (PSS)(21), a 14-item self-report scale, with excellent test-retest reliability and good construct validity in previous research(22), to assess the degree to which individuals appraise situations in their lives as stressful. Only those parents scoring above a 25 on the PSS were included. The alpha reliability co-efficient for the PSS in the current sample was 0.74. Parents also completed the Parenting Stress Index (PSI)-short form(23), a 36-item questionnaire, with good internal consistency and validity with other measures of family functioning(24), assessing both overall parenting stress and of the parent-child relationship, restrictions on parents’ life due to being a parent, parents’ parenting-related relationship problems with spouse/partner, parents’ feelings of social alienation and/or parental incompetence/guilt. The alpha reliability co-efficient for the PSI in the current sample was 0.92. Mindfulness skills were assessed before and after the interventions with the validated Mindfulness Attention Awareness Scale (MAAS) (25). The alpha reliability co-efficient for the MAAS in the current sample was 0.91.
Dietary intake for parent and child was measured using a Nutrition Questionnaire (NQ) based on the National Health And Nutrition Evaluation Survey (NHANES)(26). The alpha reliability co-efficient of the NQ in the current sample was 0.75. The Dutch Eating Behavior Questionnaire (DEBQ), validated and widely used in adults(27), assessed parents’ emotional eating, externalization, and dietary restraint (conscious restriction of food). The alpha reliability coefficient of the DEBQ in the current sample was 0.84.To measure daily physical activity, pedometers (Omron HJ-720it) were worn by parents throughout the study and triaxial accelerometers (Acti-graph Pensacola, Florida), previously validated for use in preschoolers (28), were worn by the children for a continuous 72-hr period in the pre- and post-treatment week.
The TWT is widely used to assess parenting and stress response in preschoolers and has been used longitudinally with minimal practice effects(19),(17). It is a 5-minute, parent-child interaction task that assesses observed parent and child emotions, behaviors and parenting skills, and provides a behavioral measure of stress-reduction-related benefits in parenting skills. TWT was conducted pre- and post 8-week intervention. After the parent-child dyads arrived, they were brought into the TWT laboratory room where a video camera had been set up on a tall cabinet and each child played with a few toys. Wait Task: After baseline assessments, the child was shown a new toy which was subsequently taken away and put on top of the cabinet just out of the child’s reach. All other toys were taken away and the child was given a broken toy. The parent was asked to explain to the child to wait 5 minutes for the toy and could only have it after the parent completed the paperwork. Children were given the toy after the Wait Task. TWT sessions were video-taped and coded by blinded raters trained on a standardized coding manual(19),(17). Ratings were made for the following domains and individual subscales: 1) Affect Expressions (parent and child positive/negative affect, shared positive affect); 2) Parenting Behaviors (warm/supportive parenting, parental involvement/structuring, negative/critical parenting); and 3) Mindful Parenting Behaviors (listening/engagement, low reactivity, non-judgmental acceptance). Each subscale within each domain were examined separately in analysis. In addition, we computed two composite scores for positive parenting (including subscale scores of parent positive affect, shared positive affect, listening/engagement scores, warm/supportive parenting scores) and negative parenting (including subscale scores of parent negative affect, shared negative affect, negative critical parenting, disengagement and parent reactivity and judgements)(19). The coding system has been shown to have good inter-rater reliability (ICC=.70, K=.89-.91) per our previous work(19),(29).
Phase 1 was the development and feasibility phase of the study. Early versions of the PMH+N and C+N interventions were implemented and revised based on feasibility of conducting the study procedures and input from the parents individually and in focus groups on their interest in study participation and level of engagement. Baseline assessments including parenting stress and feasibility of the TWT procedures were assessed. Data collected from Phase 1 led to further modification and refinement of the interventions implemented in Phase 2 to improve its relevance or needs to this population .
Phase 2 randomly assigned parent-child dyads to PMH+N or C+N interventions. Random assignment was conducted with a block randomization sequence using a random number generator where the random block size option selects block sizes of 2, 3, or 4 (at random) times the number of treatments. The random allocation sequence was generated by the study statistician and they conducted the random assignment and group allocation. There were 2 treatment conditions, and randomization was conducted in block sizes of 2 and 4 at any given time. Given the small pilot nature of the stdy, this approach ensured good balance of subjects across treatment groups. Parent were blind to treatment group until completion of all intake and baseline sessions and only randomized upon completion, so as to not bias baseline measurements. The parents presented for weekly group sessions, which included 30 minutes of nutrition and physical activity counseling (N), and the latter N component was the same in content across both the PMH and the C groups. All outcome measures, including the TWT, were conducted at pre- and post-treatment. These measures included parent and child weight (BMI, BMI percentile), parent nutrition data (NQ, DEBQ), physical activity (pedometer, accelerometer), mindfulness (MAAS) and stress (PSS, PSI) (Table 2). As this was a behavioral intervention true double blind maintenance is not possible. However, the TWT outcome assessments coding was conducted by blinded raters, and group therapists were not involved in any assessments and hence remained blind to outcome assessments. The PMH+N intervention was delivered by a therapist trained in mindfulness skills and cognitive behavior therapy expertise, and the Control (C+N) was delivered by a research staff member trained in the nutrition and physical activity psychoeducation by the registered dietician (Ms. Savoye). Thus, different individuals provided the PMH+N and the C+N intervention groups.
Table 2.
Measured Outcomes
| Control+N Group | PMH+N Group | |||||
|---|---|---|---|---|---|---|
| N=19 | N=19 | |||||
| Before intervention | After intervention | Before intervention | After intervention | |||
| Nutrition Data | ||||||
| Parents | Nutrition Questionnaire | Sweet Food | 45.4 (9.4) | 42.8 (9.8) | 44.4 (9.8) | 44.2 (8.6) |
| Junk Food | 36.8 (6.4) | 36.3 (9.3) | 35.9 (6.8) | 33.4 (9.2) | ||
| Healthy Food | 76.8 (14) | 82.5 (16.6)a | 71.2 (19) | 74.7 (13.5)a | ||
| DEBQ | Total Score | 94.7 (24.4) | 94.6 (25.2) | 89.5 (23.9) | 85.8 (20.9) | |
| Restrained Eating | 26.8 (6.7) | 29.9 (6.1) | 27.2 (8.8) | 28.8 (7.9) | ||
| Emotional Eating | 33 (17.2) | 33.5 (16.2) | 33.7 (14.4) | 28.9 (13.1)b | ||
| External Eating | 34.8 (9.9) | 31.2 (9.7) | 28.7 (8.9) | 28.1 (7.7) | ||
| Physical Activity | ||||||
| Parents | Pedometer | Steps (total per hour) |
341.9 (119) | 389.9 (200.8) | 300.3 (135.5) | 267.2 (149.8) |
| Children | Accelerometer | Kcals* (mean) | 718 (990.6) | 673.3 (1008.2) | 527.1 (491.2) | 842.1 (917.6) |
| Vigorous Activity** (mean) | 54.6 (82.2) | 40.3 (65.8) | 29.1 (45.8) | 60.1 (81.1) | ||
| Mindfulness Skills | ||||||
| Parents | MAAS | Self reported scores | 62.9 (15.7) | 63.3 (14.2) | 63.4 (16.8) | 59 (18.6) |
Main Effect of Time across both groups (p=0.04).
Significant reduction in Emotional Eating (DEBQ) in the PMH intervention group; no change in the control group (p=0.0112). There were no differences between intervention groups on PSS scores (p<0.26).
Kcals for each assessment period.
Minutes of vigourous activity. Mindfulness Attention Awareness Scale (MAAS) - higher scores show lower mindfulness.
Note: improvement in mindfulness abilities were seen in post- versus pre- assessments in the PMH+N but this difference was not statistically significant.
For 8 weeks, parents in the PMH+N group met weekly in a group setting for 2 hours. There were 2 groups (n=10 and n=9). Each group was composed of parents and a leader (trained research staff member with expertise in mindfulness interventions). Our integrated structured manualized intervention was based on mindfulness-based stress reduction techniques, behavioral control and decision-making and psychoeducation on healthy nutrition and physical activity. We based the intervention on the neuroscience of stress and behavioral control over stress and decision making, the MBSR protocol(18), mindful parenting concepts(30) and mindful eating and awareness of family choices(31). The content involved cultivating mindfulness, including present-focused awareness, nonjudgement of inner experience, non-reactivity to experience, and cultivating compassion, particularly in family lifestyle choices. Each session involved monitoring of current stressors and challenges to handling stressors (communication, emotional reactivity, eating, withdrawing/avoiding) and applying strategies of awareness, distancing with awareness, diverting attention, and deflecting and reflecting. Sessions 1–4 used mindfulness strategies from the Kabat-Zinn MBSR curriculum(18), adding a focus on eating/physical activity choices and adaptive decision-making for self and family. Sessions 5–8 focused on mindful-parenting concepts(30), increasing mindful eating at family meals, awareness of own and child’s body, and awareness of family lifestyle choices(31). Sessions from each cycle were videotaped with the camera focused on the group leader and a random number of sessions (minimum of 30%) were reviewed by Dr. Sinha to ensure fidelity.
For 8 weeks, parents in C+N also met weekly in a 2-hour group setting (with group leader, a different individual than PMH+N leader in order to prevent any leakage of intervention and preserve fidelity). During the C+N group sessions, participants watched a 50-minute nature video, followed by a 40-minute group discussion and received 30 minutes of nutrition and physical activity counseling (as in the PMH+N group). The group controlled for contact with a leader and other parents, engagement in a quiet but stimulating activity with benefits, and homework, as done in previous MBSR studies(32).
Based on Phase 1 feedback, all individual sessions with the dietitian were eliminated. Instead, psychoeducational nutrition counseling was developed with the study registered dietitian and included in both interventions within each group session. Each group counseling session included discussion about family food and physical activity records, goal setting, healthy eating and physical activity for parent and child. Topics included the USDA My Plate, reading food labels, decreasing sugar and increasing fruits and vegetable intake, healthy breakfast choices, and healthier fast foods choices. Goal-setting included achieving national physical activity recommendations, using pedometers effectively for self-monitoring, and increasing activity in parents and children in hot and cold weather.
Statistical analyses
Descriptive statistics on demographic and individual characteristics of parent-child dyads were conducted using t-tests, analyses of variance, and chi square tests. In Phase 2 for the pilot intervention study, Linear Mixed Effects Models (LMEs) were used to assess the effects of Intervention group (PMH+N versus C+N) and Time (pre-vs-post intervention) and Intervention Group X Time interactions on outcome measures. We also reported trend level effects (p’s<0.15) to determine effect sizes and evaluation of whether a larger study is warranted. Significant effects from the LMEs were further assessed for pre-to-post changes in each of the intervention groups. To assess the impact of PMH+N vs C+N intervention on parenting behaviors in the TWT and childhood obesity risk, we conducted a multiple regression model using pre-to-post changes in TWT parenting composite scores (both positive and negative) as covariates in the model to include the potential effects of PMH+N/C+N on parenting behaviors in assessing the effects of intervention on child BMI outcome. The primary out come of the study was child BMI and the secondary outcomes included parenting behaviors, parent emotional eating, and child and parent physical activity and healthy eating.
Results
Sixty-two parent and preschooler dyads were studied across the two phases (Table 1). The parents were of low income, majority being single, with multiple children including the target preschool child. Of the 62 parents 95% (n=59) were biological mothers, one was the biological father, one was an adoptive mother, and one was a grandmother. The parents reported high stress levels relating to multiple roles of parenting, and in some cases primary family breadwinner with multiple jobs, and caretaker of other family members.
In Phase 1, of the 20 parent-child dyads who participated in baseline assessments, seventeen (85%) continued post baseline in the study and provided feedback during participation in the initial pilot/development phase of PMH+N and C+N interventions (Figure 1; available at www.jpeds.com). Parents were found to be most responsive to online and social media recruitment strategies and stayed in touch with the research staff most effectively via texting and phone contact. In initial qualitative feedback, there was high interest in learning better ways to cope with stress, with particular focus on parent stress and making healthy choices, including nutrition, for themselves and their families. Parents responded positively to the PMH+N intervention, but overwhelmingly reported preferring fewer visits, committing to once per week sessions, and were reluctant to attend separate individual nutrition counseling appointments. Additionally, the parents appreciated financial help for transportation to-from the visits and childcare during the group sessions. C+N originally involved reading a book and group discussion, however, the participants were unable to consistently find time to read and thus the contact control condition was changed to watching and discussing nature videos during the group session. Finally, participants were provided healthy snacks during group sessions and small self-care items to support self-compassion and healthy nutrition. Based on feedback, PMH+N and C+N was modified for Phase 2.
Figure 1.
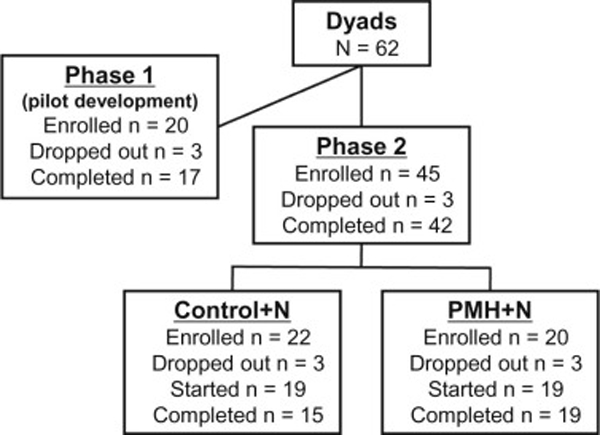
Consort Diagram.
In Phase 2, 42 parent-preschooler dyads were randomly assigned to receive either the 8-week PMH+N or C+N intervention. Thirty-eight dyads started the intervention (Figure 1).
There was a significant main effect of PMH+N vs. C+N Intervention on the domain of parenting behaviors with the parental involvement and structuring subscale (F{1,34}=4.04, p<.05, effect size f=0.34), with the PMH+N parents showing observed improvements in verbally structuring the child to the task of waiting for the toy and remaining involved with the child during that period, relative to parents in the C+N group (Figure 2, B). A trend level of significance was also found for the positive parenting Composite for the main effect of Intervention (p<0.07) and for the Intervention X Time interaction (p<0.08) for this composite, which included subscale scores of parent positive affect, shared positive affect, listening/engagement scores as well as warm/supportive parenting scores. Findings indicated that PMH+N parents increased behavioral evidence of observed positive parenting at the post-relative to pre-treatment assessment but no change was observed in the C+N parents Figure 2, B and C).
Figure 2. Results: a) Satisfaction with intervention.
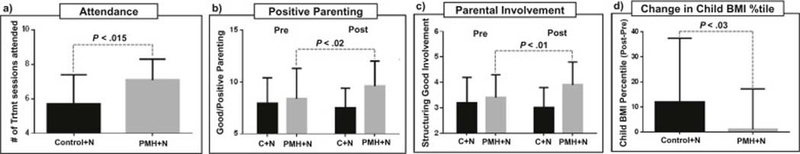
Mean attendance in the PMH+N group was significantly higher as compared with the C+N group (PMH+N mean=7.1, SD: 1.2 vs. C+N mean: 5.7, SD=1.7; p<0.015). b) and c) Parenting before and after the intervention as assessed by TWT. Improvements in ratings for positive parenting (mean change=2.1, p<0.02) and in parental involvement (mean improvement=1.0, p<0.01) in the PMH+N relative to baseline TWT response versus no significant improvement in the C+N group for positive parenting (mean change=0.6, p=ns) or parental involvement (mean change=0.2, p=ns) using blinded parent-child observer ratings in the TWT. Parental involvement during the TWT for the PMH+N group improved significantly [pre-treatment mean-scores=3.0 (SD=0.8), posttreatment mean-scores3.9 (SD=0.9); p<0.012] compared with no differences for the C+N group [pre-treatment mean-score=3.2 (SD=1.0), post-treatment mean-score=3.4 (SD=0.9); p<0.43]. Furthermore, there were significant improvements in positive parenting for the PMH+N group [pre-treatment mean-score=7.5 (SD=1.9), post-treatment mean-score9.6 (SD=2.4); p<0.015] compared with no differences for C+N [pre-treatment mean-score=7.9 (SD=2.5), post-treatment mean-score=8.4 (SD=2.9); p<0.55]. d) Child BMI percentile change in response to group intervention. Higher increase in child BMI percentile for the C+N versus the PMH+N group at post-vs-pre treatment assessment (BMI percentile change 12±25.5 vs. 1.1±16.1, respectively) Accounting for positive parenting led to a significant effects of Intervention group on child BMI percentile (F=5.39, p<0.03; Model R2=0.1665, p<.028; effect size f2=.17/ f=0.42, medium/large effect size).
There was a significant Intervention X Time interaction for the DEBQ Emotional Eating subscale scores (p<.05). PMH+N parents demonstrated significant improvements in DEBQ emotional eating scores with reductions in pre- versus post-treatment scores (mean=−4.8, SD=7.6) compared with C+N parent (mean=0.7, SD=8.0). An overall main effect of Time was observed (F{1,32}=4.53, p<0.04, effect size f=0.36) with improvements for the healthy eating subscale of the Nutrition Questionnaire (NQ) across both groups (Table 2). No other significant effects of time or intervention groups were found for the eating subscales scores (sweet food, junk food), parent BMI or on parent stress levels (p’s>0.5). Finally, mindfulness ratings, assessed with MAAS (25), were not statistically different at baseline or post intervention in mindfulness self-report.
There was no statistically significant difference in physical activity in the parents, though by steps per hour there was a trend for increased steps after C+N and a decrease in steps after PMH+N. In children, mean vigorous activity increased non-significantly after PMH+N, but not with C+N (Table 2).
To account for the changes in observed parenting behavior subscales of positive parenting and negative parenting were included as covariates in assessing the effects of PMH+N versus C+N on Child BMI percentiles in a multiple regression model. We found the that PMH+N versus C+N Intervention was significantly predictive of change in child BMI percentiles, after accounting for post-pre positive and negative parenting composite scores (p<0.03; Model R2=0.1665). Findings indicate that child BMI percentiles increased by 12±25.5 in the C+N group from pre- to post- intervention but remained stable and increased only minimally 1.1±16.1 in the PMH+N group (Figure 2, D).
Discussion
We found that intervention was significantly associated with child BMI percentile after accounting for changes in positive and negative parenting; although the mechanism is not clear, one may speculate that the observed changes in structured parental involvement during the TWT and improvements in positive parenting from pre- to post- TWT, over the 8-week period contributed to the treatment effect on child BMI, as well as possibly via improved healthy eating and physical activity choices for the children. The parenting behavior changes and consequent child BMI percentile effects were observed along with improvements in healthy eating in both groups, reductions in emotional eating among parents in the PMH+N intervention group and non-significant improvements in mindfulness abilities in the parents as well as vigorous activity in the PMH+N group children, but no significant differences between groups in parent stress levels as a function of intervention. These findings suggest that addressing high stress in obese parents of preschool children to impact health and food choices may be one way to attenuate risk for childhood obesity in chronically stressed lowincome families.
Despite evidence for stress reduction with mindfulness in adults, very few studies have examined its effects on parent stress, parenting behaviors, and very young child outcomes(33) especially in low income populations. Mindfulness interventions have the potential to make a significant impact on the family environment(34),(30),(35).
Parents are presented with challenges to their ability to regulate emotions which may compromise parenting behaviors consistent with compassion and engagement in child-focused parenting(34). Parenting around feeding and physical activity can be especially stressful. Young children often reject healthy foods at first(36), and when faced with a crying preschooler/toddler who refuses to eat vegetables, parents may have difficulty coping and calmly re-offering the healthy food choice. Thus, mindfulness interventions may improve parents’ ability to manage emotions and stress and be consistent with their goal of making healthy food and physical activity choices for the family. Uncontrolled trials with small samples have found initial evidence for mindfulness-based parenting interventions for increasing parental mindfulness in pregnant women (n=27)(37), stressed parents of preschoolers (n=24)(38), and increasing parenting satisfaction and child compliance in families with preschool-aged children with developmental delays and Attention Deficit Hyperactivity Disorder (ADHD) (n’s=2–4)(39).
To assess intervention-related improvements in parenting, the TWT was used to assess observed behavioral parenting to measure change from pre/post- 8-week interventions. We found improvements in a positive parenting composite score and in parental involvement for PMH+N compared with no improvement in positive parenting levels and in parental involvement for C+N. This suggests that the PMH+N focus on stress reduction and good choices for the family had a significant impact on parenting behaviors such as involvement in parenting.
As parent obesity is a strong risk factor for child obesity(6), we examined the effects of PMH+N on improving child BMI as well as change in parent BMI. We did not find any differences between groups in parent BMI, however, this intervention was not specifically targeted for short-term rapid weight loss. Notably, there were significant improvements in parent emotional eating scores in the PMH+N group compared with the C+N group. Significant improvements were also found across both intervention groups in parents’ healthy eating scores from pre-vs-post treatment reported on the NQ, indicating that the nutrition component of the interventions in both interventions groups was equally effective.
Limitations of this study include the small sample size, limited data on the mothers due to participants’ time restraints and preference, and short intervention duration. It is also important to note that the PMH+N and C+N interventions were delivered by different group leaders. This will need further assessment as a confound in future larger studies Given the high acceptance of PMH+N, it may be beneficial to implement a longer intervention of 12 or 16 weeks to investigate the effects on both parent BMI and the child BMI percentile.
We developed a novel intervention to target obesity risk in young children of low-income stressed parents who were obese, and found it to be acceptable and of benefit for both parenting behaviors and child BMI. Further testing with a larger sample-size and long-term follow-up is warranted.
Acknowledgements:
We thank our study participants, both parents and children, in their Willingness to actively participate in this study
Funded by the NIH NCCIH (National Center for Complementary and Integrative Health) (R21AT-007708– 01A1 [toR.S.]).
Footnotes
The authors declare no conflicts of interest with the content of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002;76(3):653–8. [DOI] [PubMed] [Google Scholar]
- 3.Guo SS, Chumlea WC. Tracking of body mass index in children in relation to overweight in adulthood. Am J Clin Nutr. 1999;70(1):145S–8S. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization Obesity and Overweight Fact Sheet 2011 [Available from:http://www.who.int/mediacentre/factsheets/fs311/en/index.html.
- 5.Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL, et al. Influence of race, ethnicity, and culture on childhood obesity: implications for prevention and treatment. Obesity (Silver Spring). 2008;16(12):2566–77. [DOI] [PubMed] [Google Scholar]
- 6.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–73. [DOI] [PubMed] [Google Scholar]
- 7.Conger RD, Ge X, Elder GH, Jr., Lorenz FO, Simons RL Economic stress, coercive family process, and developmental problems of adolescents. Child Dev. 1994;65(2 Spec No):541–61. [PubMed] [Google Scholar]
- 8.Urizar GG, Hurtz SQ, Ahn DK, King AC, Albright CL, Atienza AA. Influence of maternal stress on successful participation in a physical activity intervention: the IMPACT Project. Women Health. 2005;42(4):63–82. [DOI] [PubMed] [Google Scholar]
- 9.Dallman M, Pecoraro N, Akana S, la Fleur S, Gomez F, Houshyar H, et al. Chronic stress and obesity: a new view of “comfort food”. Proc National Academy of Science. 2003;100(20):11696–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belsky J, Woodworth S, Crnic K. Trouble in the second year: three questions about family interaction. Child Dev. 1996;67(2):556–78. [PubMed] [Google Scholar]
- 11.Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry. 2013;73(9):827–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zellner DA, Loaiza S, Gonzalez Z, Pita J, Morales J, Pecora D, et al. Food selection changes under stress. Physiol Behav. 2006;87(4):789–93. [DOI] [PubMed] [Google Scholar]
- 13.Lissau I, Sorensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343(8893):324–7. [DOI] [PubMed] [Google Scholar]
- 14.Franklin TB, Russig H, Weiss IC, Graff J, Linder N, Michalon A, et al. Epigenetic transmission of the impact of early stress across generations. Biol Psychiatry. 2010;68(5):408–15. [DOI] [PubMed] [Google Scholar]
- 15.Birch L, Savage JS, Ventura A. Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Can J Diet Pract Res. 2007;68(1):s1–s56. [PMC free article] [PubMed] [Google Scholar]
- 16.Israel AC, Guile CA, Baker JE, Silverman WK. An evaluation of enhanced self-regulation training in the treatment of childhood obesity. J Pediatr Psychol. 1994;19(6):737–49. [DOI] [PubMed] [Google Scholar]
- 17.Coatsworth JD, Duncan LG, Greenberg MT, Nix RL. Changing Parent’s Mindfulness, Child Management Skills and Relationship Quality With Their Youth: Results From a Randomized Pilot Intervention Trial. J Child Fam Stud. 2010;19(2):203–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J Mindfulness-Based Stress Reduction Curriculum Center for Mindfulness in Medicine, Health Care & Society, University of Massachusetts; 2009. [Google Scholar]
- 19.Chaplin TM, Fahy T, Sinha R, Mayes LC. Emotional arousal in cocaine exposed toddlers: prediction of behavior problems. Neurotoxicol Teratol. 2009;31(5):275–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Annual Update of the HHS Poverty Guidelines. Federal Register. 2017;82(19):8831–2. [Google Scholar]
- 21.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of health and social behavior. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 22.Cohen S, Janicki-Deverts D. Who’s Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091. Journal of Applied Social Psychology. 2012;42(6):1320–34. [Google Scholar]
- 23.Abidin RR, Psychological Assessment Resources Inc. Parenting Stress Index. 3rd. ed. Odessa FL: Psychological Assessment Resources; 2012. p. 1 professional manual (vii, 167 p. [Google Scholar]
- 24.Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. J Clin Child Adolesc Psychol. 2006;35(2):302–12. [DOI] [PubMed] [Google Scholar]
- 25.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–48. [DOI] [PubMed] [Google Scholar]
- 26.Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index revised: a measurement instrument for populations. Journal of the American Dietetic Association. 1999;99(6):697–704. [DOI] [PubMed] [Google Scholar]
- 27.Francis LA, Birch LL. Maternal influences on daughters’ restrained eating behavior. Health Psychol. 2005;24(6):548–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harvey-Berino J, Rourke J. Obesity prevention in preschool native-american children: a pilot study using home visiting. Obes Res. 2003;11(5):606–11. [DOI] [PubMed] [Google Scholar]
- 29.Chaplin TM, Sinha R, Simmons JA, Healy SM, Mayes LC, Hommer RE, et al. Parentadolescent conflict interactions and adolescent alcohol use. Addict Behav. 2012;37(5):605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duncan LG, Coatsworth JD, Greenberg MT . A model of mindful parenting: implications for parent-child relationships and prevention research. Clin Child Fam Psychol Rev. 2009;12(3):255–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treating binge eating disorder: the conceptual foundation. Eat Disord. 2011;19(1):49–61. [DOI] [PubMed] [Google Scholar]
- 32.Napoli M, Krech PR, Holley LC. Mindfulness training for elementary school students. Journal of Applied School Psychology. 2005;21:99–125. [Google Scholar]
- 33.Sawyer-Cohen JA, Semple RJ. Mindful parenting: A call for research. Journal of Child and Family Studies. 2010;19:145–51. [Google Scholar]
- 34.Dumas JE. Mindfulness-based parent training: strategies to lessen the grip of automaticity in families with disruptive children. J Clin Child Adolesc Psychol. 2005;34(4):779–91. [DOI] [PubMed] [Google Scholar]
- 35.Kabat-Zinn M, Kabat-Zinn J. Everyday blessings: The inner work of mindful parenting. . New York: Hyperion; 1997. [Google Scholar]
- 36.Birch LL. Psychological influences on the childhood diet. J Nutr. 1998;128.(2 Suppl): 407S–10S [DOI] [PubMed] [Google Scholar]
- 37.Duncan LG, Bardacke N . Mindfulness-Based Childbirth and Parenting Education: Promoting Family Mindfulness During the Perinatal Period. J Child Fam Stud. 2010;19(2):190202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maloney R, Altmaier E. An initial evaluation of a mindful parenting program. J Clin Psychol. 2007;63(12):1231–8. [DOI] [PubMed] [Google Scholar]
- 39.Singh NN, Singh AN, Lancioni GE, Singh J, Winton ASW, Adkins AD. Mindfulness training for parents and their children with ADHD increases the children’s compliance. . Journal of Child and Family Studies. 2010;19:157–66. [Google Scholar]
- 40.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48(4):893–907. [DOI] [PubMed] [Google Scholar]
- 41.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Twoyear follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146(5):618–25. [DOI] [PubMed] [Google Scholar]
- 42.Berry D, Sheehan R, Heschel R, Knafl K, Melkus G, Grey MF-bifcoAr. Family-based interventions for childhood obesity: A review. Journal of Family Nursing. 2004;10(429). [Google Scholar]


