Abstract
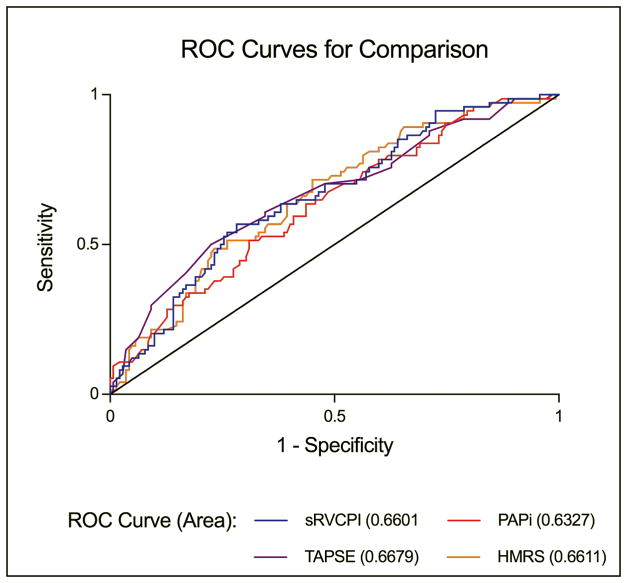
Right ventricular (RV) failure is difficult to predict and is a major determinant of poor outcomes after left ventricular assist device (LVAD) implantation. We evaluated the associations of the following variables with severe RV failure in LVAD patients: tricuspid annular plane systolic excursion (TAPSE), pulmonary artery pulsatility index (PAPi), simplified right ventricular contraction pressure index (sRVCPI), and HeartMate Risk Score (HMRS). We performed a retrospective case-control study on 216 patients who underwent continuous-flow LVAD implantation between 2008 and 2014. The primary analysis assessed the ability of HMRS, PAPi, sRVCPI, and TAPSE to predict severe RV failure. A secondary analysis evaluated the incremental benefit of combining predictive variables. Seventy-four patients developed severe RV failure (24%). Compared to the control group, the severe RV failure group had lower TAPSE (1.30 vs. 1.55, p<0.001), lower PAPi (1.77 vs. 2.47, p=0.001), lower sRVCPI (42.71 vs. 57.82, p<0.001), and higher HMRS (2.12 vs. 1.65, p<0.001). All four variables had similar ROC curves with modest AUC (0.63–0.67, all p-values <0.001). In the evaluation of combined predictive variables, the combination of TAPSE with HMRS was found to be best for predicting severe RV failure. In summary, patients at risk for severe RV failure after LVAD implantation were successfully identified using TAPSE, PAPi, sRCPI, and HMRS. The combination of TAPSE and HMRS—incidentally, the least invasive and most readily available variables—proved to be superior to RV-centric metrics for predicting severe RV failure. The predictive and clinical use of these two variables should be tested prospectively.
Keywords: Left ventricular assist device, Right ventricular failure, TAPSE, PAPi, sRVCPI, HMRS
Introduction
Left ventricular assist devices (LVADs) have improved survival and quality of life in patients with end-stage heart failure (HF).1–4 Severe right ventricular (RV) failure is a major complication of left-sided mechanical circulatory support and affects 20–40% of patients who undergo continuous-flow LVAD implantation; it remains a leading cause of death.1–3,5–7 Severe RV failure has been associated with increased bleeding, end-organ dysfunction, longer hospitalizations, and a threefold increase in the risk of death at six months.8–10 Notably, data from a high-volume LVAD center demonstrated improved mortality and bridge-to-transplant (BTT) outcomes when biventricular support was anticipated prior to surgery as opposed to RVAD implantation as secondary intervention after failure of single ventricle support.11
Several clinical variables and risk models have been evaluated in attempts to predict severe RV failure, but poor sensitivity and specificity as well as lack of external validation have limited widespread adoption of RV failure predictors.5,7,12 We hypothesized that non-invasive tests and clinical parameters might be superior invasive testing. Therefore, we sought to evaluate variables derived from different modalities (e.g. echocardiography, invasive hemodynamics, and laboratory data) for their ability to predict severe RV failure: tricuspid annular plane systolic excursion (TAPSE), pulmonary artery pulsatility index (PAPi), simplified right ventricular contraction pressure index (sRVCPI), and HeartMate Risk Score (HMRS). TAPSE is a routinely obtained echocardiographic parameter that measures the longitudinal deformation of the right ventricular free wall. sRVCPI augments TAPSE by taking RV pressure generation into account and has been correlated with right ventricular stroke work index, but its ability to predict severe RV failure after LVAD implantation has not been assessed.13,14 PAPi is a hemodynamic variable designed to assess the ability of the RV to generate a pressure gradient, but it requires invasive hemodynamics and, to date, has only been evaluated in small numbers of LVAD patients.15,16 HMRS uses readily available clinical data (age, INR, albumin, creatinine, and center LVAD volume), has been demonstrated to predict mortality at 90 days, and is routinely calculated by many centers prior to LVAD implantation. While some of the HMRS components have individually been associated with RV failure—INR, creatinine, and albumin7,10—their combination in this simple score has not been evaluated for use in predicting severe RV failure.17,18
The primary aim of our study was to compare the four identified variables for their ability to predict severe RV failure. We undertook a secondary analysis to evaluate whether a certain combination of these variables would improve prediction of severe RV failure over variables used in isolation.
Methods
This study complies with the Declaration of Helsinki and was approved by the Institutional Review Board of Washington University School of Medicine.
Data Collection
We identified 216 consecutive patients 18 years of age and older who underwent implantation of a HeartMate II (Thoratec) or HVAD (HeartWare) between June of 2008 and September of 2014 and had sufficient data to calculate TAPSE, PAPi, sRVCPI, and HMRS. No patients were undergoing pump exchange. All clinical data was extracted by review of the medical record using hemodynamic, clinical, and laboratory data recorded most proximate to LVAD implant date. Pre-implant transthoracic echocardiographic and invasive hemodynamic data were from within 90 days of LVAD implantation. All echocardiographic measurements were made according to the American Society of Echocardiography by board-certified cardiologists. sRVCPI and HMRS were measured according to Frea et al13 and Cowger et al,19 respectively. The variables were calculated as follows:
Age in years, albumin, and creatinine in g/dl. *If center LVAD volume < 15, value = 1, else = 0; this was therefore 0 in this study.
The primary analysis assessed the ability of HMRS, PAPi, sRVCPI, and TAPSE to predict severe RV failure, defined as post-implant inotropic support > 14 days, right ventricular assist device (RVAD) implantation for intra-operative or post-operative RV failure, or death within 14 days due to RV failure. A secondary analysis evaluated the incremental benefit of combining predictive variables. A combination of HMRS with the other three variables was chosen because HMRS is a well-validated and purely clinical score that is routinely used by our center in pre-LVAD evaluation to estimate near-term morality risk.
Statistical Analysis
Pre-implant characteristics from patients who developed RV failure were compared to pre-implant characteristics from those who did not using Student’s two-sample t-test for continuous variables and Fisher’s exact test for categorical variables, respectively. Non-normal and ordinal data were summarized by median (1st, 3rd quartiles) and compared using the Mann-Whitney U-test. The abilities of the four variables of interest to predict severe RV failure were assessed by determining the area under the Receiver Operating Characteristics (ROC) curves and were compared using the methods of Delong.20 Multivariable logistic regression models were used to determine if TAPSE, PAPi, or sRVCPI remained significant after adjusting for HMRS. Separate models were built for each of the three former variables.
The ability of echocardiographic or hemodynamic variables to improve prediction of severe RV failure over HMRS was further evaluated using the category-free net-reclassification index (NRI). The NRI measures the correctness of patient reclassification based on the probability of an event occurring.21 The NRI is determined as the net improvement among events plus the net improvement among non-events, where net improvement is the difference between those correctly vs. those incorrectly reclassified.
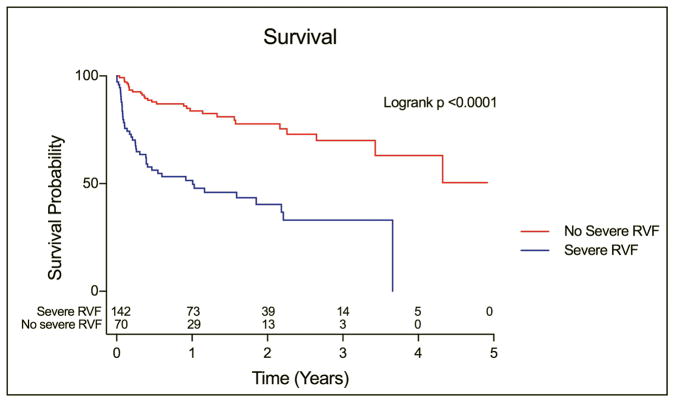
Kaplan-Meier survival curves were determined for patients with severe RV failure and without severe RV failure. Date of LVAD implant was used as the start date. Patients were censored either at date of transplant, pump exchange, or last follow-up. Curves were compared using the log-rank test. For this survival analysis, patients who died or underwent pump exchange within 14 days of implant were omitted to limit bias resulting from the definition of severe RV failure. A p-value of <0.05 was considered significant for all analyses. All statistical analyses were conducted in SAS v9.4 (SAS Institute Inc., Cary, NC). Figures were created using GraphPad Prism for Mac OS X, version 7.0a 2016 (GraphPad Software, La Jolla, California).
Results
The total study population consisted of 216 unique LVAD implants: 179 (83%) received a HeartMate II and 37 (17%) received an HVAD. The cohort was mostly male (80%), white (77%), and bridge to transplant (63%), with a mean age of 58. Seventy-four patients (34%) developed severe RV failure: 20 patients underwent RVAD implantation and 54 required inotropic support for more than 14 days without RVAD implantation. No patients included in the study population died within 14 days from RV failure. In those that developed RV failure, the baseline creatinine, INR, total bilirubin, and right atrial pressure were significantly higher than in those that did not develop RV failure. There were no other significant between-group differences (Table 1).
Table 1.
Predictors of Severe RV Failure
| Overall (N=216) | No Severe RVF (N=142) | Severe RVF (N=74) | p-value | |
|---|---|---|---|---|
| Age | 58.12 ± 10.94 | 57.14 ± 11.42 | 59.99 ± 9.78 | 0.07 |
| Male | 173 (80%) | 109 (77%) | 64 (86%) | 0.11 |
| White | 166 (77%) | 106 (75%) | 60 (81%) | 0.14 |
| BMI | 28.69 ± 5.70 | 28.20 ± 5.68 | 29.63 ± 5.66 | 0.08 |
| ICM | 98 (45%) | 61 (43%) | 37 (50%) | 0.39 |
| Diabetes | 96 (44%) | 61 (43%) | 35 (47%) | 0.57 |
| Redo Sternotomy | 59 (27%) | 34 (24%) | 25 (34%) | 0.15 |
| COPD | 33 (15%) | 21 (15%) | 12 (16%) | 0.84 |
| Bridge to Transplant | 137 (63%) | 94 (66%) | 43 (58%) | 0.21 |
| HeartMate II | 179 (83%) | 119 (84%) | 60 (81%) | 0.70 |
| Intermacs Profile | 2.0 (2.0, 2.0) | 2.0 (2.0, 2.0) | 2.0 (1.0, 2.0) | 0.49 |
| Creatinine | 1.4 (1.0, 2.0) | 1.3 (1.0, 1.8) | 1.6 (1.2, 2.1) | 0.04 |
| INR | 1.4 (1.3, 1.6) | 1.4 (1.2, 1.5) | 1.5 (1.3, 1.7) | 0.02 |
| Albumin | 3.62 ± 0.49 | 3.69 ± 0.48 | 3.50 ± 0.51 | 0.008 |
| Intubated pre-LVAD | 11 (5%) | 5 (4%) | 6 (8%) | 0.19 |
| Total bilirubin | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.5) | 1.3 (0.8, 2.2) | 0.002 |
| RA pressure (RHC) | 15.86 ± 6.84 | 14.58 ± 6.52 | 18.30 ± 6.81 | <0.001 |
| Systolic PAP | 58.55 ± 13.82 | 58.06 ± 13.33 | 59.47 ± 14.77 | 0.48 |
| Diastolic PAP | 31.11 ± 7.48 | 30.35 ± 7.19 | 32.57 ± 7.87 | 0.04 |
| Mean PAP | 40.25 ± 8.98 | 39.60 ± 8.61 | 41.50 ± 9.57 | 0.14 |
| PCWP | 27.78 ± 7.79 | 27.09 ± 7.61 | 29.14 ± 8.01 | 0.07 |
| Cardiac Index (Fick) | 1.80 ± 0.50 | 1.78 ± 0.50 | 1.85 ± 0.51 | 0.29 |
| Ejection fraction | 17.99 ± 6.65 | 18.11 ± 6.35 | 17.77 ± 7.25 | 0.73 |
| RA pressure (echo) | 13.47 ± 5.13 | 12.73 ± 5.17 | 14.96 ± 4.73 | 0.003 |
| TR Peak Velocity | 2.92 ± 0.54 | 2.98 ± 0.55 | 2.81 ± 0.52 | 0.04 |
| TAPSE | 1.47 ± 0.46 | 1.55 ± 0.45 | 1.30 ± 0.42 | <0.001 |
| HMRS | 1.81 ± 0.93 | 1.65 ± 0.86 | 2.12 ± 0.98 | <0.001 |
| RVSWI | 0.27 ± 0.16 | 0.26 ± 0.15 | 0.27 ± 0.18 | 0.63 |
| sRVCPI | 52.65 ± 27.76 | 57.82 ± 29.52 | 42.71 ± 20.82 | <0.001 |
| PAPi | 2.24 ± 1.82 | 2.49 ± 2.03 | 1.77 ± 1.22 | 0.001 |
BMI=body mass index, ICM=ischemic cardiomyopathy, RA pressure=right atrial pressure, RHC=right heart catheterization, PAP=pulmonary artery pressure, PCWP=pulmonary capillary wedge pressure, TR=tricuspid regurgitant, TAPSE=tricuspid annular plane systolic excursions, HMRS=HeartMate Risk Score, RVSWI=right ventricular stroke work index mm Hg/L*m2, sRVCPI=simplified right ventricular contraction pressure index, PAPi=pulmonary artery pulsatility index
Values are shown as absolute numbers (percentages), mean ± SD, or median (IQR).
Predictor Variables
All four variables—TAPSE, PAPi, sRVCPI, and HMRS—were significant predictors of severe RV failure (Figure 1, Table 2). The four variables performed similarly in predicting severe RV failure. Each parameter was adjusted for HMRS (our “gold standard”) and then analyzed using multivariable logistic regression—with separate models for each pair of parameters—to determine independent predictive capabilities. After HMRS adjustment, TAPSE (OR=0.27, p<0.001), PAPi (OR=0.71, p=0.015), and sRVCPI (OR=0.98, p<0.001) remained predictors of severe RV failure (Table 3).
Figure 1.
Receiver Operating Characteristics for severe RV Failure
sRVCPI=simplified right ventricular contraction pressure index; PAPi=pulmonary artery pulsatility index; TAPSE=tricuspid annular plane systolic excursion; HMRS=HeartMate risk score
Table 2.
Area Under ROC
| Predictor | AUC | 95% CI | p-value | p-value vs. HMRS |
|---|---|---|---|---|
| HMRS | 0.66 | (0.59, 0.74) | <0.001 | --- |
| TAPSE | 0.67 | (0.59, 0.75) | <0.001 | 0.90 |
| PAPI | 0.63 | (0.56, 0.71) | <0.001 | 0.60 |
| sRVCPI | 0.66 | (0.59, 0.74) | <0.001 | 0.98 |
HMRS=HeartMate Risk Score, TAPSE=tricuspid annular plane systolic excursions, PAPi=pulmonary artery pulsatility index, sRVCPI=simplified right ventricular contraction pressure index
Table 3.
Multivariable Logistic Regression Models
| OR | 95% CI | p-value | |
|---|---|---|---|
| HMRS + TAPSE | |||
| HMRS (per 1 unit increase) | 1.74 | (1.21, 2.49) | 0.003 |
| TAPSE (per 1 unit increase) | 0.27 | (0.13, 0.56) | <0.001 |
| HMRS + PAPi | |||
| HMRS (per 1 unit increase) | 1.75 | (1.23, 2.50) | 0.002 |
| PAPI (per 1 unit increase) | 0.71 | (0.54, 0.94) | 0.015 |
| HMRS + sRVCPI | |||
| HMRS (per 1 unit increase) | 1.75 | (1.22, 2.51) | 0.002 |
| sRVCPI (per 1 unit increase) | 0.98 | (0.96, 0.99) | <0.001 |
HMRS=HeartMate Risk Score, TAPSE=tricuspid annular plane systolic excursions, PAPi=pulmonary artery pulsatility index, sRVCPI=simplified right ventricular contraction pressure index
We then examined the category-free NRI to determine the incremental correct prediction gained by the addition of any of the parameters to HMRS in prediction of severe RV failure. The addition of TAPSE to HMRS produced a category-free NRI of 0.48 (p<0.001), and correctly reclassified 41% of events and 7% of non-events (Table 4). When added to HMRS, PAPi and sRVCPI also significantly reclassified patients with category-free NRI values of 0.36 (p=0.011) and 0.39 (p=0.006), respectively.
Table 4.
Category-free Net Reclassification Improvement
| Variables | NRI | 95% CI | p-value | Events correctly reclassified (%) | Non-events correctly reclassified (%) |
|---|---|---|---|---|---|
| HMRS + TAPSE | 0.48 | (0.21, 0.74) | <0.001 | 41% | 7% |
| HMRS + PAPi | 0.36 | (0.10, 0.62) | 0.011 | 43% | −7% |
| HMRS + sRVCPI | 0.39 | (0.13, 0.66) | 0.006 | 38% | 1% |
HMRS=HeartMate Risk Score, TAPSE=tricuspid annular plane systolic excursions, PAPi=pulmonary artery pulsatility index, sRVCPI=simplified right ventricular contraction pressure index
Kaplan-Meier survival curves showed significantly worse survival in those patients with severe RV failure (Figure 2). The similarities of survival curves as well as baseline characteristics indicate that the cohort in this study—with data available for TAPSE, PAPi, sRVCPI, and HMRS—is similar to the overall cohort at our institution.6
Figure 2.
Kaplan-Meier analysis of freedom from death stratified by presence of severe RV Failure
Discussion
In this study of patients undergoing implantation of continuous-flow LVADs, TAPSE, PAPi, sRVCPI, and HMRS all predicted severe RV failure after LVAD implantation. Though each predictor reached statistical significance, each variable had an AUC of 0.63–0.66, indicating only modest clinical utility. Surprisingly, HMRS—a clinical tool based on readily available data and calibrated for prediction of all-cause 90-day mortality after LVAD implantation—performed as well as the other tested predictors of severe RV failure after LVAD implantation.
Given the simplicity of HMRS, its routine use at our institution, and its prior validation in predicting mortality,17,18 we sought to evaluate (1) whether more invasive (e.g. PAPi) or RV-centric (e.g. TAPSE, sRVCPI) parameters would perform better than HMRS in our cohort, and (2) whether a combination of HMRS and one of the other three variables would perform better than HMRS alone. We demonstrated the benefit of adding any one of these three variables to HMRS and the resulting improvement in event classification. Importantly, TAPSE, PAPi, and RVCPI remained significant predictors of severe RV failure after HMRS adjustment.
We did not observe significant changes in the AUC when combinations of variables were compared to HMRS alone (Table 2). This is likely because significant changes in AUC require large differences in C-statistics that may not reflect the potential clinical usefulness of various predictors.21 Thus, to confirm the robustness of our findings, we performed category-free NRI analysis. As discussed by Pencina et al,21 the category-free NRI allows for a clear analysis of improvement with additional predictors added to a base model. Of the variables tested, TAPSE is the simplest to obtain, is noninvasive, and performed the best in evaluation by NRI. Thus, 41% of patients predicted to developed severe RV failure by HMRS alone were correctly reclassified when TAPSE was added to HMRS—i.e. the patients did not develop severe RV failure.
HMRS is a simple and robust predictor of survival in patients with LVADs, and its clinical use is well established.17–19 While TAPSE, PAPi, and sRVCPI are easily obtainable in routine clinical evaluation, data that validates and supports their use remain limited to small, retrospective studies.14,16,22 This study supports the routine use of HMRS in the evaluation of candidates for LVAD implantation for post-implant survival and extends its predictive utility to risk stratification of severe RV failure. The addition of TAPSE—a simple, routinely obtained, single echocardiographic variable—can further refine this evaluation.
Surprisingly, HMRS, which does not specifically measure RV function, performed the best of all the predictors tested. This seems to suggest that our understanding of—and ability to measure—RV function are suboptimal. Furthermore, these data support that HMRS is a robust integrator of LVAD risk that captures RV dysfunction. HMRS comprises variables that reflect extra-cardiac effects of right ventricular dysfunction, namely liver and renal dysfunction; the ability of HMRS to predict severe RV failure—which is a major contributor to post-implant mortality—likely explains the robust ability of HMRS to predict 90-day mortality. Separate from the ability of HMRS to predict death at 90 days, the ability of HMRS to predict severe RV failure supports its use in assessing LVAD candidacy as well as for intra-operative planning to support RV function.
There remains a dire lack of prospective data regarding the evaluation of predictors of severe RV failure after LVAD implantation. A recent systematic review and meta-analysis exhibited the wide variety of previously tested variables,7 all of which performed modestly. Of the four variables on which our study focuses, TAPSE was the only one represented, and it had been evaluated in a limited number of prior studies. HMRS, PAPi, and sRVCPI were not included in recent systematic review and meta-analysis. Inconsistent definitions of severe RV failure further limit use of existing studies for cross-comparison.6
Limitations
The results of this study must be interpreted in the context of some known limitations. Namely, this study was a single-center, retrospective analysis of a relatively small population. However, no prospective studies on this topic exist and advanced heart failure surgery, specifically LVAD implantation, is not yet a widely implemented therapy. The echo data were collected from multiple clinicians’ interpretations and not from a core- lab. While there is some inherent variability in this approach, it likely represents real world clinical experience. Notably, the majority of patients were supported by inotropes prior to LVAD implantation and thus, the results should be interpreted in that context. Lastly, the statistical methods for assessing predictive models remain imperfect. In attempts to address this we used both common and advanced statistical methods in our comparisons.
In summary, this study adds to the existing literature in supporting the use of HMRS to risk-stratify potential LVAD patients and reaffirms the continued need for a large, prospective study with comprehensive assessment of the risk of severe RV failure prior to LVAD implantation. Simple, noninvasive measures appear to perform as well as invasive measures in the prediction of severe RV failure, setting a higher bar for invasive or complex predictors in futures studies.
Acknowledgments
Sources of Funding: This study was supported in part by research funds from the National Institutes of Health (Grant No. U10 HL110309, Heart Failure Network), Clinical and Translational Science Award (Grant No. UL1 TR000448), and the Barnes Jewish Hospital Foundation.
Footnotes
Conflicts of Interest: All authors declare no conflicts of interest related to this study.
References
- 1.Kirklin JK, Naftel DC, Pagani FD, et al. Sixth INTERMACS annual report: a 10,000-patient database. J Hear Lung Transpl. 2014;33:555–564. doi: 10.1016/j.healun.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 2.Miller LW, Pagani FD, Russell SD, et al. Use of a Continuous-Flow Device in Patients Awaiting Heart Transplantation. N Engl J Med. 2007;357:885–896. doi: 10.1056/NEJMoa067758. [DOI] [PubMed] [Google Scholar]
- 3.Slaughter MS, Rogers JG, Milano CA, et al. Advanced Heart Failure Treated with Continuous-Flow Left Ventricular Assist Device. N Engl J Med. 2009;361:2241–2251. doi: 10.1056/NEJMoa0909938. [DOI] [PubMed] [Google Scholar]
- 4.Rogers JG, Aaronson KD, Boyle AJ, et al. Continuous flow left ventricular assist device improves functional capacity and quality of life of advanced heart failure patients. J Am Coll Cardiol. 2010;55:1826–34. doi: 10.1016/j.jacc.2009.12.052. [DOI] [PubMed] [Google Scholar]
- 5.Hayek S, Sims DB, Markham DW, Butler J, Kalogeropoulos AP. Assessment of right ventricular function in left ventricular assist device candidates. Circ Cardiovasc Imaging. 2014;7:379–89. doi: 10.1161/CIRCIMAGING.113.001127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LaRue SJ, Raymer DS, Pierce BR, Nassif ME, Sparrow CT, Vader JM. Clinical outcomes associated with INTERMACS-defined right heart failure after left ventricular assist device implantation. J Hear Lung Transplant. 2017;36:475–477. doi: 10.1016/j.healun.2016.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellavia D, Iacovoni A, Scardulla C, et al. Prediction of right ventricular failure after ventricular assist device implant: systematic review and meta-analysis of observational studies. Eur J Heart Fail. 2017 doi: 10.1002/ejhf.733. [DOI] [PubMed] [Google Scholar]
- 8.Drakos SG, Janicki L, Horne BD, et al. Risk factors predictive of right ventricular failure after left ventricular assist device implantation. Am J Cardiol. 2010;105:1030–1035. doi: 10.1016/j.amjcard.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 9.Kormos RL, Teuteberg JJ, Pagani FD, et al. Right ventricular failure in patients with the HeartMate II continuous-flow left ventricular assist device: incidence, risk factors, and effect on outcomes. J Thorac Cardiovasc Surg. 2010;139:1316–1324. doi: 10.1016/j.jtcvs.2009.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Sparrow CT, Nassif ME, Raymer DS, Novak E, LaRue SJ, Schilling JD. Pre-Operative Right Ventricular Dysfunction Is Associated With Gastrointestinal Bleeding in Patients Supported With Continuous-Flow Left Ventricular Assist Devices. JACC Heart Fail. 2015;3:956–64. doi: 10.1016/j.jchf.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Fitzpatrick JR, Frederick JR, Hiesinger W, et al. Early planned institution of biventricular mechanical circulatory support results in improved outcomes compared with delayed conversion of a left ventricular assist device to a biventricular assist device. J Thorac Cardiovasc Surg. 2009;137:971–7. doi: 10.1016/j.jtcvs.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalogeropoulos AP, Kelkar A, Weinberger JF, et al. Validation of clinical scores for right ventricular failure prediction after implantation of continuous-flow left ventricular assist devices. J Hear Lung Transpl. 2015 doi: 10.1016/j.healun.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Frea S, Bovolo V, Bergerone S, et al. Echocardiographic evaluation of right ventricular stroke work index in advanced heart failure: a new index? J Card Fail. 2012;18:886–893. doi: 10.1016/j.cardfail.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 14.Frea S, Pidello S, Bovolo V, et al. Prognostic incremental role of right ventricular function in acute decompensation of advanced chronic heart failure. Eur J Heart Fail. 2016;18:564–72. doi: 10.1002/ejhf.504. [DOI] [PubMed] [Google Scholar]
- 15.Kang G, Ha R, Banerjee D. Pulmonary artery pulsatility index predicts right ventricular failure after left ventricular assist device implantation. J Hear Lung Transplant. 2016;35:67–73. doi: 10.1016/j.healun.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Morine KJ, Kiernan MS, Pham DT, Paruchuri V, Denofrio D, Kapur NK. Pulmonary Artery Pulsatility Index Is Associated With Right Ventricular Failure After Left Ventricular Assist Device Surgery. J Card Fail. 2016;22:110–116. doi: 10.1016/j.cardfail.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 17.Adamo L, Nassif M, Tibrewala A, et al. The Heartmate Risk Score predicts morbidity and mortality in unselected left ventricular assist device recipients and risk stratifies INTERMACS class 1 patients. JACC Hear Fail. 2015;3:283–290. doi: 10.1016/j.jchf.2014.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adamo L, Tang Y, Nassif ME, et al. The HeartMate Risk Score Identifies Patients With Similar Mortality Risk Across All INTERMACS Profiles in a Large Multicenter Analysis. JACC Hear Fail. 2016;4:950–958. doi: 10.1016/j.jchf.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Cowger J, Sundareswaran K, Rogers JG, et al. Predicting survival in patients receiving continuous flow left ventricular assist devices: the HeartMate II risk score. J Am Coll Cardiol. 2013;61:313–21. doi: 10.1016/j.jacc.2012.09.055. [DOI] [PubMed] [Google Scholar]
- 20.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 21.Pencina MJ, D’Agostino RB, Sr, D’Agostino RB, Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:112–157. doi: 10.1002/sim.2929. [DOI] [PubMed] [Google Scholar]
- 22.Guazzi M, Bandera F, Pelissero G, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Hear Circ Physiol. 2013;305:H1373–81. doi: 10.1152/ajpheart.00157.2013. [DOI] [PubMed] [Google Scholar]