Abstract
Background and Objectives:
Rates of morbid obesity are skyrocketing worldwide. Not only bariatric surgeons, but also general surgeons are often operating on morbidly obese patients. Many general surgeons still use the same anatomic landmarks for patients with body mass index (BMI) over 35 mg/kg2 as they do for patients of normal weight and can therefore find accessing the morbidly obese abdominal organs difficult. This paper will describe a technique that is easily reproducible and applicable in a wide range of laparoscopic cases.
Method:
The xiphoid process is the only landmark referenced. From the xiphoid process, the surgeon puts 2 fists together and places the first trocar inferiorly 2 cm lateral to the midline in either direction. The umbilicus is not used as a landmark. This placement is 15–18 cm inferior to the xiphoid process, but allows adequate visualization for any foregut case. An optical trocar is used.
Results:
In over 1400 bariatric cases, the initial trocar was safely placed with this technique. Most of these cases were performed with the method, but some had one modification: the first trocar was placed in the midclavicular line in the subcostal area if there were previous midline scars. In no cases was an extra-long, or bariatric, trocar used.
Conclusions:
Laparoscopic access in morbidly obese patients does not have to be difficult. Using an optical trocar off the midline 15–18 cm below the xiphoid process will provide reliable, safe access in the morbidly obese patient, with excellent visualization of the target anatomy.
Keywords: Abdominal wall access, Bariatric surgery, Extra-long trocar, Trocar injury
INTRODUCTION
Rates of morbid obesity are skyrocketing worldwide.1 Not only bariatric surgeons, but also general surgeons frequently operate on patients who are morbidly obese. Many general surgeons still use the same anatomic landmarks for patients with BMIs over 35 kg/m2 as they do for patients of normal weight, leading to difficult access through the morbidly obese abdominal wall during a procedure as common as a laparoscopic cholecystectomy. Many general surgeons find that they need to use long trocars and struggle with the abdominal wall. A literature search was performed regarding access techniques, but most of the literature discusses complication rates secondary to entry and does not specifically address port placement.2
Most general surgeons have probably been in a situation in which there is a lack of good visualization because the camera port is too low in regard to the foregut. It is hard to relocate this port, as another trocar will clash with the trocar that is too low. The only good option is to remove the original trocar, but removal can lead to gas leak if the fascial defect stays open. Optimal placement from the start is the best way to prevent this problem. Proper camera port placement also obviates the need for long laparoscopes or trocars. This paper outlines a simple technique for initial trocar placement in the morbidly obese abdominal wall that is reliable, easily learned, and simply applied.
METHOD
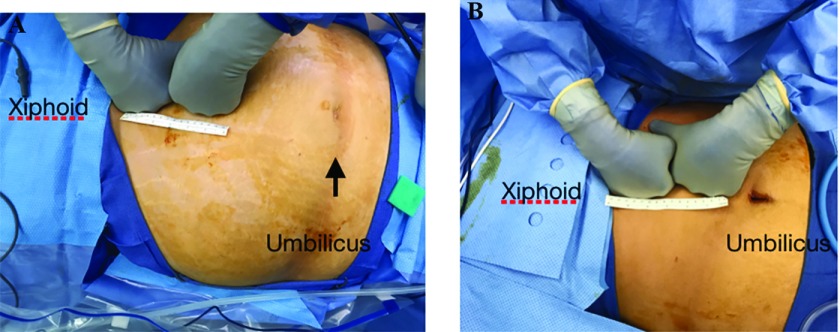
The patient is placed supine. This placement could include the French position (legs spread). This placement is best used for an optical trocar approach. The surgeon then measures the distance from the xiphoid process, as this is a fixed point. The measurement is performed by forming 2 fists, placing the hands side by side, with the starting point at the xiphoid process, and then moving 2–3 cm off the midline in either direction, depending on the operation. On average, this point will be anywhere from 15–18 cm inferior to the xiphoid process (Figure 1). In case of a surgeon with very large or very small hands, the 15-cm ruler that is in most operative kits can be used. The umbilicus is variable based on BMI, body habitus, and height and therefore should not be used as a landmark for port placement. With this technique, the camera port is nearly always appropriately located for foregut surgery. The surgeon must also remember that if there are midline scars or incisions, a lateral approach is safer for the initial trocar placement, usually safely performed in the midclavicular line immediately subcostal on the left or right side, unless an open cholecystectomy had been performed earlier.
Figure 1.
(A) Morbidly obese abdominal wall. (B) Nonobese abdominal wall. The ruler is 15 cm. Note the distance from the inferior fist to the umbilicus in the obese versus the nonobese patient.
RESULTS
More than 1400 bariatric operations were performed with this technique. The procedures included lap band placement, laparoscopic gastric bypass, and laparoscopic sleeve gastrectomy, as well as revisional bariatric surgery. Secondary to previous surgeries, the initial trocar was occasionally placed in the subcostal area but the majority (>98%) were placed with the described technique. There were no instances of bowel or vascular injury, and no cases required an extra-long laparoscope or trocars.
DISCUSSION
The surgical literature has a surprising dearth of publications dealing with positioning the first trocar to penetrate the obese abdominal wall. Most surgeons adopt their access techniques while in training and stay with the way they were taught initially. Surgeons should always be open to improvements in technique, and if there is a safe, reliable method, it should be adopted. The intent of this paper was not to champion an optical trocar over any other entry method, but instead to discuss ease of placement of the camera port for bariatric or foregut surgery.
The first step in any laparoscopic operation is trocar placement for access through the abdominal wall. For its being a necessary part of all laparoscopic procedures, the process is surprisingly dangerous. In fact, 25% of all injuries that occur in laparoscopic surgery are during initial port placement.3,4 Wind et al5 studied medicolegal claims in the Netherlands, and trocar injuries accounted for 20% of all claims regarding laparoscopic surgery. A recent review of litigated cases involving direct trocar insertion injury was recently published by Vilos et al.6 The court cases showed that vascular injuries were detected sooner, but bowel injuries were delayed 2 to 3 days.
There are 3 established techniques that may be used: Veress needle, direct insertion; an open approach (Hasson technique); or an optical trocar.7,8 The Veress needle technique usually leads to a higher risk of vascular injury, and the open technique is usually associated with bowel injury. According to a Cochrane Review, the Veress needle has a higher rate of vascular injury and also a higher failure rate of establishment of pneumoperitoneum compared with the direct-entry technique.9 The debate over which is safer has persisted for years and both are generally accepted as equally safe.4,10–13 Optical trocars are also considered safe and have been widely adopted.14
Morbidly obese patients can pose special challenges for abdominal access, secondary to the thickness of the abdominal wall, body habitus, and lack of reliable landmarks. Sundbom and Ottoson15 used the Scandinavian Obesity Surgery Registry to compare the Veress, optical trocar, and Hasson techniques and found no difference in injury between the Veress and optical trocar (injury rate for both techniques of 0.08%) with no injuries in the Hasson group.15 The location of the initial trocar placement was not recorded in this database. Optical trocars have been shown to be safe in bariatric patients in other studies. Rosenthal et al16 reported the use of the optical trocar in 849 patients, with no injuries. The initial placement was supraumbilical, and 5 cases were converted to open because of lack of long enough instruments.
The umbilicus should be considered an unreliable landmark in the obese patient. The xiphoid process is a fixed landmark that does not vary with central obesity or BMI. Katkhouda et al17 studied port placement in morbidly obese patients. The landmarks they used were the xiphoid process and the umbilicus. The initial camera port was at the umbilicus. The distance between both points was measured and, if the distance was greater than 25 cm, then additional ports for camera and instrument were placed closer to the xiphoid process.17 Tinelli et al18 specifically looked at initial trocar placement in morbidly obese females. The surgeons entered with an optical trocar through the umbilicus and found a slightly reduced risk of bleeding and bowel injury. These studies essentially stand alone, as my literature search did not find any other publications addressing initial trocar placement in the morbidly obese patient.
Besides occasional serious complications, suboptimal trocar placement can lead to frustration secondary to poor visualization, with longer operative times and potential complications. If a longer laparoscope is available, it can help overcome poor placement, although a longer laparoscope may not be immediately available to many surgeons. This method can lead to placement of additional trocars.
This paper has the usual limitations that any paper based on personal experience has, but this small modification in technique can easily be tried by any practicing surgeon and adopted or discarded as needed. For surgeons operating on patients with small or large hands, measuring 15 cm from the xiphoid process would work. The surgeon who finds the placement to be suboptimal can either leave the trocar in place and pull it out slightly or remove it and close the fascial defect with a laparoscopic suture passer. Surgeons should never hesitate in placing additional ports if it would make the operation safer.
As with any surgical procedure, laparoscopic access should prove safe before any other consideration. An injury during access is dangerous to the patient and frustrating to the surgeon. It usually starts the procedure off in a manner not conducive to a calm, smooth completion and may actually cause the surgery to be cancelled. If the placement is not optimal, it can lead to poor visualization, frustration, and even poor outcomes. The technique described can be used to provide safe and reliable access and visualization.
CONCLUSIONS
Laparoscopic access in morbidly obese patients does not have to be difficult. Use of an optical trocar off the midline 15–18 cm below the xiphoid process will provide reliable, safe access in the morbidly obese patient, with excellent visualization of the target anatomy.
References:
- 1. Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief. 2015;219 Available at: https://www.cdc.gov/nchs/data/databriefs/db219.pdf/ Accessed November 22, 2017. [PubMed] [Google Scholar]
- 2. Bhoyrul S, Vierra MA, Nezhat CR, Krummel TM, Way LW. Trocar injuries in laparoscopic surgery. J Am Coll Surg. 2001;192:677–683. [DOI] [PubMed] [Google Scholar]
- 3. Chapron CM, Pierre F, Lacroix S, Querleu D, Lansac J, Dubuisson JB. Major vascular injuries during gynecologic laparoscopy. J Am Coll Surg. 1997;185:461–465. [PubMed] [Google Scholar]
- 4. Jansen FW, Kolkman W, Bakkum EA, de Kroon CD, Trimbos-Trimbos JB. Complications of laparoscopy: an inquiry about closed versus open-entry technique. Am J Obstet Gynecol. 2004;190:634–638. [DOI] [PubMed] [Google Scholar]
- 5. Wind J, Cremers JE, van Berge Henegouwen MI, Gouma DJ, Jansen F, Bemelman WA. Medical liability insurance claims on entry-related complications in laparoscopy. Surg Endosc. 2007;21:2094–2099. [DOI] [PubMed] [Google Scholar]
- 6. Vilos GA, Ternamian A, Vilos AG, Abu-Rafea B, Zhu C. Direct laparoscopic trocar insertion: lessons learned from nine litigated cases. J Minim Invasive Gynecol. 2017;24:960–970. [DOI] [PubMed] [Google Scholar]
- 7. Kassir R, Blanc P, Lointier P, et al. Laparoscopic entry techniques in obese patient: Veress needle, direct trocar insertion or open entry technique? Obes Surg. 2014;24:2193–2194. [DOI] [PubMed] [Google Scholar]
- 8. Lal P, Vindal A, Sharma R, Chander J, Ramteke VK. Safety of open technique for first-trocar placement in laparoscopic surgery: a series of 6,000 cases. Surg Endosc. 2012;26:182–188. [DOI] [PubMed] [Google Scholar]
- 9. Ahmad F, O'Flynn H, Duffy JM, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev. 2012;2:CD006583. [DOI] [PubMed] [Google Scholar]
- 10. Ertugrul I, Kayaalp C, Yagci MA, Sumer F, Karagul S, Tolan K. Comparison of direct trocar entry and Veress needle entry in laparoscopic bariatric surgery: randomized controlled trial. J Laparoendosc Adv Surg Tech A. 2015;25:875–879. [DOI] [PubMed] [Google Scholar]
- 11. Schäfer M, Lauper M, Krähenbähl L. Trocar and Veress needle injuries during laparoscopy. Surg Endosc. 2001;15:275–280. [DOI] [PubMed] [Google Scholar]
- 12. Mober AC, Montgomery A. Primary access-related complications with laparoscopy: comparison of blind and open techniques. Surg Endosc. 2005;19:1196–1199. [DOI] [PubMed] [Google Scholar]
- 13. Jaing X, Anderson C, Schnatz P. The safety of direct trocar versus Veress needle for laparoscopic entry: a meta-analysis of randomized clinical trials. J Laparoendoscopic Adv Surg Tech A. 2012;22:362–370. [DOI] [PubMed] [Google Scholar]
- 14. Loureiro M, Ramadan M, Skalli EM, Blanc P, Fabre JM, Nocca D. A multicentric prospective study evaluating the safety and efficacy of Kii® Fios® First Entry Trocar in laparoscopic bariatric surgery. Surg Endosc. 2017;31:4680–4687. [DOI] [PubMed] [Google Scholar]
- 15. Sundbom M, Ottoson J. Trocar injuries in 17,446 laparoscopic gastric bypass: a nationwide survey from the Scandinavian Obesity Surgery Registry. Obes Surg. 2016;26:2127–2130. [DOI] [PubMed] [Google Scholar]
- 16. Rosenthal RJ, Szomstein S, Kennedy CI, Zundel N. Direct visual insertion of primary trocar and avoidance of fascial closure with laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2007;21:124–128. [DOI] [PubMed] [Google Scholar]
- 17. Katkhouda N, Moazzez A, Popek S, et al. A new and standardized approach for trocar placement in laparoscopic Roux-en-Y gastric bypass. Surg Endosc. 2009;23:659–662. [DOI] [PubMed] [Google Scholar]
- 18. Tinelli A, Malvasi A, Mynbaev O, et al. Bladeless direct optical trocar insertion in laparoscopic procedures on the obese patient. JSLS. 2013;17:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]