Obesity and depression represent two distinct disease states that commonly occur during adolescence. Childhood obesity confers risk for a number of negative psychosocial outcomes relative to healthy weight individuals, including significant reductions in health-related quality of life, poorer self-concept, and behavioral difficulties (e.g., Griffiths, Parsons, & Hill, 2010).
Cross-sectional studies indicate high rates of co-occurrence in adolescents seeking weight control treatment (Zametkin, Zoon, Klein, & Munson, 2004). Positive associations between overweight/obesity and depressed mood have also been observed in community samples of both predominantly Caucasian (Crow, Eisenberg, Story, & Neumark-Sztainer, 2006) and predominantly African American adolescents (Witherspoon, Latta, Want, & Black, 2013). Prospective studies (e.g., Boutelle, Hannan, Fulkerson, Crow, & Stice, 2010) indicate that obese adolescent girls are at greater risk for developing depressive symptoms later in adolescence than non-obese peers. There is even stronger evidence to support the relationship between adolescent depression and subsequent weight gain or onset of obesity, with six of eight longitudinal studies documenting a positive relationship (Korczak, Lipman, Morrison, Duku & Szatmari, 2013).
Major Depressive Disorder (MDD) is a common, often recurrent condition, with a lifetime prevalence of 11.7% by age 18 (Merikangas et al., 2010). Individual cognitive-behavioral therapy (CBT) has been deemed a “probably efficacious” treatment for adolescent depression based on a meta-analysis of 19 studies (David-Ferndon & Kaslow, 2008). Physical activity is the first recommendation for mild to moderate depression in Great Britain (NCCMH, 2005) and is often given for ‘homework’ in CBT as part of behavioral activation (McCauley et al., 2015). A recent review (Brown, Pearson, Braithwaite, Brown, & Biddle, 2013) indicated that across nine intervention studies examining the effects of physical activity on depressive symptoms, there was a small effect of physical activity on depressive symptoms. Effective weight control interventions for adolescents include physical activity as well as dietary recommendations with behavioral strategies, such as self-monitoring, goal setting, problem solving, and relapse prevention (Jelalian et al., 2010), that are common to CBT protocols for depression.
The purpose of the current study was to test the feasibility of a novel intervention that integrated healthy lifestyle enhancement and CBT in a clinical sample of depressed, overweight/obese adolescents. It was hypothesized that adolescents randomized to this integrated treatment (CBT-Healthy Lifestyles; CBT-HL) would demonstrate greater reductions in depressive symptoms as well as weight loss over the course of treatment and at follow-up compared to adolescents randomized to CBT for depression alone (CBT).
Method
Participants
Participants (n = 33) met the following inclusion criteria: (a) 12–18 years old, inclusive, (b) DSM-IV criteria for Current Major Depressive Episode (MDE) or Dysthymia, (c) a Clinical Depression Severity Rating Scale (CDRS) score of 65 or greater, (d) a body mass index (BMI) greater than 25 or BMI percentile ≥ 85th percentile for sex and age; and e) a parent or caregiver willing to participate. Participants were excluded if they met criteria for bipolar disorder or psychosis, or if they were on medications that were known to impact weight status, such as antipsychotics. In addition, participants taking an SSRI or stimulant were required to be on a stable dose of the medication for a minimum of 3 months.
Procedure
Participants were referred by mental health professionals, pediatricians and schools. Interested families were told the study was for depressed teens who were also overweight. Informed written parental consent and adolescent assent were obtained from 55 participant families. Of these, 33 met the inclusion/exclusion criteria and were randomized to receive either CBT-HL or CBT. This study was approved by the university and institutional IRB.
Research evaluations were conducted at baseline (pre-randomization), 12 weeks (mid-treatment), 24 weeks (end of treatment), and 48 weeks (6 months after the end of treatment). Participant condition was masked for raters. Both the teen and a parent/guardian were compensated for completing the research assessments. Following the baseline assessment, stratified randomization was conducted with an urn randomization computer program using a 2:1 randomization schedule in favor of CBT-HL. Study staff was masked to allocation sequence until interventions were assigned. Randomization was stratified on the basis of adolescent score greater than 4 on the Clinical Global Impairment-Severity of Illness rating (CGI-SOI; Guy, 1976), a one-item clinician-rated scale with ratings from 1 ‘normal, not impaired’ to 7 ‘very seriously impaired’. The project coordinator was responsible for enrolling participants and notifying families of treatment assignment.
Treatment Conditions.
Adolescents randomized to both treatment conditions received an individual CBT protocol for adolescent depression. Sessions in the acute phase (weeks 1– 12) were conducted weekly and every other week in the maintenance phase (weeks 13– 24), resulting in a total of 18 sessions. Sessions in both phases were approximately 60 minutes long. The adolescent CBT protocol was based on protocols used in prior clinical trials with depressed adolescents including two large multisite trials, TADS (March et al., 2004) and TORDIA (Brent et al. 2008), as well as a previous smaller trial by the research team (Esposito-Smythers, Spirito, Kahler, Hunt, & Monti, 2011). Core skills included Problem Solving, Cognitive Restructuring, Affect Regulation, and Behavioral Activation. Based on the adolescent’s needs, these skills were then repeated or additional modules were introduced (e.g. Family Problem Solving, Family Communication). Each session included common elements such as identifying an agenda item that would be discussed in the session, reviewing homework from the prior session, skill review or teaching of a new skill, skill practice, and addressing the patient-generated agenda item using CBT skills. Adolescents were assigned a personalized “homework” assignment at the end of the session to facilitate practice of a particular CBT skill. Two adolescents in the CBT condition included exercise (i.e. jogging and taking walks) as part of their behavioral activation plan but actual participation rates of exercise were not recorded.
For adolescents assigned to CBT-HL, the core modules for depression (described above) were enhanced to include attention to diet and physical activity as well as the relationship between depressed mood, weight, and physical activity. In addition, the CBT-HL protocol included specific content on Body Image and Coping with Food Cravings (Jelalian et al., 2015). A nutritionist was available to meet with the teen individually up to four times. Nutrition visits were followed by a check-in with the parent to review recommendations. Weekly 60-minute group aerobic exercise sessions were required and facilitated by a physical therapist.
Training and Fidelity.
Therapists were trained through didactic instruction, tape reviews, and role-plays. All sessions were videotaped. All videos for the first two participants treated by each therapist and a random selection of 20% of subsequent videos were rated on the Cognitive Therapy Rating Scale (CTRS; Young & Beck, 1980) and adherence checklists for each module, which were adapted from a prior clinical trial (Esposito-Smythers et al., 2011). On the CTRS, 97.4% of sessions in both conditions coded received scores of 44 or higher, indicating a high level of therapist competence (Brent et al., 2008); 93.7% of sessions met the minimum threshold of adherence to at least 80% of session content. The intraclass correlation between primary and secondary coders on the CTRS was .60. This figure reflects coding of 11 observations, which may have led to underestimate of agreement.
Measures
Anthropometrics.
Weight was measured on a digital scale (Seca 869) with participants wearing light clothing and no shoes. Height was measured on a wall-mounted stadiometer. BMI was calculated as kg/m2.
Physical Activity.
The SenseWear Mini (MINI; Body Media Inc) monitor was used to provide estimates of daily energy expenditure, exercise duration, and exercise intensity for seven days during each of the three assessment periods. Previous studies using both indirect calorimetry (Calabro, Welk, & Eisenmann, 2009) and doubly labeled water (Calabro, Stewart, & Welk, 2013) support the validity of the MINI in measuring physical activity in pediatric populations. Data were used if participants wore the armband for at least 6 hours for 3 consecutive days. Adherence rates were as follows: Baseline, CBT-HL (79%), CBT (89%); Week 12, CBT-HL (63%), CBT (75%); and Weeks 24 and 48, CBT-HL (47%), CBT (63%).
Depressive Symptoms.
The Beck Depression Inventory II (BDI-II; Beck, 1996), a commonly used measure with adolescents, was used to measure depressive symptoms at each time point. Internal consistency for this sample was excellent for adolescents across time points (Cronbach’s α range = .92 - .95).
The Children’s Depressive Rating Scale (CDRS; Poznanski, Freeman, & Mokros, 1984) is a 17-item clinician-rated measure of depression symptoms. Internal consistency across baseline and follow-up assessments for the current sample was adequate (α = .83 - .88). The intraclass correlation between first and second raters on the CDRS was adequate (ICC=.77).
The Kiddie Schedule for Affective Disorders and Schizophrenia-Present Version (K-SADS-P; Kaufman, Birmaher, Brent, & Rao, 1997) is a semi-structured diagnostic interview with excellent psychometric properties that was used to diagnose a mood disorder. A clinician interviewed the participating parent and adolescent regarding the adolescent’s symptoms and functioning. Adolescent diagnoses were determined by consensus of a third clinician. KSADS depression diagnoses were 100% concordant between first and second raters.
Treatment Feasibility/Acceptability.
The number of CBT and exercise sessions attended was examined as a measure of feasibility and acceptability. The Session Evaluation Form (SEF; Harper, Contreras, Bangi, & Pedraza, 2003) was given to adolescents at the end of each therapy session with questions about the usefulness of the session rated on a four-point Likert scale from “strongly agree” to “strongly disagree”.
Statistical Analysis
Data for the BDI and BMI were analyzed using linear growth curve modeling (Singer & Willett, 2003). The analysis model allows for individually varying intercepts and linear slopes for the regression of BMI and BDI over time. Model parameters were estimated using a generalized linear random effects growth curve model using Mplus software (version 7.3, Muthén & Muthén, Los Angeles, CA). This approach uses a maximum likelihood parameter estimation algorithm that allows for the inclusion of individually varying time points of observation and the inclusion of all observations under the assumption that data that are missing are missing at random conditional on the other variables in the model, consistent with the intent-to-treat principle. The effect of treatment as modeled with a dummy variable identifying the comparison condition (CBT) while the experimental condition (CBT-HL) was used as the reference group. This choice was driven by the larger size of the CBT-HL group. Because this was a pilot study and not powered to detect a significant treatment effect, the power to detect a half standard deviation effect size with a type-I error of 5% was low, 22%. Ten assessments of measured height were affected by measurement error secondary to relocation of the stadiometer. These observations were distributed across both conditions. Analyses using BMI data are reported using last height observation carried forward for these ten cases.
Data on MVPA were analyzed using piecewise univariate and bivariate linear latent growth curve models (Neter, Kutner, Nachtsheim, & Wasserman, 1996) with a time trend capturing change in MVPA at the close of the active treatment phase (12 weeks) and a second time trend capturing change from 12 weeks through the last follow-up (48 weeks).Time steps were modeled with uniform spacing matching the study design and coded so that the end of the phase (12 weeks or 48 weeks) assumed unit values. Model parameters were estimated using a generalized linear random effects growth curve model using Mplus software (version 7.11, Muthén & Muthén, Los Angeles, CA). This approach uses a maximum likelihood parameter estimation algorithm that allows for the inclusion of individually varying time points of observation and the inclusion of all observations under the assumption that data that are missing are missing at random conditional on the other variables in the model, consistent with the intent-to-treat principle. The effect of CBT-HL was modeled using a dummy variable capturing group assignment. Because of the small sample size, as a sensitivity analysis we repeated the assessment of significance levels using permutation tests (Hesterberg, Monaghan, Moore, Clipson, & Epstein, 2005). That is, after obtaining point estimates for observed effects, we repeatedly randomly assigned participants to CBT-HL and CBT groups and obtained a sampling distribution for effects of interest under the null hypothesis, and obtained a direct estimate of the p-value (the percentile rank) of the observed statistic by comparing to this empirical distribution. Because this was a pilot study and not powered to detect a significant treatment effect, the power to detect a half standard deviation effect size with a type-I error of 5% was low, 22%.
Results
The sample was recruited from an urban/suburban community in the Northeast between June of 2010 and December of 2012 and the final assessment occurred in November 2013. There were no significant differences between the conditions on baseline characteristics (see Table 1).
Table 1.
Baseline Sociodemographic, Weight, Mood Characteristics and Treatment Characteristics of Sample by Condition
| Total Sample (n = 33) |
CBT-HL (n = 24) |
CBT (n = 9) |
t-value | χ2-value | p-value | ||
|---|---|---|---|---|---|---|---|
| Demographic Variables | |||||||
| M (SD) | % (n) | M (SD) | % (n) | ||||
| Child (Female) | 70.8 (17) | 77.8 (7) | .16 | .69 | |||
| Child Age (SD) | 15.25 (1.51) | 14.44 (1.67) | 1.33 | .19 | |||
| Parent Age | 44.29 (7.29) | 40.33 (4.69) | 1.51 | .14 | |||
| Parent (Mother) | 83.3 (20) | 88.9 (8) | .16 | .69 | |||
| Child Latino | 33.3 (8) | 33.3 (3) | 0.0 | 1.0 | |||
| Child Minority Race | 58.3 (14) | 44.4 (4) | .51 | .48 | |||
| Parent Latino | 21.7 (5) | 28.6 (2) | .14 | .71 | |||
| Parent Minority Race | 29.2 (7) | 11.1 (1) | 1.16 | .28 | |||
| Parent Education | 5.16 | .08+ | |||||
| < High School | 17.4 (4) | 0 (0) | |||||
| High School | 47.8 (11) | 22.2 (2) | |||||
| > High School | 34.8 (8) | 77.8 (7) | |||||
| Household income | |||||||
| < 5,000 | 4.2 (1) | 11.1 (1) | 3.55 | .90 | |||
| 5,000 – 9,999 | 16.7 (4) | 11.1 (1) | |||||
| 10,000 – 14,999 | 4.2 (1) | 0 (0) | |||||
| 15,000 – 25,999 | 16.7 (4) | 22.2 (2) | |||||
| 26,000 – 49,999 | 20.8 (5) | 11.1 (1) | |||||
| 50,000 – 74,999 | 20.8 (5) | 33.3 (3) | |||||
| 75,000 – 99,999 | 8.3 (2) | 0 (0) | |||||
| 10,000 – 149,000 | 4.2 (1) | 11.1 (1) | |||||
| Weight Variables | |||||||
| Child Weight | 223.63 (54.74) | 220.64 (28.21) | .20 | .84 | |||
| Parent Weight | 195.56 (45.46) | 185.42 (39.22) | .59 | .56 | |||
| Depression Variables | |||||||
| Parent BDI | 10.98 (6.90) | 8.22 (7.33) | 1.0 | .32 | |||
| Child CDRS T-Score | 72.34 (8.87) | 73.39 (6.45) | .32 | .75 | |||
| Child KSADS | .39 | .53 | |||||
| MDD | 95.8 (23) | 100 (9) | |||||
| Dysthymia Only | 4.2 (1) | 0 (0) | |||||
| CGI Severity - Impairment | .68 | .88 | |||||
| Normal | 0 (0) | 0 (0) | |||||
| Minimal | 0 (0) | 0 (0) | |||||
| Mild | 4.2 (1) | 0 (0) | |||||
| Moderate | 37.5 (9) | 44.4 (4) | |||||
| Marked | 41.7 (10) | 33.3 (3) | |||||
| Severe | 16.7 (4) | 22.2 (2) | |||||
| Very Serious | 0 (0) | 0 (0) | |||||
| Treatment Variables | |||||||
| Completed CBT Treatment | 75.0 (18) | 100 (9) | 2.75 | .10 | |||
| CBT Session Attendance | 14.0 (6.05) | 16.78 (.97) | 2.18 | .04* | |||
| Exercise Attendance | 8.81 (6.88) | N/A | |||||
| Exercise Attendance | 0 – 4 5 – 1 12 + |
33 (8) 16.7 (4) 41.7 (10) |
N/A | ||||
| SEF # 2 Application | |||||||
| Parent | 90.5 (19) | 100 (8) | .82 | .37 | |||
| Adolescent | 75 (18) | 77.8 (7) | .03 | .87 | |||
| SEF # 7 Relevant | |||||||
| Parent | 100 (21) | 100 (8) | 0.0 | 1.0 | |||
| Adolescent | 83.3 (20) | 100 (9) | 1.71 | .19 | |||
| SEF # 10 Comfortable | |||||||
| Parent | 90.5 (19) | 87.5 (7) | .06 | .81 | |||
| Adolescent | 62.5 (15) | 88.9 (8) | 2.16 | .14 | |||
| SEF # 11 Helpful | |||||||
| Parent | 95.2 (10) | 87.5 (7) | .54 | .46 | |||
| Adolescent | 70.8 (17) | 88.9 (8) | 1.16 | .28 | |||
M indicates mean. SD indicates standard deviation. N/A indicates that exercise attendance was not applicable for the CBT group. SEF refers to the Session Evaluation Form completed during active treatment (Sessions 1 – 12) and % that endorsed the item across all sessions as agree or strongly agree. Item 2 – ‘I will be able to apply what I learned from this session in my life’, Item 7 – ‘The topic of this session was relevant to my life’, Item 10 ‘I felt comfortable participating in this session’, and Item 11 ‘This session was helpful to me’. Numbers in parentheses vary because some parents and some adolescents did not complete session forms.
The first two CBT-HL participants were missing exercise attendance data.
p < .05,
p < .10
Treatment Acceptability/Feasibility
Adolescents in the CBT condition attended significantly more CBT therapy sessions than those in CBT-HL (see Table 1). Those in CBT-HL attended, on average, about 9 sessions of exercise, and exercise attendance correlated positively with CBT session attendance (r=.75, p<.001). Of adolescents in CBT-HL, average exercise attendance was significantly higher for those who completed depression treatment (M=11.53, SD=6.21) compared to those who did not (M = 2.0, SD = 1.90; t(19.73) = 5.73, p < .001). On average, participants in CBT-HL attended approximately two nutrition sessions (M=1.97, SD=1.02), with a range of 0–4 visits. Only two participants did not attend any nutrition sessions.
Changes in Mood
Table 2 illustrates that BDI scores declined from the clinical to non-clinical range in both treatment conditions by the end of treatment, and remained in the non-clinical range throughout follow-up. With respect to change in depressed mood (BDI; Table 3), the model-implied baseline BDI score was 17. The experimental group (CBT-HL) is expected to show a reduction of about 11.6 BDI points over the period of a year. However, the comparison condition (CBT) is expected to show greater decline change (11.6 + 6.5) or 18.1 BDI points. For both conditions, their expected BDI score is in a range indicative of mild symptoms of depressed mood. That difference expressed as a fraction of the pooled baseline standard deviation (the standardized effect size) of BDI is d = 0.57, with a 95% confidence interval of −0.15 to 1.28. However, given the small sample size, this difference in slope was not statistically significant, χ2 (1) = 2.3, p = .13.
Table 2.
Group Differences for Measures of BMI and Depressed Mood (Beck Depression Inventory) at Baseline, 12, 24, and 48-Week Assessments for Completers
| Baseline | 12 Weeks | 24 Weeks | 48 Weeks | |||||
|---|---|---|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | N | M (SD) | n | M (SD) | |
| Depressed Mood (BDI) | ||||||||
| CBT | 9 | 25.0 (12.0) | 9 | 7.0 (5.9) | 8 | 6.9 (7.5) | 8 | 6.0 (5.6) |
| CBT-HL | 24 | 22.0 (11.0) | 21 | 9.3 (12.7) | 20 | 9.0 (10.9) | 18 | 10.3 (14.4) |
| Total | 33 | 22.6 (11.4) | 30 | 8.6 (11.0) | 28 | 8.3 (9.9) | 26 | 9.0 (12.4) |
| BMI (kg/m2)* | ||||||||
| CBT | 9 | 37.6 (4.3) | 8 | 37.9 (4.9) | 8 | 38.4 (5.3) | 7 | 39.3 (5.9) |
| CBT-HL | 24 | 36.8 (7.9) | 21 | 36.9 (8.2) | 19 | 36.1 (7.5) | 17 | 35.8 (5.9) |
| Total | 33 | 37.0 (7.0) | 29 | 37.2 (7.3) | 27 | 36.8 (6.9) | 24 | 36.8 (6.8) |
BMI calculated with last observation carried forward for height for ten observations impacted by instrument error.
Note: CBT = Cognitive-Behavioral Therapy for depression; CBT- HL= Cognitive-Behavioral Therapy plus Healthy Lifestyle enhancement. This table depicts unadjusted means and standard deviations of depression and weight among available data. Week 48 weight does not include two participants (one from CBT who developed purging behaviors during the follow-up and one from CBT-HL who underwent bariatric surgery)
Table 3.
Parameter Estimates for Linear Growth Curve Models for BDI and BMI Change over Time by Treatment Condition
| BDI | BMI | |
|---|---|---|
| Parameter | Est (SE) | Est (SE) |
| Baseline mean (CBT-HL) | 17.1 (2.0) | 36.61 (1.4) |
| CBT-HL change through end of follow-up | −11.6 (2.3) | 0.62 (0.8) |
| CBT difference in baseline mean from CBT-HL | 1.1 (3.7) | 1.1 (2.7) |
| CBT additional change through end of follow-up | −6.5 (4.2) | 1.5 (1.5) |
CBT = Cognitive-Behavioral Therapy for depression; CBT- HL= Cognitive-Behavioral Therapy plus Healthy Lifestyle enhancement; BDI = Beck Depression Inventory; BMI = Body Mass Index
Changes in Weight Status
Data regarding BMI are summarized in Table 2. Weight status was similarly distributed in CBT-HL and CBT groups at baseline. For BMI change (Table 3), the model-implied baseline BMI was 37. The experimental group (CBT-HL) is expected to remain essentially stable on BMI over the period of a year, with an expected change of only +0.6 kg/m2. However, the comparison condition (CBT) is expected to change (0.6 + 1.5) or 2.1 kg/m2. That difference expressed as a fraction of the pooled baseline standard deviation (the standardized effect size) is d = 0.22, with a 95% confidence interval of −0.20 to 0.64. However, this apparent difference in slope was not statistically significant, χ2 (1) = 1.0, p = .32.
Secondary Outcomes
Changes in percent of time spent in moderate-to-vigorous physical activity (MVPA) and sedentary behavior were examined using a piecewise linear function model. There was a significant increase in the percentage of time (3.8%) that adolescents in CBT-HL spent in MVPA at 12 weeks that was not observed in those in CBT (p=.04). These increases were not maintained at the 24 and 48 week assessments. Data regarding mean percent of time spent in MVPA and sedentary behavior are presented in Table 4.
Table 4.
Means and Standard Deviations of Percent of Time in Moderate-to-Vigorous Physical Activity (MVPE) and Sedentary Behavior by Treatment Condition
| MVPA | Sedentary Behavior | |||
|---|---|---|---|---|
| Variable | CBT-HL | CBT | CBT-HL | CBT |
| Baseline | 7.5 (4.0) | 7.9 (2.2) | 71.2 (11.5) | 69.1 (9.0) |
| Week 12/ Midtreatment | 11.6 (7.4) | 7.3(2.9) | 67.7 (14.1) | 67.7 (9.4) |
| Week 24/ End of treatment | 9.9 (5.4) | 9.3 (5.1) | 69.2 (14.5) | 69.4 (11.2) |
| Week 48/ 6 Month follow-up | 8.5 (3.9) | 8.9 (4.4) | 65.0 (12.0) | 69.0 (9.04) |
While not statistically significant, teens randomized to CBT-HL decreased time spent in sedentary behavior at the 48-week follow-up while those assigned to CBT remained stable. Among participants in CBT-HL, greater participation in the weekly supervised exercise session during active treatment was significantly related to weight loss (r = −.50, p < .05), but not depressed mood (r = −.05, p = .84).
Discussion
This study examined the feasibility and acceptability of an integrated CBT and healthy living protocol for an ethnically and socioeconomically diverse sample of depressed, overweight/obese adolescents. Findings indicate that CBT-HL and CBT conditions both resulted in a clinically significant reduction in depressed mood by the 48-week follow-up assessment. The two conditions were not significantly different in their effects on depressed mood, but the effect size favored the CBT condition over the CBT-HL condition. The additional emphasis on healthy lifestyle in the CBT-HL condition may have contributed to this smaller effect because sessions covered both healthy lifestyle and depressed mood concerns, while CBT sessions focused solely on depressed mood. Nonetheless, both conditions resulted in decreases in depressed mood to a nonclinical level at the long term follow-up. With respect to weight status, the CBT-HL condition showed a modest trend toward reduction and greater stabilization of weight status while there was a pattern of a small increase in BMI in the CBT group. Secondarily, participants who received CBT-HL demonstrated short-term increase in number of minutes spent in MVPA.
Attendance at individual therapy appointments was significantly greater for participants assigned to CBT alone, which may indicate that the added burden of attending group exercise sessions affected psychotherapy attendance. Anecdotally, as reported by therapists and observed by supervisors in videotape review, some adolescents in the CBT-HL condition seemed to find content related to weight, diet, and physical activity challenging to discuss and/or may have been less motivated to address these issues in therapy sessions, potentially impacting attendance. Some studies have found that adding treatment components can serve to dilute the “dose” of an evidenced-based approach such as CBT (Hollon, Garber, & Shelton, 2005). In this study, adolescents in the CBT-HL condition demonstrated the same clinically meaningful improvements in depressed mood as those in CBT. Although it was hypothesized that the addition of a healthy lifestyle enhancement would improve depression outcomes, the CBT group had an excellent response to the treatment, possibly making it more difficult for the CBT-HL condition to improve upon that effect. Another potential explanation for the lack of difference between groups is that some adolescents assigned to CBT-HL did not fully engage with the lifestyle intervention.
One goal of the CBT-HL protocol was to increase physical activity because of its potential effect on depressed mood. Physical activity was increased during the group exercise program, and participants assigned to the CBT-HL condition demonstrated a small short-term increase in physical activity outside of the treatment setting. This improvement was not maintained at the other follow-up points, however, and there were no differences found between conditions on percentage of time in sedentary behavior. These findings need to be interpreted cautiously because adherence to the physical activity monitoring procedure was low among participants in the study. Nonetheless, future studies might emphasize brief bouts of physical activity (i.e. 1000 steps or 10 minutes) as a strategy for increasing physical activity outside of structured exercise or add motivational enhancement to increase teen engagement with this behavior. Physical activity monitoring devices might also be provided to participants to allow them to monitor and hopefully increase their physical activity outside of structured exercise sessions.
Exercise was included as an intervention component due to its potential impact on both mood and weight. Given that adolescents in the CBT only condition demonstrated comparable improvements in mood to the CBT-HL participants and there was no relationship between exercise session attendance and depressed mood, participation in exercise did not appear to enhance mood outcomes. The current literature suggests that physical activity can lead to improvements in depressed mood but the studies have not been conducted with adolescents with the level of depression reported in this study (Brown et al., 2013). Given the low adherence to exercise prescription for some teens, it is difficult to draw firm conclusions regarding the impact of physical activity on adolescents with mood disorder.
There was a significant relationship between exercise session attendance and weight loss. Adolescents who attended a greater number of exercise sessions were also more likely to complete CBT treatment. These findings could reflect the fact that increased participation in exercise facilitated modest weight maintenance or that engagement in weekly exercise sessions was a marker for overall commitment to intervention components, including changes to exercise and dietary habits. Given that previous weight control studies do not show decrease in weight associated with increased physical activity alone (Raynor, 2009), the latter appears more plausible. Further research, including a more thorough assessment of dietary intake and physical activity, is needed to understand the mechanisms for change in weight and mood.
A secondary goal of the enhanced intervention was to improve weight status. A small effect size was observed for adolescents who received the combined intervention, suggesting potential weight stability, in contrast to continued small increase in BMI observed for those who received CBT alone. Previous studies demonstrate significant end of treatment decreases in BMI (1.3–1.5 kg/m2) and z-BMI (.16-.21) among adolescents without psychiatric comorbidity participating in lifestyle interventions (Jelalian et al., 2010). It is worth noting that such interventions commonly include weekly sessions that are entirely dedicated to key components of weight control, including caloric restriction and behavioral strategies to support adherence to eating and physical activity prescription. In comorbid populations such as the population studied here, stabilizing weight status might be considered a positive outcome, especially in light of the fact that the protocol did not emphasize weight loss but rather adopting a healthier lifestyle.
Although adolescents in depression-only treatment reported significant improvements in depressed mood, their significant increases in weight status are concerning. Without inclusion of a third no-treatment comparison condition, we cannot decipher how this rate of increase compares to that of depressed overweight/obese adolescents in general, although overweight/obese adolescents tend to increase weight over time (Lagstrom et al., 2008). While the longer term impact of increase in BMI on depressive symptoms in the CBT-alone group is unknown, it is possible that adolescents whose weight status increased over the course of the study could be more vulnerable to recurrence of depressive symptoms (Boutelle et al., 2010). It is noteworthy that while some adolescents assigned to CBT-HL expressed hesitation about topics related to weight, many parents of adolescents who received CBT-only expressed disappointment in their teens not receiving CBT-HL. In some cases, weight control was clearly more salient for parents, than their adolescent, a factor that needs to be considered in developing treatment engagement strategies for this population.
Limitations
These study findings must be considered in the context of a number of limitations. This pilot study was not powered to detect a clinically significant difference between conditions and the parameter estimates are not likely to be stable (Kraemer, Mintz, Noda, Tinklenberg, & Yesavage, 2006). Missing data from participants who we were unable to contact for follow-up assessments and those whose height data were impacted by equipment error may have also affected the findings. Of note, analyses conducted with these observations excluded, using last observation carried forward imputation, and weight status, all demonstrated the same pattern of results. A final limitation is the relatively low ICC observed on the CTRS; although this may reflect the fact that only a small subset of sessions contributed to calculation of reliability. Future research with a larger sample will be needed to test both the generalizability and efficacy of the intervention. Because some adolescents were clearly less interested in the dietary and exercise component of the CBT-HL protocol than their parents, a treatment choice design might be most relevant to furthering our understanding of the best treatment options for this population. Other potential strategies include adding a motivational interview module addressing diet and physical activity at the start of treatment and/or a different model for integrating lifestyle components (e.g. focusing only on CBT for depression for the initial treatment phase until mood is stabilized). Future studies might also consider an exercise-only comparison group in order to disentangle the specific effects of exercise and to further examine the mechanisms through which enhanced, integrated treatment might lead to improvement in mood and weight stabilization or weight loss.
Clinical implications
Despite these limitations, this study is important in demonstrating the feasibility of an enhanced intervention that addresses both mood and healthy lifestyle for depressed, overweight/obese adolescents. There was a significant portion of adolescents in CBT-HL who did not attend very many exercise sessions suggesting that the added treatment burden must be considered when recommending this type of protocol in clinical practice.
Figure 1.
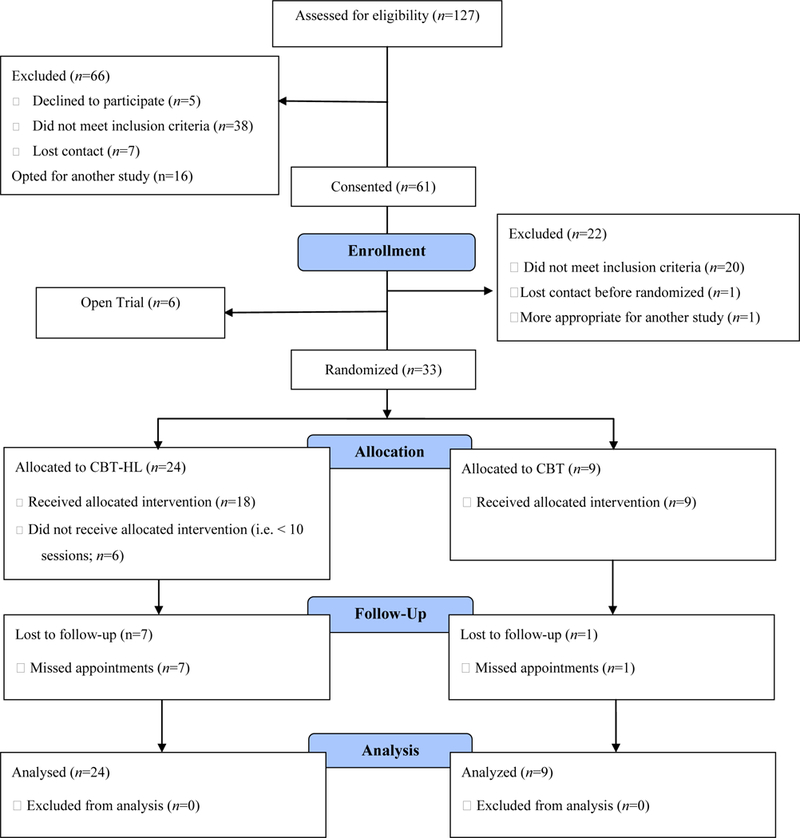
CONSORT 2010 Flow Diagram
Acknowledgments
This trial was funded by federal grant R34 MH083092. Clinicaltrials.gov identifier: NCT01128764
References
- Boutelle KN, Hannan P, Fulkerson JA, Crow SJ, & Stice E (2010). Obesity as a prospective predictor of depression in adolescent females. Health Psychology, 29, 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, …& Zelazny J (2008). Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. Journal of the American Medical Association, 299, 901–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown H, Pearson N, Braithwaite R, Brown W, & Biddle S (2013). Physical activity interventions and depression in children and adolescents: A systematic review and meta-analysis. Sports Medicine, 43, 195–206 [DOI] [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, & Neumark-Sztainer D (2006). Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. Journal of Adolescent Health, 38, 569–74. [DOI] [PubMed] [Google Scholar]
- David-Ferdon C, & Kaslow N (2008). Evidence-based psychosocial treatments for child and adolescent depression. Journal of Clinical Child and Adolescent Psychology, 37, 62–104. [DOI] [PubMed] [Google Scholar]
- Esposito–Smythers C, Spirito A, Kahler CW, Hunt J, & Monti P (2011). Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 79, 728–739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths LJ, Parsons TJ, Hill AJ (2010). Self-esteem and quality of life in obese children and adolescents: A systematic review. International Journal of Pediatric Obesity, 5, 282–304. [DOI] [PubMed] [Google Scholar]
- Guy W (1976). ECDEU assessment manual for psychopharmacology Rockville, MD: US Department of Heath, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration. [Google Scholar]
- Harper G, Contreras R, Bangi A, & Pedraza A (2003). Collaborative process evaluation: Enhancing community relevance and cultural appropriateness in HIV prevention. Journal of Prevention and Intervention in the Community, 26, 53–71. [Google Scholar]
- Hesterberg T, Monaghan S, Moore D, Clipson A, & Epstein R (2005). Bootstrap methods and permutation tests In Moore D & McCabe G (Eds.). Introduction to the practice of statistics (pp. 14–11). New York: WH Freeman. [Google Scholar]
- Jelalian E, Hadley W, Sato A, Kuhl E, Rancourt D, Oster D, & Lloyd-Richardson E (2015). Adolescent weight control: An intervention targeting parent communication and modeling compared with minimal parental involvement. Journal of Pediatric Psychology, 40, 201–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jelalian EJ, Richardson EE, Mehlenbeck RS, Hart CN, Flynn-O’Brien KF, Kaplan J, Neill M, & Wing RR (2010). Behavioral weight control treatment combined with supervised exercise or peer enhanced adventure intervention for overweight adolescents. The Journal of Pediatrics, 157, 923–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, & Rao U (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Korczak DJ, Lipman E, Morrison K, Duku E, & Szatmari P (2013). Child and adolescent psychopathology predicts increased adult Body Mass Index: Results from a prospective community sample. Journal of Developmental and Behavioral Pediatrics, 35, 108–117. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Mintz J, Noda A, Tinklenberg J, & Yesavage JA (2006). Caution regarding the use of pilot studies to guide power calculations for study proposals. Archives of General Psychiatry, 63, 484. [DOI] [PubMed] [Google Scholar]
- Lagstrom H, Hakanen M, Niinikoski H, Viikari J, Ronnemaa T, Saarinen M, Pahkala K, & Simell O (2008). Growth patterns and obesity development in overweight or normal-weight 13-year old adolescents: The STRIP Study. Pediatrics, 122, e876–e883. [DOI] [PubMed] [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, … & Severe J (2004). Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Journal of the American Medical Association, 292, 807–820. [DOI] [PubMed] [Google Scholar]
- McCauley E, Gudmundsen G, Schloredt K, Martell C, Rhew I, Hubley S, & Dimidjian S (2015). The Adolescent Behavioral Activation Program: Adapting behavioral activation as a treatment for depression in adolescence. Journal of Clinical Child and Adolescent Psychology, 1, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCCMH. (2005). Depression in children and young people: Identification and management in primary, community and secondary care. Leicester and London: The British Psychological Society and the Royal College of Psychiatrists. [PubMed] [Google Scholar]
- Paluch RA, Epstein LH, & Roemmich JN (2007). Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. American Journal of Human Biology, 19, 487–494. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, Freeman LN & Mokros HB (1984). Children’s Depression Rating Scale – Revised. Psychopharmacology Bulletin, 21, 927–989. [Google Scholar]
- Raynor H (2008). Evidenced-based treatments for childhood obesity In Jelalian E & Steele R (Eds.). Handbook of Childhood and Adolescent Obesity (pp 201–220). New York: Springer. [Google Scholar]
- Singer JD, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford: Oxford University Press. [Google Scholar]
- Witherspoon D, Latta L, Wang Y, & Black MM (2013). Do depression, self-esteem, body-esteem, and eating attitudes vary by BMI among African American adolescents? Journal of Pediatric Psychology; 38, 1112–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J, & Beck AT (1980). Cognitive therapy scale rating manual. Philadelphia, PA, University of Pennsylvania. [Google Scholar]
- Zametkin AJ, Zoon CK, Klein HW, & Munson S (2004). Psychiatric aspects of child and adolescent obesity: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 134–50. [DOI] [PubMed] [Google Scholar]


