Abstract
Objective
To evaluate the amount and content of data patients and carepartners reported using a real-time electronic safety tool compared to other reporting mechanisms, and understand their perspectives on safety concerns and reporting in the hospital.
Methods
Mixed-methods study including 20 month pre- and post-implementation trial evaluating MySafeCare, a web-based application which allows hospitalized patients/carepartners to report safety concerns in real-time. Comparison of MySafeCare submission rates for three hospital units (oncology acute care; vascular intermediate care; medical intensive care) to submissions rates of Patient Family Relations (PFR) Department, a hospital service to address patient/family concerns. Triangulation of quantitative data with thematic analysis of safety concern submissions and patient/carepartner interviews to understand submission content and perspectives on safety reporting.
Results
Thirty-two MySafeCare submissions were received with an average rate of 1.7 submissions per 1,000 patient-days and a range of 0.3 to 4.8 submissions per 1,000 patient-days across all units, indicating notable variation between units. MySafeCare submission rates were significantly higher than PFR submission rates during the post-intervention period on the vascular unit (4.3 [95% CI 2.8 – 6.5] versus 1.5 [95% CI 0.7 – 3.1], Poisson) (P=0.01). Overall trends indicated a decrease in PFR submissions after MySafeCare implementation. Triangulated data indicated patients preferred to report anonymously and did not want concerns submitted directly to their care team.
Conclusions
MySafeCare evaluation confirmed the potential value of providing an electronic, anonymous reporting tool in the hospital to capture safety concerns in real-time. Such applications should be tested further as part of patient safety programs.
Keywords: Patient Safety, Patient Experience, Patient Engagement, Safety Reporting
Introduction
Hospitalized patients and their carepartners (i.e., family, friends) often have concerns about the safety of the care they receive.1 Our understanding of patients’ and carepartners’ perspectives, who experience a wide range of concerns every day, is limited. Rates of concerns are not well-understood because they are seldom captured in hospital incident reporting systems or the medical record, particularly in the absence of a safety event that caused patient harm.1 Preventable harms continue to occur at unacceptable levels2–8; given this context the potential rates of underreported concerns are alarming.
While voluntary event-reporting systems exist in many healthcare organizations for clinician reporting, and patient safety organizations have greatly advanced our understanding of safety9–12, the lack of patient/carepartner reporting needs to be addressed.13 Yet patients have different comfort levels disclosing negative feedback, may have insufficient knowledge of reporting options, or lack reporting options optimized for a real-time response.13–15 These influences combine to greatly limit our ability to: 1) intervene in real-time, and 2) understand patient/carepartner perspectives of safety threats to inform system-wide prevention strategies.
Given that electronic tools have the potential to capture safety concerns to mitigate events in real-time and trend data for quality improvement, we developed and implemented MySafeCare at an academic medical center in the Northeastern United States. We employed a participatory user-centered design process with patients/carepartners to inform development, which will be published separately. MySafeCare is a web-based application that allowed hospitalized patients and carepartners to electronically submit and categorize safety concerns in real time. MySafeCare includes a compliment section--which patients requested--and nine concern categories: plan, medication, room, communication, hygiene, privacy, pain, waiting time, and other.
Data-driven methods to understand, mitigate, and track safety concerns from the patient and carepartner perspective could transform hospitals into accountable, patient-centered learning health systems and improve safety and outcomes.16–19 MySafeCare supplemented existing reporting options for patients/carepartners by providing a unique method for electronic reporting and the option of remaining anonymous. Examples of existing reporting options in the hospital for patients/carepartners include conversations with their care team or the hospital’s Patient Family Relations (PFR) department, which provides services to enhance the patient experience including documenting and addressing compliments and concerns received via telephone, walk-in, email, or letter.
The aims of this mixed-methods study were to evaluate patient/carepartner safety reporting submission trends using MySafeCare and to explore their perspectives on safety concerns while in the hospital.
Methods
Study Setting and Design
We conducted a 20-month pre-post intervention trial comparing pairs of time points to evaluate usage of MySafeCare on three hospital units. These three units, selected for variation in acuity and clinical domain, were a 28-bed intermediate care Vascular Unit, a 20-bed acute care Oncology Unit, and a 20-bed Medical Intensive Care Unit (MICU).
Key features of MySafeCare include the ability for patients/carepartners to: remain anonymous or self-identify, submit a concern or a compliment, categorize concerns, submit a narrative, rank concern severity, and provide optional demographic data. Submissions are viewable on a secure, password protected dashboard for each clinical unit. Primary users of the dashboard include Nurse and Medical Directors, staff nurses, and physicians. The Nurse and Medical Directors receive an automated email in real-time when a submission is received on their hospital unit. Consistent with current governance structure, the Nurse Director on each unit is responsible for following up to resolve or escalate a concern as appropriate. Additionally, sharing of aggregated de-identified data for learning occurs with hospital committees.
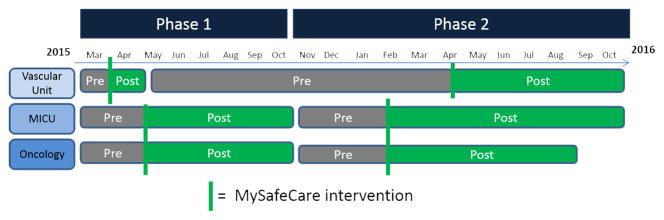
MySafeCare was user-designed, tested, and optimized within a Patient Safety Learning Laboratory.20 The trial consisted of two phases of pre-post implementation that coincided with release of a new version: phase 1 implemented version 1, and phase 2 implemented version 2 (see Figure 1). Version 2 of MySafeCare included three refinements based on end-user feedback: 1) categories’ names and icons, 2) decreased scrolling, 3) submission of multiple concerns/compliments within the same session. All other refinements that occurred were limited to technical infrastructure enhancements (i.e., not user-facing) and optimization of our dashboard, which is clinician facing, not patient/carepartner facing.
Figure 1.
Timeline of MySafeCare implementation across units and study phases
The research team conducted engagement rounds to each patient room explaining that MySafeCare was available to report any safety concerns, defined as “a worrisome or concerning event”. This definition was tested with end-users and used consistently throughout the study. The purpose of engagement rounds was not to prompt reporting (although this was potentially a natural consequence), but rather to inform patients/carepartners early in their stay that this application was available during their hospitalization if they did experience a safety concern and to provide them with printed handouts of how to access the application and study information. Engagement rounds were initially conducted daily during phase 1 of the trial and decreased to biweekly during phase 2 of the trial based on patient turnover rates. Laminated signs with study information, URL, and QR code were placed in patient rooms and family waiting areas to inform patients/carepartners how to access the application. This was a bring-your-own-device trial and an iPad was available for individuals who did not have their own device.
Quantitative Evaluation: Real-Time Reporting and Comparative Trends
We conducted quantitative analyses of MySafeCare usage and submission rates and demographic data of MySafeCare users. All rates of submissions were calculated per 1,000 patient days and reported with 95% Confidence Interval (CI). Pre-specified comparisons to rates of PFR submissions during the same time-period for the prior calendar year, as well as during the pre- and post-intervention period, were performed. We used descriptive statistics and two-sided Z tests for equal Poisson rates to compare MySafeCare submission rates to PFR rates.
We performed descriptive, exploratory analyses of HCAHPS (the Hospital Consumer Assessment of Healthcare Providers and Systems) scores across our pre- and post-study periods. Given the pre-post study design and small sample sizes this analysis was not aimed at nor powered to conclude if a change in rate of HCAHPS scores was attributed to the MySafeCare intervention, but rather to identify potential trends associated with MySafeCare for investigation in a larger trial. We used the Top Box method to analyze HCAHPS scores for each of the 11 components21 and included all patients that answered an HCAHPS survey and had been admitted to a study unit for greater than 24 hours. To address small sample sizes, we only included data for HCAHPS components with 5 or greater samples and a response rate greater than 60%.
Qualitative Evaluation: Content Analysis of Safety Concerns and Perspectives on Reporting
We performed thematic analysis of the narrative content of concerns submitted to illustrate the novel information that MySafeCare captures. We also conducted semi-structured interviews with a convenience sample of hospitalized patients/carepartners to better understand their unique perspectives related to reporting safety threats. Patients deemed clinically stable by their nurse were recruited for interviews on the Vascular and Oncology Units and, if present, carepartners were invited to participate. Given the acuity of ICU patients, we asked carepartners in the MICU waiting room if they would like to participate in an interview. Interviews were conducted by 1–2 investigators, audio-recorded and transcribed verbatim. If participant did not want to be audio-recorded 2 investigators were present and notes were taken during the interview and reviewed immediately after for completeness to serve as the interview transcript. We performed thematic analysis of the transcripts using NVivo(c) software (version 10) to identify common themes that captured the breadth of content in our data set. We performed iterative data analysis and continued data collection until saturation was reached and no new themes were identified. These thematic findings were triangulated with the free-text narratives of MySafeCare concerns to understand the current state of patient/carepartner safety reporting and to identify how data captured in MySafeCare can contribute to a learning health system. All activities were approved by our Institutional Review Board (IRB).
Results
Quantitative Evaluation: Real-Time Reporting and Comparative Trends
A total of 32 submissions were received in MySafeCare during the study. The overall rate of submissions equated to 4.8 submissions/1000 patient days on the Vascular Unit, 0.3 submissions/1000 patient days on the Oncology Unit, and 0.3 submissions/1000 patient days on the MICU. On average, this was equivalent to 3.3 submissions per month on the Vascular Unit, and 0.2 submissions per month on the Oncology Unit, and 0.1 submissions per month on the MICU.
MySafeCare was designed so that a patient/carepartner may submit multiple concerns or compliments within one submission. For example, one submission included three different concerns entered by the same individual. Accounting for this ‘one to many’ relationship, our data set included a total of 37 unique concerns and compliments, with 18/37 (49%) being concerns and 19/37 (51%) being compliments (see Table 1). Among the concerns, 56% (10/18) were submitted anonymously. Compared to concerns, fewer compliments were submitted anonymously at 26% (5/19). All individuals that chose to submit anonymous concerns indicated they had shared their concern with their care team. Categories of submitted concerns included: ‘my plan’, ‘my medication’, ‘my communication’, ‘my hygiene’, ‘my waiting time’, and ‘other’. All the concerns that related to ‘my plan’ and ‘my hygiene’ were anonymous, 1 of 1 and 3 of 3 respectively. ‘My medication’ and ‘my communication’ categories each had 1 anonymous and 1 identified concern. The only ‘my waiting time’ concern was identified. Nine concerns were categorized by patients/carepartners as ‘other’, with 4 (44%) being anonymous.
Table 1.
Instances of MySafeCare Concerns and Compliments with Submitter Demographics
| Submission Information | Concern % (n) | Compliment % (n) |
|---|---|---|
| Submitter | ||
| Patient | 50% (9) | 95% (18) |
| Family/Friend | 50% (9) | 5% (1) |
| Anonymous | 56% | 26% |
| Concern first occurred | ||
| Today | 22% (4) | n/a |
| Yesterday | 28% (5) | n/a |
| More than 2 days ago | 50% (9) | n/a |
| Level of Concern | ||
| Low concern | 17% (3) | n/a |
| Moderate concern | 44% (8) | n/a |
| High concern | 39% (7) | n/a |
| Optional questions (percent is based on number of responses received per question) | ||
| Did share concern/compliment directly with Care Team | 56% (10/18) | 33% (1/3) |
| If did NOT share, plan to share with Care Team in the future | 43% (3/7) | 50% (1/2) |
| Family is engaged with care | 75% (6/8) | 64% (9/14) |
| Episode of Care | ||
| Urgent | 55% (6/11) | 64% (7/11) |
| Planned | 46% (5/11) | 36% (4/11) |
| Gender Male | 57% (8/14) | 43% (6/14) |
| Age | ||
| Under 80 | 100% (10/10) | 91% (10/11) |
| Level of education | ||
| Completed at least some college | 100% (10/10) | 64% (7/11) |
| Primary Language English | 100% (6/6) | 100% (8/8) |
| Health Literacy | ||
| Low Literacy | 10% (1/10) | 9% (1/11) |
| Moderate/High Literacy | 90% (9/10) | 91% (10/11) |
| Total Instances | 18 | 19 |
Total instances equals 18 concerns + 19 compliments = 37 instances which is greater than number of submissions (n=32) because more than one concern or compliment can be entered per submission (instance to submission = many to one). Percent rounded to nearest whole number.
Twenty-one of the 32 individuals that entered a submission (65%) completed the optional demographics section, 95% (20/21) were under 80 years old and 67% (14/21) were male. Sixty-five percent (13/20) of patients’ hospital admissions had been urgent (i.e., not planned). Of the 14 individuals that answered the race and ethnicity questions: 93% (13/14) white, 100% (14/14) non-Hispanic. All users considered English as their primary language. Seventeen out of 21 (81%) had completed at least some college and 4/21 (19%) had completed high school/GED as their highest level of education.
During study phase 1 post-intervention period, MySafeCare received a rate of 10 submissions per 1,000 patient-days [95% CI: 4.6 – 21.4] on the Vascular Unit. During the phase 1 pre-period (same time-period prior year), PFR received a rate of 1.1 submissions per 1,000 patient-days [95% CI: 0.1 – 17.6] on the same unit. While the difference on the rates above were not statistically significant (p = 0.13), the combined rate for MySafeCare and PFR during study phase 1 post-period was significantly higher than the PFR rate the year prior on the Vascular Unit (19.1 [95% CI: 11 – 33.3] versus 1.1 [95% CI: 0.1 – 17.6]; p=0.04). This higher combined rate suggests an increased capture of patient-reported safety concerns overall after MySafeCare was implemented. During the Phase 2 intervention period, the rate per 1000 patient days of MySafeCare submissions was significantly higher than PFR submissions during that same time-period (4.3 [95% CI: 2.8 – 6.5] versus 1.5 [95% CI: 0.7 – 3.1]; p= 0.01) (see Table 2).
Table 2.
Vascular Unit Data: MySafeCare (MSC) compared to Patient Family Relations (PFR)
| Study Phase | MySafeCare Status | Data Type | Occupied Bed Days | Rate [CI] | P Value |
|---|---|---|---|---|---|
| Intermediate Vascular Unit | |||||
| Phase 1 | Pre-intervention | PFR | 455 | 1.1 [0.1 – 17.6] | 0.13 |
| Phase 1 | Post-intervention | MSC | 655 | 10.0 [4.6 – 21.4] | |
| Phase 1 | Pre-intervention | PFR | 455 | 1.1 [0.1 – 17.6] | 0.04 |
| Phase 1 | Post-intervention | MSC + PFR | 655 | 19.1 [11 – 33.3] | |
| Phase 2 | Post-intervention | MSC | 5018 | 4.3 [2.8 – 6.5] | 0.01 |
| Phase 2 | Post-intervention | PFR | 5018 | 1.5 [0.7 – 3.1] | |
| Study Phase | MySafeCare Status | Data Type | Occupied Bed Days | Rate [CI] | P Value |
| Medical Intensive Care Unit (MICU) | |||||
| Phase 1 | Post-intervention | PFR | 2849 | 0.9 [0.3 – 3.0] | 0.02 |
| Phase 2 | Pre-intervention | PFR | 2160 | 4.4 [2.3 – 8.3] | |
| Phase 2 | Pre-intervention | PFR | 2160 | 4.4 [2.3 – 8.3] | 0.03 |
| Phase 2 | Post-intervention | PFR | 3075 | 1.1 [0.4 – 3.3] | |
| Phase 1 | Post-intervention | PFR | 2848 | 0.9 [0.3 – 3.0] | 0.92 |
| Phase 2 | Post-intervention | PFR | 3075 | 1.0 [0.4 – 2.4] | |
Rates are rounded to 1 decimal point.
During the study, PFR submission rates were observed to decrease after MySafeCare was implemented and increase when MySafeCare was deactivated. This trend was observed across all units but was only statistically significant in the MICU (Table 2). When MySafeCare was initially implemented on the MICU (study phase 1 post-period), PFR rates were 0.9 [95% CI: 0.3 – 3.0] and when MySafeCare was later deactivated (study phase 2 pre-period) PFR rates increased to 4.4 [95% CI: 2.3 – 8.3] (p-value = 0.02). When MySafeCare was activated again (study phase 2 post-period) PFR rates decreased to 1.0 [95% CI: 0.4 – 2.4] (p-value = 0.007).
No statistically significant differences in HCAHPS data held across both Phase 1 and 2 intervention periods. However, the rate of satisfaction with ‘communication about medicines’ increased during the phase 2 post-intervention study period [68 to 96 (p=0.04)] on the Oncology Unit, and the rate of satisfaction with ‘communication with physicians’ decreased during one of the post-intervention study periods on the MICU [94 to 74 (p=0.03)]. It is important to note that these trends were not consistently observed across all study units, indicating they might be related to other causes than MySafeCare or to chance.
Qualitative Evaluation: Thematic Analysis of Submitted Safety Concerns and Patient and Carepartner Perspectives on Reporting
Thematic Analysis of Submitted Concerns
Patient and carepartner concerns related to the following themes: 1) Unmet care needs and preferences, 2) Inadequate communication or coordination of care, 3) Clinical protocols, 4) Facilities, 5) Lack of trust, and 6) Security (e.g., visitor access). In several narratives describing the concern, patients/carepartners identified specific safety risks relevant to the concern such as risk of pressure ulcer, risk for decompensation, risk for hypoglycemia, and risk for infection. Concerns that related to inadequate communication or coordination of care, lack of trust, and security did not include narratives in which a specific safety risk was identified, rather global concerns were noted (see Table 3).
Table 3.
Thematic Analysis of Submitted Concerns
| Theme | Synthesis of Patient/Family Narratives Submitted | Relevant Safety Risk Identified by Patient/Family | Example Quote |
|---|---|---|---|
| Unmet care needs and preferences |
|
|
“Because of poor circulation, personnel were advised multiple times (pre-op, post-op, etc) NOT to put “hospital socks” on patient’s feet - they are too constrictive and result in bruising, sores/wounds. Despite advanced warning, socks WERE put on patient and results were as expected. Fortunately, a family member spotted the problem early, advised Care Team doctor, and socks were removed. Some bruising occurred, hopefully to recede in coming weeks. This is a very dangerous situation. Prior to this stay… result was deep wounds/ulcers and exposed tendons.” |
| Inadequate Communication |
|
No specific risk identified | “[name removed] was taken for a stress test at 12:55, it is now 4:45 and I have had no update. There has been a nurse shift change and I do not know who his assigned nurse is at this time.” |
| Lack of Trust |
|
No specific risk identified | “This nurse came into my room several days later due to an alarm on my pump and never said a word to me, altered the program on the pump and never told my nurse that she changed the flow of my pump.” |
| Clinical Protocols |
|
|
“I was concerned that nurse did not seem to use alcohol wipes when flushing lines*, etc, and generally seemed less careful around sterility when giving iv drugs, etc” *Protocol was followed, but patient did not understand that protocol recommends to change IV cap rather than use alcohol. |
| Facilities |
|
|
“Waiting Room should have a sink and handwashing station” |
| Security |
|
No specific risk identified | “I am concerned that visitors are not stopped and asked for ID” |
Thematic Analysis of Patient and Carepartner Perspectives on Reporting
We conducted a total of 15 semi-structured interviews. All participants approached agreed to participate. Eleven interviews were conducted with patients only, 2 with carepartners only, and 2 with a patient and carepartners. Four high level categories were defined to group the 8 themes identified (see Table 4). Several patients and carepartners initially expressed that they had no concerns and that everything about the care was great, however, as the interviews continued their answers did illuminate areas for improvement. Patients perceived the need to balance their level of concern with the level of awkwardness they felt when giving negative feedback. They noted frustration that clinicians needed reminders, such as badges that state “Ask me if I washed my hands”. Carepartners were described as more comfortable than patients in voicing concerns. Likewise, in MySafeCare a carepartner emphasized they had voiced a concern but “…despite advanced warning, socks WERE put on patient and results were as expected…”
Table 4.
Themes of Patient and Carepartner Perspectives on Safety Concerns and Reporting
| Themes | Influences | Factors | Examples Quote |
|---|---|---|---|
| Discomfort Speaking Up | Personal |
Comfort levels vary depending on:
|
“It is hard to question everything…you reach the point where you have to speak up…even though it’s hard.” “You don’t want silly little reminders everywhere…you just want something done in the right way” |
| Cultural |
Clinicians’ attitude
|
“At some hospitals you are educated, at others you are schooled” | |
Patients “passively” voice concerns:
|
“Well, you know, the personality of the doctor was such that he was supremely confident…that this was what had to be done, and presented himself in that way. And then I can imagine that, uh, you know, many people would be cowed by that.” “I’m not supposed to get up [at night]. Some of the people empty the urinals and don’t rinse them. So it’s like they’re putting a urinal back on the table that has stale urine in it. And it’s just telling somebody to do that is very hard. So what I’ve done with that urinal issue is, when a nurse or a PCA comes in that does rinse I say, ‘Oh, I’m so relieved that you’re doing that, because, you know, not everybody does that.’ So I’m hoping that they will solve that out there [among the staff].” |
||
| Lack of Awareness of How to Speak Up | Knowledge and tool gaps | “Chain of command” for reporting not known by many patients:
|
“There should be communicating with someone that there’s a problem without really letting everybody else [know]… Even a hotline.” “They should have a committee that, if we can’t talk to a doctor or talk to a nurse, you have a team of people that do that type of job, that comes in and counsels you and then work towards it with the doctors and the nurses.” |
Clinicians’ attitude was emphasized as a variable that could either encourage open sharing, or, conversely, serve to intimidate and close off communication when a clinician was perceived to have a pre-determined plan and assumptions about the patient’s care needs. Patients articulated their use of ‘passive’, ‘subtle’, and ‘quiet’ strategies to communicate a concern due to discomfort in directly sharing negative feedback. These strategies included using positive reinforcement and simply hoping the subtle message is received or discomfort is noticed (see Table 4). One MySafeCare submission described similar discomfort: “I was concerned that nurse did not seem to use alcohol wipes when flushing lines…”
The available ways that a patient/carepartner could report a safety concern were overall not known or had not been considered by interviewees. It was not apparent to interviewees that a ‘chain of command’ exists for safety reporting and that roles such as Nurse Director and Medical Director, as well as PFR, are available to discuss concerns. Despite this lack of awareness, patients/carepartners interviewed described the need for anonymous and confidential reporting and “communication with someone that there’s a problem without really letting everybody else [know]…Even a hotline.”
DISCUSSION
We implemented a tool which enabled patients/carepartners to report concerns electronically, which they were willing to do, at least on occasion. While counts of submissions appear low they were comparable or significantly higher than submissions received by PFR at our hospital, and similar consumer safety reporting systems.13 The content of concerns included explicit identification of safety risks. The combined rate of MySafeCare and PFR submissions on the Vascular Unit was significantly higher than the rate of PFR submissions the year prior, indicating an application for hospitalized patients/carepartners to report safety concerns can capture additional safety information that was not otherwise being captured electronically. Our engagement rounds likely influenced reporting rates beyond spontaneous reporting; however, as with many patient engagement interventions, communication to inform patients/carepartners that an application exists and how to access it is a necessary part of the implementation approach. Other unit or hospital factors may have also influenced reporting, yet we believe our findings indicate the potential added value that an application such as MySafeCare can provide to patients and carepartners who may have a safety concern but are either unsure of how to communicate it or are uncomfortable voicing their concern if they might be identified.
It is most likely that the changes in HCAHPS scores were not associated with MySafeCare or the study was underpowered to detect consistent differences. It is possible that an intervention asking patients/carepartners about safety concerns could raise awareness of safety issues and that increased awareness could impact HCAHPS scores either positively or negatively; similar possibilities have been discussed elsewhere15 and could be investigated further.
Our finding that 55% of concerns were submitted anonymously, supports the provision of anonymous reporting options to patients/carepartners. Given that 45% of patients/carepartners identified themselves, these data also indicated strong potential for a safety reporting application to serve as an intervention that enables real-time identification and mitigation of safety concerns for patients/carepartners that choose to identify themselves. Interestingly, all individuals that chose to submit anonymous concerns indicated they had shared their concern with their care team. This paradox should be investigated further to understand the validity of this question and the rationale for anonymous reporting in this context. Our qualitative data indicated patients subtly convey concerns raising the question that perhaps patients subtly share a concern face-to-face but prefer an anonymous reporting option when explicitly communicating the issue. Reporting a concern in a reporting tool provides additional value to safety efforts beyond sharing a concern with a clinician. Electronic capture of anonymous concerns that were also discussed with a clinician is still of high value in a learning health system to build a corpus of data to identify system gaps and support process improvement. Due to the high number of concerns that were categorized as ‘other’ there is also the opportunity for data-driven refinement and expansion of MySafeCare concern categories. Learning how and why patients choose to categorize concerns or not, could expand our understanding of safety from the patient perspective and the complexity of the issues that patients are observing.
Our qualitative themes support the analyses of the counts and types of MySafeCare submissions described above. Patients interviewed reported feeling vulnerable and attempting to ‘nicely and subtly convey concerns and hope that they are noticed’. Patient discomfort speaking up is well documented.14 The notion that patients use implicit communication techniques to convey safety concerns is noteworthy and at odds with safety efforts for transparent communication and lack of hierarchical structures within clinician teams. These techniques require significantly deeper exploration and likely will necessitate multi-faceted interventions given the complex nature of verbal and non-verbal communication and deeply ingrained cultural attitudes of patients, carepartners, and clinicians that may be motivating their use. A safety reporting application is likely one type of intervention that can meet the needs of patients and carepartners hesitant to make their safety concerns explicit and identify themselves in doing so. Such an application could be part of system-wide, sociotechnical solution to: 1) increase awareness of safety reporting options, 2) provide anonymity in the setting of patient vulnerability, 3) increase transparency of safety concerns and understanding of their unique content by providing a central repository that can be accessed beyond the patient’s care team, and 4) provide a mechanism for real-time mitigation by an individual who is not on the patients care team if a user identified themselves.
We observed substantial variation in use of MySafeCare across clinical units. Future work should investigate cross-unit trends to better understand if unit, disease state, and prior experience with the healthcare system could impact variation in levels of safety concerns, comfort in reporting, and use of an anonymous, electronic reporting tool. Finally, our population was largely white, English speaking and highly educated with high health literacy levels. In response, we implemented a Spanish version of MySafeCare and recommend that future work actively target diverse populations and individuals at risk of health disparities.
Limitations
This study is limited by its small sample size and findings should be confirmed in other settings. Several factors may have influenced reporting rates, or HCAHPS scores, including engagement rounds or our hospital’s EHR implementation during study Phase 1. Some refinements outlined in the methods section were made to the application to increase its usability during the study. It is possible these changes impacted usage; however, only the interface terminology changed while the data elements definitions remained stable during the study period allowing for comparisons of data captured. Notably, greater variation in usage was seen across units, rather than across the two versions of MySafeCare.
CONCLUSION
MySafeCare successfully captured anonymous concerns and identified unique concerns from the patient and carepartner perspective, including identification of specific safety risks. Patients and carepartners lack knowledge of the “chain of command” available for reporting safety concerns and use passive, subtle strategies to communicate concerns, hoping that clinicians understand. These strategies represent a major gap in patient engagement strategies and the need for sociotechnical approaches to bridge this gap so that concerns are shared before they result in safety threats or harms. Electronic patient and carepartner safety reporting applications represent the next-generation of actionable measurement tools that provide a voice to, and data of, patients’ and carepartners’ safety concerns. Our findings highlight that there is a need for and value in providing electronic, anonymous reporting tools in the hospital setting to capture safety concerns from the patient and carepartner perspective in real-time.
Acknowledgments
FUNDING: Agency for Healthcare Research and Quality (AHRQ) 1P30HS0235335 Making Acute Care More Patient Centered
The authors thank the patients, carepartners, nurses, physicians and all other hospital staff who have contributed to this work. The authors also thank Adam Landman, Lesley Solomon and the Brigham iHub for their expertise and support. Software development of MySafeCare was completed by OpenClinica, LCC.
FUNDING
This work was funded by AHRQ 1P30HS0235335 Making Acute Care More Patient Centered.
Footnotes
CONTRIBUTORS
All authors have contributed sufficiently and meaningfully to the conception, design, and conduct of the study; data acquisition, analysis, and interpretation; and/or drafting, editing, and revising the manuscript.
COMPETING INTERESTS
The authors have no competing interests to declare.
References
- 1.Weingart SN, Pagovich O, Sands DZ, et al. What can hospitalized patients tell us about adverse events? Learning from patient-reported incidents. J Gen Intern Med. 2005;20(9):830–836. doi: 10.1111/j.1525-1497.2005.0180.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leape LL. Error in Medicine. JAMA J Am Med Assoc. 1994;272(23):1851. doi: 10.1001/jama.1994.03520230061039. [DOI] [PubMed] [Google Scholar]
- 3.Leape LL, Lawthers AG, Brennan TA, Johnson WG. Preventing medical injury. [Accessed November 20, 2015];QRB Qual Rev Bull. 1993 19(5):144–149. doi: 10.1016/s0097-5990(16)30608-x. http://www.ncbi.nlm.nih.gov/pubmed/8332330. [DOI] [PubMed] [Google Scholar]
- 4.Jha A, Larizgoitia I, Audera-Lopez C, Prasopa-Plaizer N, Waters H, Bates D. The global burden of unsafe medical care: analytic modelling of observational studies. BMJ Qual Saf. 2013;22:809–815. doi: 10.1136/bmjqs-2012-001748. [DOI] [PubMed] [Google Scholar]
- 5.Kohn LT, Corrigan JM, Donaldson MS, editors. Institute of Medicine (IOM) To Err Is Human: Building a Safer Health System. Washington, D.C: National Academy Press; 1999. [PubMed] [Google Scholar]
- 6.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf. 2013;9(3):122–128. doi: 10.1097/PTS.0b013e3182948a69. [DOI] [PubMed] [Google Scholar]
- 7.Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016 May;:i2139. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 8.Shojania KG, Dixon-Woods M. Re: Medical error—the third leading cause of death in the US. BMJ. 2016;353(i2139) doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 9.Okafor NG, Doshi PB, Miller SK, et al. Voluntary Medical Incident Reporting Tool to Improve Physician Reporting of Medical Errors in an Emergency Department. West J Emerg Med. 2015;16(7):1073–1078. doi: 10.5811/westjem.2015.8.27390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Patient Safety Foundation. History and Timeline. National Patient Safety Foundation; [Accessed January 25, 2016]. http://www.npsf.org/?page=historyandtimeline. Published 2016. [Google Scholar]
- 11.The Leapfrog Group. [Accessed January 25, 2016];About Leapfrog. http://www.leapfroggroup.org/about_leapfrog. Published 2016.
- 12.The Joint Commission. [Accessed January 25, 2016];Facts about patient safety. http://www.jointcommission.org/facts_about_patient_safety/. Published 2015.
- 13.Schneider EC, Ridgely MS, Quigley DD, et al. Developing and Testing the Healthcare Safety Hotline: A Prototyope Consumer Reporting System for Patient Safety Events. Final Report (Prepared by RAND Corporation under Contract HHSA290201000017I) Rockville, MD: 2016. [Accessed November 13, 2017]. https://www.ahrq.gov/sites/default/files/publications/files/healthcare-safety-hotline_0.pdf. [Google Scholar]
- 14.Watt I, Birks Y, Entwistle V, et al. [Accessed November 13, 2017];A Review of Strategies to Promote Involvement, a Study to Explore Patients’ Views and Attitudes and a Pilot Study to Evaluate the Acceptability of Selected Patient Involvement Strategies. 2009 http://www.birmingham.ac.uk/Documents/college-mds/haps/projects/cfhep/psrp/finalreports/PS034-Finalreport2009.pdf.
- 15.Lawton R, O’Hara JK, Sheard L, et al. Can patient involvement improve patient safety? A cluster randomised control trial of the Patient Reporting and Action for a Safe Environment (PRASE) intervention. BMJ Qual Saf. 2017;26(8):622–631. doi: 10.1136/bmjqs-2016-005570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halpern MT, Roussel AE, Treiman K, Nerz PA, Hatlie MJ, Sheridan S. Designing Consumer Reporting Systems for Patient Safety Events. Final Report (Prepared by RTI International and Consumers Advancing Patient Safety under Contract No. 290-06-00001-5). AHRQ Publication No. 11-0060-EF. Rockville, MD: 2011. [Google Scholar]
- 17.Hibbard JH, Greene J, Overton V. Patients with lower activation associated with higher costs; delivery systems should know their patients’ “scores”. Health Aff (Millwood) 2013;32(2):216–222. doi: 10.1377/hlthaff.2012.1064. [DOI] [PubMed] [Google Scholar]
- 18.Robbennolt J. Apologies and Medical Error. Clin Orthop Relat Res. 2009;467(2):376–382. doi: 10.1007/s11999-008-0580-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weingart SN, Zhu J, Chiappetta L, et al. Hospitalized patients’ participation and its impact on quality of care and patient safety. Int J Qual Heal care. 2011;23(3):269–277. doi: 10.1093/intqhc/mzr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality. [Accessed January 30, 2018];Improving Patient Safety Through Learning Laboratories. Content last reviewed December 2017. https://www.ahrq.gov/professionals/quality-patient-safety/ps-learning-labs.html.
- 21.Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) [Accessed June 30, 2017];HCAHPS Summary Analysis. http://www.hcahpsonline.org/SummaryAnalyses.aspx. Published 2017.