Abstract
Aims:
To examine factors that affect cost-related medication non-adherence (CRN), defined as taking medication less than as prescribed because of cost, among adults with diabetes and to determine their relative contribution in explaining CRN.
Methods:
Behavioral Risk Factor Surveillance System data for 2013–2014 were used to identify individuals with diabetes and their CRN. We modeled CRN as a function of financial factors, regimen complexity, and other contextual factors including diabetes care, lifestyle, and health factors. Dominance analysis was performed to rank these factors by relative importance.
Results:
CRN among U.S. adults with diabetes was 16.5%. Respondents with annual income <$50,000 and without health insurance were more likely to report CRN, compared to those with income ≥$50,000 and those with insurance, respectively. Insulin users had 1.24 times higher risk of CRN compared to those not on insulin. Contextual factors that significantly affected CRN included diabetes care factors, lifestyle factors, and comorbid depression, arthritis, and COPD/asthma. Dominance analysis showed health insurance was the most important factor for respondents <65 and depression was the most important factor for respondents ≥65.
Conclusions:
In addition to traditional risk factors of CRN, compliance with annual recommendations for diabetes and healthy lifestyle were associated with lower CRN. Policies and social supports that address these contextual factors may help improve CRN.
Keywords: Medication adherence, Diabetes, Income, Insurance, Lifestyle
Introduction
Approximately 30.3 million people in the U.S. have diabetes [1]. Poor medication adherence is a common phenomenon among patients with diabetes [2]. The American Diabetes Association (ADA) estimated that patients with diabetes spent 27% ($3,734 per patient in 2012) of direct medical costs for outpatient medications and supplies [3]. The high cost of diabetes care is associated with medication non-adherence [4–6], which results in poor clinical outcomes [7,8]. Patients with diabetes often have comorbidities that require medications in addition to oral and injectable diabetes medications. The complex polypharmacy regimens increase cost burden in acquiring prescribed medications, which can play a role in reducing medication adherence [9–11].
Cost-related medication non-adherence (CRN), defined as taking medication less than as prescribed because of cost, has been found to be between 16% and 19% among patients with diabetes [12,13]. For low-income individuals with diabetes, CRN may become a serious issue in managing their blood glucose and comorbid conditions that can potentially lead to further economic disparities in diabetic complications and mortality. Studying factors that affect CRN may help identify policies that could improve adherence to medication. In previous research, numerous factors have been examined and found to affect CRN [13–17]. However, it is still not clear whether medication non-adherence can truly be reduced if financial burden is lifted through insurance coverage or other fiscal policies or if there are other factors that may need to be addressed before any fiscal policies may take effect. A study on the relative importance of these factors may help in prioritizing policies for reducing CRN.
The primary objective of this study is to examine both financial and non-financial factors that affect CRN among patients with diabetes. Our secondary objective is to determine the relative contribution of factors in explaining CRN. Our hypothesis is that contextual factors (e.g., diabetes care, lifestyle, comorbidities) are significant predictors of CRN, independent of financial factors and regimen complexity.
2. Methods
2.1. Research design and study population
Our study population consisted of all persons with diabetes who used prescription medications in the U.S. in 2013–2014. We derived our study sample from the Behavioral Risk Factor Surveillance System (BRFSS), an annual telephone survey of U.S. adults about their health, chronic conditions, and preventive care utilization. The study sample included all persons with self-reported diabetes who took at least one prescription medication and resided in states that implemented the ‘Diabetes Module” in 2013 and 2014 in which questions regarding diabetes care and preventive services utilization were asked. The states included in this study are shown in Table A (Supplemental Material) along with the number of eligible respondents by year. Twenty-three and 16 states and District of Columbia (D.C.) were included in 2013 and 2014, respectively.
2.2. Main outcome
Our main outcome was the CRN. In 2013 and 2014, the BRFSS included the following question: ‘Was there a time in the past 12 months when you did not take your medication as prescribed because of cost? Do not include over-the-counter medication.” The medications were not limited to antidiabetic agents.
2.3. Conceptual model for CRN
Fig. 1 shows a conceptual model of the factors that can potentially impact CRN, adapted from Zivin et al. [13] and Piette et al. [11]. The model includes financial factors, regimen complexity, demographic factors, socioeconomic status, and ‘contextual factors” including diabetes care factors, lifestyle factors, and health factors. We conceptualize that financial factors and regimen complexity are the two main determinants of CRN and other ‘contextual factors” can modify their effects.
Fig. 1 –
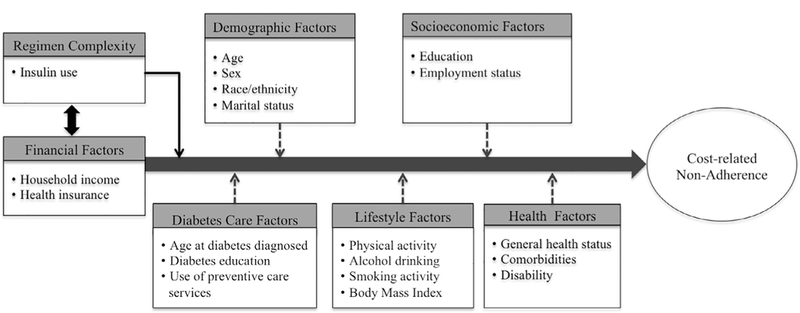
Conceptual framework for factors associated with patients’ risk of cost-related non-adherence (adapted from Piette et al. [9]).
Financial factors include household income and health insurance. Household income is the key variable for financial wherewithal to pay for prescription medications. Health insurance indicates whether the respondent has any health care coverage including any private or public health insurance plans including Medicare.
Previous studies used the number of different prescription medications as an indicator of regimen complexity [13], but BRFSS does not collect this information. Instead, we used insulin use as a proxy measure of medication regimen complexity in this study. For type 2 diabetes, insulin is recommended as a second-line agent with or without oral medications [18,19]. While it is effective in lowering blood glucose, it complicates a patient’s treatment regimen and increases overall treatment burden [20,21]. Medication regimens involving insulin may be complex because of injectable administration, variable dosing, and potentially fatal side effects such as hypoglycemia [22,23].
Demographic factors included age, race/ethnicity (Non- Hispanic [NH] White, NH Black, Hispanic, Other/Unknown), sex, and marital status (married or living with significant other vs not married or living alone). We decided to exclude patients whose ages were not reported from the study sample because they were too few to be meaningfully analyzed as a separate ‘Unknown” group (n = 423). Socioeconomic status included educational attainment and employment status. Educational attainment is a proxy for health literacy which in turn is known to be associated with drug adherence [24]. Employment status was coded into four categories: employed, not employed, retired, and not in the workforce or unknown.
Diabetes care factors included age at diabetes diagnosis and whether the respondent had used diabetes preventive care services that the ADA recommends [19]. The preventive care services included in this study are diabetes selfmanagement education (at least once), daily blood glucose self-monitoring, daily foot self-check, annual physician visit for diabetes, 2 or more A1c tests per year, annual foot exam, and annual eye exam [19]. These diabetes care factors are specific to patients with diabetes, involve self-care or care received from medical providers, and represent the level of engagement the patient has with their care of diabetes.
Lifestyle factors included body mass index, alcohol drinking in the last 30 days, smoking (never, past, current, and unknown), and any leisure time exercises or physical activities in the past month. These are related to modifiable habits and styles of life that affect health. Health factors included general health status, existing comorbid conditions, and disability. Comorbidities collected in the 2013–2014 BRFSS included heart attack, coronary heart disease, stroke, arthritis, asthma or chronic obstructive pulmonary disease (COPD), depression, skin and other cancers. Depression indicates a depressive disorder, including major and minor depression and dysthymia. Disability which indicates whether the respondent had any activity limitations because of physical, mental, or emotional problems was also included.
2.4. Statistical analysis
We excluded respondents who answered 3 (‘No medication was prescribed”), 7 (‘Don’t know/Not sure”), or 9 (‘Refused”) to the question about CRN (shown in the Main outcome section) from the analysis. This question was not asked of approximately one fourth of all respondents (n = 132,921) who responded that they did not take any prescription medications and were also excluded. For the remaining respondents, 1 (‘Yes”) was coded as indicating CRN and 2 (‘No”) as indicating that CRN was not present.
To account for the complex sampling design in the BRFSS, we conducted all statistical analyses using the Survey suite of programs in Stata SE version 14 (StataCorp, College Station, TX). Survey weights were applied to obtain population-level estimates, and subpopulation methods were used to obtain correct estimation of standard errors for subgroup analyses as well as to correctly account for exclusions [25,26].
Weighted multivariable logistic regressions were used to estimate odds ratios associated with each covariate included in the model. The full model included all covariates, including financial, regimen complexity, demographic, socioeconomic, diabetes care, lifestyle, and health factors.
To determine relative importance of predictors of CRN, we used dominance analysis developed by Azen and Budescu (2003) [27] and Azen and Traxel (2009) [28]. Unlike other methods of computing relative importance, dominance analysis provides meaningful numerical measures of relative contribution of each variable in explaining CRN [29] that can be standardized to the amount of CRN explained in the percentage scale. Luchman (2015) showed that dominance analysis can be applied to complex surveys by using the survey weights as probability weights in logistic regression models [30].
For dominance analysis, we included all factors that were statistically significant in multivariable logistic regressions, including household income or regimen complexity along with other contextual factors such as lifestyle factors, health factors, and diabetes care factors [11,13]. We combined annual foot exams and annual eye exams as one factor (‘Diabetes Care”) and exercise, smoking, drinking, and BMI as another factor (‘Lifestyle”) in dominance analysis. While each of these factors is important individually and the magnitude of their importance may vary, we decided to group these variables to reduce the number of subset regression models and provide more interpretable results.
Medicare beneficiaries have the opportunity to sign up for prescription drug coverage through Part D or a Medicare Advantage Plan. They may have different financial pressures than their younger counterparts without health insurance. To compare CRN between the populations, we estimated two full models for respondents with ages <65 years and those with ages 65 or older. We also conducted dominance analyses for these two groups separately to determine whether the factors rank differently in the two groups.
This study was exempt from IRB review because the BRFSS data is a public use data set.
3. Results
In 2013 and 2014, 956,437 persons responded to the BRFSS surveys, of whom 12.9% reported as having diabetes. After survey weights were applied, diabetes prevalence in these two years was 10.4% of the US adult population. After exclusions, there were 44,925 respondents from 25 states and the D.C. in the final sample.
Table 1 shows weighted percentages of respondents with CRN by individual characteristics. Overall, about 16.5% of respondents with diabetes who took prescription medications answered that they had not taken medications as prescribed because of cost in the past 12 months. CRN was much higher among respondents with diabetes than those without diabetes (9.9%) in the 2013–2014 BRFSS (p < 0.001). In contrast, in 2013 BRFSS, CRN was 13.0% and 10.1% for respondents with high and normal cholesterol levels and 13.8% and 9.5% forpersons with hypertensive and normotensive patients (both p < 0.001), respectively. Persons who were non-elderly, female, Hispanic, and not married or living alone had higher CRN. Also, individuals with better socioeconomic status in terms of education and employment showed lower CRN. As expected, CRN in patients with diabetes was affected by financial factors and regimen complexity. The CRN rate decreased as the annual household income level increased (24.4% for < $15,000 to 8.9% for $50,000 or more, p < 0.001), and CRN of individuals without health insurance was more than triple the rate of those with insurance (42.1% vs. 13.8%, p < 0.001). Individuals on insulin reported higher CRN compared to those without insulin treatment (19.9% vs. 14.9%, p < 0.001).
Table 1–
Respondent characteristics and weighted percentage of cost-related medication non-adherence, U.S. adults with diabetes,2013–2014 (N=44,925)
| Variables | Weighted percentage of nonadherence | P-Value* |
|---|---|---|
| Overall | 16.54% | |
| Financial Factors | ||
| Household Income | ||
| <$15k | 24.41% | <0.001 |
| 1Sk-24.9k | 22.10% | |
| 2Sk-34.9k | 18.58% | |
| 3Sk-49.9k | 14.69% | |
| $S0 k or more | 8.91% | |
| Unknown | 13.S1% | |
| Health Insurance | ||
| Yes | 13.76% | <0.001 |
| No | 42.13% | |
| Unknown | 14.S0% | |
| Regimen Complexity | ||
| Insulin Use | ||
| No | 14.93% | < 0.001 |
| Yes | 19.89% | |
| Demographic Factors | ||
| Age, y | ||
| <SS | 27.77% | <0.001 |
| SS-64 | 18.46% | |
| 6S-7S | 9.06% | |
| 7S or older | 4.34% | |
| Sex | ||
| Female | 19.35% | <0.001 |
| Male | 13.68% | |
| Race/ethnicity | ||
| NH White | 14.36% | <0.001 |
| NH Black | 20.43% | |
| Hispanic | 23.55% | |
| Other/Unknown | 16.25% | |
| Marital Status | ||
| Living Alone | 18.67% | <0.001 |
| Married or Living with SO | 14.89% | |
|
Socioeconomic Status Education | ||
| <High School | 20.12% | <0.001 |
| Some High School | 22.22% | |
| High School Grad or GED | 1S.75% | |
| Some College | 16.82% | |
| College or More | 11.12% | |
| Employment Status | ||
| Employed/self-employed | 18.12% | <0.001 |
| Not employed | 34.32% | |
| Retired | 7.29% | |
| Not in the workforce | 23.94% | |
|
Diabetes Care Factors Age at diabetes dx | ||
| <4S y | 28.05% | <0.001 |
| 4S-S4 | 19.91% | |
| SS-64 | 14.20% | |
| 6S or older | 6.54% | |
| Unknown | 13.16% | |
| Diabetes education | ||
| No | 16.30% | 0.528 |
| Yes | 16.75% | |
| Daily BG self check | ||
| No | 16.08% | 0.312 |
| Yes | 16.81% | |
| Daily feet self check | ||
| No | 1S.66% | 0.056 |
| Yes | 17.06% | |
| Annual doctor visit | ||
| No | 18.S8% | 0.018 |
| Yes | 16.19% | |
| >2 A1c tests last year | ||
| No | 19.19% | < 0.001 |
| Yes | 1S.14% | |
| Annual foot exam | ||
| No | 20.51% | <0.001 |
| Yes | 14.88% | |
| Annual eye exam | ||
| No | 24.52% | <0.001 |
| Yes | 12.47% | |
|
Lifestyle Factors Exercise | ||
| No | 18.04% | <0.001 |
| Yes | 1S.44% | |
| Drinking | ||
| No | 16.84% | 0.214 |
| Yes | 1S.85% | |
| Smoking | ||
| Never | 16.12% | <0.001 |
| Past | 12.68% | |
| Current | 25.97% | |
| Unknown | 17.14% | |
| Body Mass Index | ||
| <25 kg/m2 | 13.46% | <0.001 |
| 25–29.9 | 13.36% | |
| 30 or above | 19.00% | |
| Unknown | 18.25% | |
|
Health Factors General Health | ||
| Fair or Poor | 23.03% | <0.001 |
| Good, Very Good or Excellent | 10.98% | |
| Heart Attack | ||
| No | 16.41% | 0.342 |
| Yes | 17.23% | |
| CHD | ||
| No | 16.32% | 0.082 |
| Yes | 17.82% | |
| Stroke | ||
| No | 16.40% | 0.189 |
| Yes | 17.85% | |
| Skin Cancer | ||
| No | 17.21% | <0.001 |
| Yes | 10.61% | |
| Other Cancer | ||
| No | 16.76% | 0.047 |
| Yes | 14.88% | |
| COPD/Asthma | ||
| No | 14.12% | <0.001 |
| Yes | 23.34% | |
| Arthritis | ||
| No | 14.51% | <0.001 |
| Yes | 18.45% | |
| Depression | ||
| No | 12.28% | <0.001 |
| Yes | 27.88% | |
| Chronic Kidney Disease | ||
| No | 16.26% | 0.011 |
| Yes | 19.28% | |
| Disability | ||
| No | 12.91% | <0.001 |
| Yes | 22.02% | |
P-values were based on Pearson design-based corrected chisquare statistic.
Contextual factors other than the main determinants were also significantly associated with CRN. Individuals who received the annual recommended preventive care exams showed significantly lower CRN than individuals who did not receive those exams. Respondents with a healthy lifestyle tended to have lower CRN than those without. Furthermore, there were notable differences between CRN among patients with and without certain comorbidities, such as COPD/ asthma, arthritis, depression, chronic kidney disease, and disability.
Table 2 shows the results from the multivariable logistic regression model adjusting for all factors shown in Fig. 1. Financial factors and regimen complexity had a significant impact on CRN. Increased household income was associated with decreased CRN (p for trend <0.001). Compared to respondents whose annual household income was $50,000 or more, those whose household income was <$50,000 had 1.8 to 2.3 times higher likelihood of having CRN. Respondents who did not have health insurance were 2.2 times (OR = 2.21; 95% CI, 1.88–2.60) more likely to experience CRN, compared to those with the insurance. In addition, respondents who were on insulin had 1.2 times (OR = 1.23; 95% CI, 1.07–1.40) higher risk of CRN compared to those who were not treated with insulin.
Table 2–
Odds rations and their 95% confidence intervals for cost-related medication non-adherence among U.S. diabetes, 2013–2014*.
| Variables | OR (95% CI) | P-Value | |
|---|---|---|---|
|
Financial Factors Household Income [≥$50k] | |||
| <$15k | 1.879 | (1.516–2.331) | <0.001 |
| $15k-$24.9k | 2.268 | (1.873–2.747) | <0.001 |
| $25k-$34.9k | 2.224 | (1.817–2.722) | <0.001 |
| $35k-$49.9k | 1.838 | (1.473–2.294) | <0.001 |
| Unknown | 1.575 | (1.280–1.937) | <0.001 |
| Health Insurance [Has Insurance] | |||
| No Insurance | 2.212 | (1.884–2.597) | <0.001 |
| Unknown | 1.016 | (0.453–2.277) | 0.969 |
| Regimen Complexity | |||
| Insulin Use | 1.226 | (1.073–1.401) | 0.003 |
|
Demographic Factors
Age [75 or older] | |||
| <55 | 3.797 | (2.959–4.872) | <0.001 |
| 55–64 | 2.791 | (2.224–3.504) | <0.001 |
| 65–74 | 1.911 | (1.553–2.351) | <0.001 |
| Male | 0.737 | (0.657–0.828) | <0.001 |
| Race/ethnicity [NH White] | |||
| NH Black | 1.265 | (1.100–1.455) | 0.001 |
| Hispanic | 1.191 | (0.974–1.457) | 0.089 |
| Other/Unknown | 1.059 | (0.849–1.321) | 0.613 |
| Married [Living alone] | 1.129 | (1.007–1.265) | 0.037 |
|
Socioeconomic Factors
Education [<High School] | |||
| Some High School | 0.938 | (0.716–1.228) | 0.642 |
| High School Grad or GED* | 0.852 | (0.666–1.089) | 0.201 |
| Some College | 0.983 | (0.766–1.262) | 0.894 |
| College or More | 0.907 | (0.690–1.193) | 0.485 |
| Employment [Employed] | |||
| Not employed | 1.092 | (0.881–1.352) | 0.423 |
| Retired | 0.612 | (0.521–0.719) | <0.001 |
| Not in the workforce/unknown | 0.691 | (0.589–0.811) | <0.001 |
|
Diabetes Care Factors Age at diabetes diagnosis [<45y] | |||
| 45–54 | 0.768 | (0.656–0.899) | 0.001 |
| 55–64 | 0.753 | (0.639–0.887) | 0.001 |
| 65 or older | 0.669 | (0.545–0.820) | <0.001 |
| Unknown | 0.718 | (0.554–0.929) | 0.012 |
| Diabetes education | 1.043 | (0.927–1.173) | 0.486 |
| Daily BG* self check | 0.981 | (0.862–1.117) | 0.773 |
| Daily feet self check | 1.047 | (0.934–1.174) | 0.430 |
| Annual doctor visit | 1.096 | (0.933–1.289) | 0.265 |
| ≥2 A1c* tests last year | 0.911 | (0.808–1.027) | 0.128 |
| Annual foot exam | 0.810 | (0.715–0.918) | 0.001 |
| Annual eye exam | 0.653 | (0.584–0.729) | <0.001 |
| Lifestyle Factors | |||
| Exercise | 1.049 | (0.938–1.173) | 0.400 |
| Drinking | 1.154 | (1.016–1.311) | 0.027 |
| Smoking [Never] | |||
| Past | 0.876 | (0.773–0.993) | 0.039 |
| Current | 1.024 | (0.882–1.189) | 0.755 |
| Unknown | 1.097 | (0.820–1.468) | 0.534 |
| BMI* [<25kg/m2] | |||
| 25–29.9 | 1.066 | (0.886–1.282) | 0.498 |
| 30 or above | 1.187 | (1.000–1.409) | 0.050 |
| Unknown | 1.082 | (0.833–1.405) | 0.555 |
| Health Factors | |||
| General Health Fair or Poor | 1.602 | (1.409–1.821) | <0.001 |
| Heart Attack | 1.131 | (0.958–1.334) | 0.145 |
| CHD* | 1.151 | (0.986–1.344) | 0.074 |
| Stroke | 0.945 | (0.804–1.111) | 0.493 |
| COPD*/Asthma | 1.215 | (1.080–1.366) | 0.001 |
| Skin Cancer | 1.040 | (0.866–1.249) | 0.675 |
| Other Cancer | 1.128 | (0.975–1.306) | 0.106 |
| Arthritis | 1.269 | (1.127–1.429) | <0.001 |
| Depression | 1.644 | (1.461–1.849) | <0.001 |
| Chronic Kidney Disease | 1.048 | (0.887–1.239) | 0.581 |
| Disability | 1.322 | (1.161–1.504) | <0.001 |
NH = non-Hispanic; GED = general educational development; BG = blood glucose; A1c = glycated hemoglobin; BMI = body mass index; CHD =coronary heart disease; COPD = chronic obstructive
Among the demographic factors, age, gender, race/ethnicity were significantly associated with CRN. The youngest respondent group (age < 55) had approximately 4 times (OR = 3.80; 95% CI, 2.96–4.87) higher probability of CRN compared to the oldest group (age ≥ 75). Significant racial/ethnic disparities observed for NH black respondents (OR = 1.27; 95% CI, 1.10–1.46) compared to NH whites.
Diabetes care factors strongly predicted CRN even after adjusting for financial, regimen complexity, and demographic factors. For respondents who received annual recommended preventive care activities such as annual foot and eye exams, the risk of CRN was reduced by 35% and 19%, respectively, compared to those who did not. However, effects of A1c tests, diabetes education, or self-care practices on CRN were not statistically significant. Except for exercise, lifestyle factors were also significant determinants of CRN. Respondents who reported drinking were 1.15 times more likely to have CRN (OR = 1.15; 95% CI, 1.02–1.31) compared to those who did not drink. Compared to respondents with normal weight, obese respondents had about 19% higher risk of CRN (OR = 1.19; 95% CI, 1.00–1.41).
General health status was highly associated with CRN. Compared to those who were in good, very good, or excellent health or did not have disability, CRN were 60% higher (OR = 1.60; 95% CI, 1.41–1.82) for individuals who were in fair or poor health and 32% higher (OR = 1.32; 95% CI, 1.16–1.50) for individuals with disability. Patients who had COPD/asthma, arthritis, or depression also had significantly higher risk of CRN, compared to those without these comorbidities.
Age-stratified logistic regressions for respondents aged <65 and ≥ 65 years (Table B in the Supplemental Material) indicated that income effect was stronger among the elderly than the younger group, while insurance effect was stronger among the younger group. The results also showed that the ethnic disparities between Hispanics and NH Whites do not exist in the elderly population.
Table 3 shows results both unstandardized and standardized general dominance statistics from dominance analysis. As expected, two financial factors, health insurance and household income, topped the list for respondents <65 years of age, while depression had the largest effect on CRN among respondents ≥ 65 years, followed by household income. These top 2 factors accounted for 30% and 37% of the relative importance in explaining CRN for the younger and older groups, respectively. Depression also ranked 5th out of 15 for the younger group with a standardized dominance of about 9%. General health status ranked 3rd for the younger and 4th for the older groups, while demographic factors such as race/ethnicity and sex and insulin use, an indicator of regimen complexity, ranked toward the bottom of the list. Comorbid conditions such as COPD/asthma and disabilityranked high (5th and 6th) for the older group but ranked much lower for the younger group. Lifestyle factors including smoking, drinking, exercise, and BMI ranked 9th and 10th for the older and younger groups, respectively, with dominance <5%. In the combined analysis shown in Table C in the Online-Only Appendix, age ranked number one, followed by health insurance, employment status. Depression ranked 5th, while general health and lifestyle factors ranked 8th and 9th.
Table 3–
General dominance statistics and ranked list of the determinants of cost-related medication non-adherence*.
| Variables | Age < 65 y |
Age ≥ 65 y |
||||
|---|---|---|---|---|---|---|
| Dominance Statistic |
Ranking | Dominance Statistic |
Ranking | |||
| Unstandardized | Standardized | Unstandardized | Standardized | |||
| Health Insurance | 0.0284 | 0.1705 | 1 | 0.0007 | 0.0068 | 15 |
| Household Income | 0.0215 | 0.1290 | 2 | 0.0162 | 0.1550 | 2 |
| General Health | 0.0178 | 0.1073 | 3 | 0.0064 | 0.0610 | 4 |
| Diabetes Care Factors | 0.0164 | 0.0987 | 4 | 0.0044 | 0.0423 | 10 |
| Depression | 0.0147 | 0.0883 | 5 | 0.0221 | 0.2119 | 1 |
| Age at DM* Diagnosis | 0.0144 | 0.0863 | 6 | 0.0043 | 0.0413 | 11 |
| Employment Status | 0.0133 | 0.0797 | 7 | 0.0051 | 0.0488 | 8 |
| Disability | 0.0126 | 0.0758 | 8 | 0.0057 | 0.0544 | 6 |
| Age | 0.0066 | 0.0395 | 9 | 0.0133 | 0.1273 | 3 |
| Lifestyle Factors | 0.0058 | 0.0348 | 10 | 0.0050 | 0.0483 | 9 |
| Arthritis | 0.0041 | 0.0248 | 11 | 0.0029 | 0.0279 | 14 |
| Sex | 0.0035 | 0.0210 | 12 | 0.0054 | 0.0519 | 7 |
| COPD*/Asthma | 0.0031 | 0.0189 | 13 | 0.0059 | 0.0563 | 5 |
| Race/Ethnicity | 0.0024 | 0.0143 | 14 | 0.0030 | 0.0286 | 13 |
| Insulin Use | 0.0019 | 0.0113 | 15 | 0.0040 | 0.0381 | 12 |
COPD = chronic obstructive pulmonary disease; DM = diabetes. Diabetes care factors include annual foot exam and annual eye exam; lifestyle factors include physical exercise, alcohol drinking, smoking, and body mass index.
4. Discussion
Our results show that household income and health insurance were the most important factors in explaining CRN for younger adults <65 years of age, while depression dominated all other factors for the elderly with over 21% of CRN explained by this single factor followed by household income.
Depression ranked fifth for the younger adults. When both age groups were combined, age had the largest contribution to CRN of all predictors with individuals <55 years of age having four times higher non-adherence than those ≥75 years.
Depression is a well-known predictor of poor treatment adherence among patients with chronic diseases in general [14,31] and diabetes in particular [32]. It has also been recognized as a strong predictor of CRN among the elderly [14,33]. However, our study was the first to show that depression is the most influential factor for explaining CRN for the elderly patients with diabetes. We do not have a good explanation about whether it is additional cost burden that antidepressants place on patients or escalation of treatment non-adherence due to the condition compounded by costs that makes depression such an important determinant of CRN among the elderly. However, this result reinforces the importance of looking at medical and social challenges the elderly with depression face in order to decrease CRN.
To our best knowledge, this is the first study that showed that individuals who comply with ADA preventive care recommendations have significantly lower CRN. This finding suggests that CRN among patients with diabetes may also be a function of patient engagement/activation that sets medication adherence as a priority. Lack of knowledge or awareness on the importance of treatment adherence does not appear to be a reason for CRN in our data, because the receipt of diabetes education was not statistically significant in the adjusted model. Rather, actively involving patients in their own care may help patients increase medication adherence by enhancing their understanding of the importance of medication adherence for effective diabetes management. It is noteworthy that diabetes care factors ranked fourth with almost 10% relative contribution for the younger group but they were much less important for the elderly. This may mean that patient engagement is much more important for the younger than the older patients in reducing CRN.
We used insulin use as an indicator of regimen complexity, apart from the other diabetes care factors. Our findings that insulin use was significantly associated with higher CRN but it ranks at the bottom in dominance ranking suggest that non-adherence of insulin use may be related less to costs than to other factors such as injection site reactions, fear of hypoglycemia, and injections interfering with daily activities, meal planning and physical activity [34]. Recent report on the tripling of insulin price in 2002–2013 in the U.S., however, raises concerns about whether insulin costs may be an increasingly important issue for medication non-adherence in the future [35].
Other factors significantly associated with CRN included such non-modifiable factors as sex and race/ethnicity. Our results showed significantly higher CRN among women than men. This gender disparity in CRN is well documented and has been found among the Medicare beneficiaries [36], older patients with diabetes [17], and cancer survivors [37]. Also, our findings on the racial disparity in CRN between NH black and NH white were consistent with previous studies [36,38,39]. While our study did not indicate a significance gap in CRN between Hispanics and NH white, Frankenfield et al. (2010) [40] found a higher prevalence of CRN among Hispanic Medicare enrollees compared to non-Hispanics. Our findings along with these previous studies suggest that social support and fiscal policies should be promoted to reduce the disparities and help these vulnerable populations avert CRN.
Our finding that CRN is decreasing as patients age is consistent with previous studies [13,41]. It is interesting, however, that the elderly in our study were affected more by their income than the non-elderly with respect to CRN. It may be due to the financial burden that Medicare Part D ‘donut holes” or Part B deductibles and copayments place on the elderly persons with diabetes when they obtain diabetes medications and/or renew their prescriptions. Previous studies have shown that older Black patients are significantly more reliant on Medicare Part D for prescription drugs [42,43] and experienced more CRN than Whites when they reach the coverage limit [44]. Bakk (2015) [36] in particular showed that racial disparities in CRN was mediated by whether patients reached the coverage gap.
In our data, CRN among U.S. adults with diabetes was 16.5% based on 2013–2014 national surveys. This high CRN prevalence rate among adults with diabetes was consistent with other studies although these previous studies used a smaller sample size. A study based on a sample of 875 persons with diabetes who were aged ≥ 50 years reported that 19% had cut back on medication use due to cost [12]. Another study of a sample of 245 patients who were using medications for both diabetes and chronic pain reported that over 30% of the sample had cut back on their medications for cost- related reasons [15]. A study of 1264 Medicare Part D patients with diabetes who hit the ‘donut hole” at the end of 2006 reported that about 16% had CRN [16]. Finally, a study of Health and Retirement Survey respondents with diabetes aged ≥50 years reported a CRN rate of 18% [17].
As policy implications, our results suggest that improved compliance with ADA recommended care may be important for the younger patients on top of addressing financial where withal for acquiring prescription medications. Our results further suggest that the elderly are experiencing huge differential in CRN by their household income. It is important to examine whether Medicare Part D ‘donut holes” are to blame for the income-related CRN for the elderly patients. Under the current Affordable Care Act, this issue will be resolved when the ‘donut hole” is eliminated altogether by 2020. If and when the ACA is repealed, however, an alternative way of funding Part D to close this gap may be important as far as CRN for elderly patients with diabetes is concerned.
This study has several limitations. First, since this study was conducted in the U.S., our results may not be applied to other countries where financing for health care, drug prices, and affordability are different. Second, it is based on survey data in which response biases such as recall bias or social desirability bias may have affected the results. Third, the BRFSS survey did not collect data on several factors that have traditionally been strong predictors of CRN, including the number of prescription medications, out-of-pocket expenses on prescription medication, and whether respondents were taking diabetes medications other than insulin. These variables could impact results of CRN one way or the other. While this is the first CRN study using a national survey sample data that may reduce uncertainties in results of previous studies with smaller sample datasets, the BRFSS surveys implemented the Diabetes Module in about half of the states in 2013 and 2014. More complete data may provide better national estimates on CRN. Finally, the survey did not include a non-adherence question specific to diabetes medications, so CRN in this study includes both diabetes and other medications. The data also did not differentiate between type 1 and type 2 diabetes. Considering relatively higher insulin use in type 1 patients, who are likely to be younger, compared to type 2 patients, our conceptual model that uses insulin use as a proxy for medication regimen complexity may bias the results with respect to age and medication complexity.
5. Conclusion
CRN prevalence among U.S. adults with diabetes was 16.5% in 2013–2014. Depression and household income for respondents aged ≥65 years and health insurance and household income for those <65 years were the most important determinants of CRN. In addition to traditional risk factors of CRN, we showed that contextual factors such as compliance with ADA recommendations and healthy lifestyle were also associated with lower CRN. Policies and social supports that address the significant contextual factors may help improve CRN.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the financial support from the Agency for Healthcare Research and Quality (R01HS018542) and the National Institute of Diabetes, Digestive, and Kidney Diseases (R01DK113295). The paper presents the findings and conclusions of the authors; it does not necessarily represent the Agency for Healthcare Research and Quality or the National Institutes of Health.
Funding source
Agency for Healthcare Research and Quality (1R01HS018542) and NIH/NIDDK (1R01DK113295)
Footnotes
Conflict of Interest
The authors have no conflicts of interest to report.
Appendix A. Supplementary material
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.diabres.2018. 06.016.
REFERENCES
- [1].Centers for Disease Control and Prevention. National diabetes statistics report, 2017; 2017.
- [2].Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med 2015;32:725–37. [DOI] [PubMed] [Google Scholar]
- [3].American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Aikens JE, Piette JD. Longitudinal association between medication adherence and glycaemic control in Type 2 diabetes. Diabet Med 2013;30:338–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Garcia-Perez LE, Alvarez M, Dilla T, Gil-Guillen V, Orozco- Beltran D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther 2013;4:175–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 2005;43:521–30. [DOI] [PubMed] [Google Scholar]
- [7].Casagrande SS, Cowie CC, Genuth SM. Self-reported prevalence of diabetes screening in the U.S., 2005–2010. Am J Prev Med 2014;47:780–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Polonsky WH. Poor medication adherence in diabetes: What’s the problem? J Diabetes 2015;7:777–8. [DOI] [PubMed] [Google Scholar]
- [9].Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 2004;27:2154–60. [DOI] [PubMed] [Google Scholar]
- [10].Kerr EA, Gerzoff RB, Krein SL, Selby JV, Piette JD, Curb JD, et al. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: the TRIAD study. Ann Intern Med 2004;141:272–81. [DOI] [PubMed] [Google Scholar]
- [11].Piette JD, Heisler M, Horne R, Caleb Alexander G. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med 2006;62:846–57. [DOI] [PubMed] [Google Scholar]
- [12].Piette JD, Heisler M, Wagner TH. Problems paying out-of pocket medication costs among older adults with diabetes. Diabetes Care 2004;27:384–91. [DOI] [PubMed] [Google Scholar]
- [13].Zivin K, Ratliff S, Heisler MM, Langa KM, Piette JD. Factors influencing cost-related nonadherence to medication in older adults: a conceptually based approach. Value Health 2010;13:338–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zivin K, Madden JM, Graves AJ, Zhang F, Soumerai SB. Cost- related medication nonadherence among beneficiaries with depression following Medicare Part D. Am J Geriatr Psychiatry 2009;17:1068–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kurlander JE, Kerr EA, Krein S, Heisler M, Piette JD. Cost- related nonadherence to medications among patients with diabetes and chronic pain: factors beyond finances. Diabetes Care 2009;32:2143–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Williams J, Steers WN, Ettner SL, Mangione CM, Duru OK. Cost-related nonadherence by medication type among Medicare Part D beneficiaries with diabetes. Med Care 2013;51:193–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Zhang JX, Lee JU, Meltzer DO. Risk factors for cost-related medication non-adherence among older patients with diabetes. World J Diabetes 2014;5:945–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, et al. Consensus Statement by the American association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm - 2017 executive summary. Endocr Prac. 2017;23:207–38. [DOI] [PubMed] [Google Scholar]
- [19].American Diabetes Association. Standards of medical care in diabetes - 2017. Diabetes Care 2017;40:S1–S129.27979885 [Google Scholar]
- [20].Petznick A Insulin management of type 2 diabetes mellitus. Am Fam Phys 2011;84:183–90. [PubMed] [Google Scholar]
- [21].Inzucchi SE, Tunceli K, Qiu Y, Rajpathak S, Brodovicz KG, Engel SS, et al. Progression to insulin therapy among patients with type 2 diabetes treated with sitagliptin or sulphonylurea plus metformin dual therapy. DiabetesObes Metab 2015;17:956–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wimmer BC, Bell JS, Fastbom J, Wiese MD, Johnell K. Medication regimen complexity and polypharmacy as factors associated with all-cause mortality in older people: a population-based cohort study. Ann Pharmacother 2016;50:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Swinnen SG, Hoekstra JB, DeVries JH. Insulin therapy for type 2 diabetes. Diabetes Care 2009;32(Suppl 2):S253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Noureldin M, Plake KS, Morrow DG, Tu W, Wu J, Murray MD. Effect of health literacy on drug adherence in patients with heart failure. Pharmacotherapy 2012;32:819–26. [DOI] [PubMed] [Google Scholar]
- [25].Rao J Small area estimation. Hoboken, New Jersey: John Wiley & Sons, Inc; 2003. [Google Scholar]
- [26].Graubard BI, Korn EL. Survey inference for subpopulations. Am J Epidemiol 1996;144:102–6. [DOI] [PubMed] [Google Scholar]
- [27].Azen R, Budescu DV. The dominance analysis approach for comparing predictors in multiple regression. Psychol Methods 2003;8:129–48. [DOI] [PubMed] [Google Scholar]
- [28].Azen R, Traxel N. Using dominance analysis to determine predictor importance in logistic regression. J Educ Behav Statist 2009;34:319–47. [Google Scholar]
- [29].Gromping U Estimators of relative importance in linear regression based on variance decomposition. Am Stat 2007;61:139–47. [Google Scholar]
- [30].Luchman J Determining subgroup difference importance with complex survey designs: an application of weighted dominance analysis. Survey Practice 2015;8:1–10. [Google Scholar]
- [31].Grenard JL, Munjas BA, Adams JL, Suttorp M, Maglione M, McGlynn EA, et al. Depression and medication adherence in the treatment of chronic diseases in the United States: a meta-analysis. J Gen Intern Med 2011;26:1175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care 2008;31:2398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Bambauer KZ, Safran DG, Ross-Degnan D, Zhang F, Adams AS, Gurwitz J, et al. Depression and cost-related medication nonadherence in Medicare beneficiaries. Arch Gen Psychiatry 2007;64:602–8. [DOI] [PubMed] [Google Scholar]
- [34].Sarbacker GB, Urteaga EM. Adherence to insulin therapy. DiabetesSpectr 2016;29:166–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Cefalu WT, Dawes DE, Gavlak G, Goldman D, Herman WH, Van Nuys K, et al. Insulin access and affordability working group: conclusions and recommendations. Diabetes Care 2018. [DOI] [PubMed] [Google Scholar]
- [36].Bakk L Medicare Part D coverage gap: race, gender, and cost- related medication nonadherence. Soc Work Public Health 2015;30:473–85. [DOI] [PubMed] [Google Scholar]
- [37].Lee M, Khan MM. Gender differences in cost-related medication non-adherence among cancer survivors. J Cancer Surviv 2016;10:384–93. [DOI] [PubMed] [Google Scholar]
- [38].Bakk L, Woodward AT, Dunkle RE. The Medicare Part D coverage gap: implications for non-dually eligible older adults with a mental illness. J Gerontol Soc Work 2014;57:37–51. [DOI] [PubMed] [Google Scholar]
- [39].Lee M, Salloum RG. Racial and ethnic disparities in cost- related medication non-adherence among cancer survivors. J Cancer Surviv 2016;10:534–44. [DOI] [PubMed] [Google Scholar]
- [40].Frankenfield DL, Wei II, Anderson KK, Howell BL, Waldo D, Sekscenski E. Prescription medication cost-related nonadherence among Medicare CAHPS respondents: disparity by Hispanic ethnicity. J Health Care Poor Underserved 2010;21:518–43. [DOI] [PubMed] [Google Scholar]
- [41].Madden JM, Graves AJ, Zhang F, Adams AS, Briesacher BA, Ross-Degnan D, et al. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA 2008;299:1922–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Davidoff AJ, Stuart B, Shaffer T, Shoemaker JS, Kim M, Zacker C. Lessons learned: who didn’t enroll in Medicare drug coverage in 2006, and why? Health Aff (Millwood) 2010;29:1255–63. [DOI] [PubMed] [Google Scholar]
- [43].Skarupski KA, de Leon CF, Barnes LL, Evans DA. Medicare part D enrollment in a biracial community-based population of older adults. Gerontologist 2009;49:828–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Frankenfield DL, Howell BL, Wei II, Anderson KK. Cost-related nonadherence to prescribed medication therapy among Medicare Part D beneficiaries with end-stage renal disease. Am J Health Syst Pharm 2011;68:1339–48. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


