Abstract
Background and aim
Ventricular tachycardia (VT) represents the most frequent cause of sudden cardiac death. Information on clinical characteristics, acute management and outcome of patients with sustained VT is limited in our part of world. The aim of this study was to analyze the demography, hemodynamics, ECG features, underlying disease, mode of termination and outcome of patients presenting with VT.
Methods
This single center cohort study represents total of 107 patients of VT enrolled over 45 months.
Results
Mean age was 45 years and 59 of the patients were males. Thirty three of these patients were hemodynamically unstable (31%) and 74 were stable (69%) Coronary artery disease was the most common etiological factor accounting for 39% of patients followed by non-ischemic cardiomyopathy. Determinants of hemodynamic instability were VT in course of acute myocardial infarction (8 out of fourteen) and polymorphic pattern of VT (13 out of 26). Spontaneous termination of VT occurred in seven patients, antiarrythmic drugs terminated VT in 53 of 67 patients and in remaining 45 patients VT was terminated with direct current (DC) cardioversion. Total of twenty three patients died during the hospital stay. Factors that contributed to mortality were old age, hemodynamic instability and low ejection fraction.
Conclusion
Ischemic heart disease remains the leading cause of VT. Hemodynamically unstable VT occurs more frequently in acute myocardial infarction and polymorphic VT. Most effective method of VT termination is DC cardioversion. Old age, hemodynamic instability and ejection fraction contribute to overall mortality in VT.
Keywords: Ventricular tachycardia, Etiology, Cardiomyopathy, Hemodynamics
1. Introduction
Ventricular tachycardia (VT) is defined as three or more consecutive ventricular complexes that usually occur at the rate of 100–250 complexes per minute. VT that remains for less than 30 s or does not require immediate termination is known as non-sustained VT and that requiring immediate termination or lasting more than 30 s is sustained VT. QRS contours on electrocardiogram during the VT can be unchanging (monomorphic) or can vary randomly (polymorphic).
VT is the most common type of broad complex tachycardia, accounting for about eighty percent of all such cases.1 The symptomatology and hemodynamic consequence of VT depends on its rate and underlying heart disease. VT degenerating to VF is fatal unless intervened promptly.
The underlying substrate for VT varies. Ischemic heart disease and non-ischemic cardiomyopathies are among the most frequent causes.2 The overall incidence of sustained VT following myocardial infarction (MI) has been found to have declined in recent years due to major advances in MI management, resulting in smaller infarct scars. The VT risk in the overall population, however, has been fairly stable and could in fact be increasing, on account of an improved post-MI survival and the possibility of VT occurrence years after the initial MI, along with a progressively aging population.3 Sustained VT is an important cause of out of hospital sudden deaths. Ambulatory ECG recordings at the time of sudden death have shown that, in approximately 60% of sudden cardiac death (SCD) victims, an episode of VT was identified as the initial event.4, 5, 6 Thus the prevalence of the conditions that are substrate for VT directly influence the prevalence of SCD in the population. Information on clinical characteristics, acute management and outcome of patients with sustained VT in our population is limited. This prospective cohort study was aimed at patients presenting with sustained VT in our hospital to analyze the demographic and hemodynamic features, ECG characteristics, underlying disease, mode of termination and clinical outcome until discharge.
2. Methods
2.1. Aims of the study
To evaluate the demographics, hemodynamic and ECG characteristics, underlying disease, tachycardia termination and outcome of patients with sustained ventricular tachycardia.
2.2. Study design
This single-center hospital based prospective study, was conducted at Sher-i-Kashmir Institute of Medical Sciences, a tertiary care center in Srinagar, Jammu and Kashmir, between August 2012 and May 2016.
2.3. Study population
Inclusion criteria; All cases with definite sustained ventricular tachycardia (lasting more than 30 s or terminated by intervention) already admitted in the hospital or presenting in accident and emergency department including those with VT during the course of acute myocardial infarction for whom attending physician informed the cardiology department were included in the study.
Exclusion criteria; Following patients were excluded:
-
1)
Patients without known etiology who died early after hospitalization thereby precluding further evaluation
-
2)
Patients refusal for further evaluation.
-
3)
Patients with recurrent episodes of VT, only the first episode was considered as index event and evaluated.
-
4)
Patients with non sustained VT.
-
5)
Patients with out of hospital pulse less VT that was terminated before arrival to our hospital but had no documentation of the same.
-
6)
Patients with pre-implanted implantable cardioverter defibrillator (ICD) because of the different management of such group.
2.4. Consent and ethical issues
An informed consent was obtained from each subject after explaining the study in detail. The study was cleared by the Institutional Ethics Committee.
2.5. Initial evaluation
Every patient was placed on non invasive monitor for continuous ECG, blood pressure and pulse oxymetry monitoring. Patients with pulseless VT were initially treated as per ACLS protocol. All patients had their history recorded, underwent physical examination, 12-lead ECG registration and routine laboratory analysis. We defined two groups of patients based on hemodynamic status on presentation: hemodynamically stable and hemodynamically unstable. Hemodynamic instability was defined as need for immediate intervention (cardioversion) due to loss of consciousness, hypotension or occurrence of congestive heart failure. Otherwise the patients were defined as hemodynamically stable.
2.6. ECG interpretation
Standard 12 lead ECG during and after VT was recorded in all patients. The ECG diagnosis of VT was made by applying “The Brugada algorithm” 7 and/or “The aVR ‘Vereckei’ algorithm.”8 The ventricular rate, QRS width, VT morphology (monomorphic vs. polymorphic) were noted down. If diagnosis of VT was not clear on surface ECG, intravenous adenosine was given in select cases in increasing doses to differentiate it from supraventricular tachycardia.
2.7. Other relevant investigations
-
•
Standard posterior-anterior chest radiograph in standing position with deep inhalation was done in all patients.
-
•
Serum electrolytes. Potassium: Potassium levels were seen in all the patients. Hypokalemia was defined as potassium levels of less than 3.5 mmol/l. Hypomagnesemia was defined as serum magnesium levels of less than 1.5 mg/dl. Calcium levels were seen in all patients as a part of routine evaluation. Hypocalcaemia was defined as serum calcium levels of less than 8.8 mg/dl.
-
•
Echocardiography. A comprehensive echocardiographic examination of all patients was performed. Each patient was examined in the left lateral decubitus and supine position by precordial transthoracic two-dimensional targeted M-mode echocardiography with Doppler color flow mapping. Ejection fraction was calculated by Simpson’s method or teichholz formula whichever feasible
-
•Coronary angiography was done in patients with definitive or suspected myocardial infarction and those patients with intermediate to high risk of coronary artery disease derived from Framingham risk calculator (based on Wilson, D'Agostino, Levy et al. ‘Prediction of Coronary Heart Disease using Risk Factor Categories).9 Also patients with baseline ECG suggestive of previous MI were subjected to coronary angiography. Coronary artery disease as cause of VT was defined as following:
-
○Patient with acute MI (as evidenced by current ECG and/or coronary angiography)
-
○Patients with age indeterminate myocardial infarction (presence of significant Q waves on baseline ECG, RWMA on echocardiography and/or myocardial transmural scar on late gadolinium enhancement cardiac MRI)
-
○
-
•
Cardiac Magnetic resonance imaging was done in patients without known etiology in whom specific cardiomyopathy like that of ARVD, HCM, myocardial scarring post MI and endomyocardial disease were suspected and echocardiography was inconclusive. The diagnosis of ARVC was made as per the proposed modification of task force criteria.10
2.8. VT termination and follow-up
The therapy for termination of VT followed a well established protocol as per latest ACLS guidelines. Patients who were hemodynamically unstable were administered electrical cardioversion. With one paddle at apical position and other at the base of the sternum, 120J of external biphasic direct current (DC) was given under proper sedation and analgesia. The energy was subsequently increased to a maximum of 200J wherever required. Pulse less VT patients were administered cardiopulmonary resuscitation (CPR) till the time defibrillator was made ready for delivery of shock. Intravenous antiarryhmics drugs in recommended doses were given to hemodynamically stable patients. The choice of antiarrhythmic drug was on attending physician’s discretion. Electrical cardioversion was given to those patients who became secondarily unstable or in whom antiarrhythmic drugs failed to terminate VT. Follow-up information of each patient regarding hospital discharge or death was obtained.
2.9. Statistical analysis
Statistical analysis was performed by SPSS software package (version 20.0, SPSS Inc, Chicago, Illinois, USA). All continuous variables were expressed as mean ± SD, and categorical variables were reported as frequency and percentages. Group comparisons were performed with Student t-test or crosstabs. The Pearson chi-square test or Fisher exact test was used for categorical variables. A p-value of <0.05 was considered statistically significant.
3. Results
After excluding twelve patients (three refused further evaluation and nine were found to have supraventricular origin of tachycardia after initial enrollment as VT), total of 107 patients presenting with sustained VT over a period of 45 months were studied. Patient characteristics, underlying disease and mean of left ventricular ejection fraction in the stable and unstable patients with VT are presented in Table 1. Ischemic heart disease was the most frequent underlying disorder (n = 42, 39%). The only condition which presented with significantly higher number of hemodynamic instability was the group of patients who had VT in course of their acute myocardial infarction (MI). Among 14 patients presenting as MI, 10 patients had acute ST-elevation MI. Percutaneous coronary intervention was done in four patients, three patients were given intravenous lytic therapy and remaining three patients were not given any reperfusion as they had presented very late in course of MI, were not candidates for thrombolysis and did not not give consent for percutaneous transluminal coronary angioplasty (PTCA). Among patients with other forms of cardiomyopathy, 19 (18%) had non-ischemic dilated cardiomyopathy (idiopathic or non-ischemic secondary), two had restrictive cardiomyopathy, two had left ventricular non-compaction and one patient each had cardiac sarcoid, peripartum cardiomyopathy and acute myocarditis respectively. In eight patients, no specific cause could be found and VT was classified as idiopathic. Among them two patient had suspected congenital long QT syndrome (LQTS), three patients had morphology of outflow tract tachycardia, two had morphology suggestive of fasicular VT and one patient had brugada syndrome. Torsade de Pointes due to suspected Congenital LQTS was present in two patients. One was hemodynamically unstable and treated with DC shock and subsequently magnesium sulphate (combined therapy: electrical + pharmaco) but this patient ultimately died. Other one was stable and treated with lidocaine, magnesium sulphate and ICD (classified under combination pharmacotherapy).
Table 1.
Demographic and etiological features of hemodynamically stable and unstable group presenting as ventricular tachycardia. ARVC; arrythmogenic right venyrticular cardiomyopathy, CAD-NoMI; coronary artery disease without acute myocardial infarction, CAD-MI; coronary artery disease with acute myocardial infarction, CMP; cardiomyopathy, HCM; hypertrophic cardiomyopathy, IdVT; idiopathic ventricular tachycardia, VTmisc; ventricular tachycardia due to miscellaneous cause, VTcong; ventricular tachycardia due to repaired or unrepaired congenital heart disease.
| Hemodynamcally stable (n = 74; 69%) | Hemodynamcally Unstable (n = 33; 31%) | Total (n-107) | Significance | |
|---|---|---|---|---|
| Age | 45 (±14) | 50.3 (±15) | 47 (±14.5) | NS |
| Sex | ||||
| Males | 38 (51.3%) | 21 (63.6%) | 59 (55%) | NS |
| Females | 36 (49.7%) | 12 (36.3%) | 48 (45%) | |
| Underlying Disease | ||||
| ARVC | 9 (12%) | 6 (18%) | 15 (14%) | NS |
| CAD-NoMI | 23 (31%) | 5 (15%) | 28 (26%) | NS |
| CAD-MI | 6 (8%) | 8 (24%) | 14 (13%) | 0.0195* |
| Other CMP | 19 (25.6%) | 7 (21%) | 26 (24%) | NS |
| HCM | 3 (4%) | 1 (3%) | 4 (3.7%) | NS |
| IdVT | 8 (10.8%) | 2 (6%) | 10 (9.3%) | NS |
| VTmisc | 4 (5.4%) | 4 (1.2%) | 8 (7.4%) | NS |
| VTcong | 2 (2.7%) | 0 | 2 (1.8%) | NS |
| LVEF | 50.6 (±14.5) | 48.6 (±14.5) | 50 (±14.4) | NS |
significant p value.
Patients in whom VT was secondary to either electrolyte abnormality, medication or some extra myocardial disease were classified in a miscellaneous group. This group comprised of total eight patients out of whom two patients had amiodarone induced QT prolongation with VT, four patients had hypokalemia secondary to systemic disease or drug therapy, one had constrictive pericarditis and one patient had hypothermia.
Electrocardiographic features in stable and unstable group are depicted in Table 2. The only ECG feature that was significantly higher was polymorphic pattern in unstable group.
Table 2.
Electrocardiographic charactaristics of stable and unstable group presenting as ventricular tachycardia. LBBB; left bundle branch block, RBBB; right bundle branch.
| Hemodynamcally stable (n = 74; 69%) | Hemodynamcally unstable (n = 33; 31%) | Total (n = 107) | |
|---|---|---|---|
| Tachycardia rate | 182.9 (±18.9) | 184.9 (±17.8) | 184.2 (±18.5) |
| VT Morphology | |||
| LBBB | 22 (69%) | 10 (31%) | 34 (32%) |
| RBBB | 37 (79%) | 10 (21%) | 47 (44%) |
| Polymorphic | 15 (54%) | 13 (46%)* | 26 (24%) |
P = 0.038 (significant).
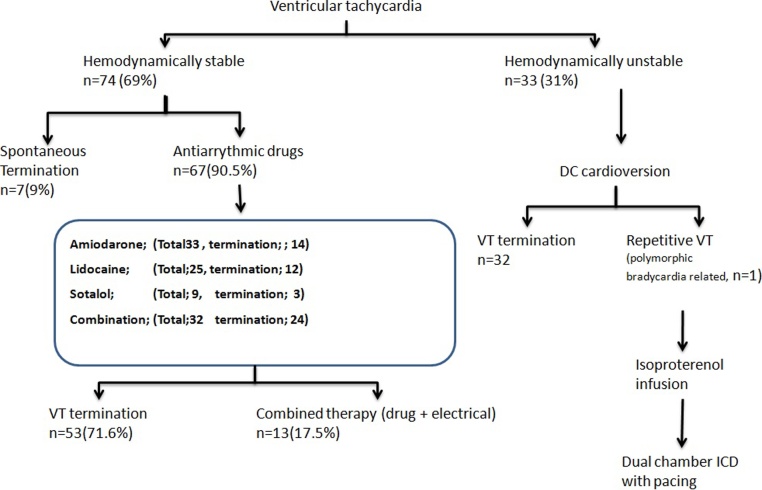
Spontaneous termination of sustained VT occurred in seven patients in hemodynamically stable group. Antiarrhythmic drug terminated VT in 53 patients and 14 patients received combined therapy (drug and electrical) after antiarrhythmic drug failure. Out of total 67 patients receiving antiarrhythmic drugs, 33 (49%) received amiodarone, 25 (36%) received lignocaine 9 (13%) received sotalol and 32 patients (48%) received combination therapy including intravenous beta-blocker. The reversion rate of these drugs is shown in Fig. 1. One patient in unstable group with polymorphic VT after receiving dc-cardioversion developed repetitive bradycardia related torses de pointes that was managed initially with isoproterenol infusion and subsequently received dual chamber implantable cardioverter defibrillator (ICD) with pacing.
Fig. 1.
Tachycardia termination of patients with VT. VT; ventricular tachycardia, ICD; implantable cardioverter defibrillator.
Twenty three of the 107 patients died during hospital stay. The number of unstable patients who died was significantly higher than the number of unstable patients in surviving group (Table 3). Fourteen among them were mere males and nine were females. The mean age of these patients was 55 years and which was significantly higher than those who survived. The mean ejection fraction in mortality group was significantly lower than survival group. There was no significant difference in mortality among different etiological groups or with respect to ECG morphology, QRS rate and QRS width.
Table 3.
Final outcome during hospital stay. EF; ejection fraction.
| Mean age (in years) | Male/Female | Hemodynamics: Stable/ Unstable | EF | Tachycardia rate (per minute) | Monomorphic/polymorphic | |
|---|---|---|---|---|---|---|
| Survived (n = 84) |
44.9 (±14.7) | 45/39 | 63 (85%)/21 (15%) | 51.3 | 184.8 | 64/20 |
| Death (n = 23) | 54.7 (±10.6)* | 14/9 | 11 (48%)/12 (52%)* | 45.3* | 182.0 | 15/8 |
| Total | 47 (±14.5) | 59/48 | 74 (69%) 33 (31%) | 50 | 184.2 | 79/23 |
significant p value (<0.05).
Total 64 out of 107 patients qualified for ICD implantation out of which only 18 ICD implantations (28%) were done due to various reasons.
4. Discussion
The main observations of our study in patients presenting as VT were as follows:
-
○
Ischemic heart disease remains the leading cause of VT.
-
○
Hemodynamically unstable VT was significantly higher in cases with acute myocardial infarction and in those who presented with polymorphic pattern of VT
-
○
Higher mean age, low mean ejection fraction and hemodynamic instability were the more common determinants of mortality.
Total number of male patients in our cohort was 55% and mean age was 47 years. This observation is contrary to popular belief that VT presents at older age and mainly in male population (as has been seen in western cohorts). We can explain this by the fact that although ischemic heart disease was the most common etiology in our study but in terms of proportion it represented much less number when we compare to previously published studies.5, 11, 12, 13 When we did the analysis of patients with coronary artery disease that comprised total of 42 patients (39%), they had higher mean age (57 years) and 62% of them were males. ARVC was the cause in 15 (14%) and dilated non-ischemic dilated cardiomyopathy (idiopathic or secondary) in eighteen (17%) patients. Both these conditions are among the known and frequent causes of VT.14, 15 Idiopathic VT was present in 10 patients with mean age of 34 years, most of them were hemodynamically stable and only one patient among this group died who was having congenital long QT syndrome. This observation was in agreement with the available literature where it has been shown that idiopathic VT presents at younger age and except for few groups, has good prognosis overall.16, 17
The ECG characteristics of our cohort showed that right bundle branch block (RBBB) pattern during tachycardia was most common morphology followed by left bundle block branch (LBBB) pattern and polymorphic pattern respectively. Except for the polymorphic pattern group in which there was significantly higher percentage of unstable patients, no other morphology correlated significantly with the hemodynamics. Polymorphic pattern was present in 2 (13%) of ARVC group, 11 (26%) in ischemic heart disease group, 7 (27%) in non-ischemic cardiomyopathy group, 2 (20%) in idiopathic VT group and 6 (75%) in miscellaneous group. Moreover, tachycardia rate and QRS width also did not have positive correlation with hemodynamic instability. Domanovits etal studies a clinical profile of VT presenting in emergency department and showed that only ECG charactaristics that correlated with the hemodynamic instability was the polymorphic pattern.5
Immediate treatment of VT can be done through several ways. Intravenous administration of various antiarrhythmic drugs is possible. The safety and efficacy of these drugs for acute management has been reported.18, 19 However it is pertinent to mention that long term use of various antiarrhythmic drugs to suppress VT have been shown to increase the mortality and thus should not be used.20 We used only amiodarone, lidocaine, sotalol and intravenous betablockers as rest of the antiarrhythmics were not available. These drugs were used as solo agents or in combination. Out of 74 stable patients, 67 were given antiarrhythmic drugs. Fifty-three out of them reverted and 13 needed additional electrical therapy because of subsequent hemodynamic instability or failure to restore sinus rythm. Thus the success rate of restoring the sinus rhythm by intravenous drug therapy was 79%. Fig. 1 demonstrates various antiarrhythmic agents used and their success rate in restoring the sinus rhythm. Most effective among them was lidocaine (alone or in combination). Electrical therapy was most effective in restoring the sinus rhythm used in 45 patients (unstable = 32, and stable = 13). It restored the sinus rhythm in all the patients. It is well known fact that bradycardia causes QT prolongation that in turn is linked to transmural dispersion of repolarization, which acts as a substrate for initiation and perpetuation of phase 2 re-entry in torsade de pointes.21, 22 This mechanism was present in one patient who was managed with intravenous isoproterenol infusion followed by ICD with pacing support.
Physicians should be well versed with the management of VT owing to its life threatening potential as depicted in our study where total of 21% (n = 23) patients died in course of their hospital stay. The predictors of mortality were hemodynamic instability, old age, and low ejection fraction. Although 64 patients required ICD implantation as per the latest ACC/AHA guidelines, actual implantation rate was only 28% (total 18 patients) due to varied reasons.
The major limitations of this study are as follows;
-
1.
Total number of patients in this study seems to be far less than disease burden in our population. Not all potential patients with VT may have been included. Only patients in whom attending physician informed the cardiology department were included in the study.
-
2.
Antiarrhythmic drugs were used on physician’s discretion and were not randomized so superiority of one drug over other in termination of VT cannot be conclusively drawn from this study.
-
3.
Although best measures were taken to exclude wide QRS non-VT rhythm, there is a chance that few supraventricular rhythm strips may have been misinterpreted as VT and vice-versa owing to the inherent limitation of ECG criteria and the fact that no electrophysiological studies were carried out in most of the patients.
-
4.
Only short term outcome (hospital discharge/death) were noted. Follow-up outcome of patients was not assessed.
-
5.
Number of patients with recurrent VT and mode of death was not recorded.
Declaration of interest
The authors have none to declare.
Acknowledgments
We acknowledge with warm thanks the cooperation of the patients for agreeing for enrolment. Sincere thanks to attending physicians of our institute for their valuable support.
References
- 1.Brady W.J., Skiles J. Wide QRS complex tachycardia: ECG differential diagnosis. Am J Emerg Med. 1999;17:376–381. doi: 10.1016/s0735-6757(99)90091-8. [DOI] [PubMed] [Google Scholar]
- 2.Aronow W.S., Ahn C., Mercando A.D. Prevalence and association of ventricular tachycardia and complex ventricular arrhythmias with new coronary events in older men and women with and without cardiovascular disease. J Gerontol A Biol Sci Med Sci. 2002;57(March (3)):M178–80. doi: 10.1093/gerona/57.3.m178. [DOI] [PubMed] [Google Scholar]
- 3.Josephson M. 4th ed. Lippincott Williams &Wilkins; Philadelphia: 2008. Recurrent ventricular tachycardia. Clinical cardiac electrophysiology; pp. 446–642. [Google Scholar]
- 4.Bayes-de-Luna A., Coumei P., Leclerc Q.J.F. Ambulatory sudden cardiac death: mechanisms of production of fatal arrhythmia on the basis of data from 157 cases. Am Heart J. 1989;117:151–159. doi: 10.1016/0002-8703(89)90670-4. [DOI] [PubMed] [Google Scholar]
- 5.Do Manovits H., Paulis M., Nikafardjam M. Sustained ventricular tachycardia in the emergency department. Resuscitation. 1999 Sept;42(1):19–25. doi: 10.1016/s0300-9572(99)00044-1. [DOI] [PubMed] [Google Scholar]
- 6.Stevenson W.G. Ventricular and ventricular tachycardia. Trans Am Clin Climatol Assoc. 2009;120:403–412. [PMC free article] [PubMed] [Google Scholar]
- 7.Brugada P., Brugada J., Mont L. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991;83:1649. doi: 10.1161/01.cir.83.5.1649. [DOI] [PubMed] [Google Scholar]
- 8.Vereckei A., Duray G., Szénási G. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. 2007;28:589–600. doi: 10.1093/eurheartj/ehl473. [DOI] [PubMed] [Google Scholar]
- 9.Wilson Peter W.F., D’Agostino Ralph B., Levy Daniel. Prediction of Coronary heart disease using risk factor categories. Circulation. 1998:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 10.Marcus F.L., McKenna W.J., Sherrill D. Diagnosis os arrythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;121:1533. doi: 10.1161/CIRCULATIONAHA.108.840827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mozaffarian D., Benjamin E.J., Go A.S. American heart association statistics committee and stroke statistics subcommittee. Heart disease and stroke statistics–2015 update: a report from the american heart association. Circulation. 2015;4:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 12.Miller J.M. The many manifestations of ventricular tachycardia. J Cardiovasc Electrophysiol. 1992;3:88–107. [Google Scholar]
- 13.Trappe H.J., Brugada P. Prognosis of patients with ventricular tachycardia and ventricular fibrillation: role of the underlying etiology. J Am Coll Cardiol. 1988;12:166. doi: 10.1016/0735-1097(88)90370-1. [DOI] [PubMed] [Google Scholar]
- 14.Nava Andrea, Bauce Barbara, Basso Cristina. Clinical profile and long-term follow-up of 37 families with arrhythmogenic right ventricular cardiomyopathy. J JACC. 2000;36(December (7)):2226–2233. doi: 10.1016/s0735-1097(00)00997-9. [DOI] [PubMed] [Google Scholar]
- 15.Milechma G., Scheinmann M.M. Ventricular dysrhythmias and sudden death in dilated cardiomyopathy. Prog Cardiol. 1989;2:1:85. [Google Scholar]
- 16.Nathani P., Shetty S., Lokhandwala Y. Ventricular tachycardia in structurally normal hearts: recognition and management. J Assoc Phys India. 2007;55(April Suppl):33–38. [PubMed] [Google Scholar]
- 17.Lemery R., Brugada P., Della Bella P. Nonischaemic ventricular tachycardia: clinical course and long term follow-up in patients without clinically overt heart disease. Circulation. 1989;79:990–999. doi: 10.1161/01.cir.79.5.990. [DOI] [PubMed] [Google Scholar]
- 18.Griffith M.J., Linker N.J., Garrat C.J. Relative efficacy and safety of intravenous drugs for termination of sustained ventricular tachycardia. Lancet. 1990;336:670–673. doi: 10.1016/0140-6736(90)92158-e. [DOI] [PubMed] [Google Scholar]
- 19.Roden D.M. Risks and benefits of antiarrhythmic therapy. New Engl J Med. 1994;331:785–791. doi: 10.1056/NEJM199409223311207. [DOI] [PubMed] [Google Scholar]
- 20.Echt Debra S., Liebson Philip R., Brent Mitchell L. Mortality and morbidity in patients receiving encainide, flecainide or placebo — the cardiac arrhythmia suppression trial. N Engl J Med. 1991;324:781–788. doi: 10.1056/NEJM199103213241201. [DOI] [PubMed] [Google Scholar]
- 21.Priori S.C., Diehl L., Schwartz P.J. Torsade de pointes. In: Podrid P.J., Kowey P.R., editors. Cardiac Arrhythmia: Mechanisms, Diagnosis and Management. Williams and Wilkins; Baltimore, MD: 1995. pp. 951–963. [Google Scholar]
- 22.Namboodiri Narayanan. Bradycardia-induced torsade de pointes – an arrhythmia less understood indian. Pacing Electrophysiol J. 2010;10(10):435–438. [PMC free article] [PubMed] [Google Scholar]