Abstract
Objective
The aim of this meta-analysis of randomized controlled trials (RCT) and retrospective cohort studies (CS) regarding the use of volar locking plate (VLP) and external fixation (EF) in distal radius fractures was to determine whether there was any evidence that one treatment was superior to the other.
Methods
The meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. Electrical databases (PubMed, EMBASE and the Cochrane library) were retrieved to find RCTs and CSs met the eligibility criteria. Two reviewers screened the studies, extracted the data and evaluated the methodological quality, and performed data analysis with RevMan 5.1. The publication bias was test by Stata 14.0. The Begg's and Egger's test were performed by Stata 14.0. The quality of evidence was graded according to the criteria of GRADE. We ultimately included ten RCTs and eleven CSs.
Results
A total of 1590 subjects were reported. Publication bias was detected by funnel plot in RCTs. VLP could provide better results such as DASH scores (RCT: MD = −6.12, 95%CI = −12.07–0.17; CS: MD = −6.43, 95%CI = −12.53–0.3), ulnar variance (RCT: MD = −0.81, 95%CI = −1.25–0.37) and infection rate (RCT: RR = 0.25, 95%CI = 0.10–0.65; CS: RR = 0.15, 95%CI = 0.06–0.40). There were no significant differences for G-W scores, VAS and grip strength between the VLP group and EF group. There was significantly greater loss of volar tilt (P = 0.01) and radial inclination (P = 0.02) in patients receiving EF, basing on the CSs.
Conclusions
VLP could provide better results, such as DASH scores, ulnar variance, volar tilt, radial inclination and infection rate. The use of VLP appear to be associated with better results of ROM (flexion, pronation, supination and radial deviation), radiographic parameters (volar tilt and radial inclination) and lower total complication rate and CRPS rate in CSs.
Level of evidence
Level 1, Therapeutic study.
Keywords: Distal radial fractures, Volar locking plate, External fixation, Meta-analysis, GRADE analysis
Introduction
Distal radius fractures (DRFs) which account for 44% of all types of hand and forearm fractures1 represent the most common type of fracture of the upper extremity and pose a serious public health concern.2 DRFs are common in old people with osteoporosis and often caused by low energy injury or a simple fall in this population. Economic costs of care of DRFs are more than USD 480 million in the United States annually.3 The burden of DFRs and the costs of cares are expected to grow, since the population aging.4 Unfortunately, the treatment for DRFs is controversial. Therefore, determining effective evidence-based treatment of DRFs is crucial.
Over the last 30 years, many different treatment methods have been recommended: cast immobilization, external fixation (EF), open reduction and internal fixation with a volar or dorsal plate. The best choice of treatment for DRFs remains a topic of controversy. The EF is a minimal invasive method which is simple to perform, and rigid stability may be achieved by EF for DRFs. EF with bridging or non-bridging fixator could be applied for DRFs. Studies show that direct skeletal EF with bridging fixators and EF with non-bridging fixators result in fewer malunions and also have satisfactory function results.5, 6, 7 Volar locking plates (VLP) have been introduced to stabilise displaced DRFs from the volar side for several years. These have two theoretical advantages: reduction in extensor tendon problems and secure fixation of osteoporotic bone because of the fixed angle conferred by the locking screws. Additionally, using the VLP have an excellent advantage of biomechanics in treatment for the DRFs, but none of the recommendations in clinical practice guidelines for DRFs published by the American Academy of Orthopaedic Surgeons (AAOS) was given a “strong” rating owing to limited strength of the evidence. Furthermore, there were some complications related to VLP, such as flexor tendon problem,8 longitudinal fractures of the near cortex,9 tenosynovitis and tendon ruptures resulting from penetration of distal screws through the dorsal cortex10 and so on. Therefore, whether VLP are superior to EF in clinical results in the treatment for DRFs remains uncertain.
Many recent randomized controlled trials11, 12 and retrospective studies13, 14 have suggested that there are few differences between them in terms of postoperative results such as grip strength, pain, and range of motion, radiographic measurements, except the subjective assessment score.
We aimed to perform a meta-analysis of randomized trials and retrospective trials comparing the clinical, functional and radiological outcomes for distal radius fractures using VLP with EF.
Materials and methods
The meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines.15
Search strategy
We searched PubMed, Embase, and the Cochrane library from their inception to Dec 28th, 2017. The main search strategy for PubMed and Embase database entered were illustrated in Table 1, and no language restrictions were used. We also searched the references of reviews and included studies to ensure that all relevant studies were checked for the meta-analysis.
Table 1.
Search strategy for PubMed and EMBASE.
| PubMed: | #1 randomized controlled trial [PT] | EMBASE: | (distal AND (radius OR radial)) AND (external AND fix*) AND (((internal OR plate OR plates OR plating) AND fix*) AND volar) AND (randomized OR randomly).mp. [mp = title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] |
| #2 controlled clinical trial [PT] | |||
| #3 comparative study [PT] | |||
| #4 randomized [tiab] | |||
| #5 randomly [tiab] | |||
| #6 trial [tiab] | |||
| #7#1 OR#2 OR#3 OR#4 OR#5 OR#6 | |||
| #8 distal radial fractures [tiab] | |||
| #9 distal radius fractures [tiab] | |||
| #10 distal radial [tiab] | |||
| #11 distal radius [tiab] | |||
| #12 colles fractures [tiab] | |||
| #13 smith fractures [tiab] | |||
| #14 wrist injuries [tiab] | |||
| #15#8 OR#9 OR#10 OR#11 OR#12 OR#13 OR#14 | |||
| #16 plate [tiab] | |||
| #17 locking plate [tiab] | |||
| #18 volar locking plate [tiab] | |||
| #19 volar plate [tiab] | |||
| #20 plate osteosynthesis [tiab] | |||
| #21 external fixation [tiab] | |||
| #22 external fixators [tiab] | |||
| #23#16 OR#17 OR#18 OR#19 OR#20 OR#21 OR#22 | |||
| #24#7 AND#15 AND#23 |
PT: Publication type; tiab: Title/Abstract.
Inclusion criteria
Studies were included in the meta-analysis if they met the following criteria: they were randomized controlled trials (RCTs) or retrospective cohort studies (CSs); they compared VLP and EF for patients with closed DRFs; they reported data on disability arm, shoulder and hand scores (DASH scores), Gartland-Werley scores (G-W scores), visual analogue scale scores (VAS scores), range of motion, radiological measurement, grip strength, and complications, and data were completely or partly available.
Exclusion criteria
Studies were excluded if they were experimental trials; data were incomplete or unavailable; they were non-original articles such as reviews, or letters and comments; or duplicated publications were excluded apart from the one with the most complete data.
Evaluated outcomes
Functional scores (DASH scores, G-W scores, VAS scores), wrist range of motion (flexion, extension, pronation, supination, ulnar deviation and radial deviation), radiological measurement (volar tilt, radial inclination, ulnar variance and radial length), grip strength and reported complications were evaluated.
Study selection
Duplicates were initially excluded. Two reviewers reviewed all studies independently by screening the titles and abstracts. The irrelevant articles were identified and eliminated. Subsequently, the remaining studies were assessed through full-text reading by two reviewers independently. Disagreements were settled by discussion. If the consensus could not be reached, the final decision was adjudicated by a third reviewer.
Data extraction
Two reviewers extracted the following data from the included studies independently, using the standardized data extraction method. They checked data each other for accuracy. The data extracted from the studies included title, published year, authors, country, study design, number of study center, sample size, age of subjects, sex distribution, the type of fracture, the type of interventions, duration of follow-up, and outcomes. We tried to obtain unpublished original raw data from the authors of each study by email. For all continuous outcomes, we extracted mean and standard deviations. When these values were not reported, P value or confidence intervals was used to calculate these values if possible. Differences and disagreements were settled by discussion.
Methodological quality assessment
Two reviewers independently assessed the methodological quality and the risk of bias of the included RCTs with a 12-item scale16 recommended by Cochrane Back Review Group. The following aspects were assessed: randomization, allocation concealment, similar baseline, patient blinded, care provider blinded, the outcome assessor blinded, selective reporting, avoided cofactors, patients' compliance, drop-out rate, similar timing, and ITT analysis. The quality of retrospective cohort studies was assessed using Newcastle–Ottawa quality assessment scale for non-randomized case controlled studies and cohort studies (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp).17 Three aspects were assessed: selection, comparability and exposure. Testing for publication bias was performed using funnel plots, Begg's test and Egger's test. The Begg's test and Egger's test were performed by software Stata 14.0 (Stata Corp, College Station, Tex). We also used the criteria of the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to evaluate the quality of evidence.18
Data synthesis and analysis
We prespecified separate analysis of RCTs and CSs given the inherent differences between these types of study designs.19 Mean differences (MD) with a 95% confidence interval (CI) were calculated to assess the effect size for continuous outcome data. Risk ratio (RR) with a 95%CI were used as effect size for dichotomous data. Inverse variance method and Mantel-Haenszel analysis method were used for continuous variables and dichotomous variables, respectively.20 The heterogeneity among the trials was assessed for significance with Q and quantified with I2. Statistically significant was set at the P value < 0.10. The heterogeneity of the trials was divided into four levels: homogeneous (an I2 less than 25%), low heterogeneity (an I2 between 25% and 50%), moderate heterogeneity (an I2 between 50% and 75%), and high heterogeneity (an I2 above 75%). If the studies were homogeneous or the statistical heterogeneity was low, we used the fixed effect model. While, random effects model was applied when the statistical heterogeneity was moderate or high. Statistical analysis was undertaken with the software program RevMan 5.1 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark).
Results
Literature search and study characteristics
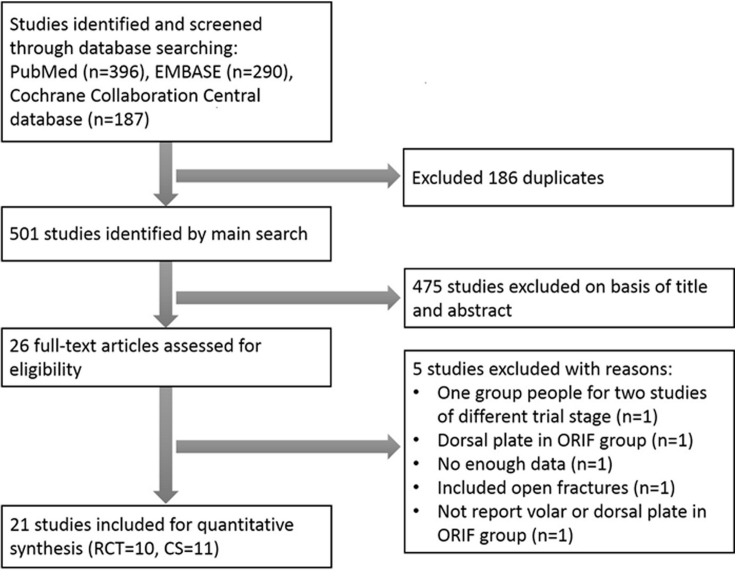
Fig. 1 illustrated the selection flow of studies in our meta-analysis. We retrieved 421 potential citations. After the title and abstract scanning, 26 full-text articles left to be assessed for eligibility. Ten RCTs11, 12, 21, 22, 23, 24, 25, 26, 27, 28 and eleven CSs13, 14, 29, 30, 31, 32, 33, 34, 35, 36, 37 satisfied the inclusion criteria. A total of 1590 subjects with closed DRF (RCT: 908; CS: 682) were reported including 781 (RCT: 432; CS: 349) with VLP and 809 (RCT: 476; CS: 333) with EF. Five trials were excluded for different reasons. The data of one RCT38 were not enough. Included patients in one trial39 were same to the other included trial.28 One trial40 used inappropriate intervention (dorsal plate). One trial41 did not report the type of the plate (volar or dorsal?). The last one trial42 included open distal radius fractures.
Fig. 1.
The flow diagram shows the selection process used in the study.
Table 2, Table 3 summarized the characteristics of included RCTs and CSs, respectively. All included trials had comparable baseline in demographic characteristics, except four trials.26, 29, 30, 36 The follow-up periods of all CSs were longer than that of RCTs. Therefore, the data at the end of the follow-up of each included trial were used in synthesis and analysis.
Table 2.
Characteristics of included RCTs.
| Study type | Included studies | Country | Study center | Sample size (VLP/EF) | Female (VLP/EF) | Mean age (VLP/EF)(years) | Fracture type | Intervention (VLP/EF) | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|---|
| Randomized controlled trials | Jeudy 2012 | France | Two | 36/39 | 26/31 | 64.7/64.6 | AO C2-3 | VLP/EF | 6 |
| Wilcke 2011 | Sweden | One | 33/30 | 25/23 | 55/56 | AO A/C1 | VLP/bridging EF | 12 | |
| Wei 2009 | USA | One | 12/22 | 9/19 | 61/55 | AO A/C | VLP/bridging EF | 12 | |
| Egol 2008 | USA | One | 38/39 | 25/22 | 52.2/49.9 | AO A/B/C | VLP/bridging EF | 12 | |
| Gradl 2013 | USA | One | 52/50 | 89§ | 63§ | AO A3/C1-3 | VLP/non-bridging EF | 12 | |
| Williksen 2013 | Norway | One | 52/59 | 89§ | 54§ | AO A2-3/C1-3 | VLP/bridging EF | 12 | |
| Shukla 2014 | India | One | 42/68 | 28/33 | 39.12§ | Cooney's type IV | VLP/bridging EF | 12 | |
| Roh 2015 | Korea | One | 36/38 | 7/8 | 54.4/55.3 | AO C2-3 | VLP/EF | 12 | |
| Sha 2015 | China | One | 61/61 | 52/50 | 64.7/64.4 | AO C1-3 | VLP/bridging EF | 12–28 | |
| Navarro 2016 | Sweden | One | 70/70 | 63/66 | 63/63 | AO A2-3/C1-3 | VLP/bridging EF | 12 |
VLP: volar locking plate; EF: external fixation; NR: not reported; §: respective data are not available in the study.
Table 3.
Characteristics of included CSs.
| Study type | Included studies | Country | Study center | Sample size (VLP/EF) | Female (VLP/EF) | Mean age (VLP/EF)(years) | Fracture type | Intervention (VLP/EF) | Follow-up time (months) |
|---|---|---|---|---|---|---|---|---|---|
| Retrospective cohort studies | Richard 2011 | USA | One | 56/59 | 28/31 | 50/50 | AO C2-3 | VLP/EF | 12 |
| Jorge-Mora 2012 | Spain | One | 40/40 | 24/21 | 52/45 | AO A/B/C1-3 | VLP/EF | 15 | |
| Schmelzer-Schmied 2009 | Germany | One | 15/15 | NR | 60§ | AO C1-2 | VLP/bridging EF | >12 | |
| Rizzo 2008 | USA | One | 41/14 | 25/8 | 48/45 | Melone type II | VLP/EF | 25–36 | |
| Wright 2005 | USA | One | 21/11 | 10/8 | 50.1/50 | NR | VP/bridging EF | 12–84 | |
| Westphal 2005 | Germany | One | 54/77 | 28/46 | 59.5/60.6 | AO A3/C2 | VP/EF | 12–40 | |
| Kumbaraci 2014 | Turkey | One | 34/35 | 16/18 | 48/52.6 | AO C1-3 | VLP/bridging EF | 12–72 | |
| Gereli 2010 | Turkey | One | 16/14 | 5/3 | 49/35 | AO C1-3 | VLP/bridging EF | 16–96 | |
| Sato 2010 | Japan | One | 13/13 | 9/11 | 69.7/65.8 | AO A/C | VLP/bridging EF | 12–39 | |
| Zhao 2011 | China | One | 30/30 | 26/26 | 59.57/60/97 | AO A3/B2-3/C1-3 | VP/bridging EF | 12–18 | |
| Yang 2013 | China | One | 29/25 | 13/12 | 45.72/44.84 | AO C1-3 | VLP/bridging EF | 12–24 |
CSs: retrospective cohort studies; VLP: volar locking plate; EF: external fixation; NR: not reported; §: respective data are not available in the study.
Study quality assessment
The methodological quality of one RCT25 was low, while the quality of left RCTs was moderate. All included RCTs did not adapt blind methods (patient, care provider and outcome assessor). Two trials11, 27 did not describe the randomizing method, and four trials12, 22, 24, 25 did not report the allocation concealed method (Table 4).
Table 4.
Methodological quality assessment of included randomized controlled trials.
| Included studies | Randomized adequatelya | Allocation concealed | Similar baseline | Patient blinded | Care provider blinded | Outcome assessor blinded | Avoided selective reporting | Similar or avoided cofactors | Patients' complianceb | Acceptable drop-out ratec | Similar timing | ITTd analysis | Quality # |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jeudy 2012 | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | Yes | No | Moderate |
| Wilcke 2011 | Unclear | Yes | Yes | No | No | No | Yes | Yes | No | Yes | Yes | Unclear | Moderate |
| Wei 2009 | Yes | Yes | No | No | No | Yes | Yes | No | No | No | Yes | Yes | Moderate |
| Egol 2008 | Yes | Yes | Yes | No | No | No | Yes | No | No | Yes | Yes | No | Moderate |
| Gradl 2013 | Yes | Unlear | Yes | No | No | No | Yes | No | No | Yes | Yes | Unclear | Moderate |
| Williksen 2013 | Yes | Yes | Unclear | No | No | No | Yes | Yes | No | Yes | Yes | Unclear | Moderate |
| Shukla 2014 | Yes | Unclear | Yes | No | No | No | No | No | No | Yes | Yes | Unclear | Low |
| Roh 2015 | Yes | Unclear | Yes | No | No | No | Yes | Yes | No | Yes | Yes | Unclear | Moderate |
| Sha 2015 | Yes | Unclear | Yes | No | No | No | No | Yes | No | Yes | Yes | Unclear | Moderate |
| Navarro 2016 | Unclear | Yes | Yes | No | No | No | No | Yes | No | Yes | Yes | Unclear | Moderate |
The frequencies of “Yes” ≥7 means “High”; >4 and <7 mean “Moderate”; ≤4 means “Low”.
Only if the method of sequence generated were explicitly described could get a “Yes”; sequence generated by “dates of admission” or “patients number” receive a “No”.
Intermittent treatment or therapeutic duration less than 6 months means “Yes”, otherwise “No”.
Drop-out rate ≥30% means “No”; <30% means “Yes”.
ITT: intention to treat, only if all randomized patients are analyzed in the group they were allocated to could receive a “Yes”.
Seven CSs achieved 7 scores, two achieved 6 score, one achieved 5 score and one achieved 4 score. The quality of all CSs was moderate to high, except Gereli's trial29 (Table 5).
Table 5.
Quality assessment according to the Newcastle–Ottawa scale.
| Study | Selection | Comparability | Exposure | Total score |
|---|---|---|---|---|
| Richard 2011 | 3 | 2 | 2 | 7 |
| Jorge-Mora 2012 | 4 | 0 | 2 | 6 |
| Schmelzer-Schmied 2009 | 3 | 2 | 2 | 7 |
| Rizzo 2008 | 3 | 2 | 2 | 7 |
| Wright 2005 | 3 | 0 | 2 | 5 |
| Westhal 2005 | 3 | 2 | 2 | 7 |
| Kumbaraci 2014 | 3 | 2 | 2 | 7 |
| Gereli 2010 | 2 | 0 | 2 | 4 |
| Sato 2010 | 3 | 2 | 2 | 7 |
| Zhao 2011 | 3 | 2 | 2 | 7 |
| Yang 2013 | 2 | 2 | 2 | 6 |
DASH scores, G-W scores and VAS scores
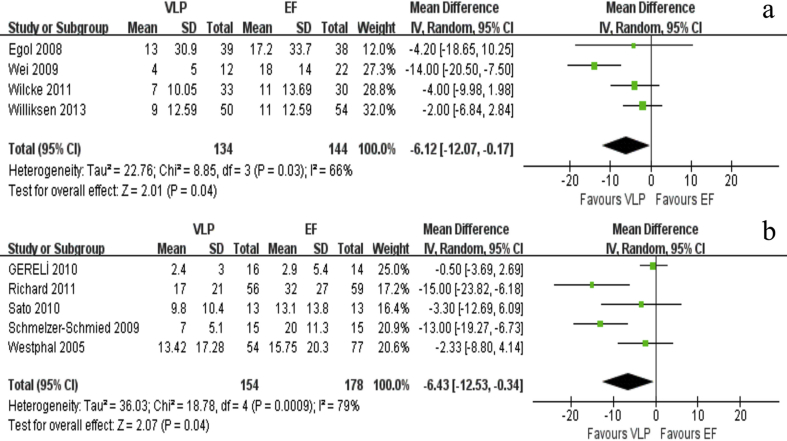
Four RCTs21, 26, 27, 28 and five CSs29, 31, 33, 34, 35 reported the DASH scores. Both included RCTs and CSs demonstrated that the DASH scores of VLP group was significantly better than that of EF group (RCT: MD = −6.12, 95%CI = −12.07–0.17, P = 0.04, I2 = 66%; CS: MD = −6.43, 95%CI = −12.53–0.34, P = 0.04, I2 = 79%) (Fig. 2). Only three CSs13, 14, 29 reported G-W scores, and two CSs31, 34 reported VAS scores. The results of a heterogeneity test indicated that there was no significant heterogeneity among the included CSs I2PI2P. There were no significant differences in G-W scoresP and VAS scores P between the two groups (Table 6).
Fig. 2.
The forest plot shows the mean difference in DASH scores between VLP and EF. a: DASH scores in RCTs; b: DASH scores in CSs.
Table 6.
Illustration of outcomes of the RCTs and CSs.
| Category | Study type | No. RCTs No. CSs | VLP | EF | I2 | Effect model | RR | MD | 95% CI | P-value |
|---|---|---|---|---|---|---|---|---|---|---|
| G-W score | CS | 3 | 79 | 74 | 0% | Fixed | – | −0.39 | [−0.88, 0.10] | 0.12 |
| VAS score | CS | 2 | 71 | 74 | 0% | Fixed | – | −0.81 | [−1.67, 004] | 0.06 |
| Flexion | RCT | 4 | 136 | 140 | 51% | Random | – | −0.71 | [−5.19, 3.78] | 0.76 |
| CS | 3 | 65 | 64 | 69% | Random | – | 7.90 | [3.02, 12.78] | 0.002* | |
| Extension | RCT | 4 | 136 | 140 | 64% | Random | – | 1.78 | [−4.36, 7.93] | 0.57 |
| CS | 3 | 65 | 64 | 41% | Fixed | – | 2.23 | [−0.47, 4.92] | 0.11 | |
| Pronation | RCT | 4 | 136 | 140 | 69% | Random | – | 3.60 | [−0.41, 7.60] | 0.08 |
| CS | 3 | 65 | 64 | 28% | Fixed | – | 5.69 | [3.53, 7.85] | <0.00001* | |
| Supination | RCT | 4 | 136 | 140 | 72% | Random | – | −0.17 | [−4.51, 4.17] | 0.94 |
| CS | 3 | 65 | 64 | 74% | Random | – | 6.35 | [1.12, 11.57] | 0.02* | |
| Ulnar deviation | RCT | 4 | 136 | 140 | 38% | Fixed | – | 0.06 | [−3.02, 3.14] | 0.97 |
| CS | 3 | 65 | 64 | 63% | Random | – | 0.99 | [−0.86, 2.83] | 0.29 | |
| Radial deviation | RCT | 4 | 136 | 140 | 0% | Fixed | – | −2.76 | [−6.36, 0.84] | 0.13 |
| CS | 3 | 65 | 64 | 42% | Fixed | – | 1.49 | [0.18, 2.80] | 0.03* | |
| Volar tilt | RCT | 5 | 198 | 213 | 68% | Random | – | 1.60 | [−0.12, 3.31] | 0.07 |
| CS | 9 | 287 | 308 | 94% | Random | – | 2.99 | [0.62, 5.36] | 0.01* | |
| Radial inclination | RCT | 4 | 148 | 159 | 81% | Random | – | −0.50 | [−2.19, 1.19] | 0.56 |
| CS | 7 | 216 | 234 | 35% | Fixed | – | 0.39 | [0.07, 0.71] | 0.02* | |
| Ulnar variance | RCT | 4 | 137 | 152 | 0% | Fixed | – | −0.81 | [−1.25, −0.37] | 0.0003* |
| CS | 6 | 213 | 238 | 79% | Random | – | −0.22 | [−1.05, 0.61] | 0.61 | |
| Radial length | RCT | 4 | 162 | 175 | 56% | Random | – | −0.26 | [−0.62, 1.13] | 0.56 |
| CS | 5 | 163 | 181 | 48% | Fixed | – | −0.01 | [−0.30, 0.27] | 0.93 | |
| Infection | RCT | 7 | 338 | 353 | 0% | Fixed | 0.25 | – | [0.07, 0.42] | 0.005* |
| CS | 8 | 277 | 265 | 0% | Fixed | 0.17 | – | [0.06, 0.40] | 0.0001* | |
| CRPS | RCT | 7 | 326 | 343 | 0% | Fixed | 0.78 | – | [0.44, 1.40] | 0.41 |
| CS | 5 | 165 | 177 | 0% | Fixed | 0.31 | – | [0.12, 0.79] | 0.01* | |
| CTS | RCT | 7 | 339 | 342 | 0% | Fixed | 1.67 | – | [0.75, 3.72] | 0.21 |
| CS | 3 | 103 | 127 | 0% | Fixed | 4.12 | – | [0.69, 24.53] | 0.12 | |
| RSD | CS | 2 | 71 | 74 | 0% | Fixed | 0.26 | – | [0.03, 2.19] | 0.21 |
RR: relative risk; MD: mean difference; CRPS: complex regional pain syndrome; CTS: carpal tunnel syndrome; RSD: Reflex Sympathetic Dystrophy. * for significant values.
Wrist range of motion (ROM)
Pooling of wrist ROM data was possible across four21, 22, 26, 27 of the ten RCTs, and three13, 29, 34 of the CSs. No heterogeneity was detected for radial deviation in RCTsI2P. Low to moderate heterogeneities were found in any other ROM variables I2. The pooled treatment effect showed significant differences favoring VLP for flexion, pronation, supination and radial deviation in CSs P. While no significant differences were detected for these ROM variables in RCTsP. No significant differences were detected in extension and ulnar deviation in RCTsP and CSsP (Table 6).
Radiological measurement
Five RCTs12, 21, 24, 26, 28 and nine CSs13, 14, 29, 30, 31, 33, 34, 35, 37 reported volar tilt, four RCTs12, 21, 24, 26 and seven CSs13, 14, 29, 30, 33, 35, 37 reported radial inclination, four RCTs21, 24, 26, 28 and six CSs13, 29, 30, 31, 33, 35 reported ulnar variance and four RCTs12, 21, 26, 28 and five CSs13, 14, 29, 35, 37 reported radial length. Table 6 summarized the radiological measurement results. No heterogeneity was detected for ulnar variance in RCTsI2P. Low to high heterogeneity was detected in any other radiological measurement variablesI2. According to the analysis of data extracted from CSs, there was significantly greater loss of volar tiltP and radial inclinationP in patients receiving EF, compared with those receiving VLP. But no significant differences were detected according to the analysis of data extracted from RCTsPP. The analysis of data extracted from RCTs indicated that VLP lead to significantly better restoration of ulnar varianceP, but no significant difference was detected for ulnar variance in CSsP. However, no statistical difference was found for radial length in either RCTsP or CSsP (Table 6).
Grip strength
Six RCTs21, 22, 24, 26, 27, 28 reported the grip strength of participants. Fixed effects model was implemented since low heterogeneity was found in this comparison (I2 = 25%, P = 0.25). No significant difference for grip strength in the pooled treatment effect (MD = 2.80, 95%CI = −0.97–6.57, P = 0.15). Only one CS31 reported the grip strength. There was significantly improved grip strength in the VLP group compared to the EF group (P = 0.007).
Complications
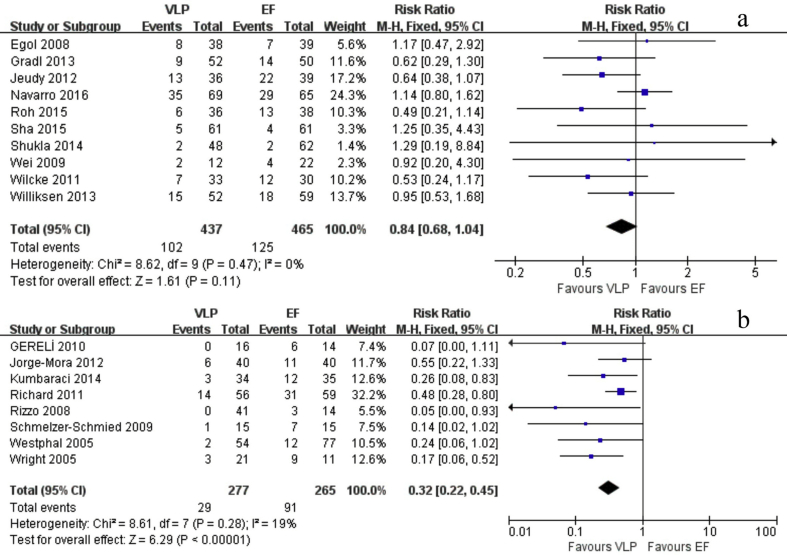
Ten RCTs and eight CSs reported the complication rate. The meta-analysis of total complication rate showed no significant difference in RCTs (RR = 0.84, 95%CI = 0.68–1.04, P = 0.11, I2 = 0%), but significantly lower complication rate for VLP group in CSs (RR = 0.32, 95%CI = 0.22–0.45, P < 0.00001, I2 = 19%) (Fig. 3). Both RCTs and CSs showed significant differences in infection rate favoring VLPP. However, both RCTs and CSs showed no significant differences for carpal tunnel syndrome (CTS) rateP. A significant difference favoring VLP in CSsP and no significant difference in RCTs was detected for complex regional pain syndrome (CRPS). Only two of the included CSs reported the Reflex Sympathetic Dystrophy (RSD), and no significant difference was detected between the two groups (Table 6).
Fig. 3.
The forest plot shows risk ratio in total complication rate between VLP and EF. a: total complication rate in RCTs; b: total complication rate in CSs.
Strength of evidence
In the GRADE system of rating quality evidence, the quality evidence of ulnar variance and carpal tunnel syndrome was moderate in RCT group. The quality evidence of the total complication rate was very low. The quality evidence of the rest of outcomes in RCT group was low. All of the outcomes in the CS group achieved the very low quality evidence. (Supplementary materials).
Publication bias
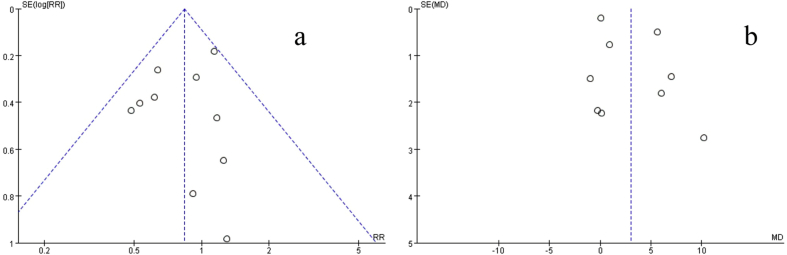
Funnel plots generated in this meta-analysis that indicated the overall postoperative complications in RCTs and volar tilt in CSs are shown in Fig. 4. The shapes of the funnel plot in RCTs reveal slight asymmetry, which indicated some evidence of publication bias. However, the Begg's test and Egger's test showed that no statistical publication bias was detected (Begg's test P = 1.000; Egger's test P = 0.789). In CSs, we did not identify any significant graphic and statistical publication bias by the funnel plot, Begg's test (P = 0.754) and Egger's test (P = 0.776).
Fig. 4.
a: The funnel plot of total complication rate shows the publication bias in RCTs. b: The funnel plot of total complication rate shows the publication bias in CSs.
Discussions
The present meta-analysis included not only the RCTs, but also CSs. We aim to find more evidence to compare the VLP to EF for the treatment of DRFs. No contradictory results were found between the RCTs and CSs. Our meta-analysis indicated that the VLP lead to significantly lower DASH scores and infection rate than EF at the end of follow-up period both in RCTs and CSs. According to the analysis of the data extracted from RCTs, VLP associated with significantly better restoration in ulnar variance comparing with EF. Basing on the analysis of the data extracted from CSs, VLP lead to significantly better flexion, pronation, supination and radial deviation range of motion, and better restoration in volar tilt and radial inclination. Furthermore, there was a significantly greater rate of total complication in the EF group, as well the CRPS. The observed differences between the findings with RCTs and CSs demonstrated that reliance on neither should be absolute, but the collective data appeared consistent confirming the presence of significant efficacy of VLP in many assessment outcomes.
RCT and CS have their individual strengths and limitations that affect the clinical context and interpretation of their results. RCT data represents the purest comparison between the two treatment strategies and can minimize treatment selection bias, since it can minimize the influence of both measured and unmeasured confounders. While, CSs may be more generalizable and less subject to enrollment bias. Hannan19 indicated that RCTs and observation studies could be used synergistically to obtain more and better information about the relative merits of alternative interventions/treatments. Therefore, both types of data are useful in assessing the relative efficacy of VLP compared with EF.
Our meta-analysis included ten RCTs, nine of which achieved moderate methodological assessment. Only one RCT achieved low methodological assessment. The number of the RCTs was more than that of the published meta-analysis,43 offering newer and more robust evidence for the treatment of DRFs with VLP or EF. To compare with the results of meta-analysis of RCTs, CSs comparing VLP and EF for patients with DRFs were included. But we did not combine the included RCTs and CSs, because Cochrane group recommended that randomized trials and non-randomized trial should not be combined in a meta-analysis.44 The quality of CSs included in the meta-analysis was moderate to high, and only one was low quality. However, the publication bias of RCTs was detected. This maybe affect the robustness of evidence. A small group of positive industry-funded studies22, 26 can suggest publication bias. Studies11, 12, 25 that did not avoid selective reporting of outcomes also can suggest publication bias.
It is known that anatomical restoration, early mobilization and minimal soft tissue trauma are the goal of open reduction and internal fixation of a DRF.45 DASH scores as the primary outcome revealed that, compared with EF, VLP led to superior performance in subjective outcome. One RCT38 also reported the similar results at six months after surgery. But another RCT39 reported that there was no significant difference for DASH scores at five years after surgery. One most possible explanation for this different outcomes could be that VLP osteosynthesis could restore the bony anatomy as a stable internal fixation, which could allow patients to get a more active early physiotherapy. But the DASH scores in EF group was improving with time and the difference between EF and VLP in DASH scores diminished after several years.
In CSs, Flexion, radial deviation, supination and pronation in VLP group were significantly better than those in the EF group. Since patients with VLP fixed typically are permitted earlier active wrist mobilization,46 it would be reasonable to expect this to contribute to some the advantage in ROM. Abnormalities in the anatomy of the wrist joint have been shown to lead to decreased range of motion.47 Dario's study48 shows that ulnar variance and volar tilt are the most important radiographic parameters to be restored to obtain good functional outcome in DRFs. Our meta-analysis showed that volar tilt, radial inclination and ulnar variance were significantly better in patients treated with VLP compared with EF. This was another explanation for differences in ROM. Chen49 and Orbay50 showed that compared with other methods of fixation, volar plating for DRFs allows for better anatomic reduction. This was similar to our meta-analysis. In RCTs, ulnar variance in VLP group was significantly better than that in the EF group. No heterogeneity was detected for ulnar variance. Hence, this result is credible. This is same for Zhang's study.43 One explanation is that VLP can offer better ability in controlling a variety of fractures and the fixation of VLP is firm. Biomechanical study51 has demonstrated that VLP can offer adequate strength to withdraw early postoperative motion. In RCTs, no statistical difference was detected in grip strength. However, one RCT39 followed five years and Richard's study31 show better grip strength in VLP group.
Other meta-analysis52 has reported that infections was more frequent in patients treated with EF, which is same to our meta-analysis. The difference of total complication rate and CRPS was significant in CSs, but not in RCTs. One conceivable explanation is that the period of follow-up in CSs is longer than those in RCTs. More complications could be investigated in VLP group, since few patients removed the plate. Study53 has reported that the incidence of 25% of RSD at 9 weeks after fracture and 17% 6 months after fracture. And the RSD was usually occurred in patients treated by EF.54 Only two CSs reported the RSD, and all of the patients suffered RSD were in EF group. However, no significant difference was detected. Additional studies were needed to evaluate this outcome.
According to the criteria of GRADE, the quality evidence of the outcomes was low to very low. The reasons as follows: 1. Two of the included studies didn't describe the randomization method; 2. Four studies didn't carry out allocation concealment; 3. One study had different baseline; 4. Nine studies didn't use ITT analysis or unclear. 5. The study design of CS and no factors that could upgrade the quality of evidence.
The results of this study should be interpreted with caution because of the following limitations. First, most of the statistically significant differences of the results were only in CSs, except DASH scores, infection rate and ulnar variance. Second, relatively small sample sizes of the included studies led to the limitation of our study and made the evidence weaker. Third, publication bias was detected in RCTs based on funnel plot, although the Begg's test and Egger's test did not detect statistical bias. The last, limited by the number of included studies in each outcome, we could not perform subgroup analysis and meta-regression to explore the source of heterogeneity.
Conclusions
In conclusion, VLP could provide better results such as DASH scores, ulnar variance and infection rate. The use of VLP appears to be associated with better results of ROM (flexion, pronation, supination and radial deviation), radiographic parameters (volar tilt and radial inclination) and lower total complication rate and CRPS rate in CSs. Large, rigorous RCTs are needed to improve the evidence.
Conflicts of interest
All of the authors declared that they had no conflict of interest.
Acknowledgments
This work was funded by National Natural Science Foundation of China (No. 81601893).
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Chung K.C., Spilson S.V. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26:908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Chung K.C., Shauver M.J., Birkmeyer J.D. Trends in the United States in the treatment of distal radial fractures in the elderly. La Radiologia Medica. 2009;91:1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shauver M.J., Yin H., Banerjee M., Chung K.C. Current and future national costs to medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36:1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 4.Nellans K.W., Kowalski E., Chung K.C. The epidemiology of distal radius fractures. Hand Clin. 2012;28:113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu Y.C., Chien S.H., Huang P.J. Use of an external fixation combined with the buttress-maintain pinning method in treating comminuted distal radius fractures in osteoporotic patients. J Trauma. 2006;60:330–333. doi: 10.1097/01.ta.0000203538.29179.5b. [DOI] [PubMed] [Google Scholar]
- 6.Atroshi I., Brogren E., Larsson G.U. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445–453. doi: 10.1080/17453670610046389. [DOI] [PubMed] [Google Scholar]
- 7.Strohm P.C., Muller C.A., Boll T., Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures. A randomized trial. J Bone Joint Surg Am. 2004;86-A:2621–2628. doi: 10.2106/00004623-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kara A., Celik H., Oc Y. Flexor tendon complications in comminuted distal radius fractures treated with anatomic volar rim locking plates. Acta Orthop Traumatol Turc. 2016;50:665–669. doi: 10.1016/j.aott.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sugun T.S., Gurbuz Y., Ozaksar K. A new complication in volar locking plating of the distal radius: longitudinal fractures of the near cortex. Acta Orthop Traumatol Turc. 2016;50:147–152. doi: 10.3944/AOTT.2015.15.0233. [DOI] [PubMed] [Google Scholar]
- 10.Gurbuz Y., Kucuk L., Gunay H. Comparison of ultrasound and dorsal horizon radiographic view for the detection of dorsal screw penetration. Acta Orthop Traumatol Turc. 2017;51:448–450. doi: 10.1016/j.aott.2017.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mellstrand Navarro C., Ahrengart L., Tornqvist H., Ponzer S. Volar locking plate or external fixation with optional addition of K-Wires for dorsally displaced distal radius fractures: a randomized controlled study. J Orthop Trauma. 2016;30:217–224. doi: 10.1097/BOT.0000000000000519. [DOI] [PubMed] [Google Scholar]
- 12.Sha L., Chen Q., Sun L. Effectiveness comparison of external fixation and volar locking compression plate in treatment of distal radius fractures of type C. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2015;29:683–687. [PubMed] [Google Scholar]
- 13.Kumbaraci M., Kucuk L., Karapinar L. Retrospective comparison of external fixation versus volar locking plate in the treatment of unstable intra-articular distal radius fractures. Eur J Orthop Surg Traumatol. 2014;24:173–178. doi: 10.1007/s00590-012-1155-0. [DOI] [PubMed] [Google Scholar]
- 14.Yang X., Zhao Y.M., Chen L. Treatment type C fracture of the distal radius with locking compression plate and external fixators. Zhongguo Gu Shang. 2013;26:997–1001. [PubMed] [Google Scholar]
- 15.Moher D., Shamseer L., Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Furlan A.D., Pennick V., Bombardier C., van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009;34:1929–1941. doi: 10.1097/BRS.0b013e3181b1c99f. [DOI] [PubMed] [Google Scholar]
- 17.Wells GA, Shea B, O'Connell D. Newcastle-Ottawa quality assessment scale for case control studies and cohort studies http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 18.Atkins D., Best D., Briss P.A. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hannan E.L. Randomized clinical trials and observational studies: guidelines for assessing respective strengths and limitations. JACC Cardiovasc Interv. 2008;1:211–217. doi: 10.1016/j.jcin.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 20.Mantel N., Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 21.Egol K., Walsh M., Tejwani N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90:1214–1221. doi: 10.1302/0301-620X.90B9.20521. [DOI] [PubMed] [Google Scholar]
- 22.Gradl G., Gradl G., Wendt M. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg. 2013;133:595–602. doi: 10.1007/s00402-013-1698-5. [DOI] [PubMed] [Google Scholar]
- 23.Jeudy J., Steiger V., Boyer P. Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation 'versus' locked volar plating. Injury. 2012;43:174–179. doi: 10.1016/j.injury.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 24.Roh Y.H., Lee B.K., Baek J.R. A randomized comparison of volar plate and external fixation for intra-articular distal radius fractures. J Hand Surg Am. 2015;40:34–41. doi: 10.1016/j.jhsa.2014.09.025. [DOI] [PubMed] [Google Scholar]
- 25.Shukla R., Jain R.K., Sharma N.K., Kumar R. External fixation versus volar locking plate for displaced intra-articular distal radius fractures: a prospective randomized comparative study of the functional outcomes. J Orthop Traumatol. 2014;15:265–270. doi: 10.1007/s10195-014-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wei D.H., Raizman N.M., Bottino C.J. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1568–1577. doi: 10.2106/JBJS.H.00722. [DOI] [PubMed] [Google Scholar]
- 27.Wilcke M.K., Abbaszadegan H., Adolphson P.Y. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop. 2011;82:76–81. doi: 10.3109/17453674.2011.552781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Williksen J.H., Frihagen F., Hellund J.C. Volar locking plates versus external fixation and adjuvant pin fixation in unstable distal radius fractures: a randomized, controlled study. J Hand Surg Am. 2013;38:1469–1476. doi: 10.1016/j.jhsa.2013.04.039. [DOI] [PubMed] [Google Scholar]
- 29.Gereli A., Nalbantoglu U., Kocaoglu B., Turkmen M. Comparison of palmar locking plate and K-wire augmented external fixation for intra-articular and comminuted distal radius fractures. Acta Orthop Traumatol Turc. 2010;44:212–219. doi: 10.3944/AOTT.2010.2325. [DOI] [PubMed] [Google Scholar]
- 30.Jorge-Mora A.A., Cecilia-Lopez D., Rodriguez-Vega V. Comparison between external fixators and fixed-angle volar-locking plates in the treatment of distal radius fractures. J Hand Microsurg. 2012;4:50–54. doi: 10.1007/s12593-012-0072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Richard M.J., Wartinbee D.A., Riboh J. Analysis of the complications of palmar plating versus external fixation for fractures of the distal radius. J Hand Surg Am. 2011;36:1614–1620. doi: 10.1016/j.jhsa.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 32.Rizzo M., Katt B.A., Carothers J.T. Comparison of locked volar plating versus pinning and external fixation in the treatment of unstable intraarticular distal radius fractures. Hand (N Y) 2008;3:111–117. doi: 10.1007/s11552-007-9080-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sato K., Furumachi K., Nishida J. Comparison of the volar locking plate and the bridging external fixator in the treatment of distal radius fracture based on range of wrist motion assessed by functional radiography. Med Sci Monit. 2010;16:Cr207–Cr212. [PubMed] [Google Scholar]
- 34.Schmelzer-Schmied N., Wieloch P., Martini A.K., Daecke W. Comparison of external fixation, locking and non-locking palmar plating for unstable distal radius fractures in the elderly. Int Orthop. 2009;33:773–778. doi: 10.1007/s00264-007-0504-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Westphal T., Piatek S., Schubert S., Winckler S. Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg. 2005;125:507–514. doi: 10.1007/s00402-005-0023-3. [DOI] [PubMed] [Google Scholar]
- 36.Wright T.W., Horodyski M., Smith D.W. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 2005;30:289–299. doi: 10.1016/j.jhsa.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 37.Zhao Y., Cui X.R., Guan J.C. A case control study on the treatment of unstable distal radius fractures with internal and external fixation. Zhongguo Gu Shang. 2011;24:894–897. [PubMed] [Google Scholar]
- 38.Safdari M., Koohestani M.M. Comparing the effect of volar plate fixators and external fixators on outcome of patients with intra-articular distal radius fractures: a clinical trial. Electron Physician. 2015;7:1085–1091. doi: 10.14661/2015.1085-1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williksen J.H., Husby T., Hellund J.C. External fixation and adjuvant pins versus volar locking plate fixation in unstable distal radius fractures: a randomized, controlled study with a 5-year follow-up. J Hand Surg Am. 2015;40:1333–1340. doi: 10.1016/j.jhsa.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 40.Kateros K., Macheras G., Galanakos S.P. External fixation versus "pi" plate for distal radius fractures. J Trauma. 2010;68:166–172. doi: 10.1097/TA.0b013e3181b0d4be. [DOI] [PubMed] [Google Scholar]
- 41.Estrella E.P., Panti P.L. Outcome of unstable distal radius fractures treated with open reduction and internal fixation versus external fixation. Hand Surg. 2012;17:173–179. doi: 10.1142/S0218810412500165. [DOI] [PubMed] [Google Scholar]
- 42.Bajwa A.S., Rammappa M., Lee L., Nanda R. Treatment of unstable distal radius fractures: non-invasive dynamic external fixator versus volar locking plate - functional and radiological outcome in a prospective case-controlled series. SICOT J. 2015;1:34. doi: 10.1051/sicotj/2015033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li-hai Z., Ya-nan W., Zhi M. Volar locking plate versus external fixation for the treatment of unstable distal radial fractures: a meta-analysis of randomized controlled trials. J Surg Res. 2015;193:324–333. doi: 10.1016/j.jss.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 44.Higgins J.P., Green S. The Cochrane Collaboration. 2008. Cochrane handbook for syatematic review of intervention.http://www.cochrane-handbook.org [Google Scholar]
- 45.Plate J.F., Gaffney D.L., Emory C.L. Randomized comparison of volar locking plates and intramedullary nails for unstable distal radius fractures. J Hand Surg Am. 2015;40:1095–1101. doi: 10.1016/j.jhsa.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 46.Smith D.W., Brou K.E., Henry M.H. Early active rehabilitation for operatively stabilized distal radius fractures. J Hand Ther. 2004;17:43–49. doi: 10.1197/j.jht.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 47.McQueen M., Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70:649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 48.Dario P., Matteo G., Carolina C. Is it really necessary to restore radial anatomic parameters after distal radius fractures? Injury. 2014;45:S21–S26. doi: 10.1016/j.injury.2014.10.018. [DOI] [PubMed] [Google Scholar]
- 49.Chen N.C., Jupiter J.B. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89:2051–2062. doi: 10.2106/JBJS.G.00020. [DOI] [PubMed] [Google Scholar]
- 50.Orbay J.L., Fernandez D.L. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 51.Dahl W.J., Nassab P.F., Burgess K.M. Biomechanical properties of fixed-angle volar distal radius plates under dynamic loading. J Hand Surg Am. 2012;37:1381–1387. doi: 10.1016/j.jhsa.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 52.Wang J., Yang Y., Ma J. Open reduction and internal fixation versus external fixation for unstable distal radial fractures: a meta-analysis. Orthop Traumatol Surg Res. 2013;99:321–331. doi: 10.1016/j.otsr.2012.11.018. [DOI] [PubMed] [Google Scholar]
- 53.Atkins R.M., Duckworth T., Kanis J.A. Algodystrophy following Colles' fracture. J Hand Surg. 1989;14B:161–164. doi: 10.1016/0266-7681_89_90118-6. [DOI] [PubMed] [Google Scholar]
- 54.Suso S., Combalía A., Segur J.M., Garcia-Ramíro S., Ramón R. Comminuted intraarticular fractures of the distal end of the radius treated with the Hoffman external fixator. J Trauma. 1993;35:61–66. doi: 10.1097/00005373-199307000-00010. [DOI] [PubMed] [Google Scholar]