Abstract
Objective
There is limited literature concerning the outcomes and role of THA as a surgical option for amputee patients. The aim of this study is to determine the mid-to long-term survival and complication rates of cementless total hip arthroplasty (THA) in patients with contralateral below knee amputations.
Methods
A retrospective review of 54 patients with below knee amputation were perfomed who underwent THA for osteoarthritis of the contralateral hip over a 5-year period between 1999 and 2014. Patients were monitored for at least 5 years and assessed with the Harris Hip Score and activities of daily living scale and by evaluating migration or osteolysis around the acetabular cup and femoral stems (amputee group). The amputee group was compared with a control group (non-amputee group) with the same number of patients.
Results
Differences in the Harris Hip Score (p = 0.021) and activities of daily living scale (p = 0.043) between the two groups were statistically significant lower in the amputee group at 3 months after surgery. However, no differences were found between the groups from 6 months postoperatively to the last follow-up (Harris Hip Score p = 0.812, activities of daily living scale p = 0.885). Radiologically, any cups or stems showed no signs of migration or osteolysis. In the amputee group, dislocation was found in 1 patient 2 months after arthroplasty (p = 0.315) and long stem revision surgery were performed on two patients due to periprosthetic fracture (p = 0.153).
Conclusions
THA performed on the contralateral side of patients with below knee amputation is considered to be an effective treatment with good clinical and radiological results at mid-to long-term follow-up.
Level of evidence
Level IV, therapeutic study.
Keywords: Below knee amputation, Lower extremity amputation, Osteoarthritis, Total hip arthroplasty, Functional recovery
Total hip arthroplasty (THA) is a safe and effective procedure for pain relief and functional improvement in patients who suffer from severe arthritis of the hip joint. Pain is the main indication for THA which cannot be relieved by conservative treatment with radiographic evidence of severe arthritis.
Lower-extremity amputation is known as one of the oldest surgically performed procedures. Amputation is still often regarded as a failure of treatment; however, amputation can be the treatment of choice for severe trauma, chronic vascular disease, congenital limb deficiency, and tumors.1 A high incidence of osteoarthritis in the hip joints has been reported in lower limb below knee amputees.2 Kulkarni et al3 retrospectively evaluated 44 lower extremity amputees and found that 8 (18%) of the contralateral hips had osteoarthritis. This rate was 2-fold higher for the contralateral hip in comparison of the non-amputee population. Struyf et al reported that the prevalence of this degenerative disease is approximately 5–10 times higher and occurs sooner in the intact limb among persons with unilateral lower limb loss compared with individuals without limb loss.4 The altered mechanics of the contralateral hip may influence clinical and radiological results after THA. However, there is limited literature concerning the outcomes and role of THA as a surgical option for amputee patients.5 Here we present the largest retrospective series of THA after contralateral lower extremity amputation. This study is aimed to determine the mid-to long-term survivorship of cementless THA and the incidence of complications, including periprosthetic fracture and early loosening of prosthesis, in patients with contralateral below knee amputation.
Patients and methods
From January 1999 to November 2014, 58 patients (57 male and 1 female) underwent THAs (Total 58 THAs) who had osteoarthritis of the contralateral hip and lower limb below knee amputation at the authors’ institutions. Of these, 54 patients (all male) satisfied the inclusion criteria: capable of undergoing THA, at least 5 years after THA, and having no other lower-extremity neurologic or musculoskeletal problems (amputee group). The cause of amputation was 23 cases of trauma, 15 cases of vascular disease, 10 cases of diabetic foot ulcers, and 6 cases of uncontrolled osteomyelitis.”
The average age of the patients at the time of surgery was 67.8 years (range, 54–75 years), and the average body mass index (BMI) was 25.5 kg/m2 (range, 19.2–33.4 kg/m2). Four senior hip surgeons performed the procedures. In 33 cases, a standard posterolateral approach was used, and in 21 cases, the modified Hardinge approach was used. In all cases, cementless prosthesis was implanted also two screws were used to improve acetabular cup stability. A ceramic-on-ceramic bearing was used in 42 hips (74%) and a metal-on polyethylene bearing was used in 12 hips (23%). A short-term antibiotic prophylaxis with a third-generation cephalosporin and low-molecular-weight heparin was prescribed to all patients. The average duration of follow-up was 84.3 months (range, 60–180 months). These 54 patients were matched for sex, age, time elapsed since surgery, weight, and height to 54 patients who had undergone primary THA with no history of amputation (non-amputee group) (Table 1).
Table 1.
Demographics of patients.
| Amputee group | Non-amputee group | p-value | |
|---|---|---|---|
| Number of hips | 54 | 54 | |
| Gender (Male) | 54 | 54 | |
| Age (years) | 67.8 (54–75) | 67.2 (55–75) | 0.764 |
| BMI (kg/m2) | 25.5 (19.2–33.4) | 24.3 (18.9–34.2) | 0.891 |
| Approach | |||
| Modified Hardinge | 21 | 21 | |
| Standard posterolateral | 33 | 33 | |
| Bearing | |||
| Ceramic – Ceramic | 42 | 42 | |
| Ceramic – Polyethylene | 12 | 12 | |
| Follow-up (Months) | 84.3 (60–180) | 83.7 (60–180) | 0.727 |
Clinical evaluations
To determine the rate of THA among the amputee population, we evaluated the total number of primary THAs performed in amputee patients at our institutions, and divide them into contralateral or ipsilateral lower extremity amputation and further divided them according to level of amputation. We also evaluated the time from amputation to THA. We evaluated our clinical results with the Harris Hip Score6 and activities of daily living scale7 at 3 months, 6 months, and every year after surgery up to 5 years. Superficial and deep infection after arthroplasty were also reviewed.
Radiological evaluations
We radiographically evaluated the patients preoperatively, postoperatively, at 3 and 6 months, and yearly thereafter with use of anteroposterior and lateral radiographs of the affected hip. The cup position was measured via the abduction and version angle by a goniometer. The inclination of the acetabular cup was measured from the line connecting the acetabular teardrop to the line tangential to the acetabular cup opening. Acetabular cup anteversion was measured using the method demonstrated by Widmer.8 We defined osteolysis around the acetabular cup as 4 mm or greater migration and 2 mm or greater radiolucent line of the cup, as reported by DeLee and Charnley.9 The stem position was assessed using goniometric measurements of the angle between the long axis of the femoral stem and the femoral shaft axis on true hip anteroposterior radiographs.10 Normal alignment was specified as a long axis of the femoral stem between 3° of valgus and 3° of varus relative to the femoral shaft axis. In addition, osteolysis around the femoral stem was assessed with anteroposterior and lateral radiographs in use of the Gruen's classification.11
We defined stem subsidence as 3° or greater change or 2 mm or greater position change without osteointegration around the femoral stem. Dislocation and periprosthetic fractures were reviewed during the follow-up period.
Radiologic measurement and evaluation for fracture classification were supervised by two orthopedic surgeons based on anteroposterior and lateral radiographs of the hip joint. Kappa coefficient tests were applied to measure the intra-observer (K1) and inter-observer (K2) reliability of the two observers; both sets of results were shown to be at reliable levels (K1 = 0.88, K2 = 0.81).
The study was approved by our institutional review board; we informed to all patients that their medical data could be used in a scientific study.
Student's t-tests and chi-square tests were calculated by SPSS 18.0 (IBM Co., Armonk, NY, USA) for comparisons between the two groups. p values less than 0.05 were considered statistically significant.
Results
Clinical results
In total, 9762 primary THAs were performed at our institution from 1999 to 2014. THA after contralateral lower extremity amputation represented 0.64% (62 cases), while THA after contralateral lower extremity below knee amputation represented 0.59% (58 cases). Mean time to THA after contralateral lower extremity below knee amputation was 27.5 ± 24.7 years.
Clinically, the differences in the Harris Hip Score6 (p = 0.021) and ADL scale7 (p = 0.043) between the amputee and non-amputee groups were statistically significant at 3 months after surgery. However, from 6 months postoperative to final follow-up, there was no significant difference between groups. There was no significant difference in HHS score6 between the non-amputee group (93.62 [84–100]) and amputee group (91.3 [86–97]) (p = 0.812) or in the ADL scale7 between the non-amputee group (5.864, 5, 6) and the amputee group (5.674, 5, 6) (p = 0.885) at last follow-up (Table 2).
Table 2.
Clinical results in patients.
| Amputee group | Non-amputee group | p-value | |
|---|---|---|---|
| Number of hips | 54 | 54 | |
| Hospital Stay (day) | 15.1 (5–28) | 16.3 (4–31) | 0.804 |
| Harris Hip Score | |||
| 3 months | 86.1 (76–91) | 90.7 (81–100) | 0.021 |
| 6 months | 89.3 (83–97) | 91.5 (84–100) | 0.742 |
| 12 months | 90.7 (85–97) | 94.2 (84–100) | 0.874 |
| 60 months | 91.3 (86–97) | 93.6 (84–100) | 0.812 |
| ADL scale | |||
| 3 months | 4.77 (4–5) | 5.25 (4–5) | 0.043 |
| 6 months | 5.59 (4–5) | 5.57 (4–6) | 0.772 |
| 12 months | 5.61 (4–6) | 5.81 (4–6) | 0.821 |
| 60 months | 5.67 (4–6) | 5.86 (4–6) | 0.885 |
ADL: activities of daily living.
Radiological results
Radiologically, all of the cups appeared to be osseointegrated without evidence of osteolysis.
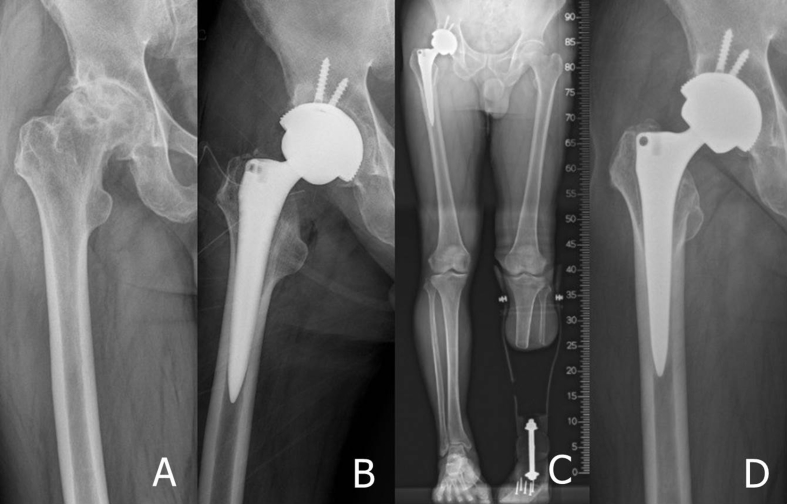
All cups showed no signs of migration or radiolucent lines. In both groups, no signs of subsidence or tilting were found in any stems during follow-up (Fig. 1); in one patient in the amputee group, a radiolucent line, <2 mm wide, was found around of the stem, but the clinical result was good (HHS score: 90, ADL scale: 5) (Fig. 2). Two patients (3.7%) in the amputee group developed a periprosthetic fracture around the femoral stem. In one patient, this occurred two months after his THA operation; he developed a Vancouver type12 B2 periprosthetic femoral fracture after falling down while removing his prosthesis. The stem was stable without any loosening or osteolysis at the last follow-up before the fracture. A long modular stem (Lima Corporate, Udine, Italy) and additional wiring together with 15 cc of auto-cancellous iliac bone graft was used. The fracture was healed 9 months postoperatively. At final follow up (6 years after initial THA operation), he presented with a Harris Hip Score of 90. The second patient developed a Vancouver type12 B2 periprosthetic femoral fracture after falling down while walking on a road due to loosening of his prosthesis four months after his THA operation. The stem was stable without any loosening or osteolysis at the last follow-up before the fracture (3 months after initial THA operation). However, the femoral stem had sunk remarkably and the fracture pattern was unstable with an oblique fracture line (Vancouver type12 B2). A long modular stem (Lima Corporate, Udine, Italy) and additional wiring together with 15 cc of auto-cancellous iliac bone graft was used. Two years after the operation, the fracture was healed successfully (Fig. 3). One patient (1.9%) in the amputee group developed dislocation while taking off his prosthesis 2 months after arthroplasty. After closed reduction, no recurrence of dislocation occurred (Table 3). Superficial and deep infection due to surgery were not found in either group.
Fig. 1.
(A) Preoperative radiographs of a 67-old-year man with primary osteoarthritis of the hip joint. (B) Postoperative radiograph shows excellent implant position of cementless total hip arthroplasty. (C) Postoperative standing whole lower extremity radiographs taken of the prosthetic leg. (D) At 7 years after the operation, the radiograph shows stable fixation of components without subsidence or changes in alignment.
Fig. 2.
(A) Preoperative radiographs of a 73-old-year man with primary osteoarthritis of the hip joint. (B) Postoperative radiograph shows excellent implant position of cementless total hip arthroplasty. (C) Postoperative standing whole lower extremity radiographs take of the prosthetic leg. (D) At 5 years after the operation, the radiograph shows stable fixation of components with a radiolucent line around the proximal femoral stem.
Fig. 3.
(A) Preoperative radiographs of a 70-old-year man with primary osteoarthritis of the hip joint. (B) Postoperative radiograph shows excellent implant position of cementless total hip arthroplasty. (C) At 3 months after the operation, the radiograph shows stable fixation of components without subsidence or changes in alignment. (D) A Vancouver type B2 fracture with stem loosening occurred after a fall 4 months postoperatively. (E) Stem revision was performed using a long distal-fitting and modular type stem with additional circular wiring. (F) At 24 months after revision surgery, an X-ray showed bony union and stable stem fixation.
Table 3.
Radiological results in patients.
| Amputee group | Non-amputee group | p-value | |
|---|---|---|---|
| Number of hips | 54 | 54 | |
| Acetabulum | |||
| Inclination | 45.27 (37–51) | 44.69 (38–50) | 0.918 |
| Anteversion | 21.22 (16–26) | 22.71 (16–25) | 0.767 |
| Osteolysis | 0 | 0 | |
| Femur | |||
| Varus malposition (%) | 1 | 0 | 0.315 |
| Osteolysis | 0 | 0 | |
| Subsidence | 0 | 0 | |
| Periprosthetic Fracture | 2 | 0 | 0.153 |
| Dislocation | 1 | 0 | 0.315 |
Discussion
Arthritis of the hip is a health condition most commonly observed in middle-aged and older individuals.13 However, among persons with unilateral lower limb loss, the prevalence of this degenerative disease is approximately 5–10 times higher and occurs sooner in the intact limb compared with individuals without limb loss.4 A reasonable explanation could be that these patients develop osteoarthritis at a faster rate than non-amputees. Changes in gait pattern with alterations of ground reaction forces in the intact limb have been documented.14 In the current literature, some evidence is found for the hypothesis that gait alteration and increased joint load exhibited by amputees with a prosthesis may result in abnormal joint loading that, over time, may lead to joint pain and degeneration.3, 15 Published data implies that traumatic leg amputees are at a greater risk than non-amputees of developing osteoarthritis in the hip of the intact limb. A retrospective cohort study including 44 male British war veterans showed a prevalence of osteoarthritis of the hip of the intact limb of 23%.3 The altered mechanics of the contralateral hip may influence clinical and radiological results after THA. The goal of the present study was to assess the mid-to long-term (at least 5 years) results of THA in patients with osteoarthritis of the hip who had undergone contralateral below knee amputation. Lower extremity amputees suffer from significant physical disabilities and emotional challenges as a result of their amputation. Most traumatic amputees are successful ambulators; hence, most are exposed to long-term prosthetic use.16 The use of lower-extremity prosthetic leads to gait abnormalities. These abnormalities have been documented such as increased metabolic energy expenditure, decreased walking speed, larger stride width, shorter stride length with the intact limb, and increased stance time and ground reaction forces in the intact limb.14, 17, 18, 19 There is evidence that an increase in ground reaction forces may contribute to weight-bearing joint overloading.20 Therefore, the gait abnormalities shown by amputees with a prosthesis may result in abnormal joint loading over time that may lead to early loosening and wearing of implants in THA patients with contralateral below knee amputation. However, after an average follow-up at least 5 years, satisfactory results found in our study when compared with THA patients without amputation. The mid-to long-term outcomes of the present series indicates that standard THA can be a feasible option for patients with osteoarthritis of the hip with a history of contralateral below knee amputation.
The authors encountered two patients who developed periprosthetic fracture during the follow-up period. There is an increased incidence of periprosthetic femoral fractures following THA.21 The increasing number of e lderly patients who are at risk of falling is the main reason, and the expanded indications for THA, which leads to increased rates of arthroplasty and hip revision arthroplasty. Kulkarni et al found that 60% of amputees advised that falling affected their daily life, work, leisure, and confidence.22 These falls are due to altered lower limb mechanics; transtibial amputees make compensatory gait adjustments. The loss of the plantar flexor muscles, combined with muscle weakness and the mechanical limitations of the prosthetic foot, predispose transtibial amputees towards an increased risk of falling compared with age-matched, able-bodied individuals.23 In amputee non-fallers, hip power absorption on the intact side was significantly smaller than that of fallers. This could reduce demands on the hip flexor musculature in the amputee non-fallers, leading to decelerated extension of the thigh as it rotated backwards in preparation for swing.24 These findings suggest that fall prevention and prosthetic rehabilitation might benefit from therapies directed towards improving eccentric muscle strength of the hip joints of the intact limb, to control progression and stability during locomotion. One notable finding is that two patients with periprosthetic (around the femoral stem) fractures experienced prosthetic leg-related falls, despite the absence of osteoporosis or problems with walking ability. The stable stem became loose secondary to the periprosthetic fracture due to excessive rotational force on the leg with THA. According to the results of the authors’ research, it seems that functional recovery of amputated patients was slower in progress than that of non-amputee patients until 3 months after HA. Dislocation and periprosthetic fractures occurred within almost 3 months related to a prosthetic leg. Therefore, the authors believed that after HA of the amputated patients with a high risk of fall, it was necessary to carry out adequate education for prevention of the trauma related to the prosthesis. (Take off the prosthetic legs in some safer state, wear it, and firmly fix not to loosen during walking, etc.).
The present study has several limitations. We included a small number of cases, the procedures were performed by four surgeons, more than one kind of prosthetic was used, and this study was retrospective in design. Nevertheless, we demonstrated that patients with below knee amputation undergoing cementless THA of the contralateral hip show favorable mid-to long-term results. Further prospective long term studies are needed in the future.
THA performed on the contralateral side of the patients with a history of below knee amputation is considered to be an effective treatment with good clinical and radiological results at mid-to long-term follow-up. However, because of the high risk of falls due to use of a prosthetic leg, fracture around the femoral stem (periprosthetic fracture) may occur, and although the femoral stem is stable before the fracture, the stem may loosen (Vancouver type12 B2 fracture).
Conflict of interest
No conflicts declared.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Gailey R., Allen K., Castles J. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45:15–29. doi: 10.1682/jrrd.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- 2.Burke M.J., Roman V., Wright V. Bone and joint changes in lower limb amputees. Ann Rheum Dis. 1978;37:252–254. doi: 10.1136/ard.37.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kulkarni J., Adams J., Thomas E., Silman A. Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clin Rehabil. 1998;12:348–353. doi: 10.1191/026921598672393611. [DOI] [PubMed] [Google Scholar]
- 4.Struyf P.A., van Heugten C.M., Hitters M.W., Smeets R.J. The prevalence of osteoarthritis of the intact hip and knee among traumatic leg amputees. Arch Phys Med Rehabil. 2009;90:440–446. doi: 10.1016/j.apmr.2008.08.220. [DOI] [PubMed] [Google Scholar]
- 5.Amanatullah D.F., Trousdale R.T., Sierra R.J. Total hip arthroplasty after lower extremity amputation. Orthopedics. 2015;38:394–400. doi: 10.3928/01477447-20150504-56. [DOI] [PubMed] [Google Scholar]
- 6.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 7.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 8.Widmer K.H. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. doi: 10.1016/j.arth.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 9.DeLee J.G., Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 10.Khalily C., Lester D.K. Results of a tapered cementless femoral stem implanted in varus. J Arthroplasty. 2002;17:463–466. doi: 10.1054/arth.2002.32171. [DOI] [PubMed] [Google Scholar]
- 11.Gruen T.A., McNeice G.M., Amstutz H.C. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 12.Brady O.H., Garbuz D.S., Masri B.A., Duncan C.P. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000;15:59–62. doi: 10.1016/s0883-5403(00)91181-1. [DOI] [PubMed] [Google Scholar]
- 13.Losina E., Weinstein A.M., Reichmann W.M. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res. 2013;65:703–711. doi: 10.1002/acr.21898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Czerniecki J.M. Rehabilitation in limb deficiency. 1. Gait and motion analysis. Arch Phys Med Rehab. 1996;77:S3–S8. doi: 10.1016/s0003-9993(96)90236-1. [DOI] [PubMed] [Google Scholar]
- 15.Norvell D.C., Czerniecki J.M., Reiber G.E. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil. 2005;86:487–493. doi: 10.1016/j.apmr.2004.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moore T.J., Barron J., Hutchinson F., Golden C., Ellis C., Humphries D. Prosthetic usage following major lower extremity amputation. Clin Orthop Relat Res. 1989;238:219–224. [PubMed] [Google Scholar]
- 17.Zuniga E.N., Leavitt L.A., Calvert J.C., Canzoneri J., Peterson C.R. Gait patterns in above-knee amputees. Arch Phys Med Rehabil. 1972;53:373–382. [PubMed] [Google Scholar]
- 18.Seroussi R.E., Gitter A., Czerniecki J.M., Weaver K. Mechanical work adaptations of above-knee amputee ambulation. Arch Phys Med Rehabil. 1996;77:1209–1214. doi: 10.1016/s0003-9993(96)90151-3. [DOI] [PubMed] [Google Scholar]
- 19.Hershler C., Milner M. Angle-angle diagrams in above-knee amputee and cerebral palsy gait. Am J Phys Med. 1980;59:165–183. [PubMed] [Google Scholar]
- 20.Robbins S., Waked E., Krouglicof N. Vertical impact increase in middle age may explain idiopathic weight-bearing joint osteoarthritis. Arch Phys Med Rehabil. 2001;82:1673–1677. doi: 10.1053/apmr.2001.26255. [DOI] [PubMed] [Google Scholar]
- 21.Lindahl H., Malchau H., Herberts P., Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 22.Kulkarni J., Toole C., Morris J., Hirons R., Wright S. Falls in patients with lower limb amputations: prevalence and contributing factors. Physiotherapy. 1996;82:130–135. [Google Scholar]
- 23.Miller W.C., Speechley M., Deathe B. The prevalence and risk fctors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil. 2001;82:1031–1036. doi: 10.1053/apmr.2001.24295. [DOI] [PubMed] [Google Scholar]
- 24.Eng J.J., Winter D.A. Kinetic analysis of the lower limbs during walking: what information can be gained from a three-dimensional model? J Biomech. 1995;28:753–758. doi: 10.1016/0021-9290(94)00124-m. [DOI] [PubMed] [Google Scholar]