Abstract
Objective
The purpose of this study was to evaluate the diagnostic value of the patellar tendon wavy (PTW) sign for an anterior cruciate ligament (ACL) tear on MRI.
Methods
One hundred MRI scans were prospectively analyzed, with 50 patients with an ACL tear underwent an ACL reconstruction (group 1) and 50 patients with knee complaints other than ACL tear (group 2). The PTW sign was confirmed on the sagittal MRI. In addition, the patellar tendon length, tibial-femoral angle and tibial anterior translation (TAT) were compared between the groups.
Results
The PTW sign was present in 41/50 (82%) MRI scans in group 1 and 10/50 (20%) in group 2, with significant difference between two groups (p = 0.000). Significant differences were also found, in medial TAT (6.29 ± 3.25 mm versus 3.12 ± 2.85 mm) and in lateral TAT (7.62 ± 3.85 mm versus 1.58 ± 3.93 mm) between two groups (both p = 0.000). Comparison of MRI with and without PTW sign, ACL injury was found to be of significant difference with 41/51 (80.4%) versus 9/49 (18.4%) (p = 0.000), and both medial and lateral TAT were with significant differences, 5.39 ± 3.90 mm versus 3.99 ± 2.71 mm (p = 0.039) and 7.67 ± 3.77 mm versus 1.40 ± 3.81 mm (p = 0.000), respectively. The sensitivity and specificity of PTW sign were 82% and 80%. The positive and negative predictive value were 80.4% and 81.6%. The diagnosis accuracy was 81%.
Conclusion
The PTW sign is a useful secondary MRI sign to establish the diagnosis of an ACL tear. It may be associated with the TAT secondary to an ACL tear.
Level of evidence
Level III, diagnostic study.
Keywords: Anterior cruciate ligament, MRI diagnosis, Secondary sign, Patellar tendon wavy sign, Tibial anterior translation
Introduction
Magnetic resonance imaging (MRI) has been a standard means in the diagnosis of anterior cruciate ligament (ACL) tear, which is a common knee injury in the clinical practice. However, the integrity of the ACL is occasionally difficult to assess because the ACL is not entirely included on a single sagittal image.1 In addition, intra-articular effusion, concomitant meniscus injury, presence of variation within the ligament and suboptimal selection of the sagittal image plane could increase the difficulty to make a definite diagnosis by direct signs,1, 2 especially for the juniors.
Therefore, recent studies have attached the importance of the secondary signs to support the presumptive diagnosis of an ACL tear. Since the ACL is a major stabilizer of the knee joint to prevent abnormal anterior translation, any damage to the ACL causes variable degrees of abnormal translation at the knee joint.3 So a series of secondary signs of the ACL injury associated with tibial anterior translational changes have been described on MRI, with different sensitivity and specificity.1, 4, 5
In our clinical practice, we have observed the wavy appearance of the patellar tendon on sagittal MRI in cases of an ACL tear and we defined it as the patellar tendon wavy (PTW) sign. The purpose of this study was to evaluate its diagnostic value for an ACL tear prospectively on MRI. The study hypothesis was that: (1) there was an association between the PTW sign and tibial anterior translation secondary to an ACL tear; (2) the PTW sign could be applied in the diagnosis of an ACL tear on MRI.
Material and methods
Patients and MRI examination
One hundred MRI scans were prospectively analyzed, with 50 patients with a ruptured ACL (group 1) and 50 patients with knee complaints other than ACL injury (group 2) at our institution from February to November in 2016. The time interval between knee complaints and MR examination ranged from 3 days to 14 months. All ACL conditions were confirmed under arthroscopy. The inclusion criteria were as follows: (1) a healthy contralateral knee; (2) no history of previous surgery on the injured knee; (3) without any other tibial-femoral ligament injury; (4) absence of patellofemoral symptoms and systemic illnesses. This study was approved by our institutional review board and informed consent was obtained from all participants. The demographic data were present in Table 1, with no statistical difference between the two groups.
Table 1.
Patient characteristics.
| Variable | ACL injury group | Non-ACL injury group | P Value | |
|---|---|---|---|---|
| Sex (M/F) | 31/19 | 34/16 | x2 = 0.396 | 0.529 |
| Side (L/R) | 28/22 | 24/26 | x2 = 0.641 | 0.423 |
| Age, y | 35.5 ± 9.0 | 34.7 ± 6.0 | t = 0.547 | 0.586 |
The MR images used for this study were obtained with a 1.5 T MRI (Sonata Magnetom, Siemens Medical Solutions, Erlagen, Germany) with the knee in or near full extension. Foam pads were placed posterior and lateral to the knee to immobilize the knee within the center of the coil and minimize patient motion. No additional padding was used to accentuate anterior translation of the tibia. The images were obtained in the sagittal and coronal planes by using spin-echo intermediate-weighted (1800–2200/20–30 [repetition time msec/echo time msec]) and T2-weighted (1800–2200/80–90) sequences, and transverse images were obtained by using a gradient-recalled-echo sequence (650/13; flip angle, 20°). The field of view was 14–16 cm, the section thickness was 3–4 mm with a 0.5-mm gap, the matrix was 192–256 × 256, and an average of one to two signals was acquired.
Image analysis
All measurements were performed on the PACS (Picture Archiving and Communications System; General Electrics, Chicago, IL) by the use of a mouse cursor with automated distance or angle calculation. All MR images were reviewed by two experienced orthopedic surgeons, who were blinded to the clinical history and examination findings. If any discrepancies arose, the MRI was reviewed by the third sports medicine specialist and the problems were solved through consensus in groups.
In this study, the patellar tendon length, tibial-femoral angle and tibial translation were measured on the sagittal MRI. In addition, the PTW sign was identified by one orthopedic surgeon and one radiologist, and the radiologist performed the second identification after 4 weeks.
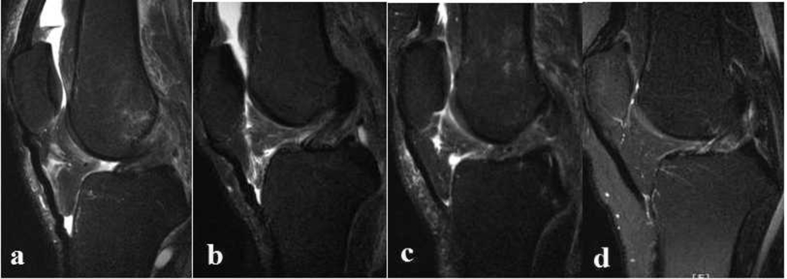
In the sagittal proton density weighted image that best showed the intra-articular course of the ACL, the appearance of the patellar tendon was observed. The whole wavy appearance or partial wavy appearance usually near the tibial attachment was confirmed to be the positive PTW sign (Fig. 1). The distance between the patellar and tibial attachment points was measured as patellar tendon length. The longitudinal axis of the tibia and femur was determined and the angle was measured as tibial-femoral angle.
Fig. 1.
Series of sagittal T2-weighted MRI demonstrated the patellar tendon wavy (PTW) sign and ACL tear. a: ACL tear (+) and PTW sign (+); b: ACL tear (−) and PTW sign (+); c: ACL tear (+) and PTW sign (−); d: ACL tear (−) and PTW sign (−). (+): positive; (−): negative.
According to the previous studies,6, 7 the slice that included the medial edge of the fibula was chosen as a landmark for the center of the lateral compartment and that with the attachment of the medial head of the gastrocnemius was as the center of the medial compartment. Two lines crossing the most posterior point of the tibial plateau and the most posterior point of the femoral condyle were drawn parallel to the long axis of the image. The perpendicular distance between these lines was measured as the lateral and medial tibial anterior translation, respectively.
Statistical analysis
Before the investigation, the sample size was estimated based on the expected sensitivity of 80%. A power calculation was performed with a confidence level of 95% (α = 0.05) and a power (1-β) of 80%. This yielded an estimated sample size of 49 patients per group.
Kappa value was calculated to analyze the intra-observer and inter-observer reliability. Values of 0.81–1.00 indicate excellent correlation; 0.61–0.80, substantial correlation; 0.41–0.60, moderate correlation; 0.21–0.40, fair correlation; and 0.00–0.20, poor correlation.
The statistical analysis was performed with SPSS 13.0 software (SPSS Inc., Chicago, IL). The Kolmogorov–Smirnov test was used to test the normality of the variances. The independent t-test was used for the parametric variance and Mann–Whitney U test for nonparametric variances. The chi-square test was for the categorical variable as the rate of the PTW sign. Significance was set at p ≤ 0.05.
Results
Kappa analysis of sign determinations yielded a value of 0.83 and 0.88, which indicates the excellent inter-observer and intra-observer correlation.
Between the ACL-injury and non-injury group, there were no significant differences for the patellar tendon length and tibial-femoral angle. Significant differences in tibial anterior translation were found, 6.29 ± 3.25 mm versus 3.12 ± 2.85 mm in medial tibial anterior translation and 7.62 ± 3.85 mm versus 1.58 ± 3.93 mm in lateral tibial anterior translation. The PTW sign was found on MRI in 41/50 (82%) ACL tears and in 10/50 (20%) non-ACL injured knees, with significant difference between two groups (Table 2).
Table 2.
Results of measurements between ACL injury and non-ACL injury group.
| ACL injury group | Non-ACL injury group | P value | ||
|---|---|---|---|---|
| Tibial-femoral angle | −0.14 ± 2.80 | 0.32 ± 2.40 | Z = 1.106 | 0.269 |
| Tibial anterior translation | ||||
| Medial | 6.29 ± 3.25 | 3.12 ± 2.85 | Z = 4.787 | 0.000 |
| Lateral | 7.62 ± 3.85 | 1.58 ± 3.93 | t = 7.766 | 0.000 |
| Patellar tendon length | 44.10 ± 4.56 | 43.31 ± 5.20 | Z = 1.145 | 0.252 |
| Patellar tendon wave sign | 41/50 (82%) | 10/50 (20%) | x2 = 38.455 | 0.000 |
Comparison of MRI with and without the PTW sign, ACL injury was found to be of significant difference with 41/51 (80.4%) versus 9/49 (18.4%), and both medial and lateral tibial anterior translation were with significant differences, 5.39 ± 3.90 mm versus 3.99 ± 2.71 mm and 7.67 ± 3.77 mm versus 1.40 ± 3.81 mm, respectively (Table 3).
Table 3.
Results of measurements on MRI with and without PTW sign.
| MRI with PTW sign | MRI without PTW sign | P value | ||
|---|---|---|---|---|
| Tibial-femoral angle | −0.22 ± 2.69 | 0.16 ± 2.53 | Z = 1.000 | 0.317 |
| Tibial anterior translation | ||||
| Medial | 5.39 ± 3.90 | 3.99 ± 2.71 | t = 2.096 | 0.039 |
| Lateral | 7.67 ± 3.77 | 1.40 ± 3.81 | t = 8.281 | 0.000 |
| Patellar tendon length | 44.04 ± 5.76 | 43.36 ± 3.79 | Z = 0.331 | 0.741 |
| ACL injury | 41/51 (80.4%) | 9/49 (18.4%) | x2 = 38.455 | 0.000 |
PTW sign: patellar tendon wavy sign.
Based on these results, the sensitivity and specificity of the PTW sign as an indirect sign of ACL tear were found to be 82% and 80%. The positive and negative predictive value were 80.4% and 81.6%. The diagnosis accuracy was 81% (Table 4).
Table 4.
Performance parameters of MRI with PTW sign in ACL tear diagnosis.
| Index | Sensitivity | Specificity | PPV | NPV | LR+ | LR− | Accuracy |
|---|---|---|---|---|---|---|---|
| MRI with PTW sign | 82% | 80% | 80.4% | 81.6% | 4.1 | 0.225 | 81% |
PTW sign: patellar tendon wavy sign; PPV: positive predictive value; NPV: negative predictive value; LR+: positive likelihood ratio; LR−: negative likelihood ratio.
Discussion
The most important finding of present study was that 82% of patients with ACL tear have a positive PTW sign on MRI, significantly more than that in non-ACL injured knees. The sensitivity and specificity of the PTW sign in the diagnosis of ACL tear were 82% and 80%, and the diagnosis accuracy was 81%. To our knowledge, this sign was first descried by a sample case,8 and the present study was the first study to evaluate its diagnostic value for an ACL tear on MRI.
MRI is a widely accepted imaging choice to diagnose of ACL tear with three direct MR findings described: (1) an irregular wavy contour of the anterior margin of the ACL, (2) high signal intensity within the substance of the ACL on T2-weighted images, and (3) discontinuity of the ACL on sagittal images.9 However, there are several reasons why the normal ACL may appear to be like tearing on the routine sagittal MRI. These include the presence of mucoid or eosinophilic degeneration within the ligament, partial volume averaging of the ACL with lateral femoral condyle or periligamentous fat, and suboptimal selection of the sagittal imaging plane to view the ACL in continuity.1, 2
Therefore, recent studies have attached the importance of secondary signs of ACL injury to improve the physician confidence and provide further supportive evidence of an ACL tear. Many secondary signs have been reported such as anterior tibial translation, buckling of posterior cruciate ligament, bone bruising, Segond fracture and uncovered lateral meniscus, with different sensitivity and specificity.1, 4, 5 And these researches are still ongoing and lateral femoral notch sign, anteromedial tibial rim sign and vertically oriented lateral collateral ligament sign have been reported one after the other recently.10, 11, 12
The present study showed that PTW sign as a secondary sign can be used to diagnose an ACL tear. The patellar tendon extends from the distal margin of the apex and slopes straightly and inferiorly to insert onto the tibial tuberosity. The longitudinal length was 40.2 mm. The width was 30.3 and 24.0 mm and thickness was 3.2 and 5.0 mm for the proximal and distal part.13, 14 Normally, it is a flat frontal structure that can be identified as a straight hypointense structure without the wavy appearance on MRI sagittal sequences.14 The whole or partial wavy appearance usually near the tibial attachment was confirmed to be the positive PTW sign. In the present study, the whole PTW sign was easily recognized, and there were some discrepancy about the partial PTW sign in five cases, 3 cases were with an ACL tear and 2 cases were without an ACL tear. Discussion in our research group and combination with the direct MRI findings of the ACL solved the discrepancy successfully.
Many factors may have an effect on the change of the patellar tendon wavy including position of patella and length of patellar tendon, knee hyperextension and the tibial anterior translation. In the process of obtaining procedure, the knee was in full or near full extension without any additional padding to accentuate tibial anterior translation, and the tibial-femoral angle was measured to be nearly 0°, so the knee hyperextension was avoided to cause the patellar tendon change. In addition, the length of patellar tendon was average 44.10 mm in the ACL injury group and 44.04 mm in the MRI with positive PTW sign group, similar to the results of a previous report.14 Comparision between the ACL injury and non-injury group, the only significant difference was the tibial anterior translation, both medial and lateral. From an anatomical view, the anterior translation of tibia relative to femur may shorten the course of the patellar tendon and result in the patellar tendon wavy appearance. The anterior tibial translation was also with significant differences between MRI with and without PTW sign groups. Therefore, the patellar tendon wavy sign may be associated with tibial anterior translation secondary to the ACL tear.
The ACL prevents both anterior tibial translation on the femur and also anterolateral rotatory instability. Therefore, the deficiency of the ACL may lead to the anterior translation of tibia, especially the lateral tibia plateau. Many studies have quantitatively analyzed the degree of anterior translation of the tibia relative to the femur on MRI with great variations. Some results were summarized in the Table 5.6, 7, 15 The reason for the variability is most likely related to factors such as the different measure methods, the degree of concurrent capsular and ligamentous injury, meniscal integrity, variable re-attachment of the ACL to the surrounding synovial envelope in cases of a chronic ACL injury.16, 17
Table 5.
Review of literature of the measurement of TAT on MRI.
| The study | Method | Patient group | Medial TAT | Later TAT |
|---|---|---|---|---|
| Vahey14 | Method 1 | Intact ACL | −0.5 ± 0.5 | 0.1 ± 0.5 |
| Acute ACL tear | 2.7 ± 0.5 | 3.3 ± 0.8 | ||
| Chronic ACL tear | 3.0 ± 0.4 | 4.5 ± 0.6 | ||
| Method 2 | Intact ACL | 0.3 ± 0.5 | 0.8 ± 0.6 | |
| Acute ACL tear | 3.4 ± 0.5 | 4.1 ± 1.0 | ||
| Chronic ACL tear | 4.3 ± 0.5 | 5.8 ± 0.7 | ||
| Okazaki7 | Method 1 | Intact ACL | −1.7 ± 1.5 | −2.0 ± 3.2 |
| ACL tear | 0.5 ± 2.4 | 8.7 ± 8.0 | ||
| Ng6 | Method 2 | Intact ACL | 0.18 ± 2.15 | 0.55 ± 3.11 |
| Partial ACL tear | 3.56 ± 5.26 | 9.27 ± 5.39 | ||
| Complete ACL tear | 4.08 ± 4.20 | 6.54 ± 3.75 | ||
| Present study | Method 2 | Intact ACL | 3.12 ± 2.85 | 1.58 ± 3.93 |
| ACL tear | 6.29 ± 3.25 | 7.62 ± 3.85 |
TAT: tibial anterior translation; Method 1: the degree of TAT is measured with regard to a plane perpendicular to the tibial plateau; Method 2: the degree of TAT is measured with regard to a plane parallel to the long axis of the image.
The present study had several limitations. First, the acute or chronic ACL tear was not distinguished and the associated meniscal or osteochondral injury was not analyzed, which may have an effect on the tibial anterior translation and the patellar tendon appearance. However, the present study is more practical because patient population is a mixture of acute and chronic injury in daily clinical practice. Second, the patient number, although meets the statistical demand, was still small, a large investigation would be better to determine its prevalence and reveal its relation to tibial anterior translation secondary to an ACL tear.
Conclusion
Based on the present study, the sensitivity and specificity of PTW sign as a secondary sign of an ACL tear was found to be of 82% and 80%. The positive and negative predictive value were 80.4% and 81.6%. The diagnosis accuracy was 81%. The PTW sign is a useful secondary MRI sign to establish the diagnosis of an ACL tear. It may be associated with the tibial anterior translation secondary to the ACL tear.
Conflicts of interest
The authors declare that they have no competing interests.
Ethical board review statement
All the methods described in this study were approved by the ethics committee of Third Hospital of Hebei Medical University and all patients gave informed consent in the study.
This material has not been published and is not under consideration elsewhere.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Tung G.A., Davis L.M., Wiggins M.E., Fadale P.D. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993;188:661–667. doi: 10.1148/radiology.188.3.8351329. [DOI] [PubMed] [Google Scholar]
- 2.Hodler J., Haghighi P., Trudell D., Resnick D. The cruciate ligaments of the knee: correlation between MR appearance and gross and histologic findings in cadaveric specimens. AJR Am J Roentgenol. 1992;159:357–360. doi: 10.2214/ajr.159.2.1632355. [DOI] [PubMed] [Google Scholar]
- 3.Dienst M., Burks R.T., Greis P.E. Anatomy and biomechanics of the anterior cruciate ligament. Orthop Clin North Am. 2002;33:605–620. doi: 10.1016/s0030-5898(02)00010-x. [DOI] [PubMed] [Google Scholar]
- 4.Brandser E.A., Riley M.A., Berbaum K.S., el-Khoury G.K., Bennett D.L. MR imaging of anterior cruciate ligament injury: independent value of primary and secondary signs. Am J Roentgenol. 1996;167:121–126. doi: 10.2214/ajr.167.1.8659355. [DOI] [PubMed] [Google Scholar]
- 5.Robertson P.L., Schweitzer M.E., Bartozzi A.R., Ugoni A. Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology. 1994;193:829–834. doi: 10.1148/radiology.193.3.7972833. [DOI] [PubMed] [Google Scholar]
- 6.Ng A.W., Griffith J.F., Hung E.H., Law K.Y., Ho E.P., Yung P.S. Can MRI predict the clinical instability and loss of the screw home phenomenon following ACL tear? Clin Imag. 2013;37:116–123. doi: 10.1016/j.clinimag.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Okazaki K., Miura H., Matsuda S. Assessment of anterolateral rotator instability in the anterior cruciate ligament-deficient knee using an open magnetic resonance imaging system. Am J Sports Med. 2007;35:1091–1097. doi: 10.1177/0363546507299530. [DOI] [PubMed] [Google Scholar]
- 8.John Hunter's MSK Collection: Knee MRI Case 154. https://www.mypacs.net/cases/ACL-TEAR-WITH-WAVY-PATELLAR-TENDON-798843.html.
- 9.Barry K.P., Mesgarzadeh M., Triolo J., Moyer R., Tehranzadeh J., Bonakdarpour A. Accuracy of MRI patterns in evaluating anterior cruciate ligament tears. Skelet Radiol. 1996;25:365–370. doi: 10.1007/s002560050096. [DOI] [PubMed] [Google Scholar]
- 10.Herbst E., Hoser C., Tecklenburg K. The lateral femoral notch sign following ACL injury: frequency, morphology and relation to meniscal injury and sports activity. Knee Surg Sports Traumatol Arthrosc. 2015;23:2250–2258. doi: 10.1007/s00167-014-3022-5. [DOI] [PubMed] [Google Scholar]
- 11.James S.L., Connell D.A. The vertically orientated fibular collateral ligament: a secondary sign of anterior cruciate ligament rupture on magnetic resonance imaging. Eur Radiol. 2006;16:1854–1856. doi: 10.1007/s00330-005-2858-y. [DOI] [PubMed] [Google Scholar]
- 12.Wissman R.D., England E., Mehta K., Burch M., Javadi A., Newton K. The anteromedial tibial rim sign: an indicator of patellotibial impaction in acute anterior cruciate ligament tears. J Comput Assist Tomogr. 2015;39:57–63. doi: 10.1097/RCT.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 13.Basso O., Johnson D.P., Amis A.A. The anatomy of the patellar tendon. Knee Surg Sports Traumatol Arthrosc. 2001;9:2–5. doi: 10.1007/s001670000133. [DOI] [PubMed] [Google Scholar]
- 14.Yoo J.H., Yi S.R., Kim J.H. The geometry of patella and patellar tendon measured on knee MRI. Surg Radiol Anat. 2007;29:623–628. doi: 10.1007/s00276-007-0261-x. [DOI] [PubMed] [Google Scholar]
- 15.Vahey T.N., Hunt J.E., Shelboume K.D. Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology. 1993;187:817–819. doi: 10.1148/radiology.187.3.8497637. [DOI] [PubMed] [Google Scholar]
- 16.Kocher M.S., Steadman J.R., Briggs K.K., Sterett W.I., Hawkins R.J. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:629–634. doi: 10.1177/0363546503261722. [DOI] [PubMed] [Google Scholar]
- 17.Snyder-Mackler L., Fitzgerald G.K., Bartolozzi A.R., Ciccotti M.G. The relationship between passive joint laxity and functional outcome after anterior cruciate ligament injury. Am J Sports Med. 1997;25:191–195. doi: 10.1177/036354659702500209. [DOI] [PubMed] [Google Scholar]