Abstract
Objective
The aim of this study was to compare the efficacy of extracorporeal shock wave therapy (ESWT) and therapeutic ultrasound (US) in the treatment of lateral epicondylosis (LE).
Methods
Our study enrolled 50 patients with LE. Patients were randomized into two groups. Group 1 underwent therapeutic US (n = 24; 5 males and 15 females; mean age: 43.75 ± 4.52) Group 2 underwent ESWT (n = 20; 8 males and 16 females; mean age: 46.04 ± 9.24). Patients were evaluated at baseline, after treatment,and 1 month following treatment. The outcome measures were the visual analog scale (VAS), algometer, grip dynamometer, quick-disability of the arm,shoulder,and hand (QDASH), patient-rated tennis elbow evaluation (PRTEE), and Short Form-36 (SF-36) health survey questionnairre.
Results
Both groups showed significant improvements in terms of VAS (all p values < 0.0001), dynamometer (p = 0.001 vs p = 0.015), algometer (all p values < 0.0001), PRTEE (all p values < 0.0001), QDASH (all p values < 0.0001), and SF-36 scores (p = 0.001 vs p = 0.005) within time. There was no significant difference between the two groups, except algometer scores in favor of ESWT (p = 0.029).
Conclusion
ESWT and therapeutic US are equally effective in treating LE. ESWT is an alternative therapeutic intervention and as effective as US.
Level of evidence
Level III, Therapeutic study.
Keywords: Lateral epicondylosis, Ekstracorporeal shock wave therapy, Ultrasound, Tennis elbow, Algometer
Introduction
Lateral epicondylosis (LE) was first identified by the German doctor Runge in 1873 as writer's cramp or tennis elbow.1,2 Although its etiology is not clearly known, Cyriax identified 26 possible mechanisms and grouped it into neuro-irritative process, repetitive pain, and tendon injury.3 The primary LE pathology is the mechanical stress at insertion of the extansor carpi radialis brevis muscle. Tendons are hypovascular in the proximal insertional site. This hypovascularity causes hypoxic tendon degenerations secondary to muscular activity. Therefore ischemia is an important etiological factor in LE. Many studies of degenerative or impaired tendons showed no inflammatory cells but indicated many fibroblasts and vascular hyperplasia. These studies demonstrate that LE is fibroblastic and demonstrate a vascular response to angiofibroblastic degeneration known as “tendinosis”.4, 5
LE is one of the most common lesions of the arm characterized by pain in the extensor muscles of the forearm and lateral epicondyle, the origin of wrist extensors.6, 7, 8 LE often presents in individuals who perform repetitive, resistance-based, and wrist–extension activities. If left untreated, it may lead to chronic pain syndrome, sensitivity, and pain in the lateral epicondyle, particularly with resistive wrist and middle-finger extension. Grip strength may decrease and activities of daily (ADL) may be drastically limited.9 LE can be diagnosed easily through clinical examination.
The main goals for treating LE are to relieve pain, decrease recovery time, ease the arm's overload, and to enable the patients' return to ADLs. Conservative therapeutic options involve orthotics, cryotherapy, extracorporeal shock wave therapy (ESWT), ultrasound (US), laser, acupuncture, massage, manipulation–mobilization, therapeutic exercises, and pharmacological treatment.4, 10
There are few studies with contradictory results, addressing the treatment of LE using ESWT.11 It is difficult to compare due to methodological differences between studies. In these studies, ESWT was tested as a single therapeutic method, and studies comparing other therapeutic methods with ESWT were limited.12 The aim of this study was to compare the effectiveness of two different therapeutic methods and determine the superior method.
Material and methods
Design
Prospective, randomized, single-blind, clinical trial.
Power analysis
In the initial study, a pilot study was conducted on 10 patients from each group. Power Analysis and Sample Size were used to determine the sample size [G * Power (v3.1.7)] (PA SS; 2008 statistical software (Utah, USA). A total of 20 patients per group would provide 80% statistical power and a 5% significance level (effect size d = 0.92) according to the algometer scores.
Patients
This study consists of 50 patients of 18–65 years who presented with minimum 3 months lasted elbow pain and were diagnosed with chronic LE between April 2014 and July 2014 at the Physical Medicine and Rehabilitation Clinic of our hospital. The study protocol was approved by the ethics committee of the hospital and written informed consent was obtained from all patients.
Patients experiencing pain and sensitivity over the lateral epicondyle or obtaining positive tests in resistive wrist extension (Cozen's test), resistive middle-finger extension (Maudley's test), and passive wrist flexion (Mill's test) were diagnosed with LE.9,13
Patients with a history of elbow surgery, corticosteroid injection in the last 1 month, forearm and arm fracture, cervical radiculopathy or entrapment neuropathy, acute infection, cardiac pace-maker, vascular disorder, and interstitial implant were excluded from the study.
Procedures
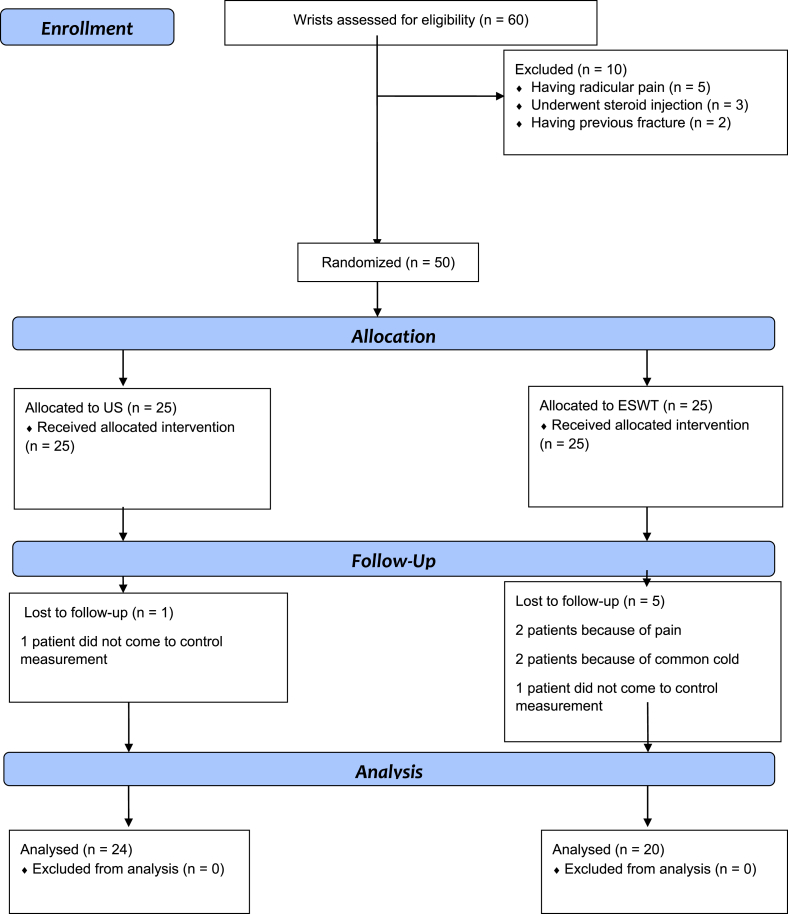
Sixty patients were eligible for the study, 10 were excluded. The patients were randomly assigned into two randomized groups (by coin tossing method) of 25 to receive either therapeutic US or ESWT. In total, 1 patient in the US group and 3 patients in the ESWT group dropped out. Two patients in the ESWT group left the study because of pain. A total of 24 patients in the US group and 20 patients in the ESWT group completed the study (Fig. 1).
Fig. 1.
Flow diagram.
Therapeutic US was administered using a BTL-58205 device (BTL Industries Limited, London, United Kingdom) with a transducer which has 1 cm2 application area, at 1.5 W/cm2, 1 MHz frequency, continuous mode in painful area, 5 min once a day, 5 days a week, for 10 sessions in total. Aquasonic gel was used along with the full contact technique in rotational movements at a vertical angle to the skin.
ESWT therapy was applied by an Elmed Vibrolith Ortho ver 3.0 device (Elmed Medical Systems, Ankara, Turkey), 10–15 Hz, 1.5–2.5 bar energy density, 2000 pulses, once a week for three sessions using aquasonic gel as the transmitting medium. The patients were evaluated before therapy (BT) and after therapy (AT) and 1 month after treatment.
Outcome measures
Pain evaluation
Patient's pain levels were measured with visual analog scale (VAS) after resistive wrist extension and following 24 h of rest.
Pressure-pain threshold was measured by Commander Algometer (JTECH Medical, Utah, USA). To obtain pressure-pain threshold measurements, the patients were seated; their shoulders were situated at 30° of abduction; elbow at 90° of flexion; and forearm, wrist, and hand on the table.14, 15, 16 Two actions were performed by applying pressure to the most sensitive area of the lateral epicondyle with the 1 cm2 tip of an algometer followed by a 30-s pause.
Grip strength evaluation
Grip force was measured as maximum grip strength with a Baseline Hydraulic Hand Dynamometer (Fabrication Enterprises Inc, NY,USA). The grip strength was defined as the maximum grip force of using a hand dynamometer and measured with the patient seated, shoulder in 0° of abduction, neutral position, elbow in 90° of flexion followed by a 30-s pause between measurements. A mean value of three measurements was calculated.9
Functional status evaluation
The disability of the arm, shoulder, and hand score (DASH/quick-DASH) questionnaire measures upper extremity disability levels. There are 11 different questions to evaluate the daily living activities, four questions concerning the ability to work and four questions concerning the ability to engage in high performance activities such as sports or music. Each activity is graded with the Likert scale as 1 = no difficulty and 5 = incapable.17 The maximum total score for this evaluation is 100.
Patient-rated tennis elbow evaluation (PRTEE) is a specific questionnaire for evaluation of LE.18 The total score for this evaluation is the sum of the pain and function scores. The maximum total score for this evaluation is 100. Turkish language validation and reliability have been shown by Altan et al.19
Quality of life evaluation
Short Form-36 (SF-36) is a 36-item valid quality of life questionnaire with eight sub-scales including physical function, role-physical, role-emotional, social function, vitality, bodily pain, general health, and mental health. The Turkish language validation of SF-36 has been shown by Koçyiğit et al.20 The physical and mental component summary scores were used in this study.
Statistical analyses
Number Cruncher Statistical System (NCSS) 2007 and Power Analysis and Sample Size (PA SS) 2008 statistical software (Utah, USA) were used for statistical analysis. Compliance with the normal distribution of parameters was evaluated by the Shapiro–Wilk test. The mean and standard deviation values were presented for normal distributed parameters. The median (minimum–maximum) values were presented for non-normally distributed parameters. The comparison of age between the two groups was analyzed by the Student's t test. Fisher's exact test and Yates' continuity correction test were used for comparing the nominal variables. Statistical significance was established at p < 0.05.
Repeated measures of ANCOVA test was used analyze the time and group interaction. The sphericity assumption was tested using Mauchly's test and a Greenhouse–Geisser correction was used where applicable. The LSD test was used to account for time which contributes to inconsistency in the statistical results. Friedman's test was performed to compare repetitive measurements of non-normally distributed parameters, whereas the Wilcoxon Signed Rank test was used with Bonferroni correction to account for time which contributes to inconsistency (statistical significance was established at p ≤ 0.02). Friedman and ANCOVA tests' p values are presented in Table 3, Table 4, Table 5
Table 3.
Group comparisons of visual analog scale at rest and during resisted wrist extension scores.
| US (n = 24) | ESWT (n = 20) | p* | ||
|---|---|---|---|---|
| VAS Rest BT#," | Median (min–max) | 3 (0–6)#," | 1.5 (0–5)#," | 0.392 |
| VAS Rest ATβ | Median (min–max) | 0 (0–5) β | 0 (0–4) | |
| VAS Rest 1 month | Median (min–max) | 0 (0–3) | 0 (0–8) | |
|
p** |
<0.0001 |
<0.0001 |
||
| VAS RWE BT#," | Median (min–max) | 7 (3–10)#," | 7 (3–9) #," | 0.674 |
| VAS RWE ATβ | Median (min–max) | 4 (1–8)β | 5.5 (2–9)β | |
| VAS RWE 1 month |
Median (min–max) |
2 (0–5) |
3 (0–8) |
|
| p** | <0.0001 | <0.0001 | ||
p* between groups.
p** within groups.
BT: Before treatment; AT: After treatment; US: Therapeutic ultrasound; ESWT: Extracorporeal shock wave therapy; VAS: Visual analog scale (0–10 cm); RWE: Resisted wrist extension.
Statistically significant differences according to post hoc analysis: #: before treatment-after treatment, ": before treatment-1 month follow up, β: after treatment-1 month follow up.
Table 4.
Group comparisons of algometer and dynamometer values.
| US (n = 24) | ESWT (n = 20) | p* | ||
|---|---|---|---|---|
| Dynamometer (kg) BT#," | Median (min–max) | 18.45 (9.6–37) #," | 18.95 (9.3–36.6)" | 0.552 |
| Dynamometer (kg) ATβ | Median (min–max) | 21 (11–38.4)β | 21.65 (11.03–34.6) | |
| Dynamometer (kg) 1 month |
Median (min–max) |
22.5 (12.3–37.6) |
22 (11.3–36) |
|
| p** | 0.001 | 0.015 | ||
| Algometer (kg/cm2) BT#," | Mean ± sd | 7.69 ± 2.11#," | 7.75 ± 2.36#," | 0.029 |
| Algometer (kg/cm2) ATβ | Mean ± sd | 11.40 ± 2.65β | 12.34 ± 1.99β | |
| Algometer (kg/cm2) 1 month |
Mean ± sd |
14.10 ± 3.19 |
16.56 ± 2.79 |
|
| p** | <0.0001 | <0.0001 | ||
p*: between groups.
p**: within groups.
BT: Before treatment; AT: After treatment; US: Therapeutic ultrasound; ESWT: Extracorporeal shock wave therapy.
Statistically significant differences according to post hoc analysis: #: before treatment-after treatment, ": before treatment-1 month follow up, β: after treatment-1 month follow up.
Table 5.
Group comparisons of Patient rated tennis elbow evaluation and Quick disability of the arm, shoulder, and hand scores.
| US (n = 24) | ESWT (n = 20) | p* | ||
|---|---|---|---|---|
| PRTEE Total BT#," | Mean ± sd | 53.90 ± 13.71#," | 54.23 ± 9.51#," | 0.636 |
| PRTEE Total AT β," | Mean ± sd | 37.87 ± 14.79β | 42.95 ± 16.97β | |
| PRTEE Total 1 month |
Mean ± sd |
29.29 ± 9.0 |
32.08 ± 14.38 |
|
| p** | <0.0001 | <0.0001 | ||
| QDASH BT#," | Median (min–max) | 53.35 (15.0–93.1)#," | 56.8 (20.4–97.7)" | 0.070 |
| QDASH ATβ | Median (min–max) | 28.35 (13.6 ± 70.4) | 44.25 (20.4–97.7)β | |
| QDASH 1 month |
Median (min–max) |
27.20 (9.0–58.6) |
27.20 (4.5–70.4) |
|
| p** | <0.0001 | <0.0001 | ||
p*: between groups.
p**: within groups.
BT: Before treatment; AT: After treatment; US: Therapeutic ultrasound; ESWT: Extracorporeal shock wave therapy; PRTEE: Patient rated tennis elbow evaluation; QDASH: Quick Disability of the Arm Shoulder and Hand
Statistically significant differences according to post hoc analysis: #: before treatment-after treatment, ": before treatment-1 month follow up, β: after treatment-1 month follow up.
Results
The mean age of the patients was 27–64 years (45.00 ± 7.49). Patient population included 29.5% male (n = 13) and 70.5% female (n = 31). There was no statistically significant difference between groups in terms of age, gender, dominant hand, symptom duration and affected side (Table 1). There was no difference between groups in before treatment parameters (Table 2).
Table 1.
Demographic properties of the groups.
| US (n = 24) | ESWT (n = 20) | p | ||
|---|---|---|---|---|
| Age | Mean ± SD | 43.75 ± 4.52 | 46.04 ± 9.24 | 0.292 |
| Gender n (%) | ||||
| Male | 8 (33.3%) | 5 (25%) | 0.786 | |
| Female | 16 (66.7%) | 15 (75%) | ||
| Dominant hand n (%) | Left | 4 (16.7%) | 3 (15%) | 1.000 |
| Right | 20 (83.3%) | 17 (85%) | ||
| Symptom duration (m) | Mean ± SD | 7.9 ± 3.3 | 8.2 ± 3.6 | 0.818 |
| Affected side n (%) | Dominant hand | 12 (50%) | 13 (35%) | 0.244 |
| Nondominant hand | 12 (50%) | 7 (65%) | ||
ESWT: Extracorporeal shock wave therapy; m: month; US: Therapeutic ultrasound.
Table 2.
Comparison of before treatment values between groups.
| US (n = 24) | ESWT (n = 20) | p | ||
|---|---|---|---|---|
| VAS Rest | Median (min–max) | 3 (0–6) | 1.5 (0–5) | 0.143 |
| VAS RWE | Median (min–max) | 7 (3–10) | 7 (3–9) | 0.549 |
| Dynamometer | Median (min–max) | 18.45 (9.6–37) | 18.95 (9.3–36.6) | 0.898 |
| Algometer | Mean ± SD | 7.69 ± 2.11 | 7.75 ± 2.36 | 0.930 |
| PRTEE total | Mean ± SD | 53.90 ± 13.71 | 54.23 ± 9.51 | 0.928 |
| QDASH | Mean ± SD | 53.35 (15.0–93.1) | 56.8 (20.4–97.7) | 0.688 |
US: Therapeutic ultrasound; ESWT: Extracorporeal shock wave therapy; VAS: Visual analog scale (0–10 cm); RWE: Resisted wrist extension; PRTEE: Patient rated tennis elbow evaluation; QDASH: Quick Disability of the Arm Shoulder and Hand.
Pain evaluation
Rest and resisted wrist extension (RWE) VAS values did not differ between the groups (Table 3). Algometer measurements differ significantly between the groups in favor of ESWT group (p = 0.029) (Table 4).
VAS-Rest and VAS-RWE values and algometer measurements significantly improved in time within both groups (Table 3, Table 4).
Grip strength evaluation
Grip strength measurements did not differ between the groups. Grip dynamometer values significantly improved in time within both groups (Table 4).
Functional status evaluation
The QDASH and PRTEE-total scores did not differ between the groups. The PRTEE-total and QDASH scores significantly improved in time within both groups (Table 5).
Statistically significant differences within time in groups were further analyzed with posthoc tests. Post hoc analysis were expressed in Table 3, Table 4, Table 5 as following symbols: #: the significant difference between before treatment and after treatment values, ": the significant difference between before treatment and 1 month follow up results, β: the significant difference between after treatment and1 month follow up results.
Quality of life evaluation
SF-36 physical component scores of both groups significantly increased at 1 month follow up (p < 0.05). SF-36 mental component scores did not reach statistically significant values at 1 month follow up in both groups (p > 0.05). There was no significant difference in terms of SF-36 physical component scores and SF-36 mental component scores at 1 month follow up between groups (Table 6).
Table 6.
Group comparisons of Short form-36 subscores.
| SF-36 subscores | US (n = 24) | ESWT (n = 20) | p* | |
|---|---|---|---|---|
| PCSS BT | Mean ± sd | 34.76 ± 7.48 | 34.31 ± 6.18 | 0.925 |
| PCSS 1 month |
Mean ± sd |
43.93 ± 5.51 |
42.19 ± 9.40 |
0.471 |
|
p** |
BT-1 month |
0.001 |
0.005 |
|
| MCSS BT | Mean ± sd | 45.37 ± 8.69 | 44.40 ± 9.21 | 0.409 |
| MCSS 1 month |
Mean ± sd |
46.23 ± 6.87 |
45.59 ± 8.23 |
0.759 |
| p** | BT-1 month | 0.668 | 0.526 | |
p*: between groups.
p**: within groups.
BT: Before treatment; AT: After treatment; US: Therapeutic ultrasound; ESWT: Extracorporeal shock wave therapy; SF-36: Short form-36; PCSS: Physical component summary score; MCSS: Mental component summary score.
Discussion
Both ESWT and therapeutic US have been found to be effective treatments for LE in this study, which evaluated patient pain levels, grip strength, functional status, and quality of life. VAS scores decreased and pressure pain threshold and grip strength increased after treatment and 1 month follow up in both groups. Improvement in terms of ADLs PRTEE, QDASH, and SF-36 scores in both groups were observed. However, there was no difference between groups in effectiveness.
Rompe et al21 applied ESWT with 0.08 mJ/mm2 low energy intensity, 1000 pulse in 3 sessions to evaluate analgesic effect of ESWT in chronic LE patients in their placebo-controlled study. They found no difference between groups after treatment. Improvements occurred at 3, 6, and 24 weeks after treatment.
In our study, significant improvements were identified in terms of pain parameters in the ESWT group after treatment and after 1 month of follow up. We applied ESWT with 2000 pulses whereas Rompe et al used 1000 pulses. The earlier improvement regarding pain levels in our study compared with Rompe et al may be due to the application of higher pulses. Rompe et al conducted another placebo-controlled study to observe different pulse counts and doses.22 They applied 0.09 mJ/mm2 and 2000 pulse in a week in 3 total sessions. They showed superiority of ESWT group in terms of pain, grip strength and function levels after 3 and 12 months of follow up. Even though similar pulse count and intensity levels of ESWT was applied in our study, comparing our results to those of Rompe et al was not possible since the schedule of evaluations were different. According to our study, the effectiveness of ESWT started right after treatment. Additional studies are required to define the most effective therapeutic protocol.
Dosage and pulse counts vary in the literature. For example, Furia et al23 applied 1085 mJ/mm2 dose of high energy ESWT. Spacca et al24 compared ESWT with placebo in LE. They applied 1.2 Bar, 4 Hz, 500 pulse and 1 Bar, 10 Hz, 1500 pulses, total 2000 pulses in 4 sessions. In our study, ESWT was applied with 10–15 Hz, 1.5–25 Bar energy, 2000 pulses once a week, in 3 total sessions. Furia et al23 reported improvements regarding pain level and quality of life evaluations after 4 and 12 weeks. Spacca et al24 found improvements regarding pain level and grip strength superior to placebo. However, the limitation of those studies includes a lack of control groups. Melikyan et al25 did not find ESWT superior to placebo in terms of pain, functional level, and dynamometric measurements when applied with a dose of 1000 mJ/mm2.
Our study found improvements in terms of pain, grip strength, and functional status, which were similar to those of recent literature. The ESWT group showed significant improvement at AT and 1-month follow up. Different from recent studies, the efficacy of ESWT in LE was compared to therapeutic US, which is well accepted and commonly used in LE treatment in physical medicine and rehabilitation clinics. To the best of our knowledge, there are limited studies comparing ESWT to other therapeutic methods.26, 27, 28 Lee et al26 compared ESWT and steroid injection in lateral and medial epicondylosis patients. Pain levels in both groups decreased after 2 weeks but improvement was better in the injection group. However, the ESWT group showed better improvements after 8 weeks. ESWT was more effective as a long-term treatment. Crowther et al27 compared steroid injection with ESWT in LE and reported improvement in steroid injection group after 6 week and 3 months.
Therapeutic US has been commonly used for LE treatment and other musculoskeletal system diseases. There are studies reporting effectiveness of therapeutic US in LE.29, 30 However, there is only one study that compared therapeutic US to ESWT.28 In that study, the first group underwent therapeutic US, hotpacks, and friction massage, a second group underwent steroid injection, and a third group underwent ESWT. Therapeutic US was applied for 5 min with 1 w/cm2 dose per session for 10 sessions. ESWT was applied with 1.4 Bar, 4 Hz and 500 pulses every other day for 10 sessions. Patients showed significant improvement in VAS and grip strength after treatment and after 1, 3 and 6. months. The study of Gündüz et al28 and study of Lee et al26 showed the effectiveness of ESWT in long term. In our study, both ESWT and therapeutic US have been found to be effective in terms of pain level and grip strength. The ESWT group did not show significant improvement in grip strength until 1 month after follow up. Increase in algometer measurements were significantly higher in ESWT group compared with US group at 1 month after follow up. We have no knowledge on long-term comparisons of the two treatment methods. Limitations include lack of longer follow up measurements such as 8 or 12 weeks. Our study provides important findings such as immediate effect of ESWT after therapy lasting at least 1 month.
Conclusion
ESWT is just effective as US for the treatment of LE in terms of improving pain level, grip strength, functional status, and quality of life but is not superior to US. ESWT should be an alternative treatment modality due to shorter sessions and application time, just for patients who do not have enough time and patients who have contraendications for ultrasound. Additional studies are required to assess long term effectiveness of ESWT and comparison of ESWT with other physical treatment methods.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Krischek O., Hopf C., Nafe B., Rompe J.D. Shock-wave therapy for tennis and golfer's elbow-1 year follow-up. Arch Orthop Trauma Surg. 1999;119(1-2):62–66. doi: 10.1007/s004020050356. [DOI] [PubMed] [Google Scholar]
- 2.Hong Q.N., Durand M.J., Loisel P. Treatment of lateral epicondylitis: where is the evidence? Joint Bone Spine. 2004;71(5):369–373. doi: 10.1016/j.jbspin.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Cyriax J.H. The pathology and treatment of tennis elbow. J Bone Joint Surg. 1936;18(4):921–940. [Google Scholar]
- 4.Trudel D., Duley J., Zastrow I., Kerr E.W., Davidson R., MacDermid J.C. Rehabilitation for patients with lateral epicondylitis-A systematic review. J Hand Ther. 2004;17(2):243–266. doi: 10.1197/j.jht.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Smedt T.D., Jong A.D., Leemput W.V., Lieven D., Glabbeek F.V. Lateral epicondylitis in tennis: update on aetiology, biomechanics and treatment-Review. Br J Sports Med. 2007;41(11):816–819. doi: 10.1136/bjsm.2007.036723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fornalski S., Gupta R., Lee T.Q. Anatomy and biomechanics of the elbow joint. Tech Hand Up Extrem Surg. 2003;7(4):168–178. doi: 10.1097/00130911-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Celli Andrea. Anatomy and biomechanics of the elbow. In: Celli Andrea, Celli Luigi, Morrey Bernard F., editors. Treatment of Elbow Lesions New Aspects in Diagnosis and Surgical Techniques. Springer; 2008. pp. 1–11. [Google Scholar]
- 8.Hoppenfeld S. Prentice – Hall Inc; New York: 1976. Physical Examination of the Spine and Extremities; pp. 35–58. [Google Scholar]
- 9.Wuori J.L., Overend T.J., Kramer J.F., MacDermid J. Strength and pain measures associated with lateral epicondylitis bracing. Arch Phys Med Rehabil. 1998;79(7):832–837. doi: 10.1016/s0003-9993(98)90366-5. [DOI] [PubMed] [Google Scholar]
- 10.Raman J., MacDermid J.C., Grewal R. Effectiveness of different methods of resistance exercises in lateral epicondylosis-A systematic review. J Hand Ther. 2012;25(1):5–26. doi: 10.1016/j.jht.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Sems A., Dimeff R., Ianotti J.P. Extracorporeal shock wave therapy in the treatment of chronic tendinopathies. J Am Acad Orthop Surg. 2006;14(4):195–204. doi: 10.5435/00124635-200604000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Wang C.J. Extracorporeal Shock wave therapy in musculoskeletal disorders. J Orthop Surg Res. 2012;7(11):1–8. doi: 10.1186/1749-799X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hinsche A., Stanley D. The clinical examination of the elbow. In: Celli Andrea, Celli Luigi, Morrey Bernard F., editors. Treatment of Elbow Lesions New Aspects in Diagnosis and Surgical Techniques. Springer; 2008. pp. 13–20. [Google Scholar]
- 14.Melzack R., Katz J. Measurement of pain. In: Turk C.D., Melzack R., editors. Handbook of Pain Assesment. 2nd ed. 2001. pp. 35–53. [Google Scholar]
- 15.Kosek E., Ekholm J., Hansson P. Pressure pain thresholds in different tissues in one body region: the influence of skin sensitivity in pressure algometry. Scand J Rehabil Med. 1999;31(2):89–93. doi: 10.1080/003655099444597. [DOI] [PubMed] [Google Scholar]
- 16.Pienimaki T., Tarvainen T., Siira P., Malmivaara A., Vanharanta H. Associations between pain, grip strength and manual tests in the treatment evaluation of chronic tennis elbow. The Clin J Pain. 2002;18(3):164–170. doi: 10.1097/00002508-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Imaeda T., Toh S., Wada T. Validation of the Japanese Society for surgery of the hand version of the quick disability of the arm, shoulder and hand (quick DASH-JSSH) questionnaire. J Orthop Sci. 2006;11(3):248–253. doi: 10.1007/s00776-006-1013-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Overend T.J., Wuori J.L., Kramer J.F., Mac Dermid J.C. Reliability of a patient forearm evaluation questionnare for patients with lateral epicondylitis. J Hand Ther. 1999;12(1):31–37. doi: 10.1016/s0894-1130(99)80031-3. [DOI] [PubMed] [Google Scholar]
- 19.Altan L., Ercan İ., Konur S. Reliability and validity of Turkish version of the patient rated tennis elbow evaluation. Rheumatol Int. 2009;30(8):1049–1054. doi: 10.1007/s00296-009-1101-6. [DOI] [PubMed] [Google Scholar]
- 20.Koçyiğit H., Aydemir Ö., Fisek G., Ölmez N., Memiş A. Kısa Form-36 (KF-36)’nın türkçe versiyonunun güvenilirliği ve geçerliliği. İlaç ve Tedavi Dergisi. 1999;12(2):102–106. [Google Scholar]
- 21.Rompe J.D., Hopf C., Kullmer K., Heine J., Burger R. Analgesic effect of extracorporeal shock wave therapy on chronic tennis elbow. J Bone Joint Surg (British) 1996;78(2):233–237. [PubMed] [Google Scholar]
- 22.Rompe J.D., Decking J., Schoeliner C., Theis C. Repetitive low energy shock wave treatment for chronic lateral epicondylitis in tennis players. Am J Sports Med. 2004;32(3):734–743. doi: 10.1177/0363546503261697. [DOI] [PubMed] [Google Scholar]
- 23.Furia J.P. Safety and efficacy of extracorporeal shock wave therapy for chronic lateral epicondylitis. The Am J Orthopedics. 2005;34(1):13–19. [PubMed] [Google Scholar]
- 24.Spacca G., Necozione S., Cacchio A. Radial shock wave therapy for lateral epicondylitis: a prospective randomised controlled single-blind study. Eur Med Phys. 2005;41(1):17–25. [PubMed] [Google Scholar]
- 25.Melikyan E.Y., Shanin E., Miles J., Bainbridge L.C. Extracorporeal shock wave treatment for tennis elbow. J Bone Joint Surg (British) 2003;85(6):852–855. [PubMed] [Google Scholar]
- 26.Lee S.S., Kang S., Park N.K. Effectiveness of initial extracorporeal shock wave therapy on the newly diagnosed lateral or medial epicondylitis. Ann Rehabil Med. 2012;36(5):681–687. doi: 10.5535/arm.2012.36.5.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Crowther M.A., Bannister G.C., Huma H., Rooker G.D. A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. J Bone Joint Surg Br. 2002;84(5):678–679. doi: 10.1302/0301-620x.84b5.12741. [DOI] [PubMed] [Google Scholar]
- 28.Gündüz R., Malas F.Ü., Borman P., Kocaoğlu S., Özçakar L. Physical therapy, corticosteroid injection and extracorporeal shock wave treatment in lateral epicondylitis, clinical and ultrasonographical comparison. Clin Rheumatol. 2012;31(5):807–812. doi: 10.1007/s10067-012-1939-y. [DOI] [PubMed] [Google Scholar]
- 29.Binder A., Hodge G., Greenwood A.M., Hazleman B.L., Page Thomas D.P. Is therapeutic ultrasound effective in treating soft tissue lesions? Br Med J. 1985;290(6467):512–514. doi: 10.1136/bmj.290.6467.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akın C., Öken Ö., Köseoğlu B.F. Short-term effectiveness of ultrasound treatment in patients with lateral epicondylitis: randomized, single-blind, placebo-controlled, prospective study. Arch Rheumatol. 2010;25(2):050–055. [Google Scholar]