Abstract
Introduction
Historically, patients undergoing an elective hip, knee or shoulder arthroplasty regularly required blood transfusions. Improved surgical techniques and perioperative optimisation have significantly decreased the requirement for blood transfusions. Currently, our patients have two group and save samples taken: one six weeks preoperatively and one on admission. This study aims to determine whether a second group and save is required prior to primary elective hip, knee or shoulder arthroplasty.
Methods
All cases of elective arthroplasty from a single centre were retrospectively analysed over a 16-month period. Each case was reviewed to determine those who had a group and save at preassessment, group and save at the time of the operation and the timing and number of blood products transfused.
Results
A total of 711 elective arthroplasty procedures were completed with 48 patients requiring a transfusion during their admission. 9.9% of hip arthroplasty patients, 3.8% of knee arthroplasty patients and 4.9% of shoulder arthroplasty patients required a transfusion. The majority of the transfusions occurred at least 24 hours postoperatively with 0.84% of patients requiring an intraoperative transfusion.
Discussion
The vast majority of transfusions were delivered more than 24 hours following the procedure, demonstrating that routinely cross-matched blood products are superfluous to requirements. It is our suggestion that a formal group and save be completed only if the need for a blood transfusion is formally established, leading to a significant cost saving, a reduction in clinical work load and patients having to undergo fewer procedures.
Keywords: Orthopaedics, Haematology, Arthroplasty, Elective surgery
Introduction
Elective arthroplasties make up the majority of elective orthopaedic practice. The UK National Joint Registry reveals that the number of total shoulder replacements, total hip replacements and total knee replacements continued to increase year on year.1 Historically, these procedures had a significant risk of patients requiring blood transfusions. In 2004, transfusion rates of 46% were reported using standard practice at the time.2 Transfusion of blood products puts patient at risk of complications including blood-borne infections, transfusion reactions and transfusion-related lung injury.
Numerous advances have reduced the requirement for transfusion in elective arthroplasty including: preoperative patient optimisation, cell salvage techniques, the use of tranexamic acid and enhanced recovery programmes after surgery. Together with these practices, the accepted threshold at which a transfusion should be given has lowered significantly. The current UK guidance from the British Committee for Standards in Haematology states that transfusion should be considered in those with a haemoglobin level less than 70 gl-1.3
At our institution, patients undergo a preoperative assessment six weeks prior to surgery. As part of this assessment, a primary group and save sample is taken to establish the patients’ blood group and to identify any atypical red cell antibodies. The presence of these antibodies may delay the availability of blood products for these patients, as they are unlikely to be available locally and advanced planning can occur. On the day of surgery, a second group and save sample is taken in anticipation of an emergency requirement for blood transfusion. This study aims to determine whether a group and save on the day of admission is required prior to elective shoulder, hip or knee arthroplasty and to quantify our transfusion rates for these procedures.
Methods
All cases of elective arthroplasty were retrospectively analysed from 01 November 2014 to 31 November 2015 and again between 1 August 2016 to 31 October 2016. Unicompartmental, resurfacing and revision arthroplasty were included in our study. Emergency arthroplasty procedures were excluded. Cases were identified via the clinical coding department theatre records and cross-referenced with the National Joint Registry and blood bank electronic records. Each case note was reviewed to determine those who had a group and save at preassessment and those who had a group and save at the time of the operation and, if applicable, the timing and number of blood products transfused.
Results
During the time periods described, a total of 711 elective arthroplasties were undertaken. The breakdown of each elective arthroplasty procedure can be seen in Table 1. The majority (83.5%) of patients underwent a preoperative group and save and day of the operation group and save, as per protocol. The remaining 16.5% were missing one or both of these prior to the operation (Table 2).
Table 1.
Elective arthroplasty procedures, 1 November 2014 to 31 November 2015 and 1 August 2016 to 31 October 2016.
| Type of procedure | Replacement procedures (n) | ||
| Primary | Revision | Other | |
| Hip | |||
| Primary total replacement | 282 | 28 | |
| Knee | 279 | 23 | 44a |
| Shoulder | 47 | 6 | 2b |
a Unicondylar replacement
b Primary hemi-arthroplasty
Table 2.
Preoperative and day of the operation group and save samples taken.
| Group and save | Hip | Knee | Shoulder | Average (%) | |||||
| Primary total | Revision | Primary total | Revision | Unicondylar | Primary total | Revision | Primary hemi-arthroplasty | ||
| Routine preoperative and valid at operation | 238 | 27 | 235 | 22 | 28 | 37 | 5 | 2 | 83.5 |
| Routine preoperative, no valid at operation | 9 | 0 | 35 | 1 | 12 | 9 | 1 | 0 | 9.4 |
| No routine preoperative and valid at operation | 22 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 3.2 |
| No routine preoperative and no valid at operation | 12 | 0 | 12 | 1 | 1 | 1 | 0 | 0 | 4.7 |
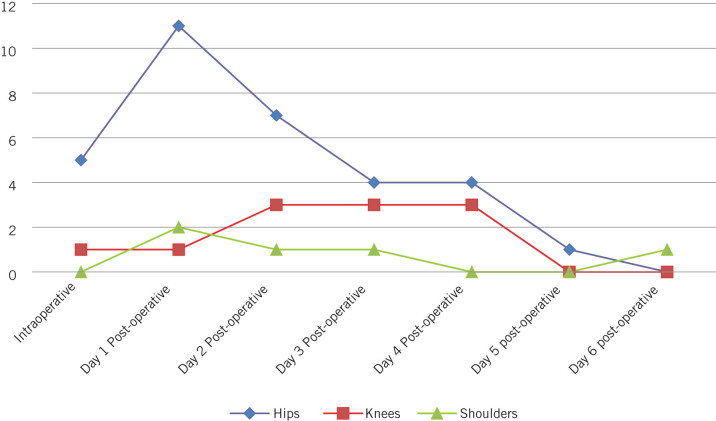
In total, 48 patients required a transfusion during their hospital stay, 9.9% of patients who underwent a hip arthroplasty, 3.8% of knee arthroplasty patients and 4.95% of shoulder arthroplasty patients (Table 3). The indications for transfusion are documented in Figure 3. The majority of the transfusions occurred postoperatively with the requirement of intraoperative transfusion in 0.84% of cases (Fig 1).
Table 3.
Indications for transfusion.
| Indicationfor transfusion | Hip | Knee | Shoulder | |||||
| Primary total | Revision | Primary total | Revision | Unicondylar | Primary total | Revision | Primary hemi-arthroplasty | |
| Intraoperative bleeding | 7 | 2 | 0 | 1 | 0 | 0 | 0 | 0 |
| Postoperative anaemia | 16 | 6 | 5 | 4 | 0 | 4 | 0 | 0 |
| Postoperative haematoma evacuated | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Anaemia on restarting anticoagulation | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Figure 1.
Numbers and timing of blood transfusion.
Discussion
Our study shows comparable rates of blood transfusion for elective arthroplasty patients to other reported studies in the literature.4
The majority of perioperative transfusions were carried out on a non-emergency basis, following review of routine postoperative bloods 24 hours following surgery. It was therefore possible to prescribe and deliver blood products in a scheduled manner. As a result of these findings, we suggest that a formal group and save need only be completed if the need for a transfusion has been determined. Owing to the rarity with which intraoperative transfusion is required, we believe that a group and save sample could be taken if it is required during the operation and, if an emergency, then O negative blood should be used.
With the implementation of this strategy, we would be able to reduce the number of elective group and save samples by up to 50%. This will lead to a significant saving. The cost of each test at our trust is currently £1.65, equating to a reduction in costs of £702.14 per annum. Another benefit is that our patients will not have to undergo a unnecessary and unpleasant test.
Conclusion
The rates of intraoperative blood transfusion for elective arthroplasties are low. The majority of postoperative transfusions are given non-urgently, which means that patients can safely undergo a second group and save sample at this time. Abandoning the practice of completing on-the-day group and save samples appears to be clinically indicated and would bring significant financial savings without putting patients at risk.
References
- 1.National Joint Registry UK National Joint Registry for England and Wales: 13th Annual Report. Hemel Hempstead: National Joint Registry; 2016. [Google Scholar]
- 2.Jones HW, Savage L, White C et al. Postoperative autologous blood salvage drains: are they useful in primary uncemented hip and knee arthroplasty? A prospective study of 186 cases. Acta Orthop Belg 2004; : 466–473. [PubMed] [Google Scholar]
- 3.Retter A, Wyncoll D, Pearse R et al. Guidelines on the management of anaemia and red cell transfusion in adult critically ill patients. Br J Haematol 2013; (4): 445–464. [DOI] [PubMed] [Google Scholar]
- 4.Mason BA, Shah J, Deglurkar M. Blood transfusion in hip and knee arthroplasties: the end of the pre-operative group and save? Eur J Orthop Surg Traumatol 2015; : 871–875. [DOI] [PubMed] [Google Scholar]