Abstract
Introduction
Patients with large ptotic breasts undergoing immediate implant-based reconstruction often require skin-reducing mastectomy to optimise the aesthetic outcome. However, healing complications, especially at the resulting inverted T-junction, leading to wound dehiscence, infection, skin necrosis, implant exposure and failed reconstruction have been widely reported. We present an innovative approach for immediate implant-based reconstruction combining porcine- or bovine-derived acellular dermal matrices with a de-epithelialised dermal sling to protect and support the implant, while improving clinical outcomes in this challenging group of patients.
Materials and methods
Demographic, tumour and surgical data were reviewed for patients undergoing Wise pattern (T-scar) skin-reducing mastectomies with immediate implant-based reconstruction combining porcine- or bovine-derived acellular dermal matrices with a de-epithelialised dermal sling.
Results
This technique was successfully employed to reconstruct five large pendulous breasts in four breast cancer patients with a median age of 50.5 years (range 34–61 years) who were not suitable for, or had declined, flap-based reconstruction. The acellular dermal matrices used were SurgiMend®, StratticeTM and Braxon® and the expandable implants were placed in the sub-pectoral (n = 3) and pre-pectoral (n = 1) planes. The technical steps and clinical outcomes are presented. One patient experienced T-junction breakdown overlying the de-epithelialised dermis without implant loss.
Conclusion
The combination of an acellular dermal matrix and a dermal sling provides a double-layer ‘water-proofing’ and support for the implants inferiorly, avoiding T-junction breakdown complications, since any dehiscence is on to well-vascularised dermis. Furthermore, the acellular dermal matrix stabilises the implant in the large mastectomy cavity (pocket control). This approach provides a viable option which facilitates mastectomy and immediate implant reconstruction in large-breasted patients.
Keywords: Acellular dermal matrix, ADM, Immediate breast reconstruction, Dermal sling, De-epithelialised dermal flap, Skin-reducing mastectomy, Wise mammoplasty pattern, T-junction complications, Conservative mastectomy, Pre-pectoral breast reconstruction, T-scar mastectomy, Inferior pedicle dermal flap
Introduction
Mastectomy is commonly performed therapeutically or prophylactically to reduce the risk of malignant breast disease.1 ‘Conservative mastectomies’, including skin-sparing mastectomy2 and nipple-sparing mastectomy,3 have improved outcomes of post-mastectomy reconstruction.4 These techniques involve the resection of breast parenchyma, maintaining the overlying subcutaneous tissue and skin, thus facilitating immediate prosthetic or autologous reconstruction. However, in patients with large ptotic breasts, the preservation of the entire skin envelope results in long and often unreliable mastectomy skin flaps and poor aesthetic outcomes, especially in implant-based reconstructions. Nava and colleagues adapted the Wise mammoplasty pattern, describing a novel ‘skin-reduction’ approach with a de-epithelialised dermal sling (or inferior pedicle dermal flap), followed by a single-stage anatomical implant insertion.5 T-junction healing complications, however, with subsequent implant exposure have been reported in up to 27% of cases.5–7
In recent years, many implant-based breast reconstructions have incorporated the use of acellular dermal matrices since they provide a number of clinical and aesthetic advantages.8–12 Acellular dermal matrices extend the sub-pectoral pocket inferolaterally enabling the accommodation of larger prostheses, broadening the suitable patient population for implant-based reconstructions. We present an innovative approach for immediate implant-only reconstruction in large-breasted patients, combining the nonhuman acellular dermal matrices SurgiMend® (TEI Biosciences Inc.), Strattice™ (Acelity) or Braxon® (Decomed) acellular dermal matrices with a de-epithelialised dermal sling to improve clinical outcomes and reduce local complication rates.
Materials and methods
Four breast cancer patients with large heavy pendulous breasts underwent immediate implant-only reconstruction as they were unsuitable for or declined flap-based techniques. The patients’ large and ptotic breasts necessitated skin-reducing mastectomies to enable implant reconstruction. The mastectomies were accomplished using the Wise pattern incorporating supporting de-epithelialised dermal flaps. To optimise the results, we employed a variety of acellular dermal matrices (porcine Strattice, bovine SurgiMend and porcine Braxon) in combination with the dermal slings. This series presents the technical steps and clinical outcomes of these four candidates (Figs 1 and 2, Tables 1 and 2). All patients were followed up for a minimum of 12 months.
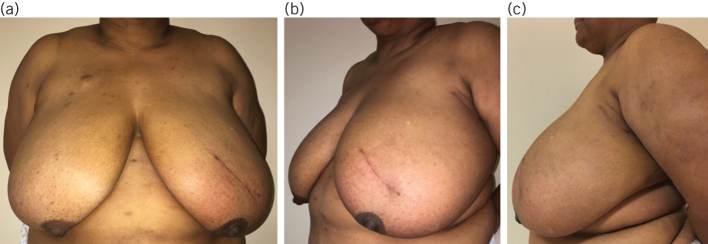
Figure 1.
Preoperative photographs of 53-year-old patient (case 4) with gigantomastia and lumpectomy scar on left breast; (a) anteroposterior view; (b) left oblique view; (c) left lateral view. She underwent T-scar skin-reducing mastectomy and immediate pre-pectoral expandable-implant reconstruction combined with a dermal sling and total implant coverage with Braxon® porcine acellular dermal matrix four weeks after completion of neoadjuvant chemotherapy.
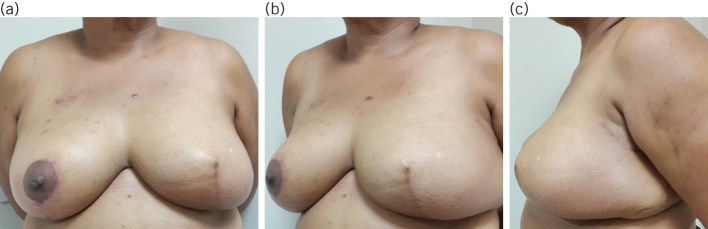
Figure 2.
Three-month postoperative photographs of 53-year-old patient (case 4) showing excellent symmetry of breasts and the inverted T-junction on the left breast; (a) anteroposterior view; (b) left oblique view; (c) left lateral view.
Table 1.
Preoperative case summaries of patients undergoing skin-reducing mastectomy and immediate breast reconstruction combining the use of an acellular dermal matrix with a de-epithelialised dermal flap.
| Case | Age (years) | Smoking status | Comorbidities | BMI | Bra cup size | Neoadjvuant chemotherapy | Radiotherapy planned | Indication for mastectomy |
| 1 | 48 | Former smoker | None | 30.8 | 34D | Yes | Yes | Right: multifocal 17 mm G2 ILC and G1 IDCLeft: 7 mm G1 IDC |
| 2 | 34 | Never smoked | None | 31.9 | 38DD | Yes | Yes | Left: 140mm ILC G2 |
| 3 | 61 | Former smoker | Hypertension | 35.4 | 36D | No | Yes | Right: multifocal 13mm G2 IDC, 11mm G1 IDC, 9mm G1 papillaryLeft: multifocal 28mm G3 IDC and 5mm G3 IDC |
| 4 | 53 | Never smoked | None | 51 | 46GG | Yes | Yes | Left: multifocal 17mm G3 NST and 6mm G3 NST and 68mm DCIS (high grade) |
BMI, body mass index; DCIS, ductal carcinoma in situ; G, grade; IDC, invasive ductal carcinoma; ILC, invasive lobular carcinoma; NST, no special type.
Table 2.
Peri- and postoperative case summaries of patients undergoing skin-reducing mastectomy and immediate breast reconstruction combining the use of an acellular dermal matrix with a de-epithelialised dermal flap.
| Case | Procedure | Axillary surgery | Mastectomy weight (g) | Anatomical expandable implant details | Hospital stay (days) | Adjuvant therapy | Postoperative complications | ||
| Right breast | Left breast | Early (< 30 days) | Late (> 30 days) | ||||||
| 1 | Therapeutic SRM and IBR with expander implant + Strattice™ ADM | Left therapeutic mammoplasty and sub-pectoral expander implant | Right ANC; left SLNB | Right – 398 | Natrelle (McGhan) Style 150 SH; gel volume 170 ml; final saline fill volumes: right 485 ml; left 310 ml; 4 postoperative inflations | 4 | Radiotherapy | None | Bilateral capsular contracture post-radiotherapy; necessitating capsulectomies and expander-to-implant exchanges |
| 2 | Risk-reducing SRM and IBR with expander implant | Therapeutic SRM and IBR with expandable implant + SurgiMend ADM | Left ANC | Right – 681Left – 671 | Natrelle (McGhan) Style 150 short height; gel volume 170 ml; final saline fill volumes: right 370 ml; left 370 ml; 3 postoperative inflations | 4 | Radiotherapy, hormones | None | Cellulitis treated with antibiotics |
| 3 | Therapeutic SRM and IBR with expandable implant and SurgiMend® ADM | Therapeutic SRM and IBR with expandable implant + SurgiMend ADM | Bilateral SLNB | Right – 760Left – 726 | Mentor Becker-35 expanders; gel volume 160 ml; final saline fill volumes: right 170 ml; left 170 ml; 1 postoperative inflation | 4 | Radiotherapy, chemotherapy, hormones | Right: skin necrosis and T-junction breakdown required skin graft | None |
| 4 | Wise-pattern breast reduction | Therapeutic SRM and IBR with expandable implant + Braxon® ADM | None | Left – 2025 | Mentor Becker-35 expander; gel volume 195 ml; final saline fill volume: left 370 ml saline; no postoperative inflations | 4 | None | None | None |
ADM, acellular dermal matrix; ANC, axillary node clearance; DIEP, deep inferior epigastric artery perforator; IBR, immediate breast reconstruction; SLNB, sentinel lymph node biopsy; SRM, skin-reducing mastectomy.
Surgical technique
The procedures were performed jointly by oncological and reconstructive surgeons. The oncological surgeons initially undertook the Wise-pattern skin-reducing mastectomy with de-epithelialisation of the dermal sling and any necessary axillary surgery. The rest of the procedure was then performed jointly. For the first three patients, the sub-pectoral pocket was dissected raising the inferomedial border of the pectoralis major muscle and releasing it medially to the eight o’clock position on the left and four o’clock on the right. The sub-pectoral pocket was then irrigated with 400 ml of 5% aqueous povidone iodine (betadine). The acellular dermal matrix was soaked in normal saline for 5–15 minutes to rehydrate it and/or remove the preservative and then sutured to the inframammary fold and lateral boundary of the breast with interrupted 2/0 polydioxanone (PDS) sutures. An expandable implant (Natrelle style 150 or Mentor Becker-35) was rinsed in 10% povidone iodine and then inserted into the acellular dermal matrix muscle pocket before its closure to the pectoralis major was completed using a running 2/0 PDS suture (Fig 3). The injection port was positioned in a subcutaneous tunnel inferolaterally and the fill tube secured with 3/0 vicryl at the inframammary fold level. The inferior dermal sling was then secured to the pectoralis major with 2/0 PDS thus covering the acellular dermal matrix. Deep dermal and subcuticular closure was subsequently achieved with 3/0 vicryl and 3/0 monocryl sutures respectively. Two suction drains (Blake’s size 15 and 10) were inserted in the peri-implant and subcutaneous pockets respectively and secured with 2/0 nylon. They were removed on day 3 postoperatively or when the drain output was less than 30 ml in 24 hours. In the single Braxon patient the expander–acellular dermal matrix complex was inserted pre-pectorally; the rest of the procedure was identical.
Figure 3.
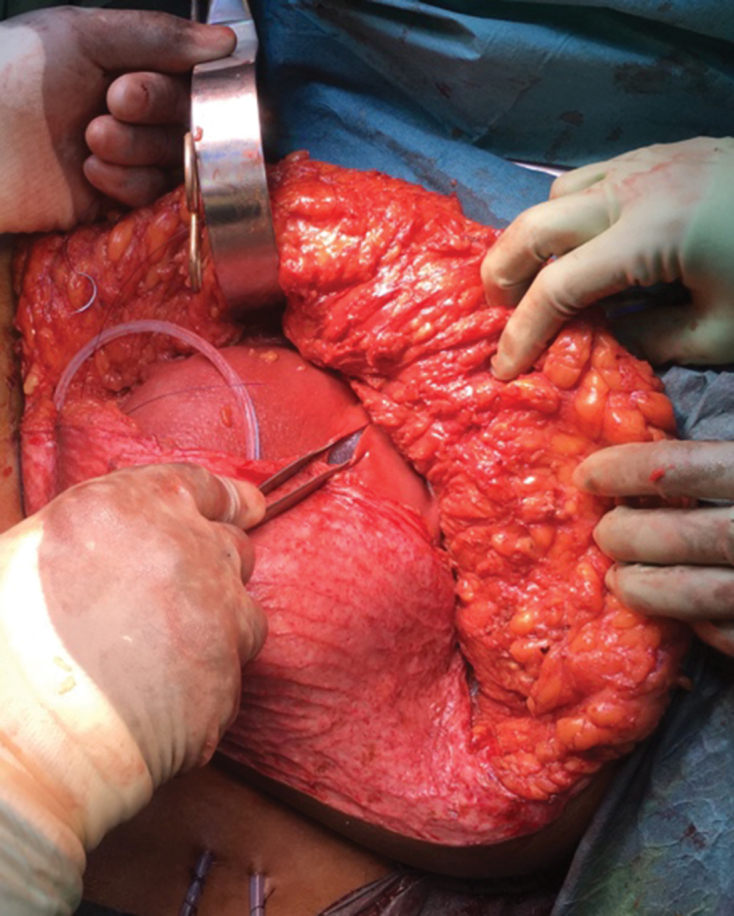
Intraoperative photograph of a de-epithelialised dermal sling and acellular dermal matrix combination.
Discussion
Since its first description in 1991, there have been a number of modifications to the Wise-pattern mastectomy and reconstruction technique employed in patients with large ptotic breasts.2,13–16 Notable among these was the application of the LeJour vertical mammoplasty pattern for mastectomy and reconstruction.13–16 Despite these innovations, T-junction breakdown is still a major limitation, endangering the underlying implant.5–7 The de-epithelialised dermal flap purportedly obviates wound complications in both the inverted-T (Wise-pattern) technique5,17–22 and the vertical-pattern skin-reducing mastectomies.23
This series demonstrates that acellular dermal matrices can be successfully combined with a de-epithelialised dermal sling to buttress the T-junction, protecting the underlying implant and improving the reconstruction reliability. Similarly, Derderian et al.24 used human acellular dermal matrices, Alloderm® (LifeCell), with an inferior dermal subcutaneous pedicle in a series of 20 Wise-pattern breast reconstructions, 25% of which experienced T-junction breakdown.24 Ours is the first study describing the combination of non-human acellular dermal matrices with inferior de-epithelialised slings for Wise-pattern mastectomy and immediate breast reconstruction.
In the present series, risk of wound breakdown, infection and implant loss was high on account of the patients’ smoking status, obesity, simultaneous axillary surgery or prior neoadjuvant chemotherapy.24 Despite this, only one of the reported patients experienced wound dehiscence and skin-flap necrosis adjacent to the T-junction. However, this breakdown did not lead to implant removal, as the implant was not exposed due to the overlying dermal sling and acellular dermal matrix combination. Complete wound healing was achieved after operative debridement and skin grafting and the patient went on to receive adjuvant radiotherapy without any delay.
This technique has recently been used in breast reconstruction involving a pre-pectoral implant, using porcine-derived acellular dermal matrices.25 The authors reported only three cases of skin ischaemia out of 33 breast operations but no infection or implant removal. Acellular dermal matrices can support the weight of an implant, theoretically reducing the tension in the dermal flaps and thus the incidence of major wound healing complications.24 Our pre-pectoral patient, contrastingly, received a Braxon total-coverage acellular dermal matrix.
A number of advantages of acellular dermal matrices with dermal sling justify the extra cost over dermal sling alone. The combination ‘double proofs’ the T-junction by providing additional coverage of the implant compared with the dermal sling alone. Additionally, acellular dermal matrices are now widely thought to protect against or reduce the incidence of radiation-induced capsular contracture hence were used when radiotherapy was planned in these large breasted patients.12 Thus, the patient is potentially saved an additional procedure of capsulectomy and implant exchange which may be needed to treat radiation-induced capsular contracture. Additionally, the T-junction breakdown in Wise pattern skin-reducing mastectomies is at least 25% so the additional implant coverage with an acellular dermal matrix is useful.24 The dermal sling also provided extra padding and volume to the breasts and possibly reduced the expansion required. The addition of the acellular dermal matrix to the muscular pocket improves the reliability of the Wise-pattern skin-reducing mastectomy technique while the vascularised dermosubcutaneous fat ‘pedicle’ serves to preserve the integrity of the reconstruction in the presence of any T-junction breakdown. The acellular dermal matrix and dermal sling thus act in a synergistic manner. Despite positive results reported in the past, this technique appears to be widely neglected by many reconstructive surgeons, who should consider it in large-breasted or significantly ptotic implant-reconstruction candidates.
In the present small series, acellular dermal matrices were successfully combined with dermal slings for double coverage of the lower poles of the reconstructed breasts. The slings provided further soft tissue support of the implant and protected it and the acellular dermal matrices from any T-junction wound healing problems. This approach is applicable to large and ptotic breasts thereby broadening the suitable population for implant-based reconstructions and widening patient choice.
Conclusions
The series of patients herein reviewed and the current literature suggest that the combination of a de-epithelialised dermal flap and an acellular dermal matrix in skin-reducing mastectomy may offer both clinical and aesthetic advantages. Creating such a flap is a relatively simple and short addition to a procedure involving an acellular dermal matrix. This combination offers another option for large-breasted or significantly ptotic implant-based reconstruction candidates especially when radiotherapy is planned. The present study, for the first time, demonstrates the applicability of the dermal flap in conjunction with nonhuman acellular dermal matrices of different types and the feasibility of this combination for use in both pre-pectoral and sub-pectoral immediate breast reconstructions.
References
- 1.Halsted CP, Benson JR, Jatoi I. A historical account of breast cancer surgery: beware of local recurrence but be not radical. Future Oncol 2014; (9): 1,649–1,657. [DOI] [PubMed] [Google Scholar]
- 2.Toth BA, Lappert P. Modified skin incisions for mastectomy: the need for plastic surgical input in preoperative planning. Plast Reconstr Surg 1991; (6): 1,048–1,053. [PubMed] [Google Scholar]
- 3.Rice CO, Strickler JH. Adeno-mammectomy for benign breast lesions. Surg Gynecol Obstet 1951; (6): 759–762. [PubMed] [Google Scholar]
- 4.Veronesi U, Stafyla V, Petit J-Y, Veronesi P. Conservative mastectomy: extending the idea of breast conservation. Lancet Oncol 2012; (7): e311–e317. [DOI] [PubMed] [Google Scholar]
- 5.Nava MB, Cortinovis U, Ottolenghi J et al. Skin-reducing mastectomy. Plast Reconstr Surg 2006; (3): 603–613. [DOI] [PubMed] [Google Scholar]
- 6.Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skin-sparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg 2002; (1): 206–211. [DOI] [PubMed] [Google Scholar]
- 7.Goyal A, Wu JM, Chandran VP, Reed MWR. Outcome after autologous dermal sling-assisted immediate breast reconstruction. BJS 2011; (9): 1,267–1,272. [DOI] [PubMed] [Google Scholar]
- 8.Sbitany H, Langstein HN. Acellular dermal matrix in primary breast reconstruction. Aesthet Surg J 2011; (7 Supplement): 30S–37S. [DOI] [PubMed] [Google Scholar]
- 9.Vardanian AJ, Clayton JL, Roostaeian J et al. Comparison of implant-based immediate breast reconstruction with and without acellular dermal matrix. Plast Reconstr Surg 2011; (5): 403e–410e. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen KT, Mioton LM, Smetona JT et al. Esthetic outcomes of ADM-assisted expander-implant breast reconstruction. Eplasty 2012; : e58. [PMC free article] [PubMed] [Google Scholar]
- 11.Forsberg CG, Kelly DA, Wood BC et al. Aesthetic outcomes of acellular dermal matrix in tissue expander/implant-based breast reconstruction. Ann Plast Surg 2014; (6): S116–S120. [DOI] [PubMed] [Google Scholar]
- 12.Lardi AM, Ho-Asjoe M, Junge K, Farhadi J. Capsular contracture in implant based breast reconstruction: the effect of porcine acellular dermal matrix. Gland Surg 2017; (1): 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malata CM, Hodgson ELB, Chikwe J et al. An application of the LeJour vertical mammaplasty pattern for skin-sparing mastectomy: a preliminary report. Ann Plast Surg 2003; (4): 345–352. [DOI] [PubMed] [Google Scholar]
- 14.Hunter JE, Malata CM. Refinements of the LeJour vertical mammaplasty skin pattern for skin-sparing mastectomy and immediate breast reconstruction. J Plast Reconstr Aesthet Surg 2007; (5): 471–481. [DOI] [PubMed] [Google Scholar]
- 15.Querci della Rovere G, Nava M, Bonomi R et al. Skin-reducing mastectomy with breast reconstruction and sub-pectoral implants. J Plast Reconstr Aesthet Surg 2008; (11): 1,303–1,308. [DOI] [PubMed] [Google Scholar]
- 16.Irwin GW, Black A, Refsum SE, McIntosh SA. Skin-reducing mastectomy and one-stage implant reconstruction with a myodermal flap: a safe and effective technique in risk-reducing and therapeutic mastectomy. J Plast Reconstr Aesthet Surg 2013; (9): 1,188–1,194. [DOI] [PubMed] [Google Scholar]
- 17.Lin IC, Bergey M, Sonnad SS et al. Management of the ptotic or hypertrophic breast in immediate autologous breast reconstruction: a comparison between the wise and vertical reduction patterns for mastectomy. Ann Plast Surg 2013; (3): 264–270. [DOI] [PubMed] [Google Scholar]
- 18.Losken A, Collins BA, Carlson GW. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy and fasciocutaneous flap in women with macromastia. Plast Reconstr Surg 2010; (3): 731–738. [DOI] [PubMed] [Google Scholar]
- 19.Colizzi L, Agostini T, Pascone C et al. A dermomuscular pocket provides superior coverage of the implant in skin-reducing mastectomies. Aesthetic Plast Surg 2010; (5): 675–657. [DOI] [PubMed] [Google Scholar]
- 20.Bayram Y, Kulahci Y, Irgil C et al. Skin-reducing subcutaneous mastectomy using a dermal barrier flap and immediate breast reconstruction with an implant: a new surgical design for reconstruction of early-stage breast cancer. Aesthetic Plast Surg 2010; (1): 71–77. [DOI] [PubMed] [Google Scholar]
- 21.Salgarello M, Visconti G, Barone-Adesi L et al. Inverted-T skin-reducing mastectomy with immediate implant reconstruction using the submuscular-subfascial pocket. Plast Reconstr Surg 2012; (1): 31–41. [DOI] [PubMed] [Google Scholar]
- 22.De Vita R, Pozzi M, Zoccali G et al. Skin-reducing mastectomy and immediate breast reconstruction in patients with macromastia. J Exp Clin Cancer Res 2015; : 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peker F, Yuksel F, Karagoz H, Ozturk S. Breast reconstruction using de-epithelialized dermal flap after vertical-pattern skin-sparing mastectomy in macromastia. A N Z J Surg 2015; (1–2): 64–68. [DOI] [PubMed] [Google Scholar]
- 24.Derderian CA, Karp NS, Choi M. Wise-pattern breast reconstruction: modification using AlloDerm and a vascularized dermal-subcutaneous pedicle. Ann Plast Surg 2009; (5): 528–532. [DOI] [PubMed] [Google Scholar]
- 25.Caputo GG, Marchetti A, Dalla Pozza E et al. Skin-reduction breast reconstructions with prepectoral implant. Plast Reconstr Surg 2016; (6): 1,702–1,705. [DOI] [PubMed] [Google Scholar]