Abstract
Over the past three decades, management of blunt splenic trauma has changed radically. Use of improved diagnostic techniques and proper understanding of disease pathology has led to nonoperative management being chosen as the standard of care in patients who are haemodynamically stable. This review was undertaken to assess available literature regarding changing trends of management of blunt splenic trauma, and to identify the existing lacunae in nonoperative management.
The PubMed database was searched for studies published between January 1987 and August 2017, using the keywords ‘blunt splenic trauma’ and ‘nonoperative management’. One hundred and fifty-three articles were reviewed, of which 82 free full texts and free abstracts were used in the current review.
There is clear evidence in published literature of the greater success of nonoperative over operative management in patients who are haemodynamically stable and the increasing utility of adjunctive therapies like angiography with embolisation. However, the review revealed a lack of universal guidelines for patient selection criteria and diagnostic and grading procedures needed for nonoperative management. Indications for splenic artery embolisation, the current role of splenectomy and spleen-preserving surgeries, together with the place of minimal access surgery in blunt splenic trauma remain grey areas. Moreover, parameters affecting the outcomes of nonoperative management and its failure and management need to be defined. This shows a need for future studies focused on these shortcomings with the ultimate aim being the formulation and implementation of universally accepted guidelines for safe and efficient management of blunt splenic trauma.
Keywords: Splenic trauma, emergency care, nonoperative management
Introduction
Trauma is the leading cause of death in people under the age of 45 years and is among the top three leading causes of death in all age groups.1 Abdominal trauma accounts for around 15% of cases presenting to the emergency department, with the spleen being the most commonly injured organ in blunt abdominal trauma.2 Splenic trauma was managed operatively for many years as it was believed that the spleen was devoid of important function, that it could not heal on its own, could rupture at a later stage, and that the mortality rate of patients who were not operated was unacceptably high.3 However, the knowledge of increased risk of susceptibility to infection after splenectomy, with its most deadly manifestation, overwhelming post-splenectomy infection, occurring in about 0.5% of all splenectomies in trauma patients and in over 20% of elective splenectomies for haematological disorders, led to a paradigm shift in the management of blunt splenic injury. Nonoperative management of splenic injuries has gradually become the standard of therapy in patients who are haemodynamically stable.4,5 Currently, three methods of treatment of splenic trauma patients are followed: conservation (with or without angiography and embolisation), spleen-preserving operations and splenectomy.6
Methodology
The PubMed database was searched for articles published between January 1987 and August 2017, using the keywords ‘blunt splenic trauma’ and ‘nonoperative management’. One hundred and fifty-three articles were identified. Case reports and small case series were excluded. The articles were then reviewed for relevance and 72 articles were used in the current review. Free full texts and free abstracts were used in the evaluation process. The articles were used to answer six relevant questions that will reflect the trends in management of blunt splenic injury:
Patient selection criteria for nonoperative management.
Trends of acceptance, success and failure of nonoperative management.
Splenic artery embolisation.
Spleen-preserving surgeries.
Grading of splenic injuries,
Evolution of minimal access surgery in splenic trauma.
Results
Criteria for nonoperative management
Nonoperative management of splenic trauma was documented as early as 1882 by Gross.7 It consists of close observation of the patient, coupled with splenic artery embolisation if necessary. Observational management involves hospitalisation, close monitoring, serial abdominal examinations and facilities of blood transfusion and computed tomography.8 Initially, nonoperative management for splenic trauma was documented in children, with excellent outcomes.7,9 However, employing nonoperative management for splenic injuries in adults was a challenge, as post-splenectomy sepsis is less frequent in adults, and in view of delayed haemostasis due to age-related structural and vascular changes of the spleen, and the risk of overlooked associated injuries and the possibility of delayed rupture of the spleen, splenosis or a post-traumatic splenic cyst.10 In 1987, Johns Hopkins Medical Institutions published criteria for nonoperative management as: 1) rapid haemodynamic stabilisation after fluid resuscitation; 2) lack of other serious intra-abdominal injuries; 3) lack of extra-abdominal trauma that requires a prolonged general anaesthesia or that results in an altered state of consciousness; 4) progressive symptomatic improvement early during the hospitalisation.11 However, there has been no universally accepted set of guidelines for patient eligibility for nonoperative management, with haemodynamic stability and low grades of injury being the commonly accepted criteria. The 2017 guidelines from the World Society of Emergency Surgery give a detailed algorithm for the management of splenic trauma, which is based broadly on haemodynamic stability of the patient, grade of injury and availability of intensive care.12
Success and failure of nonoperative management
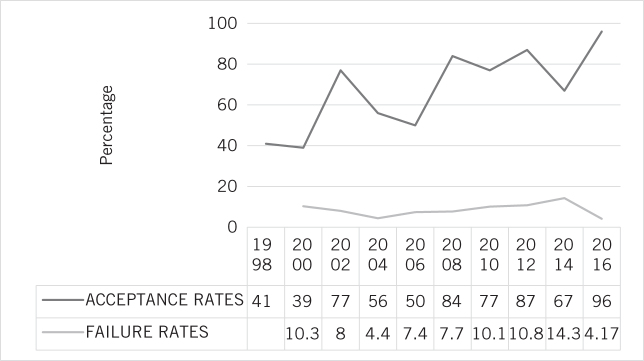
It was routine practice for most minor splenic injuries to be treated nonoperatively after 1997, with the rate of nonoperative management increasing from 48.5% between 1992 and 1996 to 63.1% between 1997 and 2001 (P = 0.02).13 Between 1989 and 1997, splenic salvage rate of low-grade injuries has been as high as 97%.14–16 Increase in nonoperative management for splenic trauma over the past two decades is shown in Figure 1.17–26
Figure 1.
Nonoperative management of blunt splenic trauma: acceptance and failure rates, 1998–2016.
Controversies remained regarding the management of higher grades of splenic injury, as failure of nonoperative management was significantly higher in grade V injuries compared with lower grades of injury (P < 0.05).27,28 Controversies also raged for defining predictive parameters for a successful nonoperative management and some authors have defined predictive parameters and outcome of this type of management (Table 1).29–33
Table 1.
Predictive parameters for successful and unsuccessful nonoperative management of blunt splenic trauma.
| Parameter | Nonoperative management | |
| Successful4,29,30 | Unsuccessful31–33 | |
| Haemodynamics | Stable/readily stabilised | Unstable (systolic blood pressure < 90 mmHg despite adequate resuscitation) |
| Blood transfusion | ≤ 4 units | > 4 units (to maintain a haemoglobin level > 10 g/dl) |
| Age(years) | ≤ 55 | > 55 |
| Leucocytosis | No | Persistent |
| Other abdominal signs and symptoms | Early resolution of splenic abnormalities obvious on imaging | Onset or aggravating signs of peritoneal irritation (suggesting further bleeding or other overlooked injuries) |
| No periods of unconsciousness or brain injuries | Intra-abdominal compartment syndrome (intravesical pressure > 20 cm H2O) | |
| Injuries | No associated intra- or retroperitoneal injuries (on CT) that would require surgical intervention | Worsening signs of splenic injury (repeated ultrasound), post-traumatic splenic defect |
| No rebound or guarding | ||
| Complete recovery of bowel movements | ||
With the advent of advanced diagnostic imaging and splenic artery embolisation, the success of nonoperative management has increased significantly.34,35 Nonoperative management has primarily reduced the risk of overwhelming post-splenectomy infection.4 Moreover, avoidance of surgery-related complications, a shorter hospitalisation period and a concomitant reduction in costs have been reported.36 In case of failure of nonoperative management, there is the possibility of a second nonoperative reintervention; for example, an attempt for splenic artery embolisation after failure of observation or proximal embolisation after failure of distal embolisation. However, nonoperative management carries a risk of delayed splenic rupture, the possibility of re-bleeding and complications related to embolisation, but exact incidences of each were not quoted in the searched literature. The fact that no (intraoperative) view can be obtained of other abdominal organs is also an important disadvantage. The common advantages, disadvantages and complications related to nonoperative management are shown in Box 1. Close monitoring of patients along with frequent computed tomography (CT) has helped overcome these drawbacks to a certain extent. Failure rates of nonoperative management are shown in Figure 1.18–23,26,37,38 Thus, for successful nonoperative management of splenic trauma, it is necessary to have an accurate knowledge of patient selection criteria as well as a precise assessment of the factors precluding conservative therapy.
Box 1.
Advantages, disadvantages and complications (immediate and delayed) of nonoperative management of splenic trauma.
Advantages
Avoids immediate and late complications of splenectomy
Avoids complications related to surgery and anaesthesia
Avoids operation costs
High success rates, especially in lower injury grades
Disadvantages
Only possible if grade of splenic injury is identified accurately
Requires intensive monitoring
Requires 24-hour availability of operating theatre, laboratory and blood transfusion facilitieas
Requires availability of interventional radiologist with computed tomography facilities
Risk of missed injuries in polytrauma
Complications
Immediate (up to 7 days):
Pseudoaneurysm formation, leading to bleeding or rupture
Peritonitis
Delayed (beyond 7 days):
Delayed rupture of spleen
Intestinal obstruction due to peritoneal adhesions
Splenosis
Splenic artery embolisation
The first angiographic embolisations used absorbable gelatine and temporary balloon occlusion, and were performed for haemostatic purposes before splenectomy.39 Recent nonoperative management protocols for splenic trauma include angiography (diagnostic and therapeutic) as an efficient alternative.40 Splenic artery embolisation can be distal (supraselective), proximal (splenic artery) and combined (Box 2).41–42 Diagnostic and therapeutic (embolisation) angiography is performed if CT shows intrasplenic vascular damage, while second-look angiography may be used in cases of recurrent bleeding and after an initially negative angiograph.43
Box 2.
Indications and complications of splenic artery embolisation (SAE).
Indications
-
Proximal: Indicated in the following hilar lesions:
>3 distinct peripheral vascular lesions
injury affects more than 50% of the splenic parenchyma.
Selective: limited vascular injuries. It is proficient because it allows proper haemostasis and adequate perfusion to remaining organ.
Combined: for multiple vascular injuries (high injury scores). It is recommended to perform multiple CT scans after SAE to monitor the vascular damage, pseudoaneurysm formation, size of infarcted area and existence of localised infection (splenic abscess).
Complications
Major (19–28.5%):
Bleeding: the most common complication caused by delayed diagnosis of pseudo aneurysms and late pseudoaneurysm formation
Overlooked injuries: usually diaphragmatic, pancreatic
Infection: splenic abscess, sepsis
Splenic atrophy
latrogenic arterial damage
Acute renal failure after contrast administration
Deep venous thrombosis
Minor (23–61.9%):
Migration of embolic material (spiral that migrates in proximal SAE needs extraction)
Angiographic vascular dissection
Vascular damage when inserting the catheter(arteriovenous fistula)
Persistent pain and hematoma at the puncture site
Post-embolisation syndrome (includes symptoms such as general discomfort, fever, local pain and/or leucocytosis, which generally persist for 3–5 days)
Pleural and pulmonary complications
Thrombocytosis
Allergic reactions to contrast
Splenic artery embolisation, although controversial in 2008, has shown a progressive reduction failure rate of nonoperative management, from 25% to 10%, and an increase in splenic salvage rate from 79% to 100%.44 Failure rates of nonoperative management in grades IV and V splenic injuries decreased from 23% (no artery embolisation) to 3% ( with artery embolisation), P = 0.04, and from 63% (no artery embolisation) to 9% (with artery embolisation), P = 0.03.45 Angiography and embolisation were recommended as an adjunct to nonoperative management for all grade III to grade V injuries.46,47 However, splenic artery embolisation is associated with various complications (Table 3).48–54 One study has shown no significant difference between embolisation and observation alone with regard to successful treatment in patients with blunt splenic trauma.55 An approach to management of blunt splenic trauma based on the reviewed literature considering the present role of nonoperative management and splenic artery embolisation is shown in Figure 2.
Figure 2 .
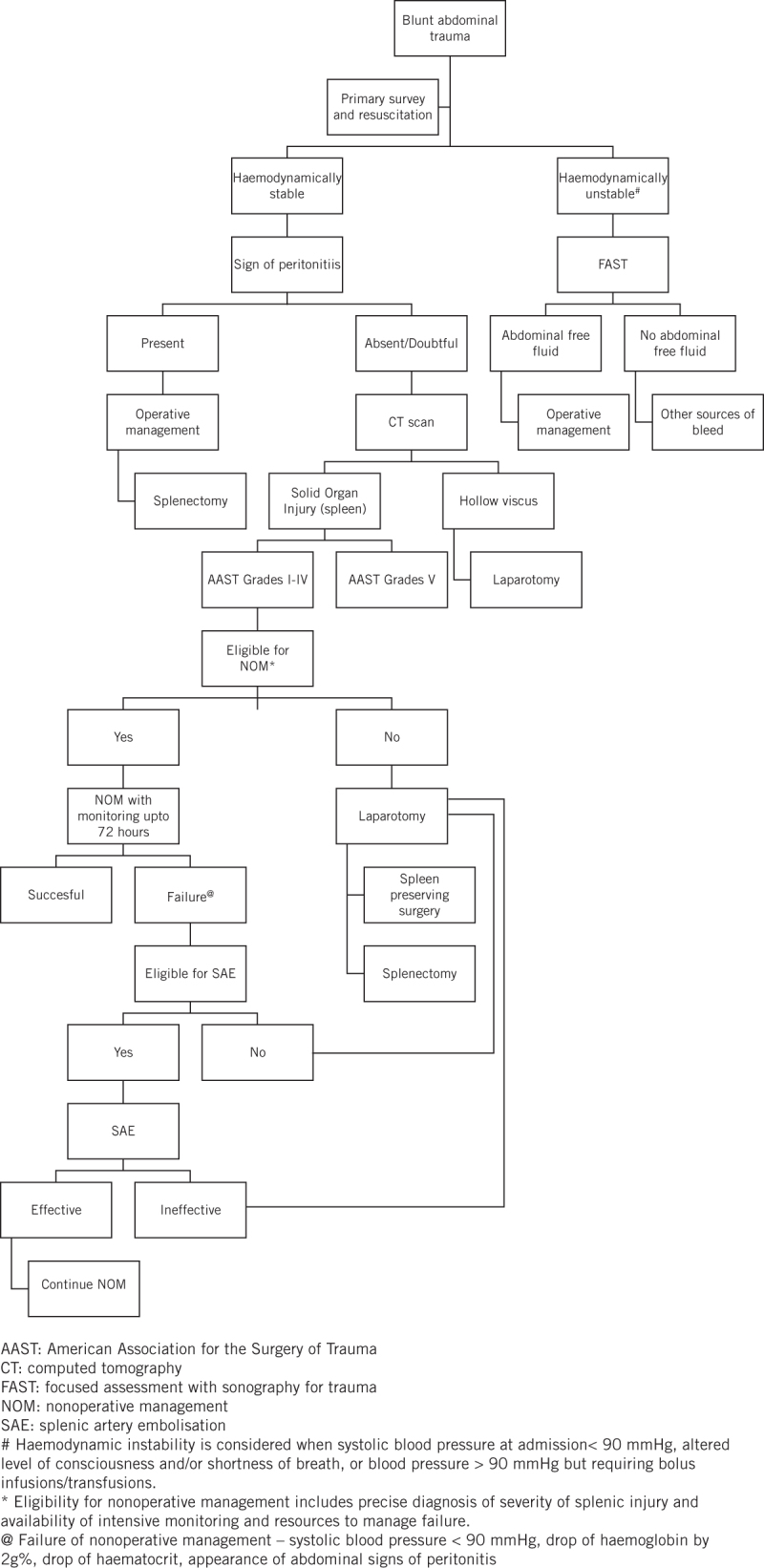
An approach to management of blunt splenic trauma in adult patients.
Spleen-preserving surgeries
Partial splenectomy requires mature judgement for patient selection as well as technical skill. A partial splenectomy or splenorrhaphy requires at least one-third of viable splenic tissue. Essential steps are atraumatic mobilisation of spleen, temporary splenic artery occlusion, selective ligation of segmental vasculature, controlled intrasplenic dissection with ultrasonic surgical aspirators and, finally, haemostasis by topical agents (oxidised cellulose) or argon plasma. Mesh splenorrhaphy includes delivering the spleen through the centre of an absorbable mesh and sewing opposite edges of the mesh to each other to produce a tamponade around the spleen. The retained spleen is observed for colour and bleeding at adequate systolic blood pressure. Drains are required only if pancreatic injury is suspected.56 Studies completed in the 1990s by scintigraphy showed that splenic autotransplantation is superior to splenectomy but less effective than preservation of the spleen.57 The technique of autotransplantation has been described by various authors.58,59 Commonly 2–4 grams of splenic tissue are minced and implanted in an omental pocket in the greater omentum. Excellent response has been reported from Germany, where 6 months after autotransplantation in adults, Howell-Jolly bodies were absent and immunoglobulins were normal.60 Splenic autotransplantation in greater omentum has also been proposed in children with a report showing some preservation of immunological function (2 of 40 measurements; 5%).57 New procedures such as polyglycolic acid elastic mesh for splenic capping, use of autologous fibrin glue and radiofrequency ablation to stop bleeding were experimented on animal models and small populations in later years ,with favourable outcomes.61–66
Grading splenic injury
The aim of a grading system is to standardise reporting and to aid management planning. The American Association for the Surgery of Trauma (AAST) Organ Injury Scale is the most widely used scale for grading splenic injuries.67 It is a classification system based on anatomical damage caused by injury to an individual organ. The injury grading scale for the spleen was revised in 1994, as a result of increasing use of CT in the management of blunt abdominal trauma. However, active bleeding and vascular injuries were not considered in this revision, thus limiting its utility as an aid to clinical decision making in nonoperative management.
Various studies between 1994–2012 have suggested that CT results alone are a poor predictor of success in nonoperative management.68–70 The need for incorporating active vascular injuries and nonbleeding vascular injuries has been stressed by some authors.71,72 In 2007, Marmery et al.73 proposed a new system (the Baltimore CT Severity Index), which included active splenic haemorrhage as well as non-bleeding vascular injuries. This was found to be superior to the AAST grading system in predicting the need for splenic artery embolisation or surgery.74 The 2013 study by Boscak et al.75 emphasised the importance of using both arterial and portal venous images to detect vascular injuries.
Minimal access surgery in splenic trauma
In 1992, laparoscopic splenectomy was beginning to be viewed as a promising alternative to open splenic surgery in haemodynamically stable patients and in spleen preserving surgeries.76,77 By 1996, with the widespread use of diagnostic laparoscopy for blunt abdominal trauma and therapeutic laparoscopy in cholecystectomy, surgeons started to use therapeutic laparoscopy in cases of mild splenic lesions. It was also used in the treatment of late consequences of splenic injury, such as post-traumatic pseudocysts.78,79 With a view to preventing immediate and later complications of splenectomy, conservative surgical techniques gradually gained success. With the establishment of nonoperative management for splenic trauma by 2008, indications for laparoscopic splenectomy were restricted to continued bleeding after splenic embolisation, splenic infarction with abscess formation or high-grade injuries.80 Robotic approach for splenectomy in blunt trauma was suggested in 2015, but needs definite conclusions.81 In 2017, laparoscopy is generally performed in cases of failure of nonoperative management and has shown significantly less blood loss and fewer transfusions compared with the open group, although there were no differences in mortality, length of stay, complications or discharge dispositions in one study.82
Conclusion
Management of splenic injury has evolved over the past three decades, with nonoperative management replacing surgical intervention as the standard of care. The patient selection criteria for nonoperative management are primarily based on haemodynamic stability, grade of splenic trauma, exclusion of multisystem injury and availability of continuous diagnostic and intensive care facilities. There has been a progressive increase in the success rates of nonoperative management, with a considerable reduction in failure rates, especially after application of splenic artery embolisation and CT diagnosis. Spleen-preserving surgeries have been performed in cases of failure of nonoperative management with favourable outcomes. Minimal access surgery now holds promise in the management of splenic trauma in the decade to come.
Questions still remain regarding formulation of definite patient selection criteria for nonoperative management and splenic artery embolisation, and their appropriate application. Formulation of management protocol of high-grade injuries, together with a decrease in the complications and failure rate of nonoperative management should be prioritised in further studies. Prospective trials with clear inclusion criteria are also needed to prove the benefit of laparoscopic splenic surgeries.
This study was limited by the fact that only free full-text articles were used and further grouping of the references for levels of evidence was not done.
References
- 1.Rhee P, Joseph B, Pandit V et al. Increasing trauma deaths in the United States. Ann Surg 2014; (1): 13–21. [DOI] [PubMed] [Google Scholar]
- 2.Poletti PA, Mirvis SE, Shanmuganathan K et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography? J Trauma 2004; (5): 1,072–1,081. [DOI] [PubMed] [Google Scholar]
- 3.Richardson JD. Changes in the management of injuries to the liver and spleen. J Am Coll Surg 2013; (5): 648–669. [DOI] [PubMed] [Google Scholar]
- 4.Uranüs S, Pfeifer J. Nonoperative management of blunt splenic injury. World J Surg 2001; : 1,405–1,407. [DOI] [PubMed] [Google Scholar]
- 5.Olthof DC, van der Vlies CH, Goslings JC. Evidence-based management and controversies in blunt splenic trauma. Curr Trauma Rep 2017; : 32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ermolov AS, Tlibekova MA, Yartsev PA et al. Laparoscopic splenectomy in patients with spleen injuries. surgical laparoscopy, endoscopy and percutaneous techniques. 2015; (6): 483–486. [DOI] [PubMed] [Google Scholar]
- 7.McClusky DA III, Skandalakis LJ, Colborn GL, Skandalakis JE. Tribute to a triad: history of splenic anatomy, physiology, and surgery, part 2. World J Surg 1999; : 514–526. [DOI] [PubMed] [Google Scholar]
- 8.Pachter HL, Guth AA, Hofstetter SR, Spencer FC. Changing patterns in the management of splenic trauma: the impact of nonoperative management. Ann Surg 1998; (5): 708–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lucas CE. Splenic trauma: choice of management. Ann Surg 1991; : 98–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gibney EJ. Non-operative management of blunt splenic injury – works well in about a quarter of patients. BMJ 1991; : 1,553–1,554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiebke EA, Sarr MG, Fishman EK, Ratych RE. Nonoperative management of splenic injuries in adults: an alternative in selected patients. Am Surg 1987; (10): 547–552. [PubMed] [Google Scholar]
- 12.Coccolini F, Montori G, Catena F et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017; : 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cadeddu M, Garnett A, Al-Anezi K, Farrokhyar F. Management of spleen injuries in the adult trauma population: a ten-year experience. Can J Surg 2006; (6): 386–390. [PMC free article] [PubMed] [Google Scholar]
- 14.Sclafani SJ, Weisberg A, Scalea TM et al. Blunt splenic injuries: nonsurgical treatment with CT, arteriography, and transcatheter arterial embolization of the splenic artery. Radiology 1991; (1): 189–196. [DOI] [PubMed] [Google Scholar]
- 15.Smith JS Jr, Cooney RN, Mucha P Jr. Nonoperative management of the ruptured spleen: a revalidation of criteria. Surgery 1996; (4): 745–750. [DOI] [PubMed] [Google Scholar]
- 16.Sclafani SJ, Shaftan GW, Scalea TM et al. Nonoperative salvage of computed tomography-diagnosed splenic injuries: utilization of angiography for triage and embolization for hemostasis. J Trauma 1995; (5): 818–825. [DOI] [PubMed] [Google Scholar]
- 17.Bain IM, Kirby RM. 10 year experience of splenic injury: an increasing place for conservative management after blunt trauma. Injury 1998; (3): 177–182. [DOI] [PubMed] [Google Scholar]
- 18.Aseervatham R, Muller M. Blunt trauma to the spleen. Aust N Z J Surg 2000; (5): 333–337. [DOI] [PubMed] [Google Scholar]
- 19.Bee TK, Croce MA, Miller PR et al. Failures of splenic nonoperative management: is the glass half empty or half full? J Trauma 2001; (2): 230–236. [DOI] [PubMed] [Google Scholar]
- 20.Lo A, Matheson AM, Adams D. Impact of concomitant trauma in the management of blunt splenic injuries. N Z Med J 2004; (1201): U1052. [PubMed] [Google Scholar]
- 21.Yang J, Gao JM, Jean-Claude B. Non-operative management of adult blunt splenic injuries. Chin J Traumatol 2006; (4): 246–248. [PubMed] [Google Scholar]
- 22.Benissa N, Boufettal R, Kadiri Y et al. Non operative management of blunt splenic trauma in adults. J Chir (Paris) 2008; (6): 556–560. [DOI] [PubMed] [Google Scholar]
- 23.Renzulli P, Gross T, Schnüriger B et al. Management of blunt injuries to the spleen. Br J Surg 2010; (11): 1,696–1,703. [DOI] [PubMed] [Google Scholar]
- 24.Clancy AA, Tiruta C, Ashman D et al. The song remains the same although the instruments are changing: complications following selective non-operative management of blunt spleen trauma: a retrospective review of patients at a level I trauma centre from 1996 to 2007. J Trauma Manag Outcomes 2012; (1): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller PR, Chang MC, Hoth JJ et al. Prospective trial of angiography and embolization for all grade III to V blunt splenic injuries: nonoperative management success rate is significantly improved. J Am Coll Surg 2014; (4): 644–648. [DOI] [PubMed] [Google Scholar]
- 26.Tugnoli G, Bianchi E, Biscardi A et al. Nonoperative management of blunt splenic injury in adults: there is (still) a long way to go. The results of the Bologna-Maggiore Hospital trauma center experience and development of a clinical algorithm. Surg Today 2015; (10): 1,210–1,217. [DOI] [PubMed] [Google Scholar]
- 27.Peitzman AB, Heil B, Rivera L et al. Blunt splenic injury in adults: multi-institutional study of the Eastern Association for the Surgery of Trauma. J Trauma 2000; (2): 177–189. [DOI] [PubMed] [Google Scholar]
- 28.Gaarder C, Dormagen JB, Eken T et al. Nonoperative management of splenic injuries: improved results with angioembolization. J Trauma 2006; (1): 192–198. [DOI] [PubMed] [Google Scholar]
- 29.Longo WE, Baker CC, McMillen MA et al. Nonoperative management of adult blunt splenic trauma; criteria for successful outcome. Ann Surg 1989; : 626–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sartorelli KH, Frumiento C, Rogers FB, Osler TM. Nonoperative management of hepatic, splenic, and renal injuries in adults with multiple injuries. J Trauma 2000; : 56–62. [DOI] [PubMed] [Google Scholar]
- 31.Velhamos GC, Chan LS, Kamel E et al. Nonoperative management of splenic injuries; have we gone too far?. Arch Surg 2000; : 674–681. [DOI] [PubMed] [Google Scholar]
- 32.Kluger Y, Rabau M, Rub R et al. Comparative study of splenic wound healing in young and adult rats. J Trauma 1999; : 261–264. [DOI] [PubMed] [Google Scholar]
- 33.Wisner DH. Injury to the Spleen In: Moore EE, Feliciano DV, Mattox KL, Trauma, 5th ed New York: McGraw-Hill; 2004: 663–685. [Google Scholar]
- 34.Liu PP, Lee WC, Cheng YF et al. Use of splenic artery embolization as an adjunct to nonsurgical management of blunt splenic injury. J Trauma 2004; (4): 768–773. [DOI] [PubMed] [Google Scholar]
- 35.Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma 2005; (3): 492–498. [DOI] [PubMed] [Google Scholar]
- 36.Watson GA, Rosengart MR, Zenati MS et al. Nonoperative management of severe blunt splenic injury: are we getting better?. J Trauma 2006; (6): 386–390. [DOI] [PubMed] [Google Scholar]
- 37.M Beuran, I Gheju, MD Venter et al. Non-operative management of splenic trauma. J Med Life 2012; (1): 47–58. [PMC free article] [PubMed] [Google Scholar]
- 38.Cirocchi R, Corsi A, Castellani E et al. Case series of non-operative management vs. operative management of splenic injury after blunt trauma. Ulus Travma Acil Cerrahi Derg 2014; (2): 91–96. [DOI] [PubMed] [Google Scholar]
- 39.Sclafani SJA. The role of angiographic hemostasis in salvage of the injured spleen. Radiology 1981; : 645–650. [DOI] [PubMed] [Google Scholar]
- 40.Sosada K, Wiewióra M, Piecuch J. Literature review of non -operative management of patients with blunt splenic injury: impact of splenic artery embolization. Wideochir Inne Tech Maloinwazyjne 2014; (3): 309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lui B, Schlicht S, Vrazas J. Role of embolization in the management of splenic trauma. Aust Radiol 2004; : 401–403. [DOI] [PubMed] [Google Scholar]
- 42.Gaarder C, Dormagen JB, Eken T et al. Nonoperative management of splenic injuries: improved results with angioembolization. J Trauma 2006; : 192–198. [DOI] [PubMed] [Google Scholar]
- 43.Haan J, Scott J, Boyd-Kranis RL et al. Admission angiography for blunt splenic injury: advantages and pitfalls. J Trauma 2001; : 1,161–1,165. [DOI] [PubMed] [Google Scholar]
- 44.Wu SC, Chen RJ, Yang AD et al. Complications associated with embolization in the treatment of blunt splenic injury. World J Surg 2008; (3): 476–482. [DOI] [PubMed] [Google Scholar]
- 45.Bhangu A, Nepogodiev D, Lal N, Bowley DM. Meta-analysis of predictive factors and outcomes for failure of non-operative management of blunt splenic trauma. Injury 2012; (9): 1,337–1,346. [DOI] [PubMed] [Google Scholar]
- 46.Dehli T, Bågenholm A, Trasti NC et al. The treatment of spleen injuries: a retrospective study. Scand J Trauma Resusc Emerg Med 2015; : 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bhullar IS, Tepas JJ 3rd, Siragusa D et al. To nearly come full circle: Nonoperative management of high-grade IV-V blunt splenic trauma is safe using a protocol with routine angioembolization. J Trauma Acute Care Surg 2017; (4): 657–664. [DOI] [PubMed] [Google Scholar]
- 48.Sclafani SJA, Shaftan GW, Scalea TM et al. Non-operative salvage of computed tomography-diagnosed splenic injuries: utilization of angiography for triage and embolization for hemostasis. J Trauma 1995; : 818–827. [DOI] [PubMed] [Google Scholar]
- 49.Haan J, Ilahi ON, Kramer M et al. Protocol-driven nonoperative management in patients with blunt splenic trauma and minimal associated injury decrease length of stay. J Trauma 2003; : 317–322. [DOI] [PubMed] [Google Scholar]
- 50.Liu PP, Lee WC, Cheng YF et al. Use of splenic artery embolisation as an adjunct to nonsurgical management of blunt splenic injury. J Trauma 2004; : 768–773. [DOI] [PubMed] [Google Scholar]
- 51.Drooz AT, Lewis CA, Allen TE et al. Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for percutaneous transcatheter embolization. J Vasc Interv Radiol 2003; : S237–S242. [PubMed] [Google Scholar]
- 52.Velmahos GC, Chahwan S, Falabella A et al. Angiographic embolisation for intraperitoneal and retroperitoneal injuries. World J Surg 2000; : 539–545. [DOI] [PubMed] [Google Scholar]
- 53.Smith HE, Biffl WL, Majercik SD et al. Splenic artery embolization: have we gone too far?. J Trauma 2006; : 541–546. [DOI] [PubMed] [Google Scholar]
- 54.Shih HC, Wang CY, Wen YS et al. Spleen artery embolization aggravates endotoxin hyporesponse of peripheral blood mononuclear cells in patients with spleen injury. J Trauma 2010; : 532–537. [DOI] [PubMed] [Google Scholar]
- 55.Olthof DC, Joosse P, Bossuyt PM et al. Observation versus embolization in patients with blunt splenic injury after trauma: a propensity score analysis. World J Surg 2016; (5): 1,264–1,271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Morgenstern L. Technique of partial splenectomy. Prob Gen Surg 1990; : 103–112. [Google Scholar]
- 57.Weber T, Hanisch E, Baum RP, Seufert RM. Late results of heterotopic autotransplantation of splenic tissue into the greater omentum. World J Surg 1998; (8): 883–889. [DOI] [PubMed] [Google Scholar]
- 58.Iapryntsev IM, Egiazarian VT, Avetian SK. Autotransplantation of splenic tissue after splenectomy. Vestn Khir Im I I Grek 1989; (8): 75–76. [PubMed] [Google Scholar]
- 59.Henneking K, Müller C, Franke F et al. Follow-up of heterotopic autotransplantation of splenic tissue after traumatic splenic rupture in childhood. Chirurg 1994; (5): 457–468. [PubMed] [Google Scholar]
- 60.Youssef S, Stauffer UG. Heterotopic autotransplantation of splenic tissue after traumatic rupture of the spleen - a solution after unavoidable splenectomy?. Z Kinderchir 1982; (3): 88–89. [DOI] [PubMed] [Google Scholar]
- 61.Takeda J, Hashimoto K, Tanaka M et al. Experimental and clinical evaluation of the splenic capping method in the treatment of injured spleens. Japan J Surg 1990; (2): 137–142. [DOI] [PubMed] [Google Scholar]
- 62.Kuzu A, Aydintug S, Karayalcin K et al. Use of autologous fibrin glue in the treatment of splenic trauma: an experimental study. J R Coll Surg Edinb 1992; (3): 162–164. [PubMed] [Google Scholar]
- 63.Felekouras E, Kontos M, Pissanou T et al. A new spleen-preserving technique using radiofrequency ablation technology. J Trauma 2004; (6): 1,225–1,229. [DOI] [PubMed] [Google Scholar]
- 64.Olmi S, Scaini A, Erba L et al. Use of fibrin glue (Tissucol) as a hemostatic in laparoscopic conservative treatment of spleen trauma. Surg Endosc 2007; (11): 2,051–2,054. [DOI] [PubMed] [Google Scholar]
- 65.Jarry J, Bodin R, Claverie D, Evrard S. Radiofrequency fulguration of the spleen under laparoscopy to stop iatrogenic hemorrhage. Surg Endosc 2012; (4): 1,163–1,164. [DOI] [PubMed] [Google Scholar]
- 66.Li Y, Cui L, Zhang W et al. Laparoscopic radiofrequency ablation for traumatic splenic rupture. J Surg Res 2013; (2): 711–716. [DOI] [PubMed] [Google Scholar]
- 67.Moore EE, Cogbill TH, Jurkovich GJ et al. Organ injury scale: spleen and liver (1994 revision). J Trauma 1995; : 323–324. [DOI] [PubMed] [Google Scholar]
- 68.Carr JA, Roiter C, Alzuhaili A. Correlation of operative and pathological injury grade with computed tomographic grade in the failed nonoperative management of blunt splenic trauma. Eur J Trauma Emerg Surg 2012; (4): 433–438. [DOI] [PubMed] [Google Scholar]
- 69.Cohn SM, Arango JI, Myers JG et al. Computed tomography grading systems poorly predict the need for intervention after spleen and liver injuries. Am Surg 2009; (2): 133–139. [PubMed] [Google Scholar]
- 70.Moore EE, Cogbill TH, Jurkovich GJ et al. Organ injury scaling: spleen and liver (1994 revision). J Trauma 1995; (3): 323–324. [DOI] [PubMed] [Google Scholar]
- 71.Shanmugathan K, Mirvis SE, Boyd-Kranis R et al. Nonsurgical management of blunt splenic trauma: use of CT criteria to select patients for splenic arteriography and potential endovascular therapy. Radiology 2000; : 75–82. [DOI] [PubMed] [Google Scholar]
- 72.Schurr MJ, Fabian TC, Gavant ML et al. Management of blunt splenic trauma: computed tomographic contrast blush predicts failure of nonoperative management. J Trauma 1995; (3): 507–513. [DOI] [PubMed] [Google Scholar]
- 73.Marmery H, Shanmuganathan K, Alexander MT, Mirvis SE. Optimization of selection for nonoperative management of blunt splenic injury: comparison of MDCT grading systems. AJR Am J Roentgenol 2007; : 1,421–1,427. [DOI] [PubMed] [Google Scholar]
- 74.Olthof DC, van der Vlies CH, Scheerder MJ et al. Reliability of injury grading systems for patients with blunt splenic trauma. Injury 2014; (1): 146–150. [DOI] [PubMed] [Google Scholar]
- 75.Boscak AR, Shanmuganathan K, Mirvis SE et al. Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology 2013; (1): 79–88. [DOI] [PubMed] [Google Scholar]
- 76.Pietra N, Carreras F, Longinotti E et al. Videolaparoscopy and conservative treatment of splenic injuries. Acta Biomed Ateneo Parmense 1992; (3–4): 317–321. [PubMed] [Google Scholar]
- 77.Lombardo G, Mastroianni V, Martelli S. Indications for laparoscopy in the diagnosis and treatment of abdominal trauma. Minerva Chir 1994; (7–8): 613–618. [PubMed] [Google Scholar]
- 78.Bové T, Delvaux G, Van Eijkelenburg P et al. Laparoscopic-assisted surgery of the spleen: clinical experience in expanding indications. J Laparoendosc Surg 1996; (4): 213–217. [DOI] [PubMed] [Google Scholar]
- 79.Targarona EM, Trías M. Laparoscopic treatment of splenic injuries. Semin Laparosc Surg 1996; (1): 44–49. [DOI] [PubMed] [Google Scholar]
- 80.Ransom KJ, Kavic MS. Laparoscopic splenectomy following embolization for blunt trauma. JSLS 2008; (2): 202–205. [PMC free article] [PubMed] [Google Scholar]
- 81.Balaphas A, Buchs NC, Meyer J et al. Partial splenectomy in the era of minimally invasive surgery: the current laparoscopic and robotic experiences. Surg Endosc 2015; (12): 3,618–3,627. [DOI] [PubMed] [Google Scholar]
- 82.Huang GS, Chance EA, Hileman BM et al. Laparoscopic splenectomy in hemodynamically stable blunt trauma. JSLS 2017; (2): pii: e2017.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]