Abstract
For decades, the main cause of failure in total knee arthroplasty (TKA) is still the malalignment of prosthetic components. The authors present a case of advanced knee arthrosis, treated by TKA. Preoperative planning was performed with a mobile application and the patient was submitted to primary TKA using an implant developed with inspiration from the theory of “modified GAP” with a rotated tibial tray. Neutral mechanical alignment of the lower limbs was obtained and the application proved to be viable regarding its proposed plan for this case.
Keywords: Mobile applications, Arthroplasty replacement knee, Bone malalignment
Resumo
Ao longo das décadas, a principal causa de insucesso em artroplastias totais do joelho (ATJ) continua a ser o mau alinhamento dos componentes protéticos. Os autores apresentam um caso de artrose avançada do joelho tratado por ATJ. O planejamento pré-operatório foi feito a partir de um aplicativo para dispositivos móveis e a paciente foi submetida à ATJ primária, com um implante desenvolvido com inspiração na teoria do “GAP modificado”, com base tibial rotatória. O alinhamento mecânico neutro dos membros inferiores foi obtido e o aplicativo mostrou-se viável em sua proposta de planejamento para este caso.
Palavras-chave: Aplicativos móveis, Artroplastia do joelho, Mau alinhamento ósseo
Introduction
With the increase of life expectancy of the population, total knee arthroplasty (TKA) has become one of the most commonly performed surgeries in the orthopedic environment.1
Over the years, the main cause of TKA failure continues to be poor alignment of prosthetic components,2 defined as a variation greater than 3° in relation to the angle formed between the center of the femoral head, the center of the knee, and the center of the ankle (ACFKA), which should ideally be neutral.3, 4, 5
Several methods can be used to estimate bone alignment. The panoramic lower limb radiograph (PLLR) is an established method.6
The present study reports the case of a 74-year-old female patient, retired, home walker, in conservative treatment for arthritis of small and large joints, complained of pain of mechanical-inflammatory pattern in both knees, though more intense in the left knee. She presented progressive gonalgia, which had interfered in her sleep for 4 months, despite treatment based on physical therapy and corticosteroid injections on two occasions.
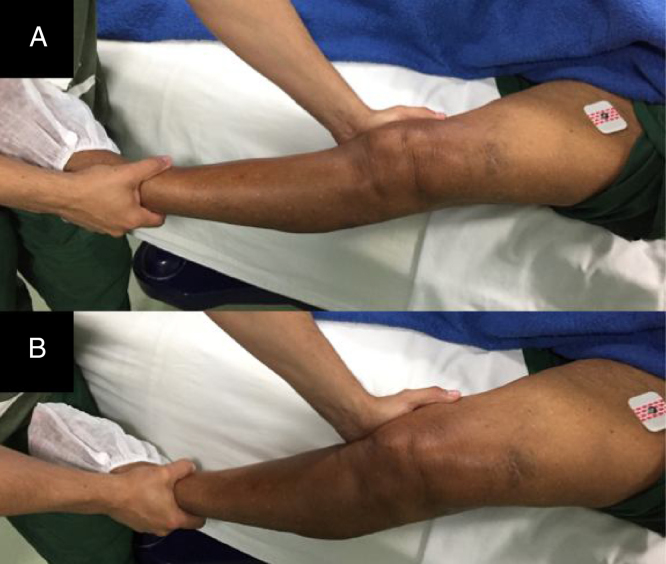
At the physical examination, the patient presented gait with primary support on the lower left limb, which indicated an increase of the support phase and shortening of the step. Upon physical assessment, she presented ‘windblown’ knee deformity, with a valgus right knee and a left varus knee, in addition to indirect signs of moderate venous insufficiency. Upon palpation, considerable crepitus was observed; the range of motion was from 0° to 100°, painful in extreme flexion, both passively and actively. Meniscal tests were strongly positive for the medial meniscus. The ligament tests indicated failure of the anterior cruciate ligament (Lachman test and positive anterior drawer test, with firm stopping) and positive lateral opening stress, with firm stopping (++/3; Fig. 1).
Fig. 1.
Physical examination under anesthesia. Estimation of lateral ligament sufficiency. A, Lateral opening at 0°; B, lateral opening at 30°.
Source: The author.
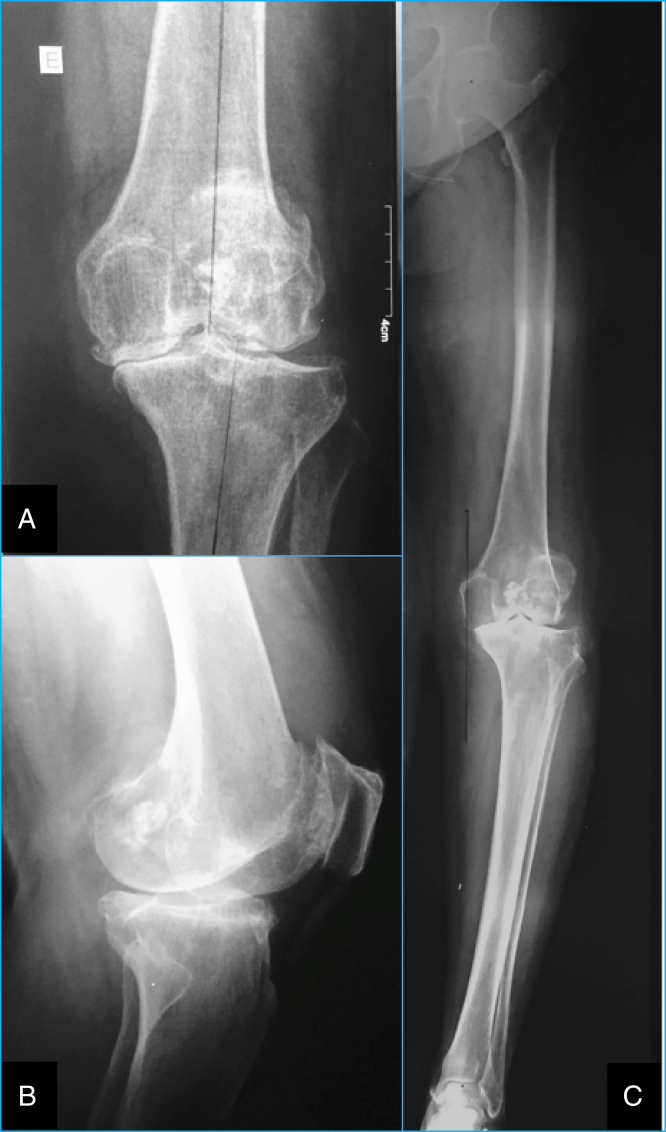
Complementary tests consisting of conventional knee radiograph (CKR) and PLLR indicated advanced arthrosis (Alhback type 4), with a varus deformity of the left knee (Fig. 2).
Fig. 2.
Pre-operative exams. A, anteroposterior conventional knee radiograph; B, lateral conventional knee radiograph; C, panoramic view of the left lower limb.
Source: The author.
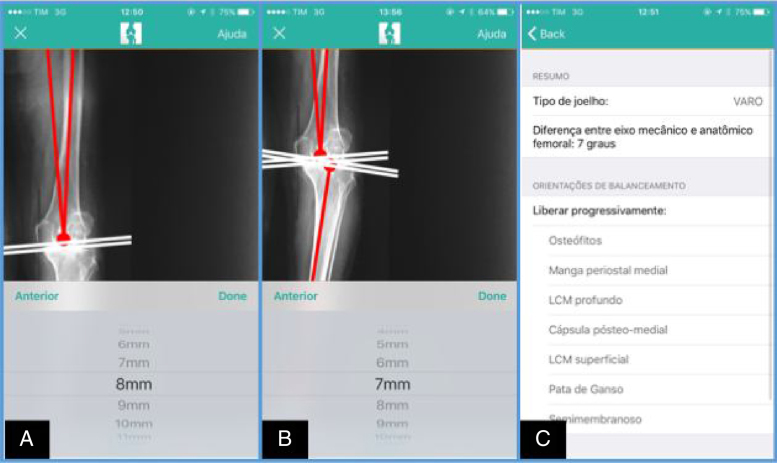
The surgical planning followed a protocol for the identification of the anatomical femoral axis (AFA), the mechanical femoral axis (MFA), the mechanical tibial axis (MTA), and the anatomical-mechanical femoral angle assessment (AMFA) using the TKA App by marking points (Fig. 3). After the bone cuts were planned, a cut line was positioned perpendicularly to the MFA and the MTA, by adjusting a millimeter scrollbar presented by the application. Thus, it was decided to resect 8 mm of the distal femur and 7 mm of the lateral plateau, preserving the bone stock in the medial plateau as much as possible (Fig. 4). The measured AMFA was 7°. As a security measure, the manual form of planning was used to confirm the planning made using the application (Fig. 5). This application was shown to be useful in the planning of this case, as it was able to accurately measure the AMFA.7
Fig. 3.
Preoperative planning through the TKA App. A, AFA and MFA calculation; B, calculation of the MTA of the AMFA; C, automatic AMFA calculation.
Source: The author.
Fig. 4.
Bone cut planning through the TKA App. A, femoral cut line (positioned at 8 mm, corresponding to the thickness of the femoral implant used); B, tibial bone cut line (showing preservation of the medial bone stock and utilization of 7 mm from the highest point of the lateral tibial plateau); C, planning summary.
Source: The author.
Fig. 5.

Safety control. Planning done in a conventional, manual manner.
Source: The author.
During surgery, the preoperative planning was respected, following a cutting angle of the distal femur of 7°. Initially, a tibial bone cut was made; the balance between the gap in extension and in flexion of 90° was observed. An asymmetrical trapezoidal gap was identified, with medial constriction and lateral opening of 12 mm, both in 90° flexion and extension. The medial structures (osteophytes and medial periosteal sleeve) were released. Subsequently, the distal femur was cut at an external rotation angle of 4°, aiming at transforming the gap, initially trapezoidal, into a rectangular, symmetrical gap. The other femoral cuts were then performed. The balance was tested again at 90° flexion and extension, which was symmetrical and rectangular. The cemented prosthetic components (femur, 4; tibia, 4; polyethylene, 12; patella, 33) were then attached (Fig. 6).
Fig. 6.

Immediate postoperative radiographic control. CKR.
Source: The author.
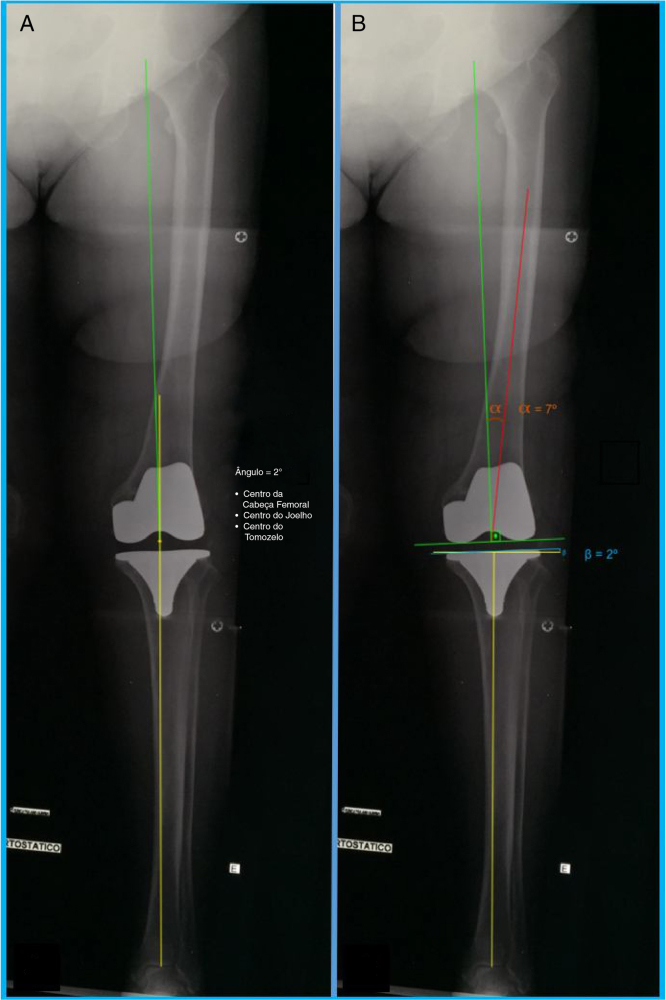
The patient evolved with improvement of pain complaints in the early postoperative period and an increase in the range of motion (0–120°). Walking was initiated on the third postoperative day, at which time a postoperative control PLLR showed satisfactory lower limb mechanical alignment (ACFKA = 2°; Fig. 7).
Fig. 7.
Postoperative PLLR. A, ACFKA measurement, showing satisfactory alignment (2 degrees); B, AMFA reproduced according to the planning (7°) and femoral component positioned perpendicular to the MFA.
Source: The author.
Discussion
PLLR is an adequate imaging exam for the planning of TKAs, as it allows the identification of extra-articular deformities and the estimation of the AFA, MFA, MTA, and AMFA.8
A counterpoint to the theory of mechanical alignment has emerged over the last few years: the kinematic alignment theory. Based on the restoration of the native anatomy of the knee, this theory advocates the reproduction of a small tibial varus and respects the three-dimensional femoral anatomy in its three axes.9, 10 However, this theory has complex reproducibility and its execution is still being refined. In turn, the literature offers broad support for the adoption of mechanical alignment of prosthetic components, and its execution has been evaluated by studies over decades, showing good reproducibility and good implant survival when the principles recommended in the neutral mechanical alignment are respected.1, 11
Manual TKA planning demands the use of not-so-portable tools: 50 cm ruler, 2 B pencil, rubber, goniometer, and protractor. Furthermore, it requires the surgeon to be familiar with a rational planning methodology. Planning with an application can simplify the surgeons’ routine, directing him to a reliable methodology supported by the literature.
A systematic review of applications in the surgical medical field demonstrates the usefulness of these applications in pre, intra, and transoperative contexts.12 When this technology is applied in education (m-learning), it can contribute to the consolidation of theories.13 Nonetheless, studies with a higher level of evidence are needed to further analyze the impact of the generalized adoption of this type of tool.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Santa Casa da Misericórdia de Fortaleza, Fortaleza, CE, Brazil.
References
- 1.Donaldson J., Joyner J., Tudor F. Current controversies of alignment in total knee replacements. Open Orthop J. 2015;9:489–494. doi: 10.2174/1874325001509010489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molicnik A., Naranda J., Dolinar D. Patient-matched instruments versus standard instrumentation in total knee arthroplasty: a prospective randomized study. Wien Klin Wochenschr. 2015;127(Suppl 5):S235–S240. doi: 10.1007/s00508-015-0703-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daniilidis K., Tibesku C.O. Frontal plane alignment after total knee arthroplasty using patient-specific instruments. Int Orthop. 2013;37(1):45–50. doi: 10.1007/s00264-012-1732-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deakin A.H., Sarungi M. A comparison of variable angle versus fixed angle distal femoral resection in primary total knee arthroplasty. J Arthroplasty. 2014;29(6):1133–1137. doi: 10.1016/j.arth.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 5.Jeffery R.S., Morris R.W., Denham R.A. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 6.Babazadeh S., Dowsey M.M., Bingham R.J., Ek E.T., Stoney J.D., Choong P.F. The long leg radiograph is a reliable method of assessing alignment when compared to computer-assisted navigation and computer tomography. Knee. 2013;20(4):242–249. doi: 10.1016/j.knee.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 7.Nogueira J.B.S., Carvalho A.C.G., Barros Filho E.M., Araújo L.H.C., Bezerra M.J.C., Demange M.K. Evaluation of utility and accuracy of a mobile application for planning total knee arthroplasties. Rev Bras Ortop. 2017 doi: 10.1016/j.rboe.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajgopal A., Vasdev A., Dahiya V., Tyagi V.C., Gupta H. Total knee arthroplasty in extra articular deformities: a series of 36 knees. Indian J Orthop. 2013;47(1):35–39. doi: 10.4103/0019-5413.106893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howell S.M., Papadopoulos S., Kuznik K.T., Hull M.L. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sport Traumatol Arthrosc. 2013;21(10):2271–2280. doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- 10.Dossett H.G., Estrada N.A., Swartz G.J., LeFevre G.W., Kwasman B.G. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J [Internet] 2014;96-B(7):907–913. doi: 10.1302/0301-620X.96B7.32812. [DOI] [PubMed] [Google Scholar]
- 11.Toliopoulos P., LeBlanc M.A., Hutt J., Lavigne M., Desmeules F., Vendittoli P.-A. Anatomic mechanically aligned total knee arthroplasty for unicompartmental knee arthroplasty revision. Open Orthop J. 2016;10(1):357–363. doi: 10.2174/1874325001610010357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mobasheri M.H., Johnston M., Syed U.M., King D., Darzi A. The uses of smartphones and tablet devices in surgery: a systematic review of the literature. Surgery. 2015;158(5):1352–1371. doi: 10.1016/j.surg.2015.03.029. [DOI] [PubMed] [Google Scholar]
- 13.Marçal E., Andrade R., Rios R. Aprendizagem utilizando dispositivos móveis com sistemas de realidade virtual. RENOTE Rev Novas Tecnol Educ. 2005;3:1–11. Available from: http://seer.ufrgs.br/renote/article/view/13824. [Google Scholar]