Abstract
Background:
Although isolated posterior cruciate ligament reconstruction (PCLR) has become a more frequently performed procedure, reports of functional outcomes and return-to-sport (RTS) rates to support its use are still limited.
Purpose:
To systematically review the literature to determine the rates of RTS and the functional outcomes of patients after isolated PCLR.
Study Design:
Systematic review: Level of evidence, 4.
Methods:
Two reviewers independently searched 5 databases for patient-based clinical studies with a minimum 2-year follow-up that analyzed functional outcome and RTS following isolated PCLR. Studies with multiligament knee reconstruction were excluded. Risk of bias was performed with a modified Downs and Black checklist. The primary outcomes were Tegner and Lysholm scores, rates of RTS, and International Knee Documentation Committee (IKDC) subjective scores. Secondary outcomes were IKDC objective scores, instrumented knee laxity assessment, and Telos radiographic analysis. Where feasible, these data were pooled via a random effects meta-analysis model.
Results:
Of the 240 titles identified, 14 studies were included. The median time from injury to surgery was 10.6 months (range, 6 weeks–21 years). The pooled mean postoperative Tegner and Lysholm scores were 5.7 (95% CI, 5.4-6.0) and 87.8 (95% CI, 85.6-90.0), respectively, following isolated PCLR; the pooled effect size between pre- and postoperative values was 2.8 (95% CI, 1.6-4.0) and 3.7 (95% CI, 2.6-4.9), respectively. An RTS rate of 44% (95% CI, 23%-66%) was identified. IKDC subjective scores improved to a pooled mean of 73.5 (95% CI, 62.8-84.1), with an effect size of 3.0 (95% CI, 0.4-5.6). The proportion of patients with postoperative IKDC objective scores of grade A/B was 82%. The pooled postoperative KT-1000/KT-2000 side-to-side difference was 3.4 mm (95% CI, 2.5-4.3 mm), with an effect size of 2.8 (95% CI, 1.1-4.5). The pooled postoperative Telos side-to-side difference measurement was 3.5 mm (95% CI, 2.8-4.3 mm), with an effect size of 3.9 (95% CI, 3.3-4.5).
Conclusion:
The results of this review demonstrate that while isolated PCLR results in a significant improvement in functional outcome scores and improved knee laxity, there is a low rate of return to preinjury level of sport. The prolonged period from injury to surgery might reduce functional improvement and RTS following reconstruction. Therefore, comparison of the outcomes of isolated PCLR and nonoperative treatment is impracticable owing to the potential for selection bias.
Keywords: isolated posterior cruciate ligament reconstruction, return to sport, systematic review, functional outcomes, ligament laxity
There is growing interest in the reconstruction of isolated posterior cruciate ligament (PCL) injuries. Traditionally, these injuries have been treated nonoperatively with good functional outcomes in the short term and with high return-to-sport (RTS) rates, at least among elite athletes.1 However, long-term studies have demonstrated that chronic high-grade PCL-deficient knees have a high incidence of articular cartilage degeneration, especially in the medial and patellofemoral compartments, owing to the posterior subluxation of the tibia.5,14,28,47 As such, the principle of isolated PCL reconstruction (PCLR) to prevent further posterior instability and subsequent chondral and meniscal injury is gaining favor.19,23 Nevertheless, PCLR is a technically demanding procedure and is not without risk of complications. Therefore, its use needs to be supported by evidence of clinical and functional benefit and translate to a high rate of RTS when performed in athletes.
Many surgical options have been described for reconstruction of the PCL-deficient knee. Most PCLRs are performed in the setting of multiligament injury. However, with improved arthroscopic instruments and techniques, a greater number of isolated PCLRs are being performed.10 In a comparative cohort study, Owesen et al38 determined that patients undergoing PCLR could expect the same improvements in patient-reported outcome scores as patients undergoing anterior cruciate ligament (ACL) reconstruction. Although the improvement is the same, patients with PCL deficiency who are undergoing PCLR have, on average, a lower preoperative score and, therefore, a lower final score when compared with patients undergoing ACL reconstruction.
Much of the literature has focused on biomechanical and functional outcomes when comparing various PCLR techniques.7,12,22,31,41,48 However, there is a growing body of information regarding patient function following isolated PCLR, including whether patients can expect RTS following surgery. The aim of this study was to systematically review and synthesize the literature to determine the functional outcome and rate of RTS and activity following isolated PCLR.
Methods
The study was performed as a systematic review of the current literature following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines.32
Search Criteria
A search for relevant studies was conducted by 2 independent reviewers (R.D. and J.C.) on October 1, 2017, through the electronic databases CINAHL, Cochrane Library, Embase, Medline, and PubMed. A search was conducted with the following 2 concepts, combined with the operator “AND,” to obtain the final yield of results.
Concept 1: (“Posterior Cruciate Ligament” OR “PCL”) AND (“reconstruction”)
Concept 2: “outcomes” AND “sport”
Search terms, where possible, were mapped to relevant MeSH terms and subject headings. A supplementary search of the reference list of relevant articles was also conducted. Publication details for the search results were uploaded to EndNote X7.4 (Thomson Reuters).
Selection Criteria
The following inclusion criteria were applied to the final yield:
Isolated PCLR
All techniques and graft types
Postoperative functional activity outcome scores or quantitative RTS scores
Minimum 2-year follow-up
Full texts available in the English language
The exclusion criteria applied for article selection were as follows:
Articles dealing exclusively with multiligament reconstruction. For articles featuring comparative groups of isolated PCLR and multiligament reconstruction, only the data for the isolated PCLR cohort were included
Reports on guidelines, technique articles, reviews, or systematic reviews
Articles for which the full text was unable to be sourced. Contact with authors was attempted, and if this was unsuccessful, the article was excluded
The title and abstract of each study were initially reviewed per the selection criteria. In the cases where it was not clear from the review of the title and abstract whether a study was appropriate for inclusion, the full-text article was examined. Two reviewers (R.D. and J.C.) applied the selection criteria independently. Consensus was used to resolve any disagreements between reviewers, with a third reviewer (B.M.D.) consulted if consensus could not be reached.
Quality Appraisal
The quality of the article was appraised with the modified Downs and Black scoring system, which is appropriate for use in cohort study designs.9 This system uses 15 categories to determine the methodological quality of a study. Items are scored 0 or 1, except for 1 item in the Reporting subscale (clearly described distributions of principal confounders), which is scored from 0 to 2. A total score ≤9 is categorized as low quality, 10 and 11 as moderate quality, and ≥12 as high quality, with a maximum possible score of 16.33,34 Any disagreements regarding the methodological quality assessments were discussed with a consensus achieved by the 2 reviewers. Each article had a level of evidence assigned per the 2011 guidelines of the Oxford Centre for Evidence-Based Medicine.15
Data Extraction
The 2 independent reviewers used a data extraction form specifically designed for this review. The primary outcomes of interest were Tegner scores, Lysholm scores, RTS rates, and International Knee Documentation Committee (IKDC) subjective scores. The secondary outcomes included IKDC objective scores, instrumented laxity assessment (KT-1000, KT-2000, and nonspecific laxity arthrometer), and Telos radiographic analysis. Instrumented laxity and Telos data were collected as side-to-side difference (SSD) measured in millimeters. The descriptive data extracted are outlined in Table 1.
TABLE 1.
Summary of Extracted Dataa
| Primary Outcome | Secondary Outcome | |||
|---|---|---|---|---|
| Study Details | Surgery Details | Functional | Patient Reported | Objective |
| Type of study | Time injury to surgery | Tegner | IKDC subjective | IKDC objective |
| No. of patients | Type of PCLR | Lysholm | KT-1000/KT-2000 | |
| Study period | Rehabilitation | Return to sport | Telos | |
| Country | ||||
| Follow-up | ||||
aIKDC, International Knee Documentation Committee; PCLR, posterior cruciate ligament reconstruction.
Data Synthesis and Analysis
A meta-analysis was performed of the primary and secondary outcome measures when these data were available in the included studies. Summary meta-analysis (based on outcome means and SE values) and proportional meta-analysis (based on frequency values) were conducted with StatsDirect statistical software (StatsDirect Ltd). Where pre- and postsurgery data were available, an effect size meta-analysis was also performed. In all cases, a random effects model was used, and a P value <.05 was considered statistically significant. Data were displayed in several comparative forest plots, with a combined score also calculated.
Results
Search Results
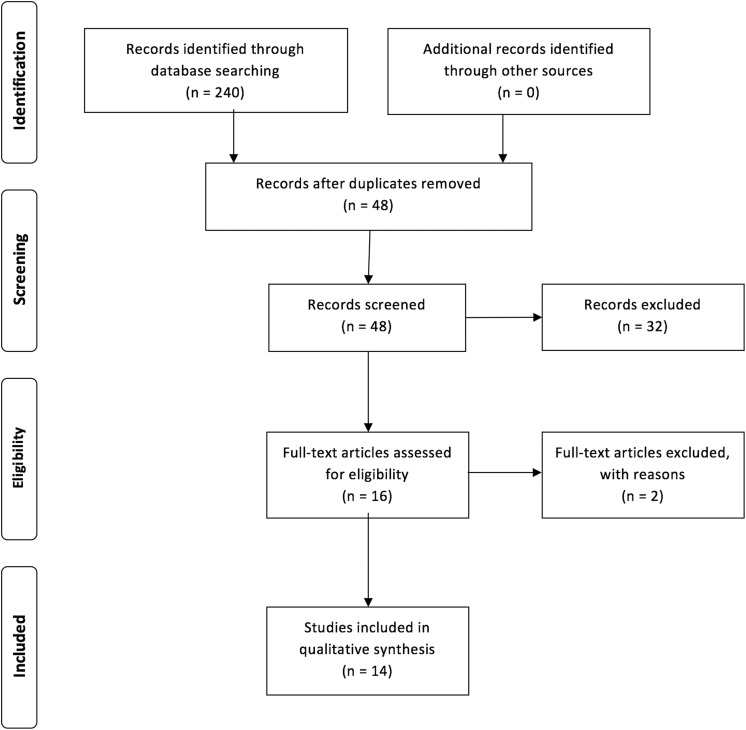
The database search resulted in 240 records being identified. Following removal of duplicates and title screening, 192 articles were excluded (Figure 1). The abstracts for the remaining 48 articles were reviewed, and 32 were removed for not meeting inclusion criteria. Full-text versions were reviewed for the remaining 16 articles. Two articles were excluded for their full text being printed in Mandarin despite displaying English abstracts.27,51 This resulted in 14 articles being included for analysis (Table 2).§
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flow diagram.
TABLE 2.
PCL Studies Outcomesa
| Study | LOE | Design | N | Country | Study Period | Injury-Surgery, mo, Mean ± SD (Range) | Type of PCLR | Rehabilitation | Follow- up, Mean (Range) | Outcome Measures | Recommendation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Boutefnouchet4 | 4 | CS | 15 | UK | Unknown | 15.5 (2-74) | Hamstring 4-stand SB transtibial | CPM 12 h, FWB 24 h, no brace + FROM by 2-3 wk, jog 3 mo, light sport 6 mo, contact sport 9-12 mo | 4.1 y (1-9) | Lysholm, Tegner, IKDC, KT-2000 | Very good restoration of knee kinematics and function with a majority of patients returned to preinjury level sport. |
| Chan6 | 4 | CS | 20 | Taiwan | 1999-2001 | 4 (3-12) | Hamstring 4-strand SB transtibial | Functional brace PWB 1 wk, FWB 6 wk, FROM 8 wk, normal activity 3 mo, light sport 6 mo, full sport 9 mo | 40 mo (36-50) | Lysholm, Tegner, IKDC, thigh muscle assessment, radiographic assessment, KT-1000 | Satisfactory functional outcomes with significant Tegner improvement post surgery. No RTS data. |
| Garofalo13 | 4 | CS | 15 | Italy | Unknown | 10.6 ± 2.5 | Patellar tendon–bone and semitendinosus autograft—DB transtibial | Extension 3 wk, PWB 6 wk, FWB 8 wk, 0°-70° ROM 4 wk, RTS 9 mo | 3.2 y (2-5) | IKDC, IKDC 2000, Lysholm, Tegner, HSS | Significant improvement in knee scores from DB PCLR, but no patients resumed preinjury level of sporting activities. |
| Lee24 | 4 | CS | 45 | Korea | 2006-2011 | 9.4 ± 3.5 | 45 patients: transtibial SB allograft remnant sparing | Extension 12 wk, TWB 4 wk, FWB 6 wk, light running 12 wk, RTS 6 mo | 48.2 ± 16.2 mo | Lysholm, Tegner, IKDC subjective, radiography MRI (n = 34), second-look scope (n = 36), KT-2000, Biodex proprioception | Transtibial remnant-preserving PCLR results in satisfactory clinical, radiologic, and morphologic outcomes. No RTS data. |
| Li25 | 3 | CC | 37 | China | 2005-2009 | Group 1: 8.9 ± 2.4 Group 2: 9.3 ± 2.9 | Group 1: 4-strand hamstring SB transtibial Group 2: allograft tibialis anterior tendon transtibial | Extension 4 wk, 12 wk PWB, normal activities 3 mo, light sport 6 mo, full preinjury sport 9-12 mo | Group 1: 2.3 y Group 2: 2.4 y | Lysholm, Tegner, IKDC rating, knee laxity arthrometer | Significant clinical improvements with both hamstring and tibialis anterior PCLR, no significant difference between graft types. No RTS data. |
| MacGillivray29 | 3 | CC | 20 | USA | 1980-1997 | Not stated | Group 1: transtibial (autologous BPTB, allograft BPTB, allograft Achilles) Group 2: tibial inlay (autologous BPTB, allograft BPTB) | Extension 4-6 wk, TWB 4 wk, PWB 2 wk, full activities 9-12 mo | Group 1: 6.3 y (2.4-15) Group 2: 4.7 y (2-7) | Tegner, Lysholm, AAOS knee scale, KT-1000 | Significant clinical improvement with PCLR. Majority of patients did not RTS. No significant difference between PCLR techniques. |
| Mariani30 | 4 | CS | 24 | Italy | 1991-1994 | 32 (11-192) | Arthroscopic BPTB transtibial PCLR | First 9 patients: ROM 1 wk, NWB 6 wk Last 15 patients: FWB PROM day 2, bicycle 4 wk, swim 8 wk, run 12 wk, RTS 6 mo | 26.5 mo (24-53) | Lysholm, Tegner, IKDC, KT-2000 | Chronic PCLR significantly results in significant activity improvement with 50% RTS rate. |
| Mygind-Klavsen35 | 3 | CS | 77 | Denmark | 2002-2010 | Not stated | Arthroscopic transtibial hamstring graft DB | NWB 6 wk, HKB 8 wk with gradual ROM | 5.9 y (3.1-9.7) | IKDC, KOOS, Tegner, KT-1000 | PCLR in isolated PCL injury knees have better outcome scores vs PCLR in multiligamentous injuries with a mean sports and recreation KOOS score of 56. |
| Noh36 | 4 | CS | 28 | Korea | 2010-2013 | 2 (1.6-16.5) | Achilles allograft looped transtibial tunnel remnant preserved | PWB day 2, FWB 2 wk, extension 5 wk, light exercise 3 mo, noncontact sport 9 mo, RTS 1 y | 27.7 ± 4.8 mo | Lysholm, IKDC, Tegner | Multiple-looping PCLR has satisfactory clinical outcomes. No RTS data. |
| Osti37 | 4 | CS | 39 | Austria | 2008-2012 | 20.7 ± 45.6 (0.4-244) | Arthroscopic tibial inlay quads tendon SB | PWB 4 wk, PCL brace with 50° flexion 4 wk, RTS 9-12 mo | 45.6 ± 21.6 mo | Lysholm, IKDC, Tegner, VAS, KOOS | Beneficial subjective and objective outcomes in the medium term with a mean sports and recreation KOOS score of 65.35. |
| Song46 | 3 | CC | 66 | Korea | 1990-2001 | 12.2 | Group 1: transtibial hamstring SB Group 2: tibial inlay BPTB | Extension 3 wk, PWB at 8 wk, FWB at 12 wk, low-impact sports 6 mo, contact sports 9 mo | Group 1: 139 ± 27.4 mo Group 2: 144 ± 26.7 mo | Lysholm, IKDC, Tegner, return to preinjury sports, postdraw, laxity Telos, OA development | Significant clinical improvement in both techniques with significant difference. No significant difference in RTS. |
| Yang52 | 2 | CC | 58 | Korea | 2001-2009 | Group 1 = 9.7 mo Group 2 = 9.2 mo | Group 1: transtibial SB mixed tibialis anterior autologous hamstring remnant preserved Group 2: transtibial SB allograft Achilles tendon remnant preserved | Extension 4 wk, PWB 4 wk, FWB 6 wk, return to full activities 9-12 mo | Group 1: 60 ± 21 mo Group 2: 58 ± 18 mo | Lysholm, Tegner, IKDC, Telos, second-look scope: group 1 66.7%, group 2 75% | Satisfactory clinical outcomes in both techniques. Higher intraoperative complication rate with Achilles tendon graft use. No RTS data. |
| Yoon53 | 2 | RCT | 58 | Korea | 2007-2007 | Group 1 = 37 (3-259) Group 2 = 35 (3-131) | Group 1: transtibial SB allograft Achilles remnant preserved Group 2: transtibial DB | Extension NWB 3 wk, FWB 6 wk, return to sports 1 y | Group 1: 31 mo (24-42) Group 2: 33 mo (24-43) | ROM, posterior stress radiography, Tegner, Lysholm, IKDC | DB PCLR resulted in better objective posterior stability than SB PCLR but no difference in clinical outcomes. Both techniques show significant Tegner improvement. No RTS data. |
| Zayni54 | 4 | CS | 21 | France | 2005-2008 | 28 (0.75-95) | SB transtibial autologous hamstring | Extension 45 d, RTS 7 mo | 29 mo (12-48) | IKDC, Tegner, Lysholm, Telos | PCLR resulted in significant improvements in clinical outcomes. A high number of patients had an RTS. Higher preinjury function resulted in better outcomes. |
aAAOS, American Academy of Orthopaedic Surgeons; BPTB, bone–patellar tendon–bone; CC, case-control study; CPM, continuous passive motion; CS, case series; DB, double bundle; FROM, functional range of motion; FWB, full weightbearing; HKB, hinged knee brace; HSS, Hospital for Special Surgery; IKDC, International Knee Documentation Committee; Injury-Surgery, time from injury to surgery; KOOS, Knee injury and Osteoarthritis Outcome Score; LOE, Level of evidence; MRI, magnetic resonance imaging; NWB, nonweightbearing; OA, osteoarthritis; PCL, posterior cruciate ligament; PCLR, posterior cruciate ligament reconstruction; PWB, partial weightbearing; RCT, randomized controlled trial; ROM, range of motion; RTS, return to sport; SB, single bundle; TWB, touch weightbearing; VAS, visual analog scale.
Quality Assessment
Of the 14 studies included in this review, there was 1 randomized controlled trial, 3 case-control studies, and 10 case series. The Downs and Black scores for the included articles ranged from 9 to 12 out of a maximum of 16 (Table 3). Only 1 study was considered high quality, with a score of 12.25 Eleven studies were deemed moderate quality,∥ while 2 studies were rated low quality.6,37 No studies provided information on the possibility of selection bias, with only 3 studies including a blinding process.
TABLE 3.
Quality Assessment Tool: Modified Downs and Blacka
| Study | Aim | Patient | Sample | Bias | Cmpr | Outcm | Valid | Blind | Find | Rand | Stat | Cnfd | Adj | Smpl Calc | Power | Total | Quality |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Li25 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 12 | High |
| Boutefnouchet4 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 2 | 1 | 0 | 0 | 10 | Mod |
| Garofalo13 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Lee24 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 10 | Mod |
| MacGillivray29 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Mariani30 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Mygind-Klavsen35 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Noh36 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 10 | Mod |
| Song46 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Yang52 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 11 | Mod |
| Yoon53 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 2 | 1 | 0 | 0 | 11 | Mod |
| Zayni54 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 10 | Mod |
| Chan6 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 9 | Low |
| Osti37 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | Low |
aScoring system: Adj, adequate adjustment for confounding; Aim, aim of study; Bias, selection bias present; Blind, attempt to blind measurers; Cmpr, comparison group identified; Cnfd, clearly described distributions of principle confounders (score, 0-2); Find, main findings of study; Outcm, clearly described outcomes; Patient, patient characteristics; Power, sufficient power in study; Rand, estimates of random variability; Sample, sample is representative; Smpl calc, reported sample size calculation; Stat, statistical tests used; Valid, measures are valid and reliable.
bQuality: ≥12, high; 10 or 11, moderate (mod); ≤9, low.
Demographic Characteristics
The 14 included studies reported on 523 patients (392 male, 131 female). The median patient age at surgery was 30.2 years (interquartile range, 5.4 years). There was a wide range in the time from injury to surgery (6 weeks–21 years) with a median time of 10.6 months for the 13 studies including these data.¶ The mean follow-up was 54.2 months.
Primary Outcomes
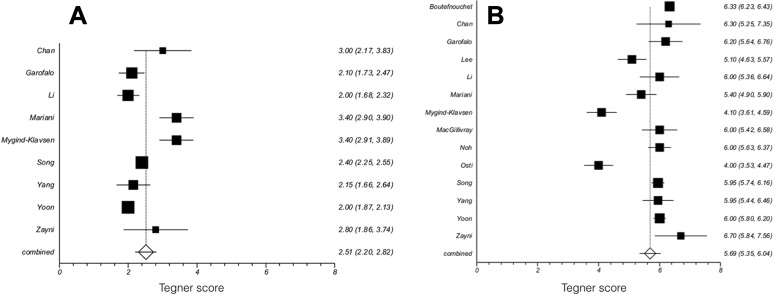
Tegner Score
Figure 2 demonstrates the pre- and postoperative Tegner scores. Preoperative Tegner scores were available for 9 studies, while all 14 included studies presented postoperative Tegner scores. The preoperative Tegner scores for Lee et al24 were not included because they were combined with the scores of patients who had undergone PCLR and posterolateral corner reconstruction, while the postoperative scores detailed PCLR in isolation. The pooled mean preoperative Tegner score was 2.5 (95% CI, 2.2-2.8). The pooled mean postoperative Tegner score was 5.7 (95% CI, 5.4-6.0). The pooled effect size between pre- and postoperative scores was 2.8 (95% CI, 1.6-4.0).
Figure 2.
Forest box plots displaying the mean and combined (A) preoperative and (B) postoperative Tegner scores with 95% CIs.
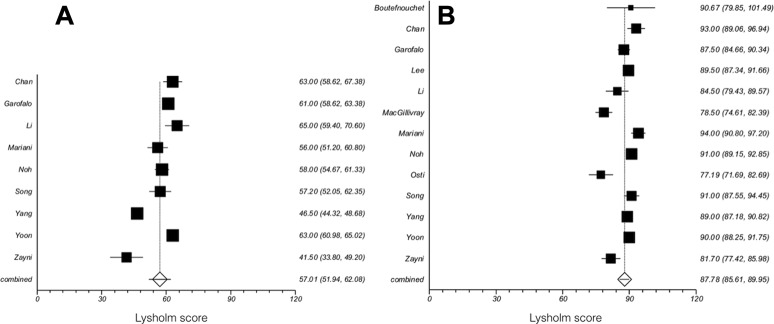
Lysholm Score
Figure 3 demonstrates the pre- and postoperative Lysholm scores. Nine studies presented preoperative Lysholm scores, and 13 studies provided postoperative Lysholm scores. The preoperative Lysholm scores for Lee et al24 were not included because they were combined with the scores of patients who had undergone PCLR and posterolateral corner reconstruction, while the postoperative scores detailed PCLR in isolation. The pooled mean preoperative Lysholm score was 57.0 (95% CI, 51.9-62.1). The pooled mean postoperative Lysholm score was 87.8 (95% CI, 85.6-90.0). The pooled effect size between pre- and postoperative scores was 3.7 (95% CI, 2.6-4.9).
Figure 3.
Forest box plots displaying the mean and combined (A) preoperative and (B) postoperative Lysholm scores with 95% CIs.
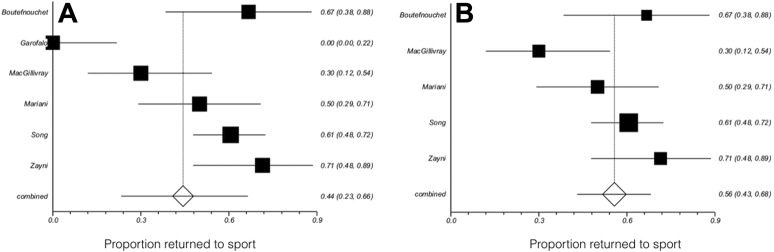
Return to Sport
Figure 4A demonstrates the return to preinjury level of sport following isolated PCLR. Only 6 of the 14 included studies provided quantitative RTS data. The pooled return to preinjury level sport rate was 44% (95% CI, 23%-66%). However, Garofalo et al13 reported that none of their 15 patients returned to preinjury sporting level following isolated PCLR. If this study is removed, the percentage of variation (I 2) across the studies, which is due to heterogeneity rather than chance, drops from 87.3% to 55.6% (Figure 4B).16,17 It also results in a mean RTS level of 56% (95% CI, 43%-66%). Song et al,46 in a study of 66 patients, reported no difference in return to preinjury sport between patients who had a transtibial PCLR (58.3%) and those who had a tibial inlay PCLR (63.6%). In a series of 21 patients, Zayni et al54 found that 95.2% of patients were performing pivot- and contact-type sport activities prior to injury, but only 71.5% returned to these types of sports following PCLR.
Figure 4.
Return-to-sport proportion with 95% CIs: (A) for 6 studies and (B) with removal of the Garofalo et al13 study, which reduces the percentage of variation (I 2) from 87.3% to 55.6%.
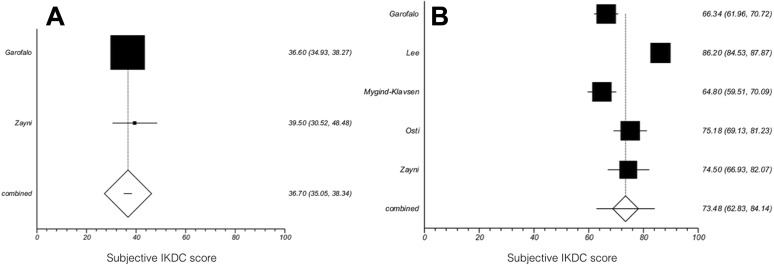
IKDC Subjective
Figure 5 demonstrates the pre- and postoperative IKDC subjective scores. Two studies provided preoperative IKDC subjective scores, and 5 provided postoperative scores. The mean preoperative IKDC subjective score was 36.7 (95% CI, 35.1-38.3). The mean postoperative IKDC subjective score was 73.5 (95% CI, 62.8-84.1). The pooled effect size between pre- and postoperative scores was 3.0 (95% CI, 0.4-5.6).
Figure 5.
Mean subjective International Knee Documentation Committee (IKDC) scores with 95% CIs: (A) preoperative and (B) postoperative.
Secondary Outcomes
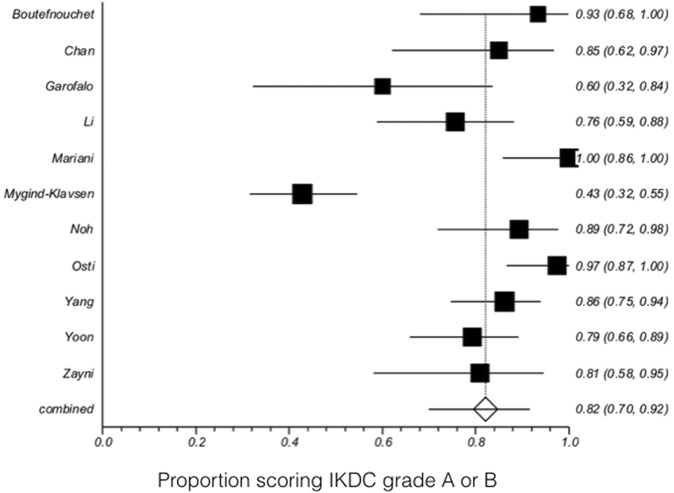
IKDC Objective
Figure 6 demonstrates the postoperative IKDC objective scores, as provided by 11 studies. IKDC objective scores were analyzed as the proportion of the cohort classified as grade A and B postoperatively. The mean postoperative grade A and B proportion was 82% (95% CI, 71%-91%).
Figure 6.
Postoperative objective International Knee Documentation Committee (IKDC) scores with proportion scoring grade A or B with 95% CIs.
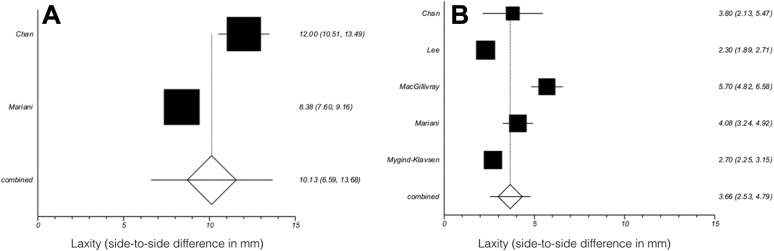
KT-1000 and KT-2000
Figure 7 demonstrates the pre- and postoperative KT-1000/KT-2000 measurements of SSD in posterior knee laxity. KT-1000 and KT-2000 scores were combined for meta-analysis. Two studies presented preoperative KT-1000/KT-2000 SSD measurements, whereas 5 provided postoperative measurements. The pooled mean preoperative KT-1000/KT-2000 SSD measurement was 9.1 mm (95% CI, 6.4-11.8 mm), and the pooled mean postoperative KT-1000/KT-2000 SSD measurement was 3.4 mm (95% CI, 2.5-4.3 mm). The pooled effect size between pre- and postoperative measurements was 2.8 (95% CI, 1.1-4.5).
Figure 7.
Mean KT-1000/KT-2000 side-to-side difference measurements with 95% CIs: (A) preoperative and (B) postoperative.
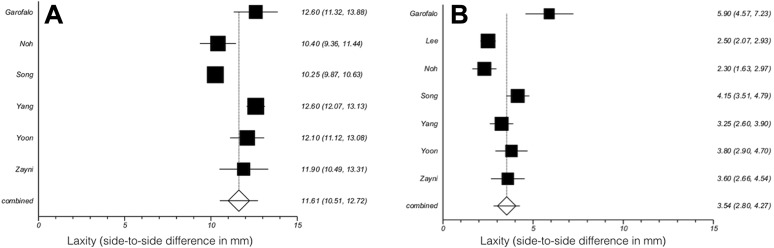
Telos
Figure 8 demonstrates the pre- and postoperative Telos SSD measurements. Six studies presented preoperative Telos SSD measurements, whereas 7 provided postoperative measurements. The pooled mean preoperative Telos SSD measurement was 11.7 mm (95% CI, 10.8-12.6 mm). The pooled mean postoperative Telos SSD measurement was 3.5 mm (95% CI, 2.8-4.3 mm). The pooled effect size between pre- and postoperative measurements was 3.9 (95% CI, 3.3-4.5).
Figure 8.
Mean Telos side-to-side difference measurements with 95% CIs: (A) preoperative and (B) postoperative.
Discussion
The main finding of this systematic review was that isolated PCLR resulted in a significant improvement in functional scores and improved knee stability. Specifically, a statistical difference was found between pre- and postoperative Tegner, Lysholm, and IKDC objective scores, as well as for instrumented knee laxity measurements. However, this translated to only modest levels of activity and, at best, fair RTS rates. These results are important in counseling patients about realistic expectations prior to undergoing PCLR.
There are conflicting results regarding the effectiveness of nonoperative treatment of isolated PCL injuries. Although some studies have reported that patients with PCL deficiency can compensate and function well,18,20 others suggest that positive early results deteriorate with time and lead to progressive dysfunction and pain.5,20 Nonetheless, most clinicians recommend nonoperative treatment as the first choice of treatment for patients with an isolated PCL injury.3 Perhaps because of this treatment strategy, PCLR is typically reserved for those patients who fail nonoperative measures. As such, a direct comparison of the outcomes between isolated PCLR and nonoperative management is fraught with difficulty, as there is likely to be a high degree of selection bias.
The effect of using nonoperative treatment as the initial approach is emphasized in a study by Owesen et al,38 which analyzed data from the Norwegian Knee Ligament Registry. The authors found a significantly increased time from injury to surgery for PCLR versus ACL reconstruction (median, 21.5 vs 8 months).2 The study also revealed that patients undergoing PCLR had lower preoperative Knee injury and Osteoarthritis Outcome Scores (KOOS) and therefore, despite similar postoperative improvements, lower final scores.38 In the current review, the median time from injury to surgery was 10.6 months. Also, in keeping with the findings of Owesen et al,38 the patients included in the meta-analysis had low presurgery functional levels, with mean Tegner and Lysholm scores of 2.5 and 57.0, respectively. Owesen et al suggested that because of prolonged reduction in preoperative functional capacity, patients may have reduced outcome expectations following surgery.38 In the current study, despite there being a significant improvement in Tegner scores following PCLR, the mean postsurgery score was only 5.7, potentially supporting this hypothesis; such a score equates to a patient being able to participate in heavy labor work, jog only for recreation, and competitively cycle and ski.49
Success of ligamentous reconstruction, rightly or wrongly, is often defined by the ability of patients to return to sporting activity. Overall, the reported RTS rates of nonoperative management of isolated PCLR are good to excellent. In a prospective study of 46 consecutive elite athletes with nonoperatively managed isolated high-grade PCL injuries, Agolley et al1 reported an RTS rate of 91.3% at 2 years, with 86.2% playing competitive sports at 5 years. Shino et al45 reported that 73% of 15 athletes returned to the same preinjury level of sport at 51 months following injury, while Fowler and Messieh11 reported a 100% rate of return to preinjury level of sport at 2.6 years among 13 acutely injured athletes. Finally, Shelbourne et al42—in a cohort of 133 patients with an isolated grade 1-2 PCL injury evaluated after a mean of 5.4 years—found that regardless of residual laxity, 50% had returned to the same level of sport or higher and 32% had returned at a lower level, while 16.5% did not return to the same sport and 1.5% did not play sport at all.
The current systematic review identified 6 studies with RTS rates ranging from 0% to 76%, and the results of the current meta-analysis indicated a combined RTS proportion of 44% following isolated PCLR. However, as mentioned earlier, it is difficult to compare these results directly with those from studies reporting on the outcome of nonoperative treatment of PCL injuries because those patients undergoing surgery had probably failed nonoperative management, as indicated by the long time from injury to surgery. Selection bias may also exist in some of the studies of nonoperative management that include elite athletes, who are likely to be highly motivated and invested in their recovery. However, 8 of the 14 studies included in this systematic review did not report RTS rates, which suggests that it was not paramount as an outcome measure or even as a realistic expectation of treatment.
In trying to analyze the differences in RTS rates following nonoperative and operative management of PCL injuries, it is important to consider whether it is possible to predict those who would benefit from PCLR at an early stage. One of the difficulties is the lack of an evidence base and consensus regarding what constitutes appropriate nonoperative treatment. The term conservative is often used to describe nonoperative treatment, and it suggests minimal intervention; however, in those studies reporting superior outcomes, the rehabilitation commenced rapidly and was far from minimal. The majority of these studies reported the use of active rehabilitation, including a PCL brace, and the focus on regaining range of motion, strength, and stability training.42 The rationale behind these methods is based on the potential of the PCL to heal, owing to its extrasynovial location.8 In a study of 46 athletes with grade 2-3 PCL injury, Agolley et al1 reported excellent functional outcomes at 5 years after patients underwent of a supervised rehabilitation program within 4 weeks of injury. The authors acknowledged that their findings represented the best-case scenario and may not reflect the findings in a normal population. Patients included in the study were all highly motivated and had access to excellent facilities and physical therapy support, which likely minimized the strain on the healing PCL, potentially allowing it to heal in a less elongated position. However, many of the studies that reported less favorable functional results did not describe the time at which nonoperative treatment commenced.39,43,44
In cases of PCL deficiency, kinematic studies have revealed that there is a change to not only posterior tibial translation but also tibial rotation,26 which has been reported to result in progressive articular degeneration, especially at the patellofemoral joint and in the medial compartment at flexion angles >70°.50 Given that one of the primary aims of PCLR is to reduce laxity, it is important to consider how effective surgery is in this regard. Our meta-analysis of instrumented laxity measurement with the KT-1000 or KT-2000 revealed an improvement of side-to-side laxity from 9.1 mm preoperatively to 3.4 mm postoperatively. Similarly, Telos stress radiography showed that posterior translations reduced from 11.7 mm preoperatively to 3.5 mm postoperatively. It is worth noting that all but one of the studies included in the instrumented laxity measurement meta-analysis used a single-bundle PCLR technique. However, despite the significant reduction in laxity, the final values are, according to IKDC classification, considered only “nearly normal.”40 It remains to be seen whether restoring the laxity of the knee to “nearly normal” results in decreased symptoms related to chondral damage or rates of osteoarthritis in the long term.
We acknowledge the limitations of this systematic review. Despite the focus on functional outcomes and the rate of RTS, there was limited information on these variables in the selected studies, particularly in relation to RTS. The quality of the articles was also limited, with only 2 high-quality articles and only 1 randomized controlled trial. All comparative articles, including the randomized controlled trial, focused on comparing various PCLR techniques rather than analyzing nonoperative versus operative techniques for isolated PCLR. This again suggests the need for further high-quality randomized controlled trials of isolated PCLR, especially studies focusing on function and RTS.
Conclusion
The results of this review demonstrate that while isolated PCLR results in a significant improvement in functional outcome scores and improved knee laxity, there is a low rate of return to the preinjury level of sport. With the increasing prevalence of isolated PCLR, it is important to understand the functional outcomes and RTS rates following surgery so as to provide patients with realistic expectations of treatment. The prolonged period from injury to surgery might reduce functional improvement and RTS following reconstruction. Therefore, comparison of the outcomes of isolated PCLR and nonoperative treatment is impracticable owing to the potential for selection bias.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Agolley D, Gabr A, Benjamin-Laing H, Haddad FS. Successful return to sports in athletes following non-operative management of acute isolated posterior cruciate ligament injuries: medium-term follow-up. Bone Joint J. 2017;99-B(6):774–778. [DOI] [PubMed] [Google Scholar]
- 2. Aroen A, Sivertsen EA, Owesen C, Engebretsen L, Granan LP. An isolated rupture of the posterior cruciate ligament results in reduced preoperative knee function in comparison with an anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1017–1022. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Musahl V, Cowan JB. Management of posterior cruciate ligament injuries: an evidence-based review. J Am Acad Orthop Surg. 2016;24(5):277–289. [DOI] [PubMed] [Google Scholar]
- 4. Boutefnouchet T, Bentayeb M, Qadri Q, Ali S. Long-term outcomes following single-bundle transtibial arthroscopic posterior cruciate ligament reconstruction. Int Orthop. 2013;37(2):337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boynton MD, Tietjens BR. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24(3):306–310. [DOI] [PubMed] [Google Scholar]
- 6. Chan YS, Yang SC, Chang CH, et al. Arthroscopic reconstruction of the posterior cruciate ligament with use of a quadruple hamstring tendon graft with 3- to 5-year follow-up. Arthroscopy. 2006;22(7):762–770. [DOI] [PubMed] [Google Scholar]
- 7. Cho DK, Rosa SP, Prestes GB, da Cunha LA, de Moura MF, Stieven Filho E. Anatomical study of the posterior cruciate ligament with the knee flexed at 90 degrees. Rev Bras Ortop. 2014;49(5):494–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cross MJ, Powell JF. Long-term followup of posterior cruciate ligament rupture: a study of 116 cases. Am J Sports Med. 1984;12(4):292–297. [DOI] [PubMed] [Google Scholar]
- 9. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eguchi A, Adachi N, Nakamae A, Usman MA, Deie M, Ochi M. Proprioceptive function after isolated single-bundle posterior cruciate ligament reconstruction with remnant preservation for chronic posterior cruciate ligament injuries. Orthop Traumatol Surg Res. 2014;100(3):303–308. [DOI] [PubMed] [Google Scholar]
- 11. Fowler PJ, Messieh SS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15(6):553–557. [DOI] [PubMed] [Google Scholar]
- 12. Gali JC, Esquerdo P, Almagro MA, da Silva PA. Radiographic study on the tibial insertion of the posterior cruciate ligament. Rev Bras Ortop. 2015;50(3):342–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garofalo R, Jolles BM, Moretti B, Siegrist O. Double-bundle transtibial posterior cruciate ligament reconstruction with a tendon-patellar bone-semitendinosus tendon autograft: clinical results with a minimum of 2 years’ follow-up. Arthroscopy. 2006;22(12):1331–1338. [DOI] [PubMed] [Google Scholar]
- 14. Gill TJ, DeFrate LE, Wang C, et al. The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med. 2004;32(1):109–115. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:D5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 17. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Inoue M, Yasuda K, Yamanaka M, Wada T, Kaneda K. Compensatory muscle activity in the posterior cruciate ligament–deficient knee during isokinetic knee motion. Am J Sports Med. 1998;26(5):710–714. [DOI] [PubMed] [Google Scholar]
- 19. Jackson WF, van der Tempel WM, Salmon LJ, Williams HA, Pinczewski LA. Endoscopically-assisted single-bundle posterior cruciate ligament reconstruction: results at minimum ten-year follow-up. J Bone Joint Surg Br. 2008;90(10):1328–1333. [DOI] [PubMed] [Google Scholar]
- 20. Keller PM, Shelbourne KD, McCarroll JR, Rettig AC. Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med. 1993;21(1):132–136. [DOI] [PubMed] [Google Scholar]
- 21. Kim SJ, Kim SH, Chun YM, Hwang BY, Choi DH, Yoon JY. Clinical comparison of conventional and remnant-preserving transtibial single-bundle posterior cruciate ligament reconstruction combined with posterolateral corner reconstruction. Am J Sports Med. 2012;40(3):640–649. [DOI] [PubMed] [Google Scholar]
- 22. Kohen RB, Sekiya JK. Single-bundle versus double-bundle posterior cruciate ligament reconstruction. Arthroscopy. 2009;25(12):1470–1477. [DOI] [PubMed] [Google Scholar]
- 23. Lee BK, Nam SW. Rupture of posterior cruciate ligament: diagnosis and treatment principles. Knee Surg Relat Res. 2011;23(3):135–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee DW, Jang HW, Lee YS, et al. Clinical, functional, and morphological evaluations of posterior cruciate ligament reconstruction with remnant preservation: minimum 2-year follow-up. Am J Sports Med. 2014;42(8):1822–1831. [DOI] [PubMed] [Google Scholar]
- 25. Li B, Wang JS, He M, Wang GB, Shen P, Bai LH. Comparison of hamstring tendon autograft and tibialis anterior allograft in arthroscopic transtibial single-bundle posterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3077–3084. [DOI] [PubMed] [Google Scholar]
- 26. Li G, Gill TJ, DeFrate LE, Zayontz S, Glatt V, Zarins B. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads—an in vitro experimental study. J Orthop Res. 2002;20(4):887–892. [DOI] [PubMed] [Google Scholar]
- 27. Liu P, Ao Y-F, Wang J-Q, Cui G-Q, An H, Liu X-P. Arthroscopic reconstruction of the posterior cruciate ligament using single-bundle bone-patella tendon-bone graft with moderate to long term follow-up [in Chinese]. Zhonghua Wai Ke Za Zhi. 2009;47(10):778–782. [PubMed] [Google Scholar]
- 28. Logan M, Williams A, Lavelle J, Gedroyc W, Freeman M. The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med. 2004;32(8):1915–1922. [DOI] [PubMed] [Google Scholar]
- 29. MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF. Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy. 2006;22(3):320–328. [DOI] [PubMed] [Google Scholar]
- 30. Mariani PP, Adriani E, Santori N, Maresca G. Arthroscopic posterior cruciate ligament reconstruction with bone-tendon-bone patellar graft. Knee Surg Sports Traumatol Arthrosc. 1997;5(4):239–244. [DOI] [PubMed] [Google Scholar]
- 31. May JH, Gillette BP, Morgan JA, Krych AJ, Stuart MJ, Levy BA. Transtibial versus inlay posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg. 2010;23(2):73–79. [DOI] [PubMed] [Google Scholar]
- 32. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–1012. [DOI] [PubMed] [Google Scholar]
- 33. Mosler AB, Agricola R, Weir A, Holmich P, Crossley KM. Which factors differentiate athletes with hip/groin pain from those without? A systematic review with meta-analysis. Br J Sports Med. 2015;49(12):810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Munn J, Sullivan SJ, Schneiders AG. Evidence of sensorimotor deficits in functional ankle instability: a systematic review with meta-analysis. J Sci Med Sport. 2010;13(1):2–12. [DOI] [PubMed] [Google Scholar]
- 35. Mygind-Klavsen B, Nielsen TG, Lind MC. Outcomes after posterior cruciate ligament (PCL) reconstruction in patients with isolated and combined PCL tears. Orthop J Sports Med. 2017;5(4):2325967117700077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Noh JH, Yoon KH, Kyung HS, Roh YH, Kang TS. Multiple looping technique for tibial fixation in posterior cruciate ligament reconstruction using free tendon Achilles allograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2640–2645. [DOI] [PubMed] [Google Scholar]
- 37. Osti M, Hierzer D, Seibert FJ, Benedetto KP. The arthroscopic all-inside tibial-inlay reconstruction of the posterior cruciate ligament: medium-term functional results and complication rate. J Knee Surg. 2017;30(3):238–243. [DOI] [PubMed] [Google Scholar]
- 38. Owesen C, Sivertsen EA, Engebretsen L, Granan LP, Aroen A. Patients with isolated PCL injuries improve from surgery as much as patients with ACL injuries after 2 years. Orthop J Sports Med. 2015;3(8):23259 67115599539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3(2):137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Petrie RS, Harner CD. Evaluation and management of the posterior cruciate injured knee. Oper Tech Sports Med. 1999;7(3):93–103. [Google Scholar]
- 41. Qi Y-S, Wang H-J, Wang S-J, Zhang Z-Z, Huang A-B, Yu J-K. A systematic review of double-bundle versus single-bundle posterior cruciate ligament reconstruction. BMC Musculoskelet Disord. 2016;17:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shelbourne KD, Davis TJ, Patel DV. The natural history of acute, isolated, nonoperatively treated posterior cruciate ligament injuries: a prospective study. Am J Sports Med. 1999;27(3):276–283. [DOI] [PubMed] [Google Scholar]
- 43. Shelbourne KD, Muthukaruppan Y. Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy. 2005;21(4):457–461. [DOI] [PubMed] [Google Scholar]
- 44. Shelbourne KD, Rubinstein RA., Jr Methodist Sports Medicine Center’s experience with acute and chronic isolated posterior cruciate ligament injuries. Clin Sports Med. 1994;13(3):531–543. [PubMed] [Google Scholar]
- 45. Shino K, Horibe S, Nakata K, Maeda A, Hamada M, Nakamura N. Conservative treatment of isolated injuries to the posterior cruciate ligament in athletes. J Bone Joint Surg Br. 1995;77(6):895–900. [PubMed] [Google Scholar]
- 46. Song EK, Park HW, Ahn YS, Seon JK. Transtibial versus tibial inlay techniques for posterior cruciate ligament reconstruction: long-term follow-up study. Am J Sports Med. 2014;42(12):2964–2971. [DOI] [PubMed] [Google Scholar]
- 47. Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ. Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy. 2003;19(3):262–268. [DOI] [PubMed] [Google Scholar]
- 48. Takahashi M, Matsubara T, Doi M, Suzuki D, Nagano A. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14(11):1055–1059. [DOI] [PubMed] [Google Scholar]
- 49. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 50. Van de Velde SK, Bingham JT, Gill TJ, Li G. Analysis of tibiofemoral cartilage deformation in the posterior cruciate ligament–deficient knee. J Bone Joint Surg Am. 2009;91(1):167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Xu Y, Yin Y, Wang JQ, Ao YF. Comparison of single and double bundle isolate posterior cruciate ligament reconstruction with hamstring autograft [in Chinese]. Zhonghua Wai Ke Za Zhi. 2013;51(3):247–251. [PubMed] [Google Scholar]
- 52. Yang JH, Yoon JR, Jeong HI, et al. Second-look arthroscopic assessment of arthroscopic single-bundle posterior cruciate ligament reconstruction: comparison of mixed graft versus Achilles tendon allograft. Am J Sports Med. 2012;40(9):2052–2060. [DOI] [PubMed] [Google Scholar]
- 53. Yoon KH, Bae DK, Song SJ, Cho HJ, Lee JH. A prospective randomized study comparing arthroscopic single-bundle and double-bundle posterior cruciate ligament reconstructions preserving remnant fibers. Am J Sports Med. 2011;39(3):474–480. [DOI] [PubMed] [Google Scholar]
- 54. Zayni R, Hager JP, Archbold P, et al. Activity level recovery after arthroscopic PCL reconstruction: a series of 21 patients with a mean follow-up of 29 months. Knee. 2011;18(6):392–395. [DOI] [PubMed] [Google Scholar]