Abstract
Context:
Low back pain is common in golfers. The risk factors for golf-related low back pain are unclear but may include individual demographic, anthropometric, and practice factors as well as movement characteristics of the golf swing.
Objective:
The aims of this systematic review were to summarize and synthesize evidence for factors associated with low back pain in recreational and professional golfers.
Data Sources:
A systematic literature search was conducted using the PubMed, CINAHL, and SPORTDiscus electronic databases through September 2017.
Study Selection:
Studies were included if they quantified demographic, anthropometric, biomechanical, or practice variables in individuals with and without golf-related low back pain.
Study Design:
Systematic review and meta-analysis.
Level of Evidence:
Level 3.
Data Extraction:
Studies were independently reviewed for inclusion by 2 authors, and the following data were extracted: characterization of low back pain, participant demographics, anthropometrics, biomechanics, strength/flexibility, and practice characteristics. The methodological quality of studies was appraised by 3 authors using a previously published checklist. Where possible, individual and pooled effect sizes of select variables of interest were calculated for differences between golfers with and without pain.
Results:
The search retrieved 73 articles, 19 of which met the inclusion criteria (12 case-control studies, 5 cross-sectional studies, and 2 prospective longitudinal studies). Methodological quality scores ranged from 12.5% to 100.0%. Pooled analyses demonstrated a significant association between increased age and body mass and golf-related low back pain in cross-sectional/case-control studies. Prospective data indicated that previous history of back pain predicts future episodes of pain.
Conclusion:
Individual demographic and anthropometric characteristics may be associated with low back pain, but this does not support a relationship between swing characteristics and the development of golf-related pain. Additional high-quality prospective studies are needed to clarify risk factors for back pain in golfers.
Keywords: golf, low back pain, swing, biomechanics, risk factors
Golf is one of the most frequently played sports in the world. More than 6 million people across Europe and 26 million people in the United States report playing at least 1 round of golf per year.17 Because of the physical activity and social interaction inherent in the sport, playing golf is associated with benefits to cardiovascular, respiratory, and metabolic health, particularly in older adults.42 However, in comparison with other sports and recreational activities, golf is also associated with a moderate risk of musculoskeletal injury.7,47 Low back pain (LBP) is one of the most common musculoskeletal problems reported by recreational and professional golfers.21,39,40 The prevalence of lower back injuries has been estimated to be between 15% and 35% in amateurs and up to 55% in professionals10 and is associated with significant time lost from golf play and practice.16,21 Multiple factors have been identified as potential causes of LBP in golfers. These include movement characteristics of the golf swing, individual demographic and physical characteristics, and volume of play/practice.
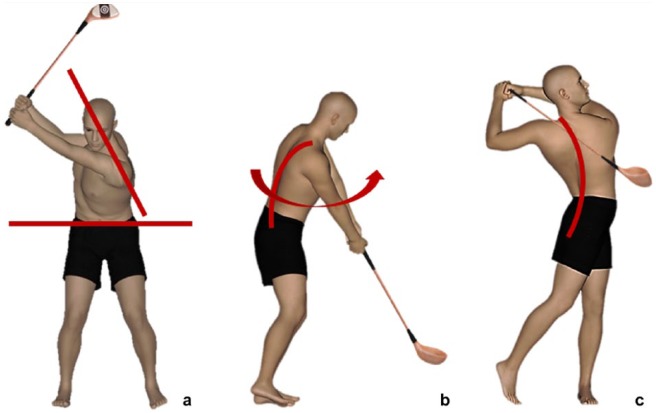
Back pain in golfers is often attributed to the mechanical demands of golfing. The golf swing is a repetitive, asymmetrical motion that is associated with high segmental angular velocities and substantial compressive, torsional, and shear loading of the spine.28 In particular, several characteristics of the modern swing technique have been identified as potential contributors to LBP. In comparison with traditional swing mechanics, the modern swing technique uses increased separation between the upper trunk/shoulders and pelvis at peak backswing and during the downswing.10,18 The separation angle between the upper trunk and pelvis is called the X-factor (Figure 1a). Increasing the X-factor may enhance angular velocity of the trunk toward the lead (nondominant) side and therefore increase the velocity of the clubhead,20 but also requires adequate spinal mobility. Modern swing technique is also associated with increased lateral flexion to the trail (dominant) side. This peaks at impact and during early follow-through. The combination of axial plane angular velocity toward the lead side and lateral flexion toward the trail side is termed the crunch factor (Figure 1b).41,50 An additional component of the modern swing that has been proposed to contribute to LBP is the trunk hyperextension, or “reverse-C” position, that occurs during follow-through (Figure 1c).10 Increased trunk hyperextension and crunch factor may result in greater compressive and shearing forces on the lumbar spine. To date, however, there is no clear evidence regarding swing mechanics and the development of LBP in golfers.
Figure 1.
Characteristics of the modern swing technique. (a) X-factor: Axial separation between upper trunk and pelvis at backswing and during downswing. (b) Crunch factor: Combination of trunk lateral flexion and axial angular velocity at impact and early follow-through. (c) Reverse-C: Trunk hyperextension during follow-through.
In addition to the mechanics of the golf swing, factors specific to the individual golfer have been proposed to increase the risk of developing LBP. These include limited or asymmetrical hip rotation range of motion,43 increasing age,51 and the method used to transport the golf bag.45 As most LBP in golfers is attributed to overuse or repetitive strain rather than a single precipitating event,36 the frequency and duration of playing and practice has also been hypothesized to contribute to symptoms, particularly in professionals.42 However, the evidence for any of these factors is limited and often conflicting.
Because of the popularity of golf, it is important to establish evidence-informed preventative and rehabilitation strategies for LBP in golfers. Therefore, the objective of this review was to systematically appraise, and synthesize where possible, evidence for risk factors that may be associated with LBP in recreational and professional golfers.
Methods
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines were utilized in the development of this review.33 The protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42017067927).
Eligibility Criteria
Peer-reviewed studies were included if they quantified demographic, anthropometric, biomechanical, or practice variables in individuals with and without golf-related LBP. Studies of amateur and professional golfers of all ages and abilities were included. Case-control, cross-sectional, and prospective longitudinal study designs were eligible for inclusion. Studies were excluded if they were conference abstracts, case reports, treatment studies, review articles, or if they did not include comparisons of individuals with and without back pain. Studies were also excluded if the full text was not available in English.
Search Strategy
A literature search was conducted in October 2016 using the PubMed, CINAHL, and SPORTDiscus electronic databases, without date restriction. The search terms were entered in 3 groups: (1) low back pain and synonyms (lower back pain, lumbago, sciatica, back ache); (2) golf; and (3) modern swing, swing characteristics, crunch factor, kinematics, kinetics, electromyography, biomechanics, handicap, epidemiology, risk factors, risks, predictors, and injury prevention. The terms from all 3 groups were combined with “AND.” Terms within groups were combined with “OR.” Reference lists from all accessed articles and previous reviews were also screened to identify any additional relevant studies. The search was repeated using the same search terms in the same databases on September 25, 2017, to identify any research articles published since the original search.
Study Selection and Data Extraction
Two authors independently reviewed the titles and abstracts of all identified studies to determine eligibility. The following data were extracted from eligible studies: study design, study population and sample size (setting, recruitment approach), definition/criteria for LBP, demographics, anthropometric variables, biomechanical golf swing variables, strength and flexibility variables, practice/expertise variables, and other factors (eg, transport of golf clubs).
Quality Assessment
Assessment of study quality and risk of bias was conducted using a previously published 16-item checklist (Table 1).23,54,55 The total quality score was calculated as the sum of all positively scored checklist items from numbers 3 through 16 relevant to that study type, divided by the total possible score for that study type (8, 12, and 9 for cross-sectional, case-control, and prospective cohort studies, respectively) and expressed as a percentage. Three authors first independently scored the studies and then discussed any study where there was disagreement until a consensus score was reached.
Table 1.
Checklist for assessment of methodological quality for cross-sectional (CS), case-control (CC), and prospective cohort (PC) study designs23,55
| Domain | Item No. | Description | CS | CC | PC |
|---|---|---|---|---|---|
| Study objective | |||||
| 1 | Positive, if the study had a clearly defined objective | + | + | + | |
| Study population | |||||
| 2 | Positive, if the main features of the study population are described (sampling frame and distribution of the population according to age and sex) | + | + | + | |
| 3 | Positive, if cases and controls are drawn from the same population and a clear definition of cases and controls is given and if patients with the disease/symptom in the past 3 months are excluded from the control group | + | |||
| 4 | Positive, if the participation rate is at least 80% or if the participation rate is 60%-80% and the nonresponse is not selective (data shown) | + | + | + | |
| 5 | Positive, if the participation rate at main moment of follow-up is at least 80% or if the nonresponse is not selective (data shown) | + | |||
| Measurements | |||||
| 6 | Positive, if data on history of the disease/symptom are collected and included in the statistical analysis | + | + | + | |
| 7 | Positive, if the outcome is measured in an identical manner among cases and controls | + | |||
| 8 | Positive, if the outcome assessment is blinded with regard to disease status | + | + | ||
| 9 | Positive, if the outcome is assessed at a time before the occurrence of the disease/symptom | + | |||
| Assessment of the outcome | |||||
| 10 | Positive, if the time period on which the assessment of disease/symptom was based was at least 1 year | + | |||
| 11 | Method for assessing injury status: physical examination blinded to exposure status (+); self-reported: specific questions relating to symptoms/disease/use of mannequin (+), single question (−) | + | + | + | |
| 12 | Positive, if incident cases were included (prospective enrollment) | + | |||
| Analysis and data presentation | |||||
| 13 | Positive, if the measures of association estimated were presented (odds ratio/relative risk), including CIs and numbers in the analysis | + | + | + | |
| 14 | Positive, if the analysis is controlled for confounding or effect modification: individual factors | + | + | + | |
| 15 | Positive, if the analysis is controlled for confounding or effect modification: other factors | + | + | + | |
| 16 | Positive, if the number of cases in the final multivariate model was at least 10 times the number of independent variables in the analysis | + | + | + | |
| Total possible score (sum of items 3 to 16) | 8 | 12 | 9 | ||
Data Synthesis
Where possible, effect sizes for case-control or cross-sectional group comparisons were extracted or calculated. For continuous data, the standardized mean difference was calculated using Cohen d. Confidence intervals (95% CIs) for the Cohen d estimate were also calculated using the z or t distribution for samples larger or smaller than 30 individuals, respectively. Odds ratios (ORs) and CIs were extracted or calculated where possible for dichotomous data. For studies where sample frequencies or means and SDs/standard errors were not reported, attempts were made to contact the authors to request the data. Meta-analysis, consisting of calculation of a pooled standardized mean difference and 95% CI, was then conducted for all variables for which appropriate data were available in at least 2 studies and where studies were sufficiently similar in population and outcome assessment. A random-effects model was used to account for remaining study heterogeneity.5 The I2 statistic was also calculated, with I2 greater than 0.75 indicative of substantial heterogeneity across studies.25 For prospective longitudinal studies, statistical measures of the relationship between independent variables and occurrence of LBP over the study period were extracted. All statistical analyses were conducted using the open-source R statistical platform (version 3.4.1; R Foundation for Statistical Computing).13
Results
Search Results
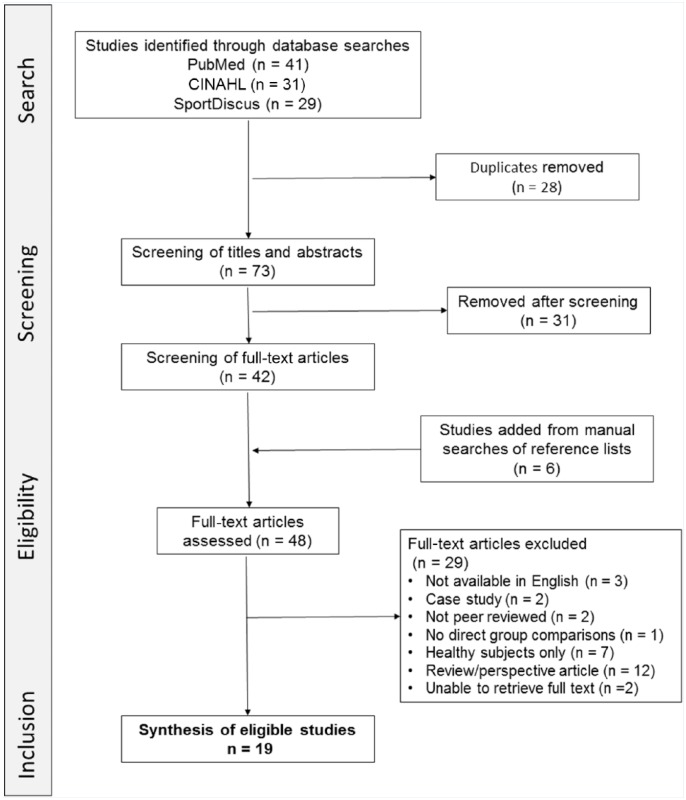
Nineteen studies were retained for the review. Of these, 12 were case-control studies,9,11,12,15,27,30,34,35,43,48,52,53 5 were cross-sectional studies,3,21,22,40,44 and 2 were prospective longitudinal studies6,16 (Figure 2).
Figure 2.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of study search and inclusion procedures.
Study Characteristics
Ten of the studies investigated recreational golfers. Of these, 3 specified a minimum duration of golf experience or frequency of play for inclusion,11,15,44 and 2 required a handicap below 20.30,52 Three studies included both professional and elite recreational golfers,21,27,35 and 4 investigated professional golfers exclusively16,22,34,53 (Table A1 in the Appendix, available in the online version of this article).
Methodological Quality
Agreement among the 3 reviewers on each checklist item ranged from 80% to 100%. The least agreement occurred on items 4 (participation rate) and 14 (control of individual confounding factors) (Table A1 in the Appendix, available online).
Prevalence and Incidence of LBP
In the cross-sectional studies, prevalence of golf-related LBP in recreational golfers varied from 12.4%21 to 26.9%.3 In cross-sectional studies of professional golfers, prevalence ranged from 40.0% to 58.1%.21,22 In these studies, it was unclear whether the reported prevalence of LBP was specific to the time of the study, over the course of a year, or lifetime prevalence. In the longitudinal studies, the incidence of new or recurrent back pain episodes was 31.6% (novice recreational golfers) and 57.1% (young elite golfers) across the course of a year or a playing season, respectively.6,16
Demographic Factors
The pooled results from 10 case-control and cross-sectional studies indicated that greater age was significantly associated with LBP (standardized mean difference [SMD], 0.57; 95% CI, 0.07 to 1.07; I2, 79.9%) (Figure A1a in the Appendix, available online).9,11,12,27,34,35,40,43,48,52 The studies included in this meta-analysis included cohorts of both professional and recreational golfers with disparate age distributions. Therefore, separate subanalyses for the relationship between age and LBP in recreational and professional golfers were also conducted. These demonstrated the same trends (recreational golfers: SMD, 0.50; 95% CI, –0.14 to 1.14; I2, 80.0%; professional golfers: SMD, 0.83; 95% CI, –0.95 to 2.61; I2, 89.1%) (Figure A1b in the Appendix, available online). One of the 4 studies reporting the association between sex and LBP found that male golfers are more likely to experience pain (OR, 3.4; 95% CI, 1.3 to 13.4),44 but this finding was not replicated in other cohorts.3,40,43 One study reported a higher percentage of lower back injuries in professionals compared with recreational golfers (OR, 4.7; 95% CI, 2.7 to 8.3).21 In the prospective study data, the only demographic factor that was a significant predictor of occurrence of back pain over 12 months (in novice recreational golfers) was a previous history of back pain (relative risk, 9.8; 95% CI, 4.5 to 21.4).6
Anthropometric Characteristics
Pooled results from case-control and cross-sectional studies indicated that mass was significantly associated with LBP (SMD, 0.36; 95% CI, 0.09 to 0.63; I2, 0.0%) (Figure A2a in the Appendix, available online). Golfers with LBP were heavier than healthy controls. Separate subanalyses for recreational and professional golfers were again conducted to account for the different data distributions in each group. Subanalyses demonstrated that a relationship between mass and LBP existed only in recreational golfers (recreational golfers: SMD, 0.64; 95% CI, 0.21 to 1.06; I2, 0.00%; professional golfers: SMD, 0.08; 95% CI, –0.45 to 0.60; I2, 0.00%) (Figure A2b in the Appendix, available online). One longitudinal study showed that, in trainee professional golfers, body mass index (BMI) was significantly negatively correlated with frequency (% time) of LBP symptoms over a 10-month period (r = −0.7).16 There was no evidence that hand dominance is associated with LBP.43
Golf Swing Movement Characteristics
Kinematic and muscle activation characteristics of the golf swing in individuals with and without LBP were investigated in 7 case-control and cross-sectional studies.9,11,12,27,34,48,52 All but 2 studies34,52 divided the swing into address, backswing, downswing, impact, and follow-through events and phases.
Pooled analyses of kinematic data (Table 2) were limited by heterogeneity in methodology, particularly in the approach taken to modeling trunk motion, and results were inconsistent. Two studies investigated crunch factor, defined as the instantaneous product of trunk or lumbar axial angular velocity and trunk or lumbar lateral flexion angle.11,34 There was no significant difference between peak crunch factor in individuals with and without LBP in either study. Peak X-factor was reported in 2 studies, with conflicting results (Table 2).11,52
Table 2.
Summary of individual study findings for swing kinematics, with calculated effect sizes (Cohen d) and CIs for group comparisons
| Study | Variable | Finding in Low Back Pain Group | Swing Phase | Effect Size (95% CI) |
|---|---|---|---|---|
| Lindsay and Horton34 | Peak trunk lateral flexion to lead side | Increased | Entire swing | 2.0 (0.4 to 3.5) |
| Lindsay and Horton34 | Peak trunk lateral flexion angular velocity | Increased | Entire swing | 1.3 (–0.1 to 2.7) |
| Lindsay and Horton34 | Trunk flexion angular velocity | Decreased | Entire swing | 2.1 (0.5 to 3.7) |
| Tsai et al52 | Peak trunk axial rotation to trail side | Decreased | Entire swing | 1.6 (0.7 to 2.4) |
| Cole and Grimshaw11 | Peak crunch factor | No difference | Follow-through | 0.1 (–0.7 to 0.9) |
| Lindsay and Horton34 | Peak crunch factor | No difference | Entire swing | 0.2 (–1.1 to 1.5) |
| Tsai et al52 | Peak X-factor | No difference | Entire swing | 0.3 (–0.4 to 1.1) |
| Cole and Grimshaw11 | Peak X-factor | Trend toward decreased | Peak backswing | 0.7 (–0.1 to 1.6) |
Two studies investigated the timing of trunk muscle activity during the golf swing.12,27 Pooled analysis of both studies indicated no relationship between timing of lead side external oblique onset relative to the beginning of backswing in golfers and LBP (SMD, –1.33; 95% CI, –4.83 to 2.18; I2, 95.82). Cole and Grimshaw12 reported that onsets of bilateral upper and lower lumbar erector spinae were earlier relative to the beginning of backswing in the LBP group (d range, 0.7-1.0).12 In 1 study, differences in amplitude of erector spinae and external oblique activity between individuals with and without LBP showed different trends in high-handicap and low-handicap golfers,9 while another reported no difference in abdominal muscle activity between groups in professionals.27 Silva et al48 reported that activity of the lead biceps femoris during backswing was the most important factor to distinguish between golfers with and without LBP using a nonlinear machine learning approach.
Strength/Flexibility Characteristics
Several cross-sectional/case-control studies demonstrated a relationship between trunk and hip muscle performance and LBP (Table 3). Peak trunk extensor strength, endurance of the trunk extensors and flexors, and endurance in the side-bridge position did not predict development of LBP over 10 months in young professionals.16 However, side-to-side asymmetry of side-bridge endurance was significantly associated with development of LBP (r = 0.6), explaining 36% of the variability.
Table 3.
Summary of individual study findings for trunk and hip muscle strength and performance, with calculated effect sizes (Cohen d) and CIs for group comparisons where appropriate data were available
| Study | Variable | Finding in Low Back Pain Group | Effect Size (95% CI) |
|---|---|---|---|
| Evans and Oldreive15 | Transversus abdominis endurance | Decreased | 1.3 (0.3 to 2.3) |
| Kalra et al30 | Trunk strength in all planes | Decreased | |
| Lindsay and Horton35 | Trunk axial rotation endurance toward lead side | Decreased | 1.4 (0.5 to 2.3) |
| Tsai et al52 | Peak isokinetic trunk extension | Decreased | 1.04 (0.3 to 1.8) |
| Tsai et al52 | Peak isometric lead hip adduction | Decreased | 1.0 (0.2 to 1.7) |
Pooled analyses of trunk extension range of motion data (SMD, 3.2; 95% CI, –2.6 to 9.0; I2, 98.0%) and 2 out of 3 individual studies investigating active trunk motion in all other planes did not indicate an association between trunk range of motion and LBP.30,52,53 Four studies investigated hip range of motion.22,43,52,53 Pooled analyses of lead and trail hip internal rotation did not demonstrate an association between range of motion and LBP (lead limb: SMD, 1.25; 95% CI, –1.3 to 3.8; I2, 96.8; trail limb: SMD, 0.13; 95% CI, –0.3 to 0.5; I2, 0.0%). Similarly, lead and trail hip external rotation were not associated with LBP (lead limb: SMD, 0.1; 95% CI, 0.7 to 0.9; I2, 61.3%; trail limb: SMD, 0.1; 95% CI, –0.9 to 1.1; I2, 72.8%). Two studies reported that side-to-side asymmetry in hip internal rotation was significantly greater in individuals with LBP, with the LBP groups having reduced range of motion in the lead hip,43,53 but appropriate data were not available to pool these results or calculate effect sizes.
Practice Characteristics
The pooled analysis of case-control and cross-sectional studies demonstrated no relationship between handicap and LBP (SMD, 0.0; 95% CI, –0.3 to 0.4; I2, 0.0%). Although multiple studies investigated frequency and duration of play/practice, the heterogeneity in how practice characteristics were measured precluded pooled analyses. One study reported that there was a lower risk of LBP in individuals who performed less than 1 hour of full shot practice per week (OR, 0.5; 95% CI, 0.3 to 0.8),40 and another described increasing rates of spinal pain with increasing rounds and shots played per week.21 However, multiple other studies found no significant difference in playing frequency or chipping/full shot practice in individuals with and without LBP.3,34,43,44 There was no evidence of any influence of warm-up, stretching, or strengthening behaviors on LBP status in either the case-control/cross-sectional21,22 or prospective studies.6 Gosheger et al21 reported that individuals in their sample who reported regularly carrying their golf bag were significantly more likely to have experienced LBP.
Discussion
This study confirms that LBP is a widespread problem in golfers. Pooled analyses indicated that LBP is associated with individual demographic and anthropometric characteristics, but current limited evidence does not conclusively link kinematic or electromyographic features of swing technique to golf-related LBP.
In this review, age and previous history of symptoms emerged as potential contributors to LBP. The mean age of recreational golfers in the pooled data was 51.5 years, consistent with reported mean ages of recreational golfers in the United States, Europe, and Australia.2,14,49 In the general population, the prevalence of LBP also increases with age until the sixth decade.29 This has been attributed to a transition from short, acute episodes of pain in young adulthood to more persistent symptoms over time.56 One high-quality longitudinal study indicated that the strongest predictor of future episodes of golf-related LBP is a previous history of LBP.6 This finding also supports results from studies of the general population and in other athletic groups.8,56 Other predictors of future episodes of LBP after an initial episode include the severity of pain during the initial episode,19 alterations in central nervous system structure and function,38 and depression and psychological distress.46 These factors were not investigated in any of the studies reviewed and should be included in future studies of golf-related LBP.
This review found that in recreational golfers, as in nongolfers, greater mass is associated with more LBP. This is potentially because of increased spinal loading. However, increased mass may also be a consequence of reduced physical activity due to the presence of pain.32 In contrast, in young professional golfers, development of LBP over time was associated with a lower BMI. The mechanism by which lower BMI may increase risk for LBP does not appear to be mediated by muscle mass, as in the longitudinal study by Evans et al,16 there was no relationship between BMI and strength. They speculated that taller individuals with lower body mass may be at heightened risk of injury due to increased trunk range of motion or increased lever arm for forces at the spine, but these hypotheses have not been further examined.
This study does not indicate a consistent link between features of the modern swing and golf-related LBP. Increased X-factor, crunch factor, and trunk hyperextension may all result in greater loading of the spine and may be associated with asymmetrical patterns of spinal degenerative changes.50 However, the absence of significant group differences in these swing mechanics in current studies likely reflects a multifactorial relationship between cumulative mechanical loading and an individual’s risk of developing LBP. Although 2 small studies demonstrated altered timing and activation of the trunk musculature during the swing in individuals with back pain, the characteristics that were affected were inconsistent and varied in golfers with high and low handicap.9 Substantial evidence in nongolfers indicates that motor control adaptations with LBP are highly individual.26
The results in this review do not support a relationship between lead/trail hip range of motion and LBP. Biomechanical analysis in healthy professional golfers indicates that golfers with limited lead hip internal rotation utilize greater lumbopelvic motion throughout the golf swing and suggests that this increased spinal motion may lead to back pain over time.31 However, this relationship is not consistently evident in current research, and this may be due to disparities between available single-planar joint range of motion measured in an unweighted position and the dynamic, multiplanar motion utilized during the swing.24
Individual cross-sectional and case-control studies reported impairments in multiple aspects of trunk muscle performance in golfers with LBP. As these studies examined different variables, data could not be pooled.15,35,52 Decrements in trunk muscle strength and endurance have also been reported in nongolfers with LBP. These have primarily been attributed to deconditioning, exertional pain, and fear avoidance.1,4,37 In a longitudinal study that reported that trunk endurance asymmetry was predictive of back pain in young elite golfers, multiple participants had a history of LBP at baseline, and therefore, it is unclear to what extent this strength asymmetry was a result of previous episodes of pain rather than a cause of ongoing symptoms.
Limitations
Pooling of data in this review was limited by study heterogeneity and is reflected by high I2 statistics for some variables. There was substantial variability in how LBP was operationalized in terms of severity or duration across studies. Additionally, studies that investigated the biomechanics of the golf swing utilized disparate approaches to estimating global or regional trunk motion. The methodological quality of studies in this review varied widely. However, quality scores in the present study were similar to those in previous systematic reviews of risk factors for musculoskeletal disorders utilizing the same methodological checklist.23,55 Only 3 studies in this review controlled for potential confounding factors in the analysis,6,9,44 and 5 reported measures of association and confidence intervals.6,16,43,44,48 Very few reported the participation rate relative to the available population or utilized blinded assessment.
Conclusion
Age and body mass are associated with golf-related LBP. BMI and previous history of back pain may predict golfers who will experience symptoms. However, because of generally low quality and heterogeneity of current evidence, additional research is needed to facilitate evidence-based prevention and rehabilitation of LBP in golfers.
Supplemental Material
Supplemental material, 28951_Appendix for Risk Factors Associated With Low Back Pain in Golfers: A Systematic Review and Meta-analysis by Jo Armour Smith, Andrew Hawkins, Marybeth Grant-Beuttler, Richard Beuttler and Szu-Ping Lee in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Adams MA, Mannion AF, Dolan P. Personal risk factors for first-time low back pain. Spine (Phila Pa 1976). 1999;24:2497-2505. [DOI] [PubMed] [Google Scholar]
- 2. AustraliaGolf. Golf Participation Report. 2016. http://www.golf.org.au/site/_content/document/00037437-source.pdf. Accessed December 2017.
- 3. Batt M. A survey of golf injuries in amateur golfers. Br J Sports Med. 1992;26:63-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beneck GJ, Baker LL, Kulig K. Spectral analysis of EMG using intramuscular electrodes reveals non-linear fatigability characteristics in persons with chronic low back pain. J Electromyogr Kinesiol. 2013;23:70-77. [DOI] [PubMed] [Google Scholar]
- 5. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Fixed-effect versus random-effects models. In: Borenstein M, Hedges LV, Higgins JPT, Rothstein HR, eds. Introduction to Meta-Analysis. Chichester, England: Wiley; 2009:77-86. [Google Scholar]
- 6. Burdorf A, Van Der Steenhoven GA, Tromp-Klaren EG. A one-year prospective study on back pain among novice golfers. Am J Sports Med. 1996;24:659-664. [DOI] [PubMed] [Google Scholar]
- 7. Cabri J, Sousa JP, Kots M, Barreiros J. Golf-related injuries: a systematic review. Eur J Sport Sci. 2009;9:353-366. [Google Scholar]
- 8. Cholewicki J, Silfies SP, Shah RA, et al. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine (Phila Pa 1976). 2005;30:2614-2620. [DOI] [PubMed] [Google Scholar]
- 9. Cole MH, Grimshaw PN. Electromyography of the trunk and abdominal muscles in golfers with and without low back pain. J Sci Med Sport. 2008;11:174-181. [DOI] [PubMed] [Google Scholar]
- 10. Cole MH, Grimshaw PN. The biomechanics of the modern golf swing: implications for lower back injuries. Sports Med. 2016;46:339-351. [DOI] [PubMed] [Google Scholar]
- 11. Cole MH, Grimshaw PN. The crunch factor’s role in golf-related low back pain. Spine J. 2014;14:799-807. [DOI] [PubMed] [Google Scholar]
- 12. Cole MH, Grimshaw PN. Trunk muscle onset and cessation in golfers with and without low back pain. J Biomech. 2008;41:2829-2833. [DOI] [PubMed] [Google Scholar]
- 13. Core Team R. A language and environment for statistical computing. 2013. http://www.r-project.org/. Accessed July 14, 2017.
- 14.EnglandGolf. Golf Club Membership Questionnaire. 2016. http://www.englandgolf.org/page.aspx?sitesectionid=448&sitesectiontitle=Golf+Club+Membership+Questionnaire. Accessed December 11, 2017.
- 15. Evans C, Oldreive W. A study to investigate whether golfers with a history of low back pain show a reduced endurance of transversus abdominis. J Man Manip Ther. 2000;4:162-171. [Google Scholar]
- 16. Evans K, Refshauge KM, Adams R, Aliprandi L. Predictors of low back pain in young elite golfers: a preliminary study. Phys Ther Sport. 2005;6:122-130. [Google Scholar]
- 17. Farrally MR, Cochran AJ, Crews DJ, et al. Golf science research at the beginning of the twenty-first century. J Sports Sci. 2003;21:753-765. [DOI] [PubMed] [Google Scholar]
- 18. Finn C. Rehabilitation of low back pain in golfers. Sports Health. 2013;5:313-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fritz JM, Beneciuk JM, George SZ. Relationship between categorization with the STarT Back screening tool and prognosis for people receiving physical therapy for low back pain. Phys Ther. 2011;91:722-732. [DOI] [PubMed] [Google Scholar]
- 20. Gluck GS, Bendo JA, Spivak JM. The lumbar spine and low back pain in golf: a literature review of swing biomechanics and injury prevention. Spine J. 2008;8:778-788. [DOI] [PubMed] [Google Scholar]
- 21. Gosheger G, Liem D, Ludwig K, Greshake O, Winkelmann W. Injuries and overuse syndromes in golf. Am J Sports Med. 2003;31:438-443. [DOI] [PubMed] [Google Scholar]
- 22. Gulgin HR, Armstrong CW. Passive hip rotation range of motion in LPGA golfers. Clin Kinesiol. 2008;62(2):9-15. [Google Scholar]
- 23. Hamstra-Wright KL, Huxel Bliven KC, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. Br J Sports Med. 2015;49:362-369. [DOI] [PubMed] [Google Scholar]
- 24. Harris-Hayes M, Sahrmann SA, Van Dillen LR. Relationship between the hip and low back pain in athletes who participate in rotation-related sports. J Sport Rehabil. 2009;18:60-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(suppl 3):S90-S98. [DOI] [PubMed] [Google Scholar]
- 27. Horton JF, Lindsay DM, Macintosh BR. Abdominal muscle activation of elite male golfers with chronic low back pain. Med Sci Sports Exerc. 2001;33:1647-1654. [DOI] [PubMed] [Google Scholar]
- 28. Hosea T, Gatt CJ. Back pain in golf. Clin Sports Med. 1996;15:37-53. [PubMed] [Google Scholar]
- 29. Hoy D, March L, Brooks P, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968-974. [DOI] [PubMed] [Google Scholar]
- 30. Kalra N, Singh J, Neethi M. Study of trunk movement deficits in golfers with low back pain symptoms. Indian J Physiother Occup Ther. 2012;6:141-145. [Google Scholar]
- 31. Kim SB, You JH, Kwon OY, Yi CH. Lumbopelvic kinematic characteristics of golfers with limited hip rotation. Am J Sports Med. 2015;43:113-120. [DOI] [PubMed] [Google Scholar]
- 32. Lake JK, Power C, Cole TJ. Back pain and obesity in the 1958 British birth cohort: cause or effect? J Clin Epidemiol. 2000;53:245-250. [DOI] [PubMed] [Google Scholar]
- 33. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:B2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lindsay D, Horton J. Comparison of spine motion in elite golfers with and without low back pain. J Sports Sci. 2002;20:599-605. [DOI] [PubMed] [Google Scholar]
- 35. Lindsay DM, Horton JF. Trunk rotation strength and endurance in healthy normals and elite male golfers with and without low back pain. N Am J Sports Phys Ther. 2006;1:80-89. [PMC free article] [PubMed] [Google Scholar]
- 36. Lindsay DM, Vandervoort AA. Golf-related low back pain: a review of causative factors and prevention strategies. Asian J Sports Med. 2014;5:e24289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Luoto S, Heliövaara M, Hurri H, Alaranta H. Static back endurance and the risk of low-back pain. Clin Biomech (Bristol, Avon). 1995;10(6):323-324. [DOI] [PubMed] [Google Scholar]
- 38. Mansour AR, Baliki MN, Huang L, et al. Brain white matter structural properties predict transition to chronic pain. Pain. 2013;154:2160-2168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McHardy A, Pollard H, Luo K. One-year follow-up study on golf injuries in Australian amateur golfers. Am J Sports Med. 2007;35:1354-1360. [DOI] [PubMed] [Google Scholar]
- 40. McHardy AJ, Pollard HP, Luo K. Golf-related lower back injuries: an epidemiological survey. J Chiropr Med. 2007;6:20-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Morgan DA, Sugaya H, Banks S, Cook F. A new “twist” on golf kinematics and low back injuries: the crunch factor. In: Proceedings of the 21st Annual Meeting of the American Society of Biomechanics, Clemson University. Clemson, SC: The Bioengineering Alliance of South Carolina; 1997:274-275. [Google Scholar]
- 42. Murray AD, Daines L, Archibald D, et al. The relationships between golf and health: a scoping review. Br J Sports Med. 2017;51:12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Murray E, Birley E, Twycross-Lewis R, Morrissey D. The relationship between hip rotation range of movement and low back pain prevalence in amateur golfers: an observational study. Phys Ther Sport. 2009;10:131-135. [DOI] [PubMed] [Google Scholar]
- 44. Nicholas JJ, Reidy M, Oleske DM. An epidemiologic survey of injury in golfers. J Sport Rehabil. 1998;7:112-121. [Google Scholar]
- 45. Parziale JR, Mallon WJ. Golf injuries and rehabilitation. Phys Med Rehabil Clin N Am. 2006;17:589-607. [DOI] [PubMed] [Google Scholar]
- 46. Pincus T, Vogel S, Burton AK, Santos R, Field AP. Fear avoidance and prognosis in back pain: a systematic review and synthesis of current evidence. Arthritis Rheum. 2006;54:3999-4010. [DOI] [PubMed] [Google Scholar]
- 47. Sheu Y, Chen LH, Hedegaard H. Sports- and recreation-related injury episodes in the United States, 2011-2014. Natl Health Stat Rep. 2016;(99):1-12. [PubMed] [Google Scholar]
- 48. Silva L, Vaz JR, Castro MA, Serranho P, Cabri J, Pezarat-Correia P. Recurrence quantification analysis and support vector machines for golf handicap and low back pain EMG classification. J Electromyogr Kinesiol. 2015;25:637-647. [DOI] [PubMed] [Google Scholar]
- 49. Stachura M. The NGF’s annual golf participation report uncovers favorable trends for the game’s future. GolfDigest.com. 2017. https://www.golfdigest.com/story/the-ngf-annual-golf-participation-report-uncovers-favorable-trends-for-the-games-future. Accessed December 11, 2017.
- 50. Sugaya H, Tsuchiya A, Moriya H, Morgan DA. Low back injury in elite and professional golfers: an epidemiologic and radiographic study. In: Farrally MR, Cochran AJ, eds. Science and Golf III: Proceedings of the World Scientific Congress of Golf. Leeds, England: Human Kinetics; 1999:83-91. [Google Scholar]
- 51. Sutcliffe J, Ly JQ, Kirby A, Beall DP. Magnetic resonance imaging findings of golf-related injuries. Curr Probl Diagn Radiol. 2008;37:231-241. [DOI] [PubMed] [Google Scholar]
- 52. Tsai Y-S, Sell TC, Smoliga JM, Myers JB, Learman KE, Lephart SM. A comparison of physical characteristics and swing mechanics between golfers with and without a history of low back pain. J Orthop Sports Phys Ther. 2010;40:430-438. [DOI] [PubMed] [Google Scholar]
- 53. Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32:494-497. [DOI] [PubMed] [Google Scholar]
- 54. van der Windt DA, Thomas E, Pope DP, et al. Occupational risk factors for shoulder pain: a systematic review. Occup Environ Med. 2000;57:433-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. van der Worp H, van Ark M, Roerink S, Pepping GJ, van den Akker-Scheek I, Zwerver J. Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med. 2011;45:446-452. [DOI] [PubMed] [Google Scholar]
- 56. Waxman R, Tennant A, Helliwell P. A prospective follow-up study of low back pain in the community. Spine (Phila Pa 1976). 2000;25:2085-2090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 28951_Appendix for Risk Factors Associated With Low Back Pain in Golfers: A Systematic Review and Meta-analysis by Jo Armour Smith, Andrew Hawkins, Marybeth Grant-Beuttler, Richard Beuttler and Szu-Ping Lee in Sports Health: A Multidisciplinary Approach