Abstract
Background:
Few population-based descriptive studies on the incidence of anterior cruciate ligament (ACL) reconstruction and concomitant pathology exist.
Hypothesis:
Incidence of ACL reconstruction has increased from 2002 to 2014.
Study Design:
Descriptive clinical epidemiology study.
Level of Evidence:
Level 3.
Methods:
The Truven Health Analytics MarketScan Commercial Claims and Encounters database, which contains insurance enrollment and health care utilization data for approximately 158 million privately insured individuals younger than 65 years, was used to obtain records of ACL reconstructions performed between 2002 and 2014 and any concomitant pathology using Current Procedures Terminology (CPT) and International Classification of Diseases, Ninth Revision (ICD-9) codes. The denominator population was defined as the total number of person-years (PYs) for all individuals in the database. Annual rates were computed overall and stratified by age, sex, and concomitant procedure.
Results:
There were 283,810 ACL reconstructions and 385,384,623 PYs from 2002 to 2014. The overall rate of ACL reconstruction increased 22%, from 61.4 per 100,000 PYs in 2002 to 74.6 per 100,000 PYs in 2014. Rates of isolated ACL reconstruction were relatively stable over the study period. However, among children and adolescents, rates of both isolated ACL reconstruction and ACL reconstruction with concomitant meniscal surgery increased substantially. Adolescents aged 13 to 17 years had the highest absolute rates of ACL reconstruction, and their rates increased dramatically over the 13-year study period (isolated, +37%; ACL + meniscal repair, +107%; ACL + meniscectomy, +63%). Rates of isolated ACL reconstruction were similar for males and females (26.1 vs 25.6 per 100,000 PYs, respectively, in 2014), but males had higher rates of ACL reconstruction with concomitant meniscal surgery than females.
Conclusion:
Incidence rates of isolated ACL reconstruction and rates of concomitant meniscal surgery have increased, particularly among children and adolescents.
Clinical Relevance:
A renewed focus on adoption of injury prevention programs is needed to mitigate these trends. In addition, more research is needed on long-term patient outcomes and postoperative health care utilization after ACL reconstruction, with a focus on understanding the sex-based disparity in concomitant meniscal surgery.
Keywords: ACL, anterior cruciate ligament, ACL reconstruction, meniscus surgery, epidemiology
Anterior cruciate ligament (ACL) tears and ruptures are among the most severe knee injuries.8,11,15 The precise number of ACL injuries in the United States is unknown but has been approximated to be between 60,000 and 200,000 injuries annually.8,12-15 Because of the devastating nature of an ACL tear or rupture, many people undergo surgical intervention to reconstruct the ligament and stabilize the knee.7,11,16,23 Despite the fact that a large number of ACL reconstructions are performed annually in the United States, information about the clinical epidemiology of these procedures is relatively limited. One factor contributing to this paucity of basic epidemiologic information is the lack of large population-based data sources that capture a broad spectrum of individuals. The use of data sources such as administrative claims databases is one means of addressing this knowledge gap in orthopaedic research.10,20 The primary aim of this study was to describe the clinical epidemiology of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States. We quantified trends in the annual incidence rates of ACL reconstruction from 2002 to 2014 overall and by a variety of factors, including concomitant procedures, age, and sex.
Methods
This study used the Truven Health Analytics MarketScan Commercial Claims and Encounters database for the years 2002 through 2014. This administrative database contains information for a large sample (approximately 158 million people) of privately insured individuals younger than 65 years who obtain employer-sponsored health insurance.3 Multiple insurance providers are included and more than 20 billion claims are stored in the database, allowing investigators to track an individual’s health care utilization over time while they are enrolled in an employer-sponsored health insurance plan. We quantified the annual incidence rates of ACL reconstruction from 2002 through 2014 overall and by setting (outpatient vs inpatient), approach (open vs arthroscopic), and concomitant procedures. Analyses were stratified by clinically meaningful age groups (<13, 13-17, 18-30, 31-40, and >40 years) and sex. The study was determined to be exempt from review by the University of North Carolina at Chapel Hill institutional review board.
Event Definition
Individuals who underwent ACL reconstruction were identified using both the Outpatient and Inpatient Services files of the database from January 1, 2002 through December 31, 2014. Current Procedural Terminology (CPT) codes for arthroscopically aided ACL reconstruction or augmentation (CPT 29888) or ligamentous reconstruction of the knee (CPT 27428) with concurrent identification of new or prior ACL tear (ICD-9 diagnosis codes 717.83 or 844.2) were used to identify incident surgeries. International Classification of Diseases, Ninth Revision (ICD-9) procedure code 81.45 (other repair of the cruciate ligaments) was also used with concurrent ICD-9 diagnosis codes. Given that we analyzed the epidemiology of incident reconstruction and not incident injury, all ACL reconstructions were included as events; however, to ensure that a reconstruction was not counted more than once, only 1 ACL reconstruction per patient per 30-day period was included in the sample. If the patient had more than 1 claim for an ACL reconstruction per 30-day period, only the first instance (first date) was included.
Denominator Definition
The incidence rate denominator reflects person-time at risk for all unique individuals enrolled in a commercial insurance plan captured in the database. Given the variable length of enrollment in the database for each participant, time at risk for the outcome was defined as person-months at risk. Participants were required to have continuous enrollment in the database for the full month. It was possible for individuals to have more than 1 incident ACL reconstruction within a calendar year and therefore be counted as a case more than once in a calendar year. However, based on the definition used for an incident ACL reconstruction in this study, it was not possible for individuals to experience more than 1 ACL reconstruction in a given month. The denominator is presented as person-years (PYs) for ease of interpretation.
Concomitant Procedures
To analyze the incidence of concomitant procedures performed with the ACL reconstruction, the following definitions were used: medial and/or lateral meniscectomy (CPT: 29880, 29881, 27332), medial and/or lateral meniscal repair (CPT: 29882, 29883, 27403), chondroplasty (CPT: 29877), microfracture (CPT: 29879), collateral ligament (medial or lateral) repair or reconstruction (CPT: 27405, 27409, 27427), and posterior cruciate ligament (PCL) repair or reconstruction (CPT: 29889). Patients who underwent ACL reconstruction without any of these prespecified concomitant procedures were defined as having isolated ACL reconstructions.
Results
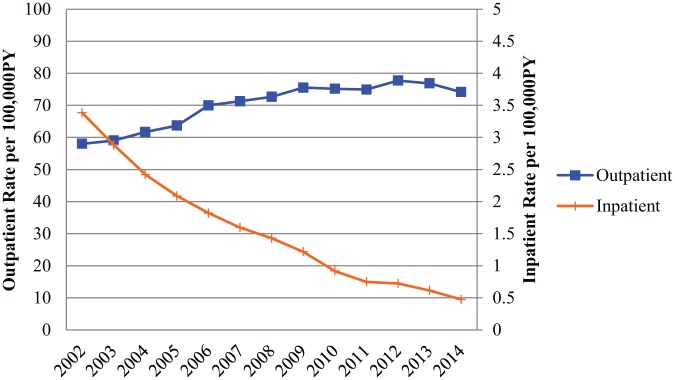
There were 283,810 unique ACL reconstructions and 385,384,623 PYs at risk identified from January 1, 2002 to December 31, 2014. Overall, the rate of ACL reconstruction was 73.6 reconstructions per 100,000 PYs. The rate of ACL reconstructions per 100,000 PYs increased 22% from 61.4 in 2002 to 74.6 in 2014 (Figure 1).
Figure 1.
Annual trends in incidence rate of inpatient versus outpatient anterior cruciate ligament reconstruction per 100,000 person-years (PYs) among patients included in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014.
Setting and Approach
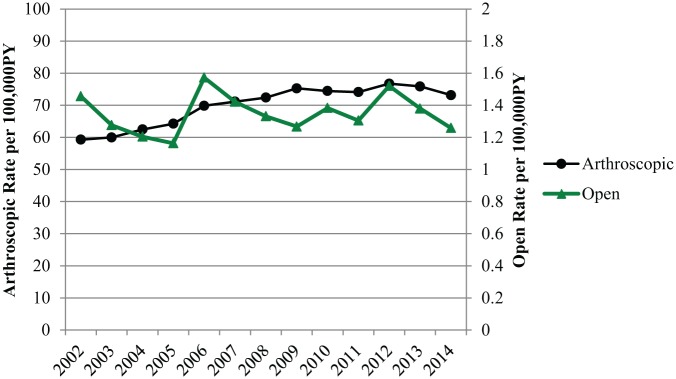
Most ACL reconstructions were performed in an outpatient setting (98%) using an arthroscopic approach (98%) (Table 1). Outpatient procedures increased 28% over the study period from 58.0 to 74.1 per 100,000 PYs, with a concurrent decrease in inpatient procedures (Figure 1). Similarly, arthroscopic procedures increased from 59.3 per 100,000 PYs in 2002 to 73.2 per 100,000 PYs in 2014. However, open procedure rates remained relatively stable (1.5 to 1.3 per 100,000 PYs) (Figure 2).
Table 1.
Demographics of patients who underwent ACL reconstruction and were captured in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014 (N = 283,810)
| n | % | |
|---|---|---|
| Setting | ||
| Inpatient | 4806 | 1.7 |
| Outpatient | 279,004 | 98.3 |
| Approach | ||
| Open | 5215 | 1.8 |
| Arthroscopic | 277,465 | 97.8 |
| Missing | 1130 | 0.4 |
| Sex | ||
| Male | 162,399 | 57.2 |
| Female | 121,411 | 42.8 |
| Age group, y | ||
| <13 | 1424 | 0.5 |
| 13-17 | 64,793 | 22.8 |
| 18-30 | 96,381 | 34.0 |
| 31-40 | 57,443 | 20.2 |
| >40 | 63,769 | 22.5 |
| Concomitant procedures | ||
| Meniscectomy | 103,831 | 36.6 |
| None (isolated ACL) | 98,433 | 34.7 |
| Meniscal repair | 26,666 | 9.4 |
| Meniscal repair, meniscectomy | 15,512 | 5.5 |
| Meniscectomy, chondroplasty | 9196 | 3.2 |
| Meniscectomy, microfracture | 7451 | 2.6 |
| Chondroplasty | 7409 | 2.6 |
| Microfracture | 2620 | 0.9 |
| Collateral ligament | 2298 | 0.8 |
| Meniscectomy, collateral ligament | 1394 | 0.5 |
| Meniscal repair, chondroplasty | 1049 | 0.4 |
| Meniscectomy, chondroplasty, microfracture | 868 | 0.3 |
| Meniscal repair, microfracture | 855 | 0.3 |
| Meniscal repair, meniscectomy, chondroplasty | 836 | 0.3 |
| Meniscal repair, meniscectomy, microfracture | 822 | 0.3 |
| PCL | 712 | 0.3 |
| Meniscal repair, collateral ligament | 624 | 0.2 |
| Meniscectomy, PCL | 506 | 0.2 |
| Collateral ligament, PCL | 431 | 0.2 |
| Chondroplasty, microfracture | 388 | 0.1 |
| Meniscal repair, meniscectomy, collateral ligament | 304 | 0.1 |
| Meniscectomy, PCL, microfracture | 274 | 0.1 |
| Meniscectomy, PCL, collateral ligament | 165 | 0.1 |
| Collateral ligament, chondroplasty | 155 | 0.1 |
| Other combinations of concomitant procedures | 1011 | 0.4 |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Figure 2.
Annual trends in incidence rate of open versus arthroscopic anterior cruciate ligament reconstruction per 100,000 person-years (PYs) among patients included in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014.
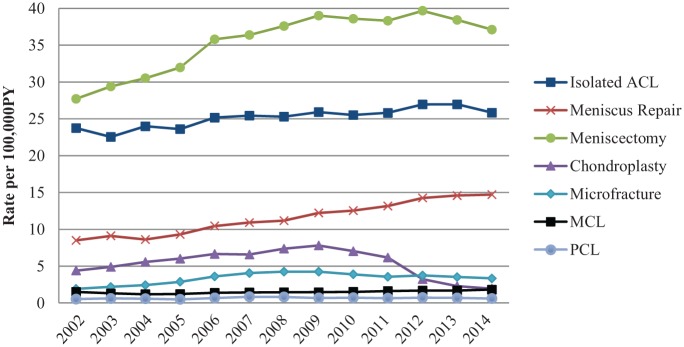
Concomitant Procedures
Overall, isolated ACL reconstruction rates increased slightly over the study period, ranging from a low of 22.6 per 100,000 PY in 2003 to a high of 27.0 per 100,000 PYs in 2012 and 2013 (Figure 3). Approximately 50% of patients underwent concomitant meniscectomy, which was the most common concomitant procedure (Table 1). Concomitant meniscal repairs and meniscectomies both increased appreciably over the study period (73% and 34% increase, respectively), as did concomitant microfracture surgery (75% increase) (Figure 3). Concomitant collateral ligament repair or reconstruction and PCL repair or reconstruction also increased over the study period (21% and 16% increase, respectively). Between 2002 and 2009, there were increasing rates of concomitant chondroplasty, followed by a sharp decrease in rates from 2009 to 2014 (Figure 3).
Figure 3.
Annual trends in incidence rate of anterior cruciate ligament (ACL) reconstruction with concomitant procedures per 100,000 person-years (PYs) among patients included in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014. MCL, medial collateral ligament; PCL, posterior cruciate ligament.
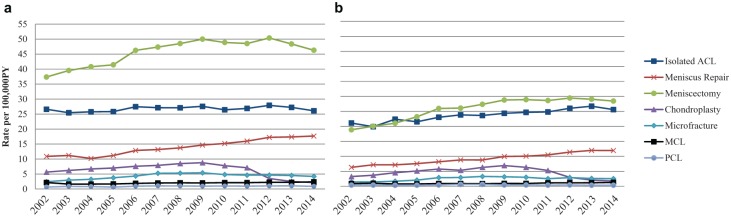
For males, rates of isolated ACL reconstruction appeared relatively stable (Figure 4a); however, rates of isolated ACL reconstruction increased 21% among females from 21.1 per 100,000 PYs in 2002 to 25.6 per 100,000 PYs in 2014 (Figure 4b). In 2014, rates of isolated ACL reconstruction were approximately similar for males and females (26.1 vs 25.6 per 100,000 PYs, respectively). Trends in other concomitant procedures performed were consistent between males and females, though males had higher absolute rates of concomitant procedures performed than females (Figure 4). Specifically, males had appreciably higher rates of ACL reconstruction with concomitant meniscal surgery than females (2014: 17.7 vs 11.9 per 100,000 PYs for meniscal repair and 46.3 vs 28.4 per 100,000 PYs for meniscectomy, respectively).
Figure 4.
Annual trends in incidence rate of anterior cruciate ligament (ACL) reconstruction with concomitant procedures per 100,000 person-years (PYs) comparing (a) males and (b) females among patients included in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014. MCL, medial collateral ligament; PCL, posterior cruciate ligament.
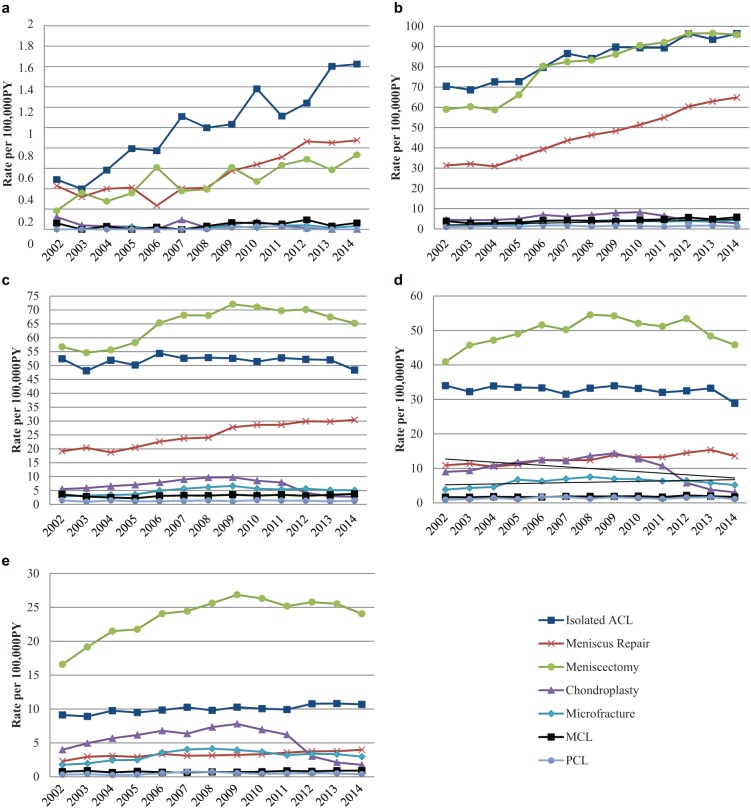
Among age strata, rates and trends of concomitant procedures performed varied widely (Figure 5). Rates of both isolated ACL reconstruction and ACL reconstruction with concomitant meniscal repair and/or concomitant mensicectomy increased substantially among children and adolescents (Figure 5, a and b, respectively). Among the same groups, rates of other concomitant procedures were low, in comparison. Although children younger than 13 years had low absolute rates of isolated ACL reconstruction, rates tripled from 0.49 per 100,000 PYs in 2002 to 1.62 per 100,000 PYs in 2014. Over the same time period, rates of concomitant meniscus repair doubled from 0.43 to 0.88 per 100,000 PYs and rates of concomitant meniscectomy quadrupled from 0.18 to 0.73 per 100,000 PYs among this age group. Children younger than 13 years were also the only age group where rates of concomitant meniscal repair were similar to or higher than rates of concomitant meniscectomy.
Figure 5.
Annual trends in incidence rate of anterior cruciate ligament (ACL) reconstruction with concomitant procedures per 100,000 person-years (PYs) comparing (a) <13-year-olds, (b) 13- to 17-year-olds, (c) 18- to 30-year-olds, (d) 31- to 40-year-olds, and (e) >40-year-olds included in the Truven Health Analytics MarketScan Commercial Claims and Encounters database 2002-2014. MCL, medial collateral ligament; PCL, posterior cruciate ligament.
Adolescents aged 13 to 17 years had the highest absolute rates of isolated ACL reconstruction and ACL reconstruction with concomitant meniscal repair. The rate of isolated ACL reconstruction increased 37% from 70.4 per 100,000 PYs in 2002 to 96.3 per 100,000 PYs in 2014 in this age group. ACL reconstructions with concomitant meniscal repair and those with concomitant meniscectomy had even greater increases. Concomitant meniscal repairs increased from 31.4 per 100,000 PYs in 2002 to 64.9 per 100,000 PYs in 2014 (107% increase), and concomitant meniscectomies increased from 59.0 per 100,000 PYs in 2002 to 95.9 per 100,000 PYs in 2014 (63% increase; Figure 5b).
Among adults aged 18 to 30 (Figure 5c), 31 to 40 (Figure 5d), and older than 40 years (Figure 5e), rates and trends of concomitant procedures were similar; however, adults aged 18 to 30 years had higher absolute rates of isolated ACL reconstruction (48.4 per 100,000 PYs vs 28.9 for patients 31-40 years and 10.7 for patients >40 years in 2014), and adults >40 years had the lowest rates of concomitant meniscal repair (4.0 per 100,000 PYs in 2014).
Discussion
This study provides an assessment of ACL reconstruction trends among commercially insured individuals in the United States that is more comprehensive than prior research.12-15 We observed increasing rates of ACL reconstruction since 2002. Across the study period, outpatient and arthroscopic ACL reconstruction rates increased, while inpatient ACL reconstruction rates decreased and open ACL reconstruction rates remained relatively stable. In terms of concomitant procedures, meniscal repair procedures increased appreciably over the study period. Isolated ACL reconstruction increased slightly overall; however, we noted larger increases in isolated ACL reconstructions among women and younger age groups.
A population-based study of the incidence of ACL reconstructions was recently performed using the National Hospital Discharge Survey (NHDS) and the National Survey of Ambulatory Surgery (NSAS) in 1994, 1995, 1996, and 2006.15 The incidence of ACL reconstruction had increased over the time period from approximately 32.9 reconstructions per 100,000 PYs to 43.5 reconstructions per 100,000 PYs.15 The rate of ACL reconstruction in our sample showed a similar increase; however, the incidence rates in our study were much higher at 61.4 per 100,000 PYs in 2002 to 74.6 per 100,000 PYs in 2014. A direct comparison of the rates observed in 2006 also suggests that rates may be much higher among the commercially-insured patient population compared with individuals sampled in the NHDS and NSAS, with our analysis yielding a rate of 71.8 reconstructions per 100,000 PYs in 2006 compared with 43.5 reconstructions per 100,000 PYs in the previous study for the same year.
Another previous study using the Nationwide Inpatient Sample from 2003 to 2011 found that inpatient ACL reconstructions represented approximately 7% of ACL reconstructions performed in the United States, and the annual incidence of inpatient ACL reconstructions was decreasing over time.2 Our results support this finding, with approximately an 86% decrease in the incidence rate of inpatient ACL reconstruction identified from 2002 to 2014. The NSAS was also used to study the trends of all outpatient knee arthroscopies in the United States between 1996 and 2006 and found a corresponding increase in the proportion of ACL reconstructions performed in the outpatient setting.12 Similarly, our results suggest an increase in both outpatient and arthroscopic procedures that highlights the shift in the standard-of-care for ACL reconstruction in recent years.
We noted increases in meniscal procedures over time, particularly meniscal repairs, and especially among younger age groups. Another study analyzed trends of ACL reconstruction with concomitant meniscal procedures reported to the American Board of Orthopaedic Surgery.19 Similar to our study, that study showed an increase in rate of meniscal procedures, including repair and meniscectomy, performed at the time of ACL reconstruction. Our study findings are also consistent with a previous study from the MOON cohort that reported a relatively high proportion of concomitant meniscus pathology, with 36% of reconstructions having a medial meniscus tear and 44% having a lateral meniscus tear.6 In that study, meniscectomy was also more commonly performed than meniscal repair. Interestingly, males had much higher rates of concomitant meniscal surgery than females in our study. This may indicate a difference in treatment or a difference in injury type and severity between groups. Given the association between meniscal pathology and long-term joint health,5 further research into this topic is warranted.
Of special concern are the rates of isolated ACL reconstruction and ACL reconstruction with concomitant meniscal treatment among children and adolescents, both of which increased substantially. This finding is consistent with a recently published brief report among this same population noting a dramatic increase in ACL reconstructions, particularly among 13- to 17-year-olds.9 Adding to the findings from the previously published report, the data presented here suggest that not only are ACL reconstructions increasing, but treatment of concurrent meniscal pathology is also increasing. It is possible that advances in surgical procedures have led to increased utilization of meniscal preservation procedures. Alternatively, the severity of ACL injuries may be increasing over time because of higher and more intense levels of sports participation. Regardless, the increased incidence of concomitant meniscal treatment noted among younger age groups underscores the importance of injury prevention and further research on long-term outcomes after ACL reconstruction.
Our study also noted an increase in concomitant microfracture and decrease in concomitant chondroplasty procedures, which could represent an increase in propensity for performing cartilage restoration procedures to reduce the risk of posttraumatic osteoarthritis; however, the decrease in observed concomitant chondroplasty could be driven by a change in procedure coding and/or reimbursement by commercial insurance plans rather than a change in procedures performed. Specifically, in 2012, the guideline for meniscectomy reporting changed such that chondroplasty became inclusive with the CPT code for meniscectomy. Subsequently, the decrease in chondroplasties identified in our dataset may represent the fact that chondroplasty codes are no longer coded for reimbursement separately when performed with meniscectomy from 2012 onward. Furthermore, the increase in concomitant microfracture, as well as the increase in concomitant collateral ligament and PCL repairs or reconstructions, could also represent a change in practice patterns and increased comfort level with performing these challenging procedures at the time of ACL reconstruction over time.
These findings add to the existing literature on the epidemiology of ACL reconstruction in the United States. Given the high volume and increasing incidence of ACL reconstruction procedures in the United States, coupled with the known association between ACL tear and posttraumatic osteoarthritis,4,17,18,22 a renewed focus on research on both ACL injury prevention and optimal clinical care should be prioritized. Additionally, the long-term impact of these increases in children and adolescents is highly concerning. A growing body of literature demonstrates the progression to osteoarthritis and other functional limitations after ACL injury.4,17,18,22 Thus, there is a need for research on optimizing long-term patient outcomes and limiting health care costs for patients who sustain an ACL injury in their adolescent years.
Strengths and Limitations
The current study provides a comprehensive assessment of multiple aspects of ACL reconstruction, including analysis of arthroscopic and open ACL reconstructions, inpatient and outpatient ACL reconstructions, and concomitant procedures performed, in addition to analyzing trends across age and sex. This study also improves on methods used for analyzing incidence rates in an insurance claims database by using person-months at risk as the denominator in our rate calculation, which accounts for the variable number of participants contained in the database over time. However, this study is not without limitations. The primary limitation relates to generalizability of the results, as the study only includes commercially insured individuals in the United States. Therefore, inference cannot be made to uninsured or publicly insured patients. However, it is important to note that a previous study found the distribution of participants included in the MarketScan database to be comparable to a nationally representative privately-insured population in the United States.1 There is potential for misclassification of cases in this study due to insurance claims reporting. Although no validation study has been performed for ACL reconstruction codes used in administrative databases, previous studies have suggested fairly high sensitivity, specificity, positive predictive value, and negative predictive value for orthopaedic procedures.21 Furthermore, the significance and expense related to an ACL reconstruction likely limits the potential for misclassification within an insurance claims database.
Conclusion
Incidence rates of isolated ACL reconstruction and rates of concomitant meniscal surgery have increased, particularly among children and adolescents. A renewed focus on adoption of injury prevention programs is needed to mitigate these trends. In addition, there is a need for research on long-term patient outcomes and postoperative health care utilization after ACL reconstruction, with a focus on understanding the sex disparity in concomitant meniscal surgery.
Footnotes
The following authors declared potential conflicts of interest: Mackenzie M. Herzog, MPH, and Jeffrey T. Spang, MD, are supported by a University of North Carolina at Chapel Hill Junior Faculty Development Award, and Stephen W. Marshall, PhD, is supported by grants from the Department of Defense and the National Institutes of Health.
References
- 1. Aizcorbe A, Liebman E, Pack S, Cutler DM, Chernew ME, Rosen AB. Measuring health care costs of individuals with employer-sponsored health insurance in the U.S.: a comparison of survey and claims data. Stat J IAOS. 2012;28:43-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bates NA, McPherson AL, Rao MB, Myer GD, Hewett TE. Characteristics of inpatient anterior cruciate ligament reconstructions and concomitant injuries. Knee Surg Sports Traumatol Arthrosc. 2016;24:2778-2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Commercial Claims and Encounters Medicare Supplemental Source: Truven Health MarketScan Research Databases. Data Year 2013 Edition. Ann Arbor, MI: Truven Health Analytics; 2013. [Google Scholar]
- 4. Dare D, Rodeo S. Mechanisms of post-traumatic osteoarthritis after ACL injury. Curr Rheumatol Rep. 2014;16:448. [DOI] [PubMed] [Google Scholar]
- 5. Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol. 2012;8:412-419. [DOI] [PubMed] [Google Scholar]
- 6. Fetzer GB, Spindler KP, Amendola A, et al. Potential market for new meniscus repair strategies: evaluation of the MOON cohort. J Knee Surg. 2009;22:180-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Flynn RK, Pedersen CL, Birmingham TB, Kirkley A, Jackowski D, Fowler PJ. The familial predisposition toward tearing the anterior cruciate ligament: a case control study. Am J Sports Med. 2005;33:23-28. [DOI] [PubMed] [Google Scholar]
- 8. Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44:2716-2723. [DOI] [PubMed] [Google Scholar]
- 9. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Incidence of anterior cruciate ligament reconstruction among adolescent females in the United States, 2002 through 2014. JAMA Pediatr. 2017;171:808-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jacobs JJ, King TR, Klippel JH, et al. Beyond the decade: strategic priorities to reduce the burden of musculoskeletal disease. J Bone Joint Surg Am. 2013;95:e1251-e1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Joseph AM, Collins CL, Henke NM, Yard EE, Fields SK, Comstock RD. A multisport epidemiologic comparison of anterior cruciate ligament injuries in high school athletics. J Athl Train. 2013;48:810-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994-1000. [DOI] [PubMed] [Google Scholar]
- 13. Leathers MP, Merz A, Wong J, Scott T, Wang JC, Hame SL. Trends and demographics in anterior cruciate ligament reconstruction in the United States. J Knee Surg. 2015;28:390-394. [DOI] [PubMed] [Google Scholar]
- 14. Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91:2321-2328. [DOI] [PubMed] [Google Scholar]
- 15. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42:2363-2370. [DOI] [PubMed] [Google Scholar]
- 16. Mather RC, 3rd, Koenig L, Kocher MS, et al. Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95:1751-1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nelson F, Billinghurst RC, Pidoux I, et al. Early post-traumatic osteoarthritis-like changes in human articular cartilage following rupture of the anterior cruciate ligament. Osteoarthritis Cartilage. 2006;14:114-119. [DOI] [PubMed] [Google Scholar]
- 18. Nordenvall R, Bahmanyar S, Adami J, Mattila VM, Fellander-Tsai L. Cruciate ligament reconstruction and risk of knee osteoarthritis: the association between cruciate ligament injury and post-traumatic osteoarthritis. a population based nationwide study in Sweden, 1987-2009. PLoS One. 2014;9:e104681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Parker BR, Hurwitz S, Spang J, Creighton R, Kamath G. Surgical trends in the treatment of meniscal tears: analysis of data from the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2016;44:1717-1723. [DOI] [PubMed] [Google Scholar]
- 20. Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database and registry research in orthopaedic surgery: part I: claims-based data. J Bone Joint Surg Am. 2015;97:1278-1287. [DOI] [PubMed] [Google Scholar]
- 21. Singh JA, Kundukulam JA, Bhandari M. A systematic review of validated methods for identifying orthopedic implant removal and revision using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(suppl 1):265-273. [DOI] [PubMed] [Google Scholar]
- 22. vonPorat A Roos EM Roos H.. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wilder FV, Hall BJ, Barrett JP, Jr, Lemrow NB. History of acute knee injury and osteoarthritis of the knee: a prospective epidemiological assessment. The Clearwater Osteoarthritis Study. Osteoarthritis Cartilage. 2002;10:611-616. [DOI] [PubMed] [Google Scholar]