Abstract
Objective:
To justify and describe an integrated rehabilitation programme for patients with chronic low back pain prior to evaluation in a randomized controlled trial.
Method:
The Template for Intervention Description and Replication (TIDieR) checklist was used as a structural framework for the description of the integrated rehabilitation programme. As a part of the description, the Medical Research Council guidance, ‘Developing and evaluating complex interventions’, was used as a framework to justify the integrated rehabilitation programme.
Intervention description:
The integrated rehabilitation programme adopts a participatory biopsychosocial approach integrating inpatient activities supported by a multidisciplinary team and learning located within the patient’s own environment. The integrated rehabilitation programme comprises 3 weeks of inpatient stay and 11 weeks of home-based activities. The inpatient part of the programme consists of 38 clinical activities, some of them delivered more than once. The 38 clinical activities were described in an activity sheet developed for this purpose, combining five items from the TIDieR.
Conclusion:
An integrated rehabilitation programme for patients with chronic low back pain has been justified and described. The intervention description is currently being used for successful structuring and standardization of the content and delivery of the integrated rehabilitation programme in a randomized controlled trial.
Trail registration:
ClinicalTrials.gov: NCT02884466.
Keywords: Chronic low back pain, complex interventions, biopsychosocial model, TIDieR, medical research council (MRC) guidance
Introduction
Besides pain and disability, patients with chronic low back pain often experience psychosocial consequences affecting their social, leisure and work life.1–3 Recognition of the biopsychosocial consequences of disease in general4,5 led to the development of the biopsychosocial model.1,6–8 In multidisciplinary rehabilitation,7,9 where the consequences of disability are managed,7 the biopsychosocial model is widely accepted. Multidisciplinary rehabilitation of patients with chronic low back pain is considered a complex intervention carried out in a complex environment.10,11 Evaluation of complex interventions in randomized controlled trials is a major research area. Detailed published descriptions of interventions are needed as it enables implementation of the intervention into a real-life setting,12–14 it enables other researchers to replicate or build on research findings13,14 and it further enables reviewers to synthesize extant evidence.14,15 The Template for Intervention Description and Replication (TIDieR) checklist was developed to improve this issue.13
We developed an integrated rehabilitation programme adopting a participatory biopsychosocial approach and integrating inpatient activities supported by a multidisciplinary team and learning located in the patient’s own environment. The aim of this article is to justify and describe the integrated rehabilitation programme in detail prior to a randomized controlled trial (ClinicalTrials.gov: NCT02884466).
Intervention description
The TIDieR checklist13 was used to structure the detailed description of the integrated rehabilitation programme.
Item 1. Brief name
An integrated rehabilitation programme alternating between inpatient stays and home-based activities in patients with chronic low back pain.
Item 2. Why: describe rational and theory essential to the intervention
The integrated rehabilitation programme was justified using a systematic iterative model developed by the British Medical Research Council for developing and evaluating complex interventions.16,17 Patients, providers, administrators and managers were continuously involved18 in the development and piloting stages. The development stage consists of three steps: (1) identifying the evidence base, (2) identifying/developing theory and (3) modelling process and outcomes.16,17
In the first step, 55 randomized controlled trials were identified as the existing evidence base. In total, 53 studies were included in a Cochrane review on multidisciplinary biopsychosocial rehabilitation for chronic low back pain.1 The Cochrane review found rehabilitation to be more effective than usual care (moderate quality evidence) and physical treatments (low quality evidence) in reducing long-term pain and disability in patients with chronic low back pain.1 The effect for pain and disability were generally larger in the short and medium term than in the long term.1 An updated literature search identical to the Cochrane review1 was performed, and further two studies were included in the evidence base;19,20 this did not alter the conclusion of the Cochrane review.1 In total, 5 of the 55 studies20–24 assessed a rehabilitation programme with subsequent booster sessions. Two of the five studies21,22 assessed an inpatient rehabilitation programme with booster sessions; of these, only one study compared two inpatient rehabilitation programmes, one of which included booster sessions.22 This study22 compared a three-week orthopaedic inpatient rehabilitation programme with two four-week multidisciplinary inpatient rehabilitation programmes, one of which included seven subsequent telephone booster sessions. Significant advantages in favour of the multidisciplinary programmes were found on pain coping strategies. However, no difference was found on disability or between the two multidisciplinary programmes.22
In the second step, the theoretic foundation of the integrated rehabilitation programme was based on a biopsychosocial rehabilitation model and approach7,11,25,26 and the Chronic Care Model.27–30 Following the development of the biopsychosocial model, multidisciplinary rehabilitation programmes that target the biopsychosocial aspects of chronic low back pain have been widely discussed and partly implemented.1,31 The International Classification of Functioning, Disability and Health (ICF)26 addresses the dimensions of disability9,26 and offers a framework for applying the biopsychosocial model to clinical practice, especially to multidisciplinary rehabilitation.7,9 An important aspect in biopsychosocial rehabilitation is the time the patients spend practicing and learning which assigns the patients a central role in managing their own health.7,25 Most activities are directly influenced by the context, and any process aiming at optimizing functioning must therefore take the patient’s environment into account.7 Thus, patients undergoing rehabilitation should practice in the environment in which the activity takes place; this will mainly be in everyday life situations and contexts rather than in institutions. A multidisciplinary team can effectively manage the complex problems with regard to functioning and disability by assisting practicing and learning through expert assessment, identification of self-directed goals, advice regarding a suitable plan, teaching encouragement and providing feedback.7,11,25
The mind-set described above is concurrent with essential elements in the Chronic Care Model, developed to guide and encourage high-quality chronic care for a variety of chronic illnesses, healthcare settings and target populations.27 The Chronic Care Model pays attention to patient self-management and self-management support from skilled providers.27 Due to the long-time horizon and fluctuating course of most chronic diseases, regular interaction between patients and providers is required.27 Therefore, the Chronic Care Model emphasizes the importance of regularly scheduled booster sessions in order to assess response to therapy and self-management skills and adjust treatment,27 and in order to obtain information on functional status, identify potential barriers, check progress and reinforce patient efforts.28 Booster sessions are described to improve patient outcome and can be accomplished by, for example, scheduled return visits, telephone calls or emails.28,29 It is suggested that a context outside the traditional healthcare setting (e.g. the patients’ home) is more effective in the care of chronic diseases.30
In the third step, the processes and outcomes were modelled as recommended.32 As a result, the clinical activities were grouped into 10 key components delivered by the multidisciplinary team (see Table 1).
Table 1.
The 10 key components and the 38 clinical activities.
| Key component | Clinical activity |
|---|---|
| Clinical assessment | Physical assessment Psychosocial assessment |
| Motivation and change | Instruction in exercise app Introduction to rehabilitation Exercise theory Introduction to mindfulness Involvement of relatives Motivation and anchoring The next step |
| Pain knowledge and management | Chronic pain and chronic back pain Experiences with pain Knowledge about pain Knowledge about analgesic medicine Living with pain |
| Multidisciplinary intervention | Welcome meeting Multidisciplinary conference Open counselling Midterm evaluation |
| Exercise and physical activity | Aqua gymnastic Circuit training Intro electric bicycle Exercise capacity training Healthy feet Closing activity |
| Individual counselling | Individual nurse counselling Individual physiotherapy counselling Individual occupational therapy counselling Individual dietary counselling Individual rheumatological counselling |
| Essential activity | Activity and health Balanced activity Activity and social relations Lifelong activity |
| Activities of daily living | Sleep House and garden |
| Nutrition and weight loss | Permanent weight loss strategies Healthy lifestyle |
| Individual exercise | Individual exercise |
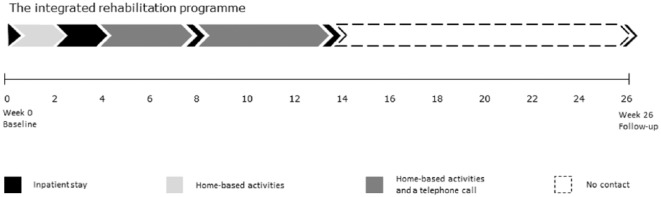
The 38 clinical activities from an existing rehabilitation programme were reorganized into the integrated rehabilitation programme. Thus, the clinical activities in the two programmes are identical; however, the two programmes differ in mode of delivery, with the existing rehabilitation programme being a 4-week inpatient programme and the integrated rehabilitation programme being a 14-week programme alternating between in total 3 weeks of inpatient activities and 11 weeks of home-based activities (see Figure 1). The two programmes will be compared in a randomized controlled trial.
Figure 1.
The integrated rehabilitation programme consists of (1) a pre-admission day, (2) 2 weeks of home-based activities, (3) 2 weeks of inpatient programme, (4) 4 weeks of home-based activities, (5) two days of inpatient programme, (6) 6 weeks of home-based activities, (7) two days of inpatient programme and (8) 26-week follow-up.
To summarize the development stage: despite a large body of literature on multidisciplinary biopsychosocial rehabilitation and chronic low back pain, there is a lack of evidence supporting how to maintain the best long-term effect of a rehabilitation programme. Furthermore, evidence regarding the effectiveness of continuous integration of learning into the patient’s own environment underpinned and aided by inpatient booster sessions delivered by a multidisciplinary team is lacking. Based on the evidence base and the identified theoretic foundation,7,11,25–30 we assumed that a rehabilitation programme integrating inpatient stays supported by a multidisciplinary team and home-based activities would allow for a high degree of learning. When at home, the patients will be able to integrate what they have learned while being inpatient into activities and participation in interaction with their everyday life situations and environment. When inpatient, the patients’ experiences from home will be integrated in the inpatient rehabilitation process supported by a multidisciplinary team. We hypothesized this integration of inpatient stays, and home-based activities would improve rehabilitation efforts and optimize long-term effect. The hypothesis was in accordance with clinical experiences and requests from patients, providers, administrators and managers.
The piloting stage consists of three steps: (1) testing procedures, (2) estimating recruitment/retention and (3) determining sample size.16,17 In the first step, the procedures were tested. This lead to fine-tuning of administrative and practical procedures, for example, permanent overbooking each week as two to three patients in every group postponed their appointments.
In the second step, recruitment/retention was estimated deeming the number of eligible patients, and the intended willingness to participate was large enough to recruit a sufficient number of patients. In the third step, sample size was estimated resulting in a planned recruitment of 160 patients. Altogether, information obtained from the development and piloting stages comprised the rationale justifying the evaluation of the integrated rehabilitation programme.
Item 3. What (materials)
The facilities include classrooms, learning labs (e.g. a fully equipped kitchen), conversation rooms, a small hot water pool and indoor and outdoor fitness facilities with cardio exercise equipment and strength training equipment.
A welcome pamphlet describing the clinical activities and a pamphlet containing individualized preparation material focusing on facilitation of goal setting as well as physical and mental preparation before the next inpatient stay are provided.
Item 4. What (procedures)
The 38 clinical activities addressing different components in the ICF model were grouped into 10 key components (Table 1). Activity sheets describing the clinical activities are provided as a supplementary file. See Table 2 for an example of an activity sheet.
Table 2.
Example of an activity sheet developed to describe the clinical activities.
| What (procedures) | Aqua gymnastic Aerobe and anaerobe exercises as well as exercises focusing on mobility and stability/balance |
|
| Tailoring | The exercises are chosen and adjusted based on the individual patient | |
| Who provided | Physiotherapist | |
| How | Group session | |
| When and how much | Number of sessions | Supervised: four sessions Non-supervised: six sessions |
| Duration | 30 minutes including warm-up and cool-down | |
| Intensity | Borg 11–15 | |
Item 5. Who provided
The multidisciplinary team consists of a rheumatologist, a nutritional counsellor, three nurses, three occupational therapists and six physiotherapists. The majority of the providers are trained in motivational interviewing. Other employees are administrative assistants, night-shift nurses, groundsmen, a chef, a cleaner and a daily manager, all in close contact with the patients. All providers have the required skills in delivering the clinical activities. See supplementary file for further details.
Item 6. How: modes of delivery
Patients will be contacted by phone at the time of visitation and four weeks before the pre-admission day. In addition, the welcome pamphlet (see item 3) will be emailed to the patients at this point. The integrated rehabilitation programme is delivered as a combination of theory and practice consisting of individual counselling, group sessions and lectures. Sessions are delivered face-to-face except for the non-supervised exercise. In order to assure support for the patients between the inpatient stays, a pamphlet (see item 3) and telephone calls once during each of the last two home periods (see Figure 1) will be used. Furthermore, patients are allowed to contact the providers online twice until the end of the 14-week programme. See supplementary file for further details.
Item 7. Where: type of location
The department under study is the Danish Rheumatism Association’s highly specialized multidisciplinary rehabilitation centre Sano Aarhus. Patients are referred from both rural and urban areas of Denmark based on a rheumatic or musculoskeletal disease and their ability and motivation to participate in a rehabilitation programme. The programme is tax-financed. A new group of six to eight patients is admitted each week, which means that approximately 28 patients divided between four groups are inpatient at the same time.
Item 8. When and how much
During the inpatient stays, 38 clinical activities are provided, some of them more than once. See supplementary file for further details.
Item 9. Tailoring
The integrated rehabilitation programme is partly standardized and partly patient-centred. Patient-centred rehabilitation requires tailoring of the programme to the individual patient. Tailoring occurs (1) during the multidisciplinary conference including the identification of self-directed goals,33 (2) in the individual counselling and (3) in the exercise and physical activity sessions. Therefore, what the patients actually receive differs as a result of tailoring the intervention to individual needs. See Table 1 and the supplementary file for further details.
Item 10. Modifications during the course of the study
An ongoing process evaluation34 is conducted in order to register modifications during the full-scale randomized controlled trial. Modifications will be reported in the evaluation study.
Item 11. How well (planned)
Attendance to inpatient stays, time between the inpatient stays and attendance to the clinical activities during inpatient stays are registered in each individual patient’s electronic health record.
Item 12. How well (actual)
Attendance will be reported in the evaluation study.
Discussion
An integrated rehabilitation programme for patients with chronic low back pain has been developed and described using the TIDieR. In order to justify the integrated rehabilitation programme, we embarked on a development and piloting process in accordance with the Medical Research Council guidelines.17 Identical to previous descriptions of complex interventions,35–37 we experienced difficulties integrating information from the development and piloting stage into the TIDieR framework. Therefore, a description of the development and piloting process was included in item 2 in order to provide evidence supporting and justifying the integrated rehabilitation programme. A transparent development and piloting process may lead to a better understanding of the possible mechanisms and effects of a rehabilitation programme.
The TIDieR was useful in providing a structured framework offering an opportunity to describe in detail the main characteristic of each of the 38 clinical activities comprising the integrated rehabilitation programme. In order to structure and standardize the description of the clinical activities, we developed an activity sheet. The activity sheet combines ‘What (procedures)’, ‘Who provided’, ‘How’, ‘When (and how much)’ and ‘Tailoring’ from the TIDieR. It is reasonable to use the activity sheet as the TIDieR does not reflect the order in which information should be presented.13 The Consensus on Exercise Reporting Template (CERT)12 is a valuable adjunct to or extension of the TIDieR when describing exercise interventions. For consistency, the CERT has harmonized its domains and the order of items with the TIDieR. In addition to the TIDieR, the CERT integrates precise information about the type of exercise, dosage, intensity, frequency and supervision/individualization.12 Inspired by the CERT, we incorporated the precise information needed for exercise interventions in the activity sheet.
The integrated rehabilitation programme is designed to integrate inpatient learning into the everyday life of patients with chronic low back pain. The strengths of the integrated rehabilitation programme are as follows. First is the adoption of a systematic and transparent approach using the Medical Research Council guidelines;16 this process ensured the overall approach of the integrated rehabilitation programme and proceeding to a full-scale study was justified. Second, the detailed description as recommended for complex interventions ensured implementation into a real-life clinical setting and replication in other contexts following the evaluation. Third, patients, providers, administrators and managers were continuously involved in the development, piloting and detailed description of the integrated rehabilitation programme, thereby ensuring commitment, broad support, engagement and ownership from all persons involved in the study.
Due to the complexity of the integrated rehabilitation programme it is difficult if not impossible to synthesis and justify the evidence supporting each of the 38 clinical activities.
It is a premise that a complete, detailed description of a complex intervention, that consists of multiple clinical activities, involves a multidisciplinary team, is partly tailored and is sensitive to the context, is impossible. The integrated rehabilitation programme was described to a level of detail that was found adequate, as the main function of the intervention is now clearly described.
The development, piloting and description of the Sano study was iterative and time-consuming, but necessary when aiming to minimise the risk that the research project would be a waste of time or unetichal or both. We cannot reject that the integrated rehabilitation programme could be identical to earlier rehabilitation programmes assessed in randomized controlled trials as most of the earlier studies lack detailed descriptions of their rehabilitation programme. The intervention description is currently being used for successful structuring and standardization of the content and delivery of the integrated rehabilitation programme in a randomized controlled trial.
Clinical messages.
An integrated rehabilitation programme integrating learning into the patient’s environment was justified and described in detail.
The Template for Intervention Description and Replication (TIDieR) checklist provided helpful recommendations for the reporting of a multidisciplinary rehabilitation programme.
An activity sheet combining five items from the TIDieR checklist and presenting the clinical activities was developed.
Supplemental Material
Supplemental material, Supplementary_Material for The Sano study: justification and detailed description of a multidisciplinary biopsychosocial rehabilitation programme in patients with chronic low back pain by Anne Mette Schmidt, Helle Terkildsen Maindal, Trine Bay Laurberg, Berit Schiøttz-Christensen, Charlotte Ibsen, Kirstine Bak Gulstad and Thomas Maribo in Clinical Rehabilitation
Acknowledgments
Helle Algren Brøgger and Gorm Høi Jensen are thanked for constructive discussions in the development of the integrated rehabilitation programme. The authors are grateful to all patients and providers who contributed to the development, piloting and description of the integrated rehabilitation programme, and to Sano for hosting the study. All authors have contributed substantially to (1) conception and design, or analysis and interpretation of data; (2) drafting or revising the article critically for important intellectual content; and (3) final approval of the version to be published.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by Aarhus University (grant number 19526435), the Danish Rheumatism Association (grant number R150-A4394-B1251) and Sano.
ORCID iD: Anne Mette Schmidt  https://orcid.org/0000-0002-3077-4985
https://orcid.org/0000-0002-3077-4985
References
- 1. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 2015; 350: h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Waddell G. Chapter 5. The epidemiology of back pain. In: Waddell G, Schoene M. (eds) The back pain revolution. 2nd ed. London: Churchill Livingstone, 2004, p.71. [Google Scholar]
- 3. Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol 2010; 24: 769–781. [DOI] [PubMed] [Google Scholar]
- 4. Statens Institut for Folkesundhed. Kapitel 7. Muskel- og skeletsygdomme. Folkesundhedsrapporten, Danmark 2007, http://www.si-folkesundhed.dk/upload/kap_7_muskel-_og_skeletsygdomme.pdf (accessed 13 October 2017).
- 5. Waddell G. Chapter 6. Risk factors for back pain. In: Waddell G, Schoene M. (eds) The back pain revolution. 2nd ed. London: Churchill Livingstone, 2004, p.91. [Google Scholar]
- 6. Chiarotto A, Deyo RA, Terwee CB, et al. Core outcome domains for clinical trials in non-specific low back pain. Eur Spine J 2015; 24: 1127–1142. [DOI] [PubMed] [Google Scholar]
- 7. Wade D. Rehabilitation – a new approach. Part two: the underlying theories. Clin Rehabil 2015; 29: 1145–1154. [DOI] [PubMed] [Google Scholar]
- 8. Pincus T, Kent P, Bronfort G, et al. Twenty-five years with the biopsychosocial model of low back pain – is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine (Phila Pa 1976) 2013; 38: 2118–2123. [DOI] [PubMed] [Google Scholar]
- 9. Waddell G. Chapter 14. The biopsychosocial model. In: Waddell G, Schoene M. (eds) The back pain revolution. 2nd ed. London: Churchill Livingstone, 2004, p.265. [Google Scholar]
- 10. Wade DT, Smeets RJ, Verbunt JA. Research in rehabilitation medicine: methodological challenges. J Clin Epidemiol 2010; 63: 699–704. [DOI] [PubMed] [Google Scholar]
- 11. Wade D. Rehabilitation – a new approach. Part three: the implications of the theories. Clin Rehabil 2016; 30: 3–10. [DOI] [PubMed] [Google Scholar]
- 12. Slade SC, Dionne CE, Underwood M, et al. Consensus on Exercise Reporting Template (CERT): explanation and elaboration statement. Br J Sports Med 2016; 50(23): 1428–1437. [DOI] [PubMed] [Google Scholar]
- 13. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: Template for Intervention Description and Replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687. [DOI] [PubMed] [Google Scholar]
- 14. Yamato T, Maher C, Saragiotto B, et al. The TIDieR checklist will benefit the physiotherapy profession. Physiother Theor Pr 2017; 33: 267–268. [DOI] [PubMed] [Google Scholar]
- 15. Hoffmann TC, Oxman AD, Ioannidis JP, et al. Enhancing the usability of systematic reviews by improving the consideration and description of interventions. BMJ 2017; 358: j2998. [DOI] [PubMed] [Google Scholar]
- 16. The Medical Research Council. Developing and evaluating complex interventions: new guidance, http://www.mrc.ac.uk/documents/pdf/complex-interventions-guidance/ (accessed 13 October 2017).
- 17. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Richards D. The critical importance of patient and public involvement. In: Richards D, Hallberg I. (eds) Complex interventions in health: an overview of research methods. 1st ed Oxon and New York: Routledge, 2015, p.46. [Google Scholar]
- 19. Linden M, Scherbe S, Cicholas B. Randomized controlled trial on the effectiveness of cognitive behavior group therapy in chronic back pain patients. J Back Musculoskelet Rehabil 2014; 27: 563–568. [DOI] [PubMed] [Google Scholar]
- 20. Tavafian SS, Jamshidi AR, Mohammad K. Treatment of low back pain: randomized clinical trial comparing a multidisciplinary group-based rehabilitation program with oral drug treatment up to 12 months. Int J Rheum Dis 2014; 17: 159–164. [DOI] [PubMed] [Google Scholar]
- 21. Härkäpää K, Järvikoski A, Mellin G, et al. A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Part 1. Pain, disability, compliance, and reported treatment benefits three months after treatment. Scand J Rehabil Med 1989; 21: 81–89. [PubMed] [Google Scholar]
- 22. Mangels M, Schwarz S, Worringen U, et al. Evaluation of a behavioral-medical inpatient rehabilitation treatment including booster sessions: a randomized controlled study. Clin J Pain 2009; 25: 356–364. [DOI] [PubMed] [Google Scholar]
- 23. Bendix AE, Bendix T, Haestrup C, et al. A prospective, randomized 5-year follow-up study of functional restoration in chronic low back pain patients. Eur Spine J 1998; 7: 111–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Monticone M, Ferrante S, Rocca B, et al. Effect of a long-lasting multidisciplinary program on disability and fear-avoidance behaviors in patients with chronic low back pain: results of a randomized controlled trial. Clin J Pain 2013; 29: 929–938. [DOI] [PubMed] [Google Scholar]
- 25. Wade D. Rehabilitation – a new approach. Part four: a new paradigm, and its implications. Clin Rehabil 2016; 30: 109–118. [DOI] [PubMed] [Google Scholar]
- 26. Stucki G, Cieza A, Melvin J. The International Classification of Functioning, Disability and Health (ICF): a unifying model for the conceptual description of the rehabilitation strategy. J Rehabil Med 2007; 39: 279–285. [DOI] [PubMed] [Google Scholar]
- 27. Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001; 20: 64–78. [DOI] [PubMed] [Google Scholar]
- 28. Von Korff M, Gruman J, Schaefer J, et al. Collaborative management of chronic illness. Ann Intern Med 1997; 127: 1097–1102. [DOI] [PubMed] [Google Scholar]
- 29. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q 1996; 74: 511–544. [PubMed] [Google Scholar]
- 30. Dunn P, Conard S. Chronic Care Model in research and in practice. Int J Cardiol 2018; 258: 295–296. [DOI] [PubMed] [Google Scholar]
- 31. Wade DT, Halligan PW. The biopsychosocial model of illness: a model whose time has come. Clin Rehabil 2017; 31: 995–1004. [DOI] [PubMed] [Google Scholar]
- 32. Sermeus W. Modelling process and outcomes in complex interventions. In: Richards D, Hallberg I. (eds) Complex interventions in health: an overview of research methods. 1st ed Oxon and New York: Routledge, 2015, p.111. [Google Scholar]
- 33. Feeley N, Cossette S. Testing the waters: piloting a complex intervention. In: Richards D, Hallberg I. (eds) Complex interventions in health: an overview of research methods. 1st ed Oxon and New York: Routledge, 2015, p.166. [Google Scholar]
- 34. Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015; 350: h1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cunningham P, Turton AJ, Van Wijck F, et al. Task-specific reach-to-grasp training after stroke: development and description of a home-based intervention. Clin Rehabil 2016; 30: 731–740. [DOI] [PubMed] [Google Scholar]
- 36. Van Vliet P, Hunter SM, Donaldson C, et al. Using the TIDieR checklist to standardize the description of a functional strength training intervention for the upper limb after stroke. J Neurol Phys Ther 2016; 40: 203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Metzelthin S, Zijlstra G, Rossum E, et al. ‘Doing with …’ rather than ‘doing for …’ older adults: rationale and content of the ‘Stay Active at Home’ programme. Clin Rehabil 2017; 31: 1419–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_Material for The Sano study: justification and detailed description of a multidisciplinary biopsychosocial rehabilitation programme in patients with chronic low back pain by Anne Mette Schmidt, Helle Terkildsen Maindal, Trine Bay Laurberg, Berit Schiøttz-Christensen, Charlotte Ibsen, Kirstine Bak Gulstad and Thomas Maribo in Clinical Rehabilitation