Abstract
Background
Transversus abdominis plane (TAP) block can provide effective analgesia for abdominal surgery. However, many randomized controlled trials (RCTs) have shown controversial results in hysterectomy. We conducted a meta-analysis of RCTs to investigate the effectiveness of TAP block after hysterectomy.
Methods
Studies were gathered from PubMed, MEDLINE, EMBASE, Cochrane Library, Web of Science, and ClinicalTrials.gov databases up to March 2018. RCTs involving TAP blocks in women undergoing hysterectomy were selected. The primary outcome of mean 24 hours morphine consumption and other outcomes, such as time to first request for analgesic, rest, and pain scores on movement at different times, and rates of nausea and vomiting, were compared between TAP block and no or sham block groups.
Results
A total of 841 participants were included in the 13 selected RCTs. Compared with no or sham blocks, TAP block reduced mean 24-hour morphine consumption in abdominal hysterectomy (AH) (weighted mean difference [WMD] −10.77 mg, P=0.04) but not in laparoscopic hysterectomy (LH)/robotic-assisted hysterectomy (RH) (WMD −1.39 mg, P=0.24). TAP block in AH prolonged analgesic time and reduced nausea and vomiting rates. TAP block also reduced the postoperative pain score at rest and on movement at different times in the AH subgroup, but it did not significantly reduce the postoperative pain score at rest, 6–8, and 24 hours, as well as the pain score on movement at 2, 6–8, and 24 hours in the LH/RH subgroup.
Conclusion
TAP block is an effective analgesic for AH. TAP block can reduce postoperative morphine consumption in AH and pain scores at rest and on movement for AH without increasing side effects. However, TAP block has limited analgesic effects for women undergoing LH/RH, as it does not reduce postoperative morphine consumption and pain scores at rest and on movement.
Keywords: TAP block, ultrasound-guided, hysterectomy, meta-analysis, abdominal, laparoscopic
Introduction
Hysterectomy is one of the common surgical procedures leading to severe postoperative pain in women.1 Poor pain control after hysterectomy is associated with increased length of stay and recovery, and it also has an impact on psychological changes, quality of life, and patient satisfaction.2 Adequate control of pain can prevent the development of chronic pain after hysterectomy.3 Opioids are routinely used to relieve postsurgical pain.4 However, the use of opioids will increase side effects, such as nausea and vomiting, as well as increase the risk of long-term abuse.5
Since the first description of the transversus abdominis plane (TAP) block in 2007,6 many studies have reported that TAP block is a useful strategy to reduce opioid consumption and support the management of postoperative pain for patients undergoing abdominal surgery, including hysterectomy.7–9 However, other studies have demonstrated that ultrasound-guided TAP block has no effects on pain control and postoperative opioid consumption after hysterectomy.10,11 Therefore, the effectiveness of TAP block for hysterectomy still remains controversial.
Although previous meta-analyses have shown that TAP block is safe and effective,12,13 these meta-analyses included abdominal surgery in general and were not specific for hysterectomy. There was a meta-analysis of TAP block for hysterectomy in 2013, but many new clinical trials have been conducted in recent years.14 Although another meta-analysis15 evaluated the analgesic and opioid-sparing effects of TAP block for elective hysterectomy, this study did not pool the result via subgroup analysis based on the type of surgery. To our knowledge, the abdominal incisions of abdominal and laparoscopic or robotic-assisted surgery are completely different, and TAP block was designed to anesthetize the nerves supplying the anterior abdominal wall.16 Therefore, it is necessary to further confirm the effect of TAP block in hysterectomy. Here, we conducted a meta-analysis of randomized controlled trials (RCTs) to determine the effectiveness and safety of TAP block after hysterectomy.
Methods
Search strategy
We applied the recommendations of the PRISMA statement.17 Literature searches were performed in the PubMed, MEDLINE, EMBASE, Cochrane Library, Web of Science, and ClinicalTrials.gov databases up to March 2018. The Medical Subject Headings (MeSH), common keywords, and their comprehensive combination included “transversus abdominis plane block” OR “TAP block” OR “transversus abdominis” OR “transverse abdominis” OR “transverse abdominis plane block” AND “hysterectomy” OR “hysterectomies”. Search results were limited to English.
Inclusion and exclusion criteria
Two authors (HZ and JP) performed the searches and independently reviewed and extracted data from each study. The search results were compared, and disagreements in opinions were resolved by further discussion. The inclusion criteria were as follows: 1) including women who underwent hysterectomy regardless of abdominal, laparoscopic, or robotic-assisted surgery; 2) including women who received TAP block pre- or postoperation; 3) being an RCT; and 4) being a comparative study between TAP block and sham or no block groups. Exclusion criteria were as follows: 1) being a nonrandomized study; 2) failing to focus on TAP block compared with sham block or no block; 3) being a case report, review paper, or unpublished literature; and 4) undergoing a surgery other than hysterectomy.
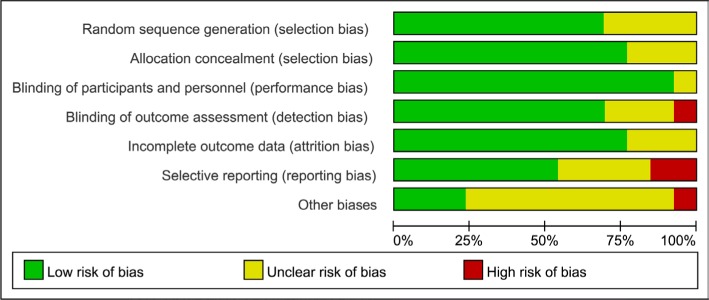
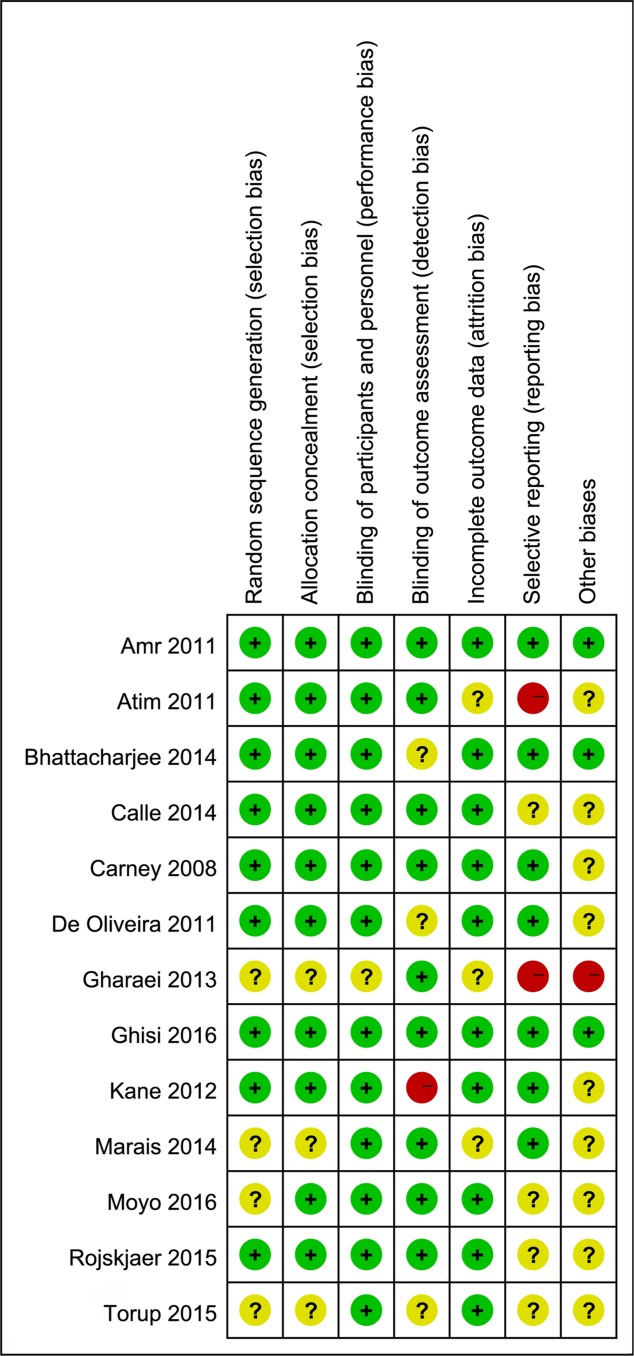
Risk of bias in studies
The Cochrane Collaboration tool was used to assess the risk of bias in the included studies, which included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases.
Data extraction
All data were extracted onto a standard form by HZ and JP: 1) characteristics of the studies, including year, name of author, group, and number of patients; 2) characteristics of study participants, including age and body mass index (BMI); 3) characteristics of hysterectomy, including surgical approach, anesthesia method, block timing, drugs used in the block, and pain assessment; 4) characteristics of outcome measures, including primary outcomes, such as mean 24-hour morphine consumption, and secondary outcomes, such as time to first request for analgesic, pain score at rest, and pain score on movement at different times postoperatively, including 2, 4, 6–8, 12, 24, and 48 hours between TAP group and control group, or TAP block combined with adjuvants group and TAP group, or preoperative group and postoperative group; and (5) adverse events, including nausea and vomiting. For the purpose of calculation, the VAS of 0–100 for pain intensity was converted to scales from 0 (no pain) to 10 (worst possible pain).18 As some studies evaluated pain score either at 6 or 8 hours postoperation, we merged the pain score at 6 and 8 hours to “6 to 8 hours” for this period. Data of mean values, SDs, standard errors (SEs), 95% CIs, number of events, and total number of participants were extracted from each study. If the literature only provided the median, range, and sample size, we calculated the mean values and SDs in accordance with previous study.19 In addition, data in charts were extracted by means of Engauge Digitizer 4.1. If the study included two groups of TAP block, the combined mean values and SDs were calculated according to the formula of the Cochrane Handbook for Systematic Reviews of Interventions, version 5.1.0.
Subgroup meta-analysis
Hysterectomy was carried out by abdominal hysterectomy (AH), laparoscopic hysterectomy (LH), or robotic-assisted hysterectomy (RH). The type of surgery performed will cause different results, and the LH and RH similarly use multiple small incisions. Therefore, we performed a subgroup meta-analysis to assess the effectiveness and adverse events between the TAP block group and the control group with regard to the type of surgery, as in a previous meta-analysis20 that included AH and LH/RH subgroups.
Statistical analysis
We conducted a meta-analysis when two or more trials reported similar outcomes. Results of meta-analysis were analyzed by Review Manager software, version 5.3 (Cochrane Collaboration, Oxford, UK). For dichotomous variables and continuous variables, the ORs and weighted mean differences (WMDs) were calculated, respectively, and reported with 95% CIs. I2 was used to evaluate heterogeneity with predetermined thresholds for low (25%–49%), moderate (50%–74%), and high (>75%) levels. The chi-squared test with significance set at P<0.10 was used to measure heterogeneity of the results among the included studies. The I2 statistics quantified the heterogeneity. Results were aggregated and analyzed using a fixed-effects model with I2<50%. If the I2statistic was higher than 50%, a random-effects analysis was performed. P<0.05 of a two-tailed test was considered to be statistically significant in all tests. Publication bias of included trials in our meta-analysis was evaluated via funnel plots.
Results
Literature search and quality assessment
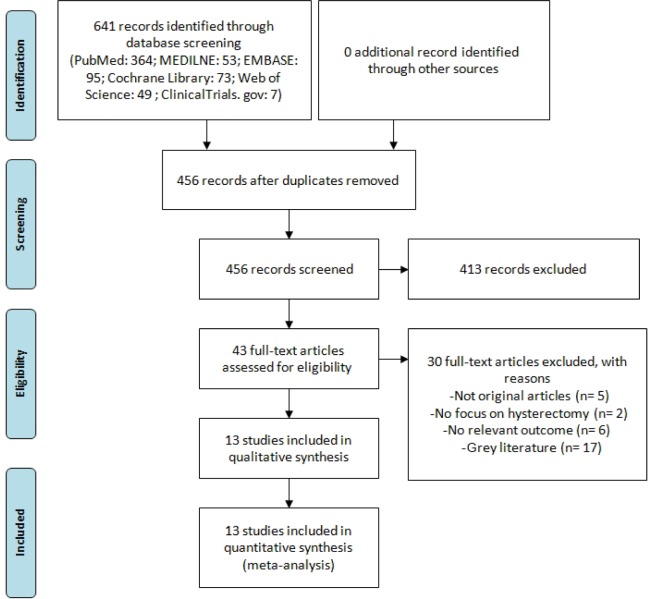
A total of 641 studies were identified after the initial search from PubMed (n=364), MEDLINE (n=53), EMBASE (n=95), Cochrane Library (n=73), Web of Science (n=49), and ClinicalTrials.gov (n=7) databases. After removing 185 duplicates, the titles and abstracts of 456 studies were screened. In total, 413 studies were excluded after records screening. The full texts of the remaining 43 articles were retrieved for full evaluation. At last, 13 prospective randomized controlled studies published from 2008 to 2016 were included for quantitative synthesis (Table 1).7,10,11,21–30 The flow diagram of study selection is summarized in Figure 1. Potential sources of methodological bias according to the Cochrane Collaboration Risk of Bias tool were evaluated in all the included studies and summarized in Figures 2 and 3. Overall, the majority of trials had a low risk of bias.
Table 1.
Characteristics of the included studies
| Year | Authors | Group (n) | Age (years) (mean or median) | BMI (kg/m2)/weight (kg) (mean or median) | Surgery | Anesthesia | Blocking time | Block solution | Pain assessment | Primary outcome |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| 2008 | Carney et al7 | TAP: 24, Sham: 26 | TAP: 54, Sham: 50 | TAP: 26, Sham: 27 | TAH | GA | Pre | 0.75% RP (1.5 mg/kg) | VAS (10) | MC |
| 2011 | Amr and Amin21 | TAP (pre): 23, TAP (post): 23, Sham: 22 | TAP (pre): 54, TAP (post): 52 Sham: 51 | TAP (pre): 80, TAP (post): 82, Sham: 82 | TAH | GA | Pre and post | 0.375% BP (20 mL) | VAS (100) | MC |
| 2011 | Atim et al22 | TAP: 18, Sham: 18, INF: 19 | TAP: 47, Sham: 44, INF: 40 | TAP: 71, Sham: 67, INF: 65 | TAH | GA | Post | 0.25% BP (20 mL) | VAS (10) | PP |
| 2011 | De Oliveira et al23 | TAP (0.25% RP): 21, TAP (0.5% RP): 22, Sham: 23 | TAP (0.25% RP): 46, TAP (0.5% RP): 45, Sham: 47 | TAP (0.25% RP): 27, TAP (0.5% RP): 25, Sham: 27 | LH | GA | Pre | (0.25%–0.5%) RP (20 mL) | NRS (10) | QoR-40 |
| 2012 | Kane et al10 | TAP: 28, NC: 28 | TAP: 46, NC: 44 | TAP: 31, NC: 30 | LH | GA | Pre | 0.5% RP+EP (20 mL) | VAS (100) | QoR-40 |
| 2013 | Gharaei et al24 | TAP: 21, NC: 21 | TAP: 64, NC: 65 | TAP: 71, NC: 72 | TAH | GA | Post | 0.2% RP (0.5 mg/kg) | VAS (10) | PP |
| 2014 | Bhattacharjee et al25 | TAP: 45, Sham: 45 | TAP: 46, Sham: 45 | TAP: 53, Sham: 53 | TAH | GA | Pre | 0.25% BP (0.5 mL/kg) | VAS (100) | PP |
| 2014 | Calle et al26 | TAP: 100, Sham: 97 | TAP: 44, Sham: 43 | TAP: 25, Sham: 26 | LH | GA | Post | 0.25% BP (20 mL) | VAS (10) | PP |
| 2014 | Marais et al27 | TAP: 15, Sham: 15 | TAP: 47, Sham: 48 | TAP: 25, Sham: 28 | TAH | GA | Pre | 0.25% BP (20 mL) | VAS (10) | MC |
| 2015 | Røjskjaer et al28 | TAP: 23, Sham: 23 | TAP: 49, Sham: 47 | TAP: 28, Sham: 25 | TAH | GA | Pre | 0.75% RP (20 mL) | VAS (100) | MC |
| 2015 | Torup et al29 | TAP: 34, Sham: 31 | TAP: 53, Sham: 57 | TAP: 24, Sham: 29 | RH | GA | Pre | 0.5% RP (20 mL) | VAS (100) | MC |
| 2016 | Ghisi et al11 | TAP: 22, NC: 22 | TAP: 46, NC: 48 | TAP: 59, NC: 61 | LH | GA | Pre | 0.375% LBP (20 mL) | NRS (10) | MC |
| 2016 | Moyo et al30 | TAP+Dxm: 16, Sham: 16 | TAP+Dxm: 41, Sham: 47 | TAP+Dxm: 24, Sham: 24 | AH | GA | Pre | 0.25 % BP (20 mL), Dxm (4 mg) | VAS (10) | PP |
Abbreviations: AH, abdominal hysterectomy; BP, bupivacaine; Dxm, dexamethasone; EP, epinephrine; GA, general anesthetic; INF, surgical site infiltration; LBP, levobupivacaine; LH, laparoscopic hysterectomy; MC, morphine consumption; NC, no block; PP, postoperative pain; Post, postoperation; Pre, preoperation; QoR-40, quality of recovery score; RH, robotic-assisted hysterectomy; RP, ropivacaine; SA, spinal anesthesia; Sham, sham block; TAH, total abdominal hysterectomy, TAP, transversus abdominis plane block; VAS, visual analogue scale; NRS, numerical rating scale.
Figure 1.
PRISMA flow diagram of study identification and selection process.
Note: Reproduced from PLoS Medicine (OPEN ACCESS) Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097.44
Figure 2.
Distribution of bias in the included trials.
Notes: Green = low risk of bias. Red = high risk of bias. Yellow = unclear risk of bias.
Figure 3.
Cochrane collaboration’s risk of bias summary: evaluation of risk of bias items for each included study.
Notes: Green = low risk of bias. Red = high risk of bias. Yellow = unclear risk of bias.
Characteristics of study participants
A total of 841 participants were included in the 13 RCTs selected. Among the 13 studies, women in eight studies7,21,22,24,25,27,28,30 underwent total or partial AH and women in five studies10,11,23,26,29 underwent LH/RH. All trials used standard general anesthesia. Nine studies7,10,11,23,25,27–30 performed TAP block preoperatively, and three studies22,24,26 performed TAP block postoperatively. One study21 compared the effects of preoperative and postoperative approaches to TAP block. Primary outcomes of the included studies were morphine consumption, postoperative pain, and quality of recovery score (QoR-40), and most included studies revealed no significant differences between groups regarding age and BMI or weight (Table 1).
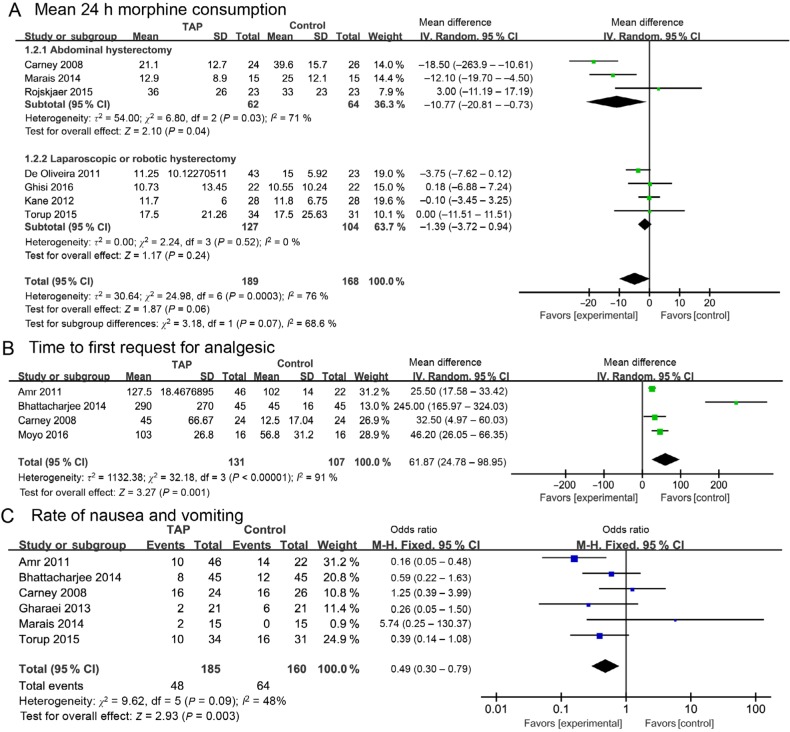
Effect of TAP block on analgesic after hysterectomy
Seven studies7,10,11,23,27–29 assessed the mean 24-hour morphine consumption for the effect of TAP block for hysterectomy. Compared with no or sham block, TAP block did not reduce mean 24-hour morphine consumption in any hysterectomy (WMD −4.80 mg, 95% CI −9.82 to 0.22 mg, P=0.07) with high heterogeneity (I2=76%). However, in subgroup analysis, TAP block in AH reduced mean 24-hour morphine consumption (WMD −10.77 mg, 95% CI −20.81 to −0.73 mg, P=0.04) with high heterogeneity (I2=71%). In addition, TAP block in LH/RH had no significant difference in mean 24-hour morphine consumption (WMD −1.39 mg, 95% CI −3.72 to 0.94 mg, P=0.24) with no heterogeneity (I2=0%) (Figure 4A). For women’s first request for analgesic after operation, the pooled result of four studies7,21,25,30 on TAP block in AH had a longer time than no block or sham block (WMD 61.87 minute, 95% CI 24.78 to 98.95 minute, P=0.001) with high heterogeneity (I2=91%) (Figure 4B).
Figure 4.
Forest plots of the effect of TAP block group vs control group.
Notes: (A) Mean 24-hour morphine consumption. (B) Time to first request for analgesic. (C) Rate of nausea and vomiting.
Abbreviations: h, hours; TAP, transversus abdominis plane.
Degree of pain of TAP block vs no or sham block
Pain score at rest for TAP block compared with no or sham block was assessed with the AH and LH/RH subgroups at 2 hours in nine trials,7,10,11,21,22,24,28–30 at 6–8 hours in eight trials,7,11,21,22,24,27–29 at 12 hours in three trials,7,21,24 at 24 hours in 10 trials,7,10,11,21–23,26–29 and at 48 hours in three trials.7,21,24 TAP block significantly reduced the pain score at rest at 2 hours (WMD −1. 41, 95% CI −2.57 to −0.26, P=0.002), at 6–8 hours (WMD −1.29, 95% CI −1.91 to −0.68, P<0.0001), at 12 hours (WMD −1.25, 95% CI −2.23 to −0.27, P=0.01), and at 48 hours (WMD −1.27, 95% CI −1.91 to −0.62, P=0.0001) postoperatively in the AH group compared with the control group with high heterogeneity (I2>50%) (Table 2). In the LH/RH subgroup, although TAP block significantly reduced the pain score at rest at 2 hours (WMD −0.83, 95% CI −1.52 to −0.14, P=0.02), it did not significantly reduce the pain score at rest at 6–8 hours (WMD −0.61, 95% CI −1.51 to −0.29, P=0.19) and 24 hours (WMD −0.64, 95% CI −1.45 to 0.16, P=0.12) with high heterogeneity (I2 >50%) (Table 2) (Figure S1).
Table 2.
Pain score results at different times of postoperation of TAP vs NC/SB
| Outcomes | Subgroup | Studies included | No. of patients (Exp/Con) | Weighed mean (95% CI) | P-value | Heterogeneity
|
|
|---|---|---|---|---|---|---|---|
| P-value | I2 test | ||||||
|
| |||||||
| Pain score at rest at 2 hours | AH | 6 | 148/126 | −1.41 (−2.57, −0.26) | 0.002 | <0.0001 | 97% |
| LH/RH | 3 | 84/84 | −0.83 (−1.52, −0.14) | 0.02 | 0.73 | 0% | |
| Pain score at rest at 6–8 hours | AH | 6 | 146/125 | −1.29 (−1.91, −0.68) | <0.0001 | <0.0001 | 91% |
| LH/RH | 2 | 56/53 | −0.61 (−1.51, 0.29) | 0.19 | 0.06 | 73% | |
| Pain score at rest at 12 hours | AH | 3 | 91/69 | −1.25 (−2.23, −0.27) | 0.01 | 0.05 | 67% |
| Pain score at rest at 24 hours | AH | 5 | 124/104 | −0.73 (−1.33, −0.14) | 0.02 | <0.0001 | 91% |
| LH/RH | 5 | 227/201 | −0.64 (−1.45, 0.16) | 0.12 | 0.0006 | 80% | |
| Pain score at rest at 48 hours | AH | 3 | 91/69 | −1.27 (−1.91, −0.62) | 0.0001 | 0.05 | 67% |
| Pain score on movement at 2 hours | AH | 5 | 127/105 | −1.91 (−3.30, −0.53) | 0.007 | <0.0001 | 98% |
| LH/RH | 2 | 56/53 | 0.22 (−0.62, 1.06) | 0.61 | 0.56 | 0% | |
| Pain score on movement at 6–8 hours | AH | 5 | 125/104 | −1.39 (−2.16, −0.63) | 0.0004 | <0.0001 | 91% |
| LH/RH | 2 | 56/53 | 0.98 (0.58, 1.38) | <0.0001 | 0.81 | 0% | |
| Pain score on movement at 12 hours | AH | 2 | 70/48 | −1.60 (−1.93, −1.28) | <0.0001 | 0.86 | 0% |
| Pain score on movement at 24 hours | AH | 5 | 124/104 | −1.12 (−1.91, −0.33) | 0.005 | <0.0001 | 93% |
| LH/RH | 2 | 56/53 | 0.11 (−0.68, 0.90) | 0.78 | 0.78 | 0% | |
| Pain score on movement at 48 hours | AH | 2 | 70/48 | −1.62 (−2.14, −1.10) | <0.0001 | 0.24 | 27% |
Abbreviations: AH, abdominal hysterectomy; Con, control group; Exp, experimental group; LH, laparoscopic hysterectomy; NC, no block; RH, robotic-assisted hysterectomy; SB, sham block; TAP, transversus abdominis plane block.
For pain score on movement, the pooled results of five trails7,21,22,28,30 for AH showed that TAP block significantly reduced when compared with the control group at 2 hours (WMD −1.91, 95% CI −3.30 to −0.53, P=0.007) with high heterogeneity (I2=98%). The pooled results of trials showed that TAP block significantly lowered the pain score on movement compared with the control group at 6–8 hours (WMD −1.39, 95% CI −2.16 to −0.63, P=0.0004), at 12 hours (WMD-1.60, 95% CI −1.93 to −1.28, P<0.0001), at 24 hours (WMD −1.12, 95% CI −1.91 to −0.33, P=0.005), and at 48 hours (WMD −1.62, 95% CI −2.14 to −1.10, P<0.0001). For the LH/RH subgroup, the pooled results of two trials at 2 and 24 hours showed no significant difference in the pain score on movement between TAP block and no or sham block at 2 hours (WMD 0.22, 95% CI −0.62 to 1.06, P=0.61; WMD 0.11, 95% CI −0.68 to 0.90, P=0.78). Moreover, TAP block showed a significantly higher pain score on movement than no or sham block at 6–8 hours (WMD 0.98, 95% CI 0.58 to 1.38, P<0.0001) with no heterogeneity (I2=0%) (Table 2) (Figure S1).
Side effects of TAP block for hysterectomy
Moreover, we investigated the side effects, such as the rate of nausea and vomiting, of TAP block. Six studies7,21,24,25,27,29 compared TAP block with no or sham block, and the rate of nausea and vomiting after operation was significantly lower than no or sham block with low heterogeneity (OR 0.49, 95% CI 0.30 to 0.79, P=0.003, I2=48%) (Figure 4C).
Sensitivity analysis
In order to confirm the effect of TAP block in the LH/RH subgroup, we conducted a sensitivity analysis on this subgroup. As we only included one study of RH, we evaluated the effect of TAP block in LH studies only. The results of mean 24-hour morphine consumption, pain score at rest at 2 hours and pain score at rest at 24 hours showed similar results for all the studies (Table 3).
Table 3.
Sensitivity analysis of studies for laparoscopic hysterectomy
| Outcomes | Studies included | References | No. of patients (Exp/Con) | Weighed mean (95% CI) | P-value | Heterogeneity
|
|
|---|---|---|---|---|---|---|---|
| P-value | I2 test | ||||||
|
| |||||||
| Mean 24-hour morphine consumption | 3 | 10,11,23 | 71/73 | −0.04 (−2.72, 2.64) | 0.98 | 1.00 | 0% |
| Pain score at rest at 2 hours | 2 | 10,11 | 50/50 | −1.00 (−1.81, −0.19) | 0.02 | 1.00 | 0% |
| Pain score at rest at 24 hours | 4 | 10,11,23,26 | 171/170 | −0.44 (−1.21, 0.23) | 0.20 | 0.04 | 64% |
Abbreviations: Con, control group; Exp, experimental group.
Publication bias
Representative funnel plots for the TAP block group vs control group including mean 24-hour morphine consumption, rest pain at 2 hours postoperatively, and rate of nausea and vomiting are shown in Figure 5. No significant publication bias was found (Figure 5). Funnel plots of other results are shown in Figure S2.
Figure 5.
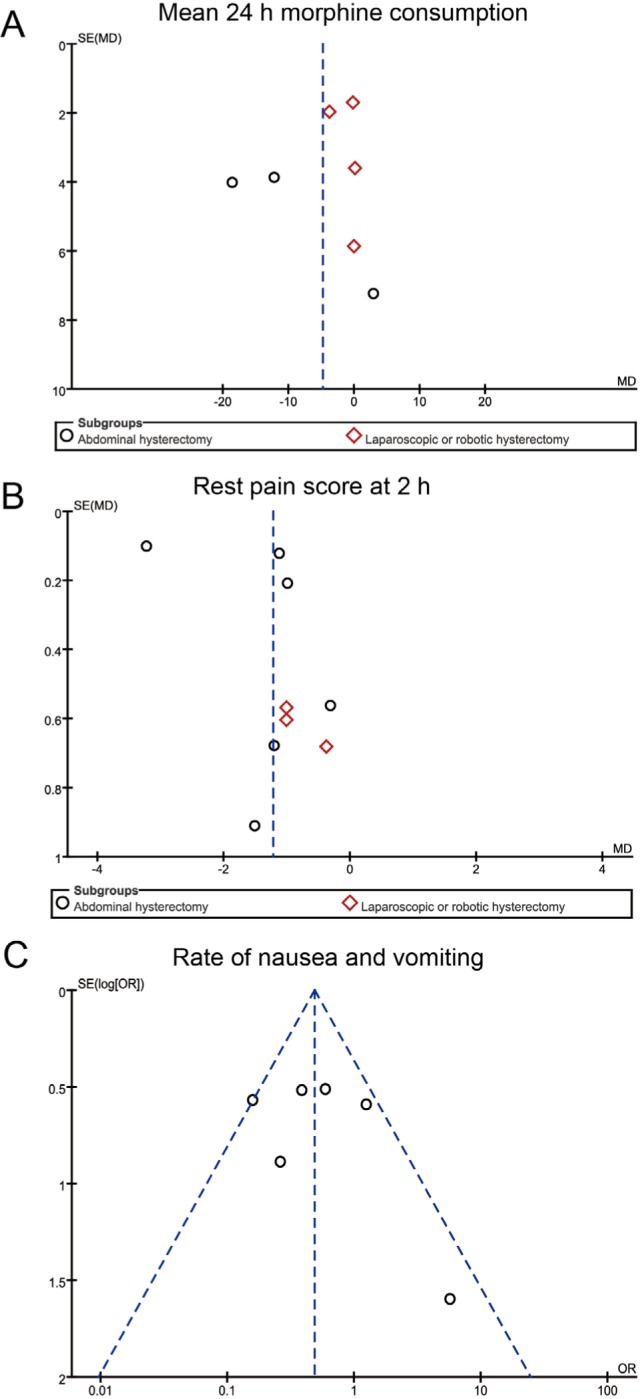
Representative funnel plots for TAP block group vs control group. Notes: (A) Mean 24-hour morphine consumption; (B) Rest pain score at 2 hours; (C) Rate of nausea and vomiting.
Abbreviations: h, hours; MD, mean difference; SE, standard error; TAP, transver-sus abdominis plane.
Discussion
We conducted a meta-analysis of RCTs to evaluate the analgesic effect of TAP block after hysterectomy. To our knowledge, this meta-analysis updated the current understanding of the effects of TAP block for hysterectomy. Compared with the previous meta-analysis of TAP block after hysterectomy,14 our meta-analysis included more studies and patients with different types of hysterectomy and further investigated morphine consumption at 24 hours and pain scores at rest and on movement at different times based on two subgroups, AH and LH/RH. In addition, we also reported the pooled results of the rate of nausea and vomiting with TAP block. Compared with the recent meta-analysis15 pointing out that the TAP can have moderate opioid-sparing effects after hysterectomy, we further confirmed that the TAP block can provide effective analgesia for AH. However, from our results, the effect of TAP block in LH/RH is limited.
Although the analgesic effect of TAP block has been confirmed in previous meta-analyses in several surgeries,14,15,31–35 the effects of TAP block in hysterectomy are still controversial. For women who underwent hysterectomy, although many studies had shown effective analgesia, we found some studies11,29 focusing on LH/RH that showed TAP block could not provide effective analgesia. Therefore, the evaluation of the effectiveness of TAP block for hysterectomy based on different surgical approaches is necessary. We used the result of mean 24-hour morphine consumption as the primary outcome to assess the analgesic effect of TAP block in different subgroups. The pooled results of different subgroups show that TAP may reduce mean 24-hour morphine consumption after hysterectomy with marginal significance. However, for further subgroup analysis, our results show that TAP block significantly reduced mean 24-hour morphine consumption and prolonged the time to first request for analgesic in AH only, and TAP block has limited effectiveness for participants who underwent LH or RH. Similarly, TAP block also significantly reduced the pain scores at rest and on movement postoperatively at different times in AH but not in LH or RH. In our pooled results, we demonstrated that TAP block did not reduce analgesic consumption in LH or RH.
The possible reason is that pain after hysterectomy mainly originates from somatic and visceral components, and TAP block is a peripheral nerve block technique that mainly reduces the pain from skin and muscle of the abdominal wall via blocking thoracolumbar nerves (T6-L1).29 Pain from the skin incisions in AH is considerably worse than that in LH or RH. Several studies36,37 have also demonstrated low VAS scores after LH or RH compared with open hysterectomy, indicating that LH or RH may be less painful because of smaller incisions and, to an extent, that the basic treatment with NSAIDs may be sufficient for LH or RH.29 Moreover, the TAP block is not believed to cover visceral pain, unless there is a systemic effect by absorption of the local anesthetics into the systemic circulation.38 This might be the reason why TAP block shows more of an analgesic effect in AHs compared with minimally invasive procedures. Therefore, our meta-analysis confirmed the result of the limited analgesic effect of TAP block in LH patients.
Some studies39,40 have been concerned whether TAP block will increase the rate of nausea and vomiting after hysterectomy. Interestingly, our pooled results showed that TAP block significantly reduced the rate of nausea and vomiting after the operation. This result is similar to the previous meta-analysis33 of TAP block performed in different abdominal surgeries. Nausea and vomiting and delayed recovery of bowel mobility after the operation are the main complications of opioid consumption. As TAP block significantly reduced pain levels and led to a reduction in postoperative opioid consumption, it can potentially reduce the side effects, such as nausea and vomiting. This result was also consistent with a previous study that found that TAP block did not affect the recovery of gastrointestinal function.41 For other outcomes, such as rehabilitation after operation and patient satisfaction, our included studies did not have sufficient data to pool the results. However, a current study42 reported that TAP block did not significantly reduce the time to ambulation after AH, and another retrospective study43 recently reported that TAP block did not reduce the total length of hospital stay. Moreover, postoperative QoR-40 was assessed for the effect of TAP block in LH, and the scores of comfort, emotions, and independence had no significant difference.11 Therefore, these current studies showed that TAP block is a safe method for hysterectomy but does not provide significant improvement in recovery of patients after hysterectomy. More RCT studies are still needed to evaluate the effect of TAP block in perioperative recovery outcomes after hysterectomy.
Despite some interesting findings, the results of our updated meta-analysis still have some limitations. First, although we set strict inclusion criteria and carried out subgroup analysis, the heterogeneities of some results remained high. Factors such as different doses and types of anesthetics and different postoperative analgesic methods may impact the heterogeneity of the meta-analysis. Second, more RCTs with larger sample sizes in these fields are still needed to strengthen the results of meta-analysis. Finally, because of limited outcomes of included studies, the effect of TAP block on the postoperative recovery of patients undergoing hysterectomy still needs to be further determined.
Conclusion
Our meta-analysis showed that TAP block is an effective analgesic for women who underwent AH. In addition, TAP block can reduce postoperative morphine consumption and pain scores at rest and on movement for AH. Also, TAP block will not increase the side effects of nausea and vomiting. However, TAP block has limited analgesic effects for women who underwent LH/RH, as it did not reduce postoperative morphine consumption and pain scores at rest and on movement. Overall, more RCTs with larger patient cohorts with perioperative recovery outcomes are still essential to further demonstrate the value of the robotic approach.
Supplementary materials
Forest plots of pain score at different times postoperation for TAP block group vs control group.
Note: (A) Rest pain score at 2 hours; (B) rest pain at 6–8 hours; (C) rest pain score at 12 hours; (D) rest pain score at 24 hours; (E) rest pain score at 48 hours; (F) movement pain score at 2 hours; (G) movement pain score at 6–8 hours; (H) movement pain score at 12 hours; (I) movement pain score at 24 hours; and (J) movement pain score at 48 hours.
Abbreviations: h, hours; TAP, transversus abdominis plane.
Funnel plots for TAP block group vs control group.
Note: (A) Time to first request for analgesic; (B) rest pain at 6–8 hours; (C) rest pain score at 12 hours; (D) rest pain score at 24 hours; (E) rest pain score at 48 hours; (F) movement pain score at 2 hours; (G) movement pain score at 6–8 hours; (H) movement pain score at 12 hours; (I) movement pain score at 24 hours; and (J) movement pain score at 48 hours.
Abbreviations: h, hours; TAP, transversus abdominis plane.
Acknowledgments
The authors thank Prof Chi Chiu Wang from Department of Obstetrics and Gynecology of the Chinese University of Hong Kong for the assistance in language edit.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wright JD, Herzog TJ, Tsui J, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122(2 Pt 1):233–241. doi: 10.1097/AOG.0b013e318299a6cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blanton E, Lamvu G, Patanwala I, et al. Non-opioid pain management in benign minimally invasive hysterectomy: a systematic review. Am J Obstet Gynecol. 2017;216(6):557–567. doi: 10.1016/j.ajog.2016.12.175. [DOI] [PubMed] [Google Scholar]
- 3.Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9(5):723–744. doi: 10.1586/ern.09.20. [DOI] [PubMed] [Google Scholar]
- 4.Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504. doi: 10.1001/jamasurg.2017.0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251. doi: 10.1136/bmj.g1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35(4):616–617. [PubMed] [Google Scholar]
- 7.Carney J, Mcdonnell JG, Ochana A, Bhinder R, Laffey JG. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107(6):2056–2060. doi: 10.1213/ane.0b013e3181871313. [DOI] [PubMed] [Google Scholar]
- 8.El Hachem L, Small E, Chung P, et al. Randomized controlled double-blind trial of transversus abdominis plane block versus trocar site infiltration in gynecologic laparoscopy. Am J Obstet Gynecol. 2015;212(2):182.e1–9. doi: 10.1016/j.ajog.2014.07.049. [DOI] [PubMed] [Google Scholar]
- 9.Hotujec BT, Spencer RJ, Donnelly MJ, et al. Transversus abdominis plane block in robotic gynecologic oncology: a randomized, placebo-controlled trial. Gynecol Oncol. 2015;136(3):460–465. doi: 10.1016/j.ygyno.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Kane SM, Garcia-Tomas V, Alejandro-Rodriguez M, Astley B, Pollard RR. Randomized trial of transversus abdominis plane block at total laparoscopic hysterectomy: effect of regional analgesia on quality of recovery. Am J Obstet Gynecol. 2012;207(5):419.e1–419.e5. doi: 10.1016/j.ajog.2012.06.052. [DOI] [PubMed] [Google Scholar]
- 11.Ghisi D, Fanelli A, Vianello F, et al. Transversus abdominis plane block for postoperative analgesia in patients undergoing total laparoscopic hysterectomy: a randomized, controlled, observer-blinded trial. Anesth Analg. 2016;123(2):488–492. doi: 10.1213/ANE.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 12.Ma N, Duncan JK, Scarfe AJ, Schuhmann S, Cameron AL. Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: a systematic review and meta-analysis. J Anesth. 2017;31(3):432–452. doi: 10.1007/s00540-017-2323-5. [DOI] [PubMed] [Google Scholar]
- 13.Sun N, Wang S, Ma P, Liu S, Shao A, Xiong L. Postoperative analgesia by a transversus abdominis plane block using different concentrations of ropivacaine for abdominal surgery: a meta-analysis. Clin J Pain. 2017;33(9):853–863. doi: 10.1097/AJP.0000000000000468. [DOI] [PubMed] [Google Scholar]
- 14.Champaneria R, Shah L, Geoghegan J, Gupta JK, Daniels JP. Analgesic effectiveness of transversus abdominis plane blocks after hysterectomy: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2013;166(1):1–9. doi: 10.1016/j.ejogrb.2012.09.012. [DOI] [PubMed] [Google Scholar]
- 15.Tubog TD. Opioid-sparing effects of transversus abdominis plane block in elective hysterctomy: a systematic review and meta-analysis. AANA J. 2018;86(1):41–55. [PubMed] [Google Scholar]
- 16.Gasanova I, Grant E, Way M, Rosero EB, Joshi GP. Ultrasound-guided transversus abdominal plane block with multimodal analgesia for pain management after total abdominal hysterectomy. Archives of gynecology and obstetrics. Jul. 2013;288(1):105–111. doi: 10.1007/s00404-012-2698-3. [DOI] [PubMed] [Google Scholar]
- 17.Schulz KF, Altman DG, Moher D. Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010;1(2):100–107. doi: 10.4103/0976-500X.72352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinto RZ, Maher CG, Ferreira ML, et al. Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis. Ann Intern Med. 2012;157(12):865–877. doi: 10.7326/0003-4819-157-12-201212180-00564. [DOI] [PubMed] [Google Scholar]
- 19.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baeriswyl M, Kirkham KR, Kern C, Albrecht E. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesth Analg. 2015;121(6):1640–1654. doi: 10.1213/ANE.0000000000000967. [DOI] [PubMed] [Google Scholar]
- 21.Amr YM, Amin SM. Comparative study between effect of pre- versus post-incisional transversus abdominis plane block on acute and chronic post-abdominal hysterectomy pain. Anesth Essays Res. 2011;5(1):77–82. doi: 10.4103/0259-1162.84199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atim A, Bilgin F, Kilickaya O, et al. The efficacy of ultrasound-guided transversus abdominis plane block in patients undergoing hysterectomy. Anaesth Intensive Care. 2011;39(4):630–634. doi: 10.1177/0310057X1103900415. [DOI] [PubMed] [Google Scholar]
- 23.De Oliveira GS, Jr, Milad MP, Fitzgerald P, Rahmani R, Mccarthy RJ. Transversus abdominis plane infiltration and quality of recovery after laparoscopic hysterectomy: a randomized controlled trial. Obstet Gynecol. 2011;118(6):1230–1237. doi: 10.1097/AOG.0b013e318236f67f. [DOI] [PubMed] [Google Scholar]
- 24.Gharaei H, Imani F, Almasi F, Solimani M. The effect of ultrasound-guided TAPB on pain management after total abdominal hysterectomy. Korean J Pain. 2013;26(4):374–378. doi: 10.3344/kjp.2013.26.4.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhattacharjee S, Ray M, Ghose T, Maitra S, Layek A. Analgesic efficacy of transversus abdominis plane block in providing effective perioperative analgesia in patients undergoing total abdominal hysterectomy: a randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2014;30(3):391–396. doi: 10.4103/0970-9185.137274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calle GA, López CC, Sánchez E, et al. Transversus abdominis plane block after ambulatory total laparoscopic hysterectomy: randomized controlled trial. Acta Obstet Gynecol Scand. 2014;93(4):345–350. doi: 10.1111/aogs.12351. [DOI] [PubMed] [Google Scholar]
- 27.Marais A, Porrill O, James MF, Dyer RA. The use of ultrasound-guided transversus abdominis plane blocks for total abdominal hysterectomy: a double-blind, controlled trial. South Afr J Anaesth Analg. 2014;20:117–121. [Google Scholar]
- 28.Røjskjaer JO, Gade E, Kiel LB, et al. Analgesic effect of ultrasound-guided transversus abdominis plane block after total abdominal hysterectomy: a randomized, double-blind, placebo-controlled trial. Acta Obstet Gynecol Scand. 2015;94(3):274–278. doi: 10.1111/aogs.12567. [DOI] [PubMed] [Google Scholar]
- 29.Torup H, Bøgeskov M, Hansen EG, et al. Transversus abdominis plane (TAP) block after robot-assisted laparoscopic hysterectomy: a randomised clinical trial. Acta Anaesthesiol Scand. 2015;59(7):928–935. doi: 10.1111/aas.12516. [DOI] [PubMed] [Google Scholar]
- 30.Moyo N, Madzimbamuto FD, Shumbairerwa S. Adding a transversus abdominis plane block to parenteral opioid for postoperative analgesia following trans-abdominal hysterectomy in a low resource setting: a prospective, randomised, double blind, controlled study. BMC Res Notes. 2016;9(1):50. doi: 10.1186/s13104-016-1864-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Charlton S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. . Cochrane Database Syst Rev. 2010(12):CD007705. doi: 10.1002/14651858.CD007705.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Ma N, Duncan JK, Scarfe AJ, Schuhmann S, Cameron AL. Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: a systematic review and meta-analysis. J Anesth. 2017;31(3):432–452. doi: 10.1007/s00540-017-2323-5. [DOI] [PubMed] [Google Scholar]
- 33.Hain E, Maggiori L, Prost À La Denise J, Panis Y. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis. Colorectal Dis. 2018;20(4):279–287. doi: 10.1111/codi.14037. [DOI] [PubMed] [Google Scholar]
- 34.Peng K, Ji FH, Liu HY, Wu SR. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract. 2016;25(3):237–246. doi: 10.1159/000444688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis. 2012;14(10):e635–e642. doi: 10.1111/j.1463-1318.2012.03104.x. [DOI] [PubMed] [Google Scholar]
- 36.O’Neill M, Moran PS, Teljeur C, et al. Robot-assisted hysterectomy compared to open and laparoscopic approaches: systematic review and meta-analysis. Archives of Gynecology and Obstetrics. May. 2013;287(5):907–918. doi: 10.1007/s00404-012-2681-z. [DOI] [PubMed] [Google Scholar]
- 37.Olsson JH, Ellstrom M, Hahlin M. A randomised prospective trial comparing laparoscopic and abdominal hysterectomy. British Journal of Obstetrics and Gynaecology. 1996;103(4):345–350. doi: 10.1111/j.1471-0528.1996.tb09740.x. [DOI] [PubMed] [Google Scholar]
- 38.Koppert W, Weigand M, Neumann F, et al. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesthesia and Analgesia. 2004;98(4):1050–1055. doi: 10.1213/01.ANE.0000104582.71710.EE. [DOI] [PubMed] [Google Scholar]
- 39.Wegner R, Akwar D, Guzman-Reyes S, et al. Evaluating the Adjuvant Effect of Dexamethasone to Ropivacaine in Transversus Abdominis Plane Block for Inguinal Hernia Repair and Spermatocelectomy: A Randomized Controlled Trial. Pain Physician. 2017;20(5):413–418. [PubMed] [Google Scholar]
- 40.Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: a systematic review. Reg Anesth Pain Med. 2012;37(2):193–209. doi: 10.1097/AAP.0b013e3182429531. [DOI] [PubMed] [Google Scholar]
- 41.Smith SR, Draganic B, Pockney P, et al. Transversus abdominis plane blockade in laparoscopic colorectal surgery: a double-blind randomized clinical trial. International Journal of Colorectal Disease. 2015;30(9):1237–1245. doi: 10.1007/s00384-015-2286-7. [DOI] [PubMed] [Google Scholar]
- 42.Yoshida T, Furutani K, Watanabe Y, Ohashi N, Baba H. Analgesic efficacy of bilateral continuous transversus abdominis plane blocks using an oblique subcostal approach in patients undergoing laparotomy for gynaecological cancer: a prospective, randomized, triple-blind, placebo-controlled study. British Journal of Anaesthesia. 2016;117(6):812–820. doi: 10.1093/bja/aew339. [DOI] [PubMed] [Google Scholar]
- 43.Dai C, Zhang K, Huang J. The Efficacy of Transversus Abdominis Plane Block for Abdominal Hysterectomy Post-operative Analgesia. Cureus. 2018;10(8):e3131. doi: 10.7759/cureus.3131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Forest plots of pain score at different times postoperation for TAP block group vs control group.
Note: (A) Rest pain score at 2 hours; (B) rest pain at 6–8 hours; (C) rest pain score at 12 hours; (D) rest pain score at 24 hours; (E) rest pain score at 48 hours; (F) movement pain score at 2 hours; (G) movement pain score at 6–8 hours; (H) movement pain score at 12 hours; (I) movement pain score at 24 hours; and (J) movement pain score at 48 hours.
Abbreviations: h, hours; TAP, transversus abdominis plane.
Funnel plots for TAP block group vs control group.
Note: (A) Time to first request for analgesic; (B) rest pain at 6–8 hours; (C) rest pain score at 12 hours; (D) rest pain score at 24 hours; (E) rest pain score at 48 hours; (F) movement pain score at 2 hours; (G) movement pain score at 6–8 hours; (H) movement pain score at 12 hours; (I) movement pain score at 24 hours; and (J) movement pain score at 48 hours.
Abbreviations: h, hours; TAP, transversus abdominis plane.