ABSTRACT
The aim of this experiment was to quantify physiological and perceptual responses to exercise with and without restrictive heat loss attire in hot and temperate conditions.
Ten moderately-trained individuals (mass; 69.44±7.50 kg, body fat; 19.7±7.6%) cycled for 30-mins (15-mins at 2 W.kg−1 then 15-mins at 1 W.kg−1) under four experimental conditions; temperate (TEMP, 22°C/45%), hot (HOT, 45°C/20%) and, temperate (TEMPSUIT, 22°C/45%) and hot (HOTSUIT, 45°C/20%) whilst wearing an upper-body “sauna suit”.
Core temperature changes were higher (P<0.05) in TEMPSUIT (+1.7±0.4°C.hr−1), HOT (+1.9±0.5°C.hr−1) and HOTSUIT (+2.3±0.5°C.hr−1) than TEMP (+1.3±0.3°C.hr−1). Skin temperature was higher (P<0.05) in HOT (36.53±0.93°C) and HOTSUIT (37.68±0.68°C) than TEMP (33.50±1.77°C) and TEMPSUIT (33.41±0.70°C). Sweat rate was greater (P<0.05) in TEMPSUIT (0.89±0.24 L.hr−1), HOT (1.14±0.48 L.hr−1) and HOTSUIT (1.51±0.52 L.hr−1) than TEMP (0.56±0.27 L.hr−1). Peak heart rate was higher (P<0.05) in TEMPSUIT (155±23 b.min−1), HOT (163±18 b.min−1) and HOTSUIT (171±18 b.min−1) than TEMP (151±20 b.min−1). Thermal sensation and perceived exertion were greater (P<0.05) in TEMPSUIT (5.8±0.5 and 14±1), HOT (6.4±0.5 and 15±1) and HOTSUIT (7.1±0.5 and 16±1) than TEMP (5.3±0.5 and 14±1).
Exercising in an upper-body sauna suit within temperate conditions induces a greater physiological strain and evokes larger sweat losses compared to exercising in the same conditions, without restricting heat loss. In hot conditions, wearing a sauna suit increases physiological and perceptual strain further, which may accelerate the stimuli for heat adaptation and improve HA efficiency.
KEYWORDS: Sauna suit, heat stress, thermoregulation, physiological strain, heat acclimation, training, restrictive heat loss, exercise
Introduction
Heat acclimation (HA) is an intervention undertaken for athletic [1,2] and occupational purposes [3,4], completed in the days or weeks prior to competition or undertaking physical work in heat stress. HA improves the capacity of an individual to dissipate heat via augmented sweating [5], increases the capacity for heat storage by reducing body temperature [6], and reduces the negative thermal sensations [7]. The benefits of HA include enhanced endurance performance [8,9], improved thermal comfort [10,11] and a reduction in the likelihood of heat illness [12,13]. The HA phenotype is induced across numerous integrated physiological systems, such as cardiovascular [14], neuromuscular [15], and at a cellular/molecular level [16], which occurs following repeated exposures to potentiating stimuli for adaptation (e.g. core temperature ≥38.5°C [17], increased skin temperature [18] and elevated sweat rates [19]).
Whilst notable experimental work has highlighted the benefits of utilising passive HA (e.g. resting in hot-dry or hot-humid conditions) [20–22], or by implementing thermal exposures, such as hot water immersion (HWI) [23,24], or sauna post-exercise [25], the most common and potentially most potent HA methods require exercise-heat stress [2]. A variety of HA protocols have been published ranging in durations of 4–20 days, utilising prolonged exposures (30-120-mins) typically in hot-dry or hot-humid conditions (∼40°C, 40% relative humidity [RH]) [26]. Accordingly, two fundamental criteria are required during HA to stress the body, which is achieved by raising and sustaining an elevated core (Tre) and skin temperature (Tskin), and promoting profuse sweating, which concomitantly provide a multitude of prominent physiological and perceptual adaptations [3].
Most HA interventions are completed within controlled environmental chambers, however, the duration of HA training, allied with logistical and financial issues, may limit the prescription of current laboratory HA protocols [1] and disrupt training quality prior to competition. These are likely reasons for only 15% of athletes undertaking a recognised HA intervention prior to the IAAF World Championships, in spite of hot climates being forecast [27]. A proposed method for inducing (should access to an environmental chamber not be possible), or enhancing the efficiency (by accelerating the attainment of necessary physiological stimuli for adaptation) of HA is the wearing of clothing/garments which restrict heat loss during exercise [28]. Wearing garments that inhibit evaporative heat loss such as vinyl suits, or by overdressing in regular clothing, attenuates the rate of heat dissipation in temperate training environments [28-31]. Inhibited heat loss results in a greater rate of heat storage during exercise and ultimately, elevations in physiological strain [29]. The elevation in Tre is a key stimuli for increasing Tskin and sweat output, with associated elevations in skin blood flow reducing blood pressure, elevating cardiovascular strain (e.g. heart rate), the initiation of cellular signalling and inducing thermal discomfort [32]. Greater physiological strain theoretically provides the necessary mechanisms to induce heat adaptation and may present an alternative strategy to be undertaken during normal training as opposed to that within simulated hot environments (e.g. within a chamber) or additional sessions (e.g. post-exercise HWI). Furthermore, the use of restrictive heat loss attire during typical HA within environmental chambers may provide an ergogenic benefit without the necessity of increasing exercise intensity, time and, or volume during important training periods (e.g. tapering), although investigation is required.
The primary aims of this experiment were to determine whether the wearing of an upper-body sauna suit during exercise in temperate conditions (22°C, 45% RH) would; 1) increase key potentiating stimuli for heat adaptation in comparison to exercising in regular clothing, and 2) whether these increases in temperate conditions were equivalent to exercise performed in a hot-dry environment replicating typical HA conditions (40°C, 20% RH). This study also aimed to 3) determine whether wearing an upper-body sauna suit in hot-dry conditions would enhance key potentiating stimuli required during heat acclimation. It was hypothesised that wearing a sauna suit in temperate conditions would elicit physiological strain equivalent to exercising in regular clothing in hot conditions, and that wearing the vinyl suit in hot conditions would provide a more rapid attainment of the necessary physiological strain to induce heat adaptation.
Methods
Participants
Ten moderately trained participants (6 males and 4 females; mean ± standard deviation [SD] age: 25 ± 3 years, mass: 69.44 ± 7.50 kg, stature: 175 ± 9 cm, body surface area 1.84 ± 0.13 m2, and body fat: 19.7 ± 7.6%) volunteered, after providing written informed consent. Participants had not exercised in hot conditions (>25°C) for >3 months, nor were they regular sauna, steam or hot bath users. Each participant abstained from strenuous exercise, caffeine and alcohol 24-hrs prior to each session. Food intake was restricted 2-hrs prior to exercise, normal diets were maintained throughout the study. Participants arrived euhydrated, as indicated by urine osmolality (Uosm) <700mOsm·kg−1 and specific gravity (Usg) <1.020 [33]. All female participants were taking oral contraceptive pills, beginning experimentation on day 2 of the pill phase, which occurred during the early-follicular phase (e.g. 3–5 days after the onset of menstruation) of their self-reported menstrual cycle, as verified by a questionnaire [34,35]. The study was conducted in accordance with the Institution's ethics and governance committee, and Declaration of Helsinki [36]. Exercise was terminated if Tre ≥39.7°C (zero incidence).
Experimental design
A randomised, repeated-measures design was adopted, with each participant visiting the laboratory on four occasions, 72-hrs apart to minimise any acclimation effect from repeated heat exposures. During each visit, following instrumentation and 15-mins passive rest in temperate laboratory conditions, participants cycled for 30-mins, replicating the onset of a typical isothermic HA protocol [37], within four conditions; temperate (TEMP: 22°C, 45% RH), temperate whilst wearing an upper-body sauna suit (TEMPSUIT: 22°C, 45% RH), hot (HOT: 45°C, 20% RH) and hot whilst wearing an upper-body sauna suit (HOTSUIT: 45°C, 20% RH). In addition to shorts, socks and shoes (plus sports bra for females), only an upper-body suit was worn to mitigate against excessive heat gain, whilst still ensuring that sites for maximal relative sweating and thus evaporation, remained restricted (i.e. back, forearm, axilla, chest, abdomen and buttocks) [38].
Exercise protocol
Each trial was completed inside a controlled environmental chamber, (WatFlow, TISS, Hampshire, UK). Participants cycled (Monark, 620 Ergomedic, Vansbro, Sweden) at a power output prescribed relative to body mass (2 W.kg−1 for 15-mins, then 1 W.kg−1 for the following 15-mins [37], as opposed to intensities relative to maximal oxygen uptake (V̇O2max), thus removing the requirement to undertake a V̇O2max test. During the TEMPSUIT and HOTSUIT trials, each participant wore a commercially available, upper-body vinyl sauna suit (Everlast, London, UK), to restrict evaporative heat loss throughout the 30-mins of exercise. Fluid ingestion was not permitted during the trials. Physiological and perceptual measures were recorded every 5-mins during the exercise protocol.
Physiological measures
On the first visit, skinfold thickness was calculated using calipers (Harpenden, Burgess Hill, UK) and a four site skin fold calculation [39], later body fat (%) was calculated from body density [40]. Stature and nude body mass (NBM) were measured using a stadiometer (Detecto Scale Company, Missouri, USA) and weighing scales (Adam Equipment Inc., Connecticut, USA [to the nearest 0.01 kg [±0.2%]]), respectively, with these data used to estimate body surface area (BSA) [41].
Hydration status was measured prior to each experimental session using a Pocket Pal-Osmo meter (Uosm: Vitech Scientific Ltd., West Sussex, UK) and light refractometer (Usg: Atago Co., Tokyo, Japan). Tre was continuously monitored using a single-use probe (Henleys Medical, Hertfordshire, UK) self-inserted 10 cm past the anal sphincter. Tskin was measured using telemetry thermistors (U-Type and Gen II transmitter, Eltek, UK) attached to the right-hand side of the body at the pectoralis major muscle belly (Tchest), lateral head of triceps brachii (Tarm), rectus femoris muscle belly (Tthigh) and lateral head of the gastrocnemius (Tcalf). Mean Tskin [42] and Tre:Tskin gradient were retrospectively calculated [43]. Heart rate (HR) was continuously monitored using a Polar 810i strap (Polar, Electro Oy, Kempele, Finland). Sweat rate was estimated by the difference in towel-dried NBM pre and post-exercise, corrected for time, urine output (zero incidence), but not metabolic or respiration losses, which were assumed negligible and similar between trials [44].
Perceptual measures
Ratings of perceived exertion (RPE [45]) from 6 (no exertion) to 20 (maximal exertion), thermal comfort (TC [46]) from 0 (comfortable) to 4 (very uncomfortable), and thermal sensation scale (TSS [47]) from 0 (unbearably cold) to 8 (unbearably hot), were assessed every 5-mins during exercise.
Statistical analyses
Data are reported as mean ± SD, and were assessed for normality and sphericity prior to further statistical analyses (SPSS, IBM version 22.0). Baseline measures of NBM, Uosm and Usg and calculated sweat rate during each trial were analysed using a 1-way ANOVA. Individual sites of peak Tchest, Tarm, Tthigh and Tcalf were also analsyed using a 1-way ANOVA between the four experimental conditions (TEMP, TEMPSUIT, HOT, HOTSUIT) as participants only wore an upper-body sauna suit covering only 60% of BSA. All other dependent variables were analysed using a 2-way repeated-measures ANOVA between the four experimental conditions (TEMP, TEMPSUIT, HOT, HOTSUIT) and seven time points (0-mins, 5-mins, 10-mins, 15-mins, 20-mins, 25-mins, 30-mins), with Bonferroni correction applied during post-hoc analysis. Whilst a 3-way ANOVA separating environmental conditions (TEMP and HOT) and clothing (suit and no suit) would theoretically present an additional level of analysis, this would not permit all comparisons (i.e. between HOT and TEMPSUIT), thus it was not utilised. This statistical approach also befits the research question whereby each experimental condition may be a strategy in its own right. Statistical significance was accepted as P<0.05. Effect sizes were estimated and meaningful differences evaluated for peak data using Cohen's d, with interpretation of data as; small = 0.2, moderate = 0.5, and large = 0.8 [48]. A-priori interpretation boundaries for meaningful physiological changes (Δ) were; ΔTre >0.20°C, ΔHR >5 b.min−1 and Δsweat rate >0.20 L.h−1, and >1 in scale scores for perceptual measures [11]. Pearson's product moment correlation coefficients were used to identify relationships between trials for peak physiological and perceptual measures.
Results
The physiological and perceptual measures during each trial are displayed within Table 1, whereas the differences between trials and their associated effect size are displayed within Table 2. Prior to commencing testing, no differences (P>0.05) were observed between conditions for Uosm (F = 0.3), Usg (F = 0.7) or NBM (F = 0.6) (Table 1).
Table 1.
Mean ± SD physiological and perceptual measures during each trial.
| TEMP | TEMPSUIT | HOT | HOTSUIT | |
|---|---|---|---|---|
| Rest measures | ||||
| Tre (°C) | 37.20 ± 0.36 | 37.17 ± 0.35 | 37.21 ± 0.42 | 37.18 ± 0.41 |
| Tskin (°C) | 30.72 ± 1.44 | 29.99 ± 0.54 | 29.42 ± 0.90 | 30.32 ± 0.82 |
| HR (b.min−1) | 70 ± 9 | 69 ± 12 | 71 ± 16 | 70 ± 11 |
| NBM (kg) | 69.45 ± 7.47 | 69.61 ± 7.50 | 69.28 ± 7.70 | 69.43 ± 7.40 |
| Uosm (mOsm·kg−1) | 350 ± 178 | 365 ± 197 | 371 ± 215 | 354 ± 197 |
| Usg | 1.011 ± 0.002 | 1.014 ± 0.005 | 1.012 ± 0.003 | 1.010 ± 0.004 |
| Exercise measures | ||||
| Peak Tre (°C) | 37.84 ± 0.34bcd | 38.02 ± 0.32ad | 38.11 ± 0.31ad | 38.33 ± 0.32abc |
| ΔTre (°C.hr−1) | 1.3 ± 0.3bcd | 1.7 ± 0.4ad | 1.9 ± 0.5ad | 2.3 ± 0.5abc |
| Peak Tskin (°C) | 33.06 ± 0.97cd | 33.41 ± 0.70cd | 36.53 ± 0.93abd | 37.68 ± 0.68abc |
| Mean Tre:Tsk (°C) | 5.3 ± 1.9cd | 5.5 ± 0.5cd | 2.8 ± 1.1ab | 1.7 ± 0.8ab |
| Peak HR (b.min−1) | 151 ± 20 cd | 155 ± 23d | 163 ± 18ad | 171 ± 18abc |
| Sweat rate (L.hr−1) | 0.56 ± 0.27bcd | 0.89 ± 0.24ad | 1.14 ± 0.48ad | 1.51 ± 0.52abc |
| Peak RPE | 14 ± 1cd | 14 ± 1d | 15 ± 1a | 16 ± 1ab |
| Peak TSS | 5.3 ± 0.5cd | 5.8 ± 0.5cd | 6.4± 0.5abd | 7.1 ± 0.5abc |
| Peak TC | 1 ± 1 | 2 ± 1 | 2 ± 1 | 3 ± 1abc |
Note; adifference vs. TEMP (P<0.05), bdifference vs. TEMPSUIT (P<0.05), cdifference vs. HOT (P<0.05), ddifference vs. HOTSUIT (P<0.05)
Table 2.
Mean ± SD differences between trials (effect size and correlation coefficient).
| TEMP vs. TEMPSUIT | TEMP vs. HOT | TEMP vs. HOTSUIT | TEMPSUITvs. HOT | TEMPSUITvs. HOTSUIT | HOT vs. HOTSUIT | |
|---|---|---|---|---|---|---|
| Peak Tre (°C) | 0.18 ± 0.11* (d = 0.5, r = 0.95) | 0.27 ± 0.13*† (d = 0.8, r = 0.93) | 0.50 ± 0.09*† (d = 1.5, r = 0.97) | 0.09 ± 0.19 (d = 0.3, r = 0.84) | 0.31 ± 0.14*† (d = 1.0, r = 0.92) | 0.23 ± 0.11*† (d = 0.7, r = 0.95) |
| ΔTre (°C.hr−1) | 0.41 ± 0.27*† (d = 0.4, r = 0.75) | 0.53 ± 0.36*† (d = 1.5, r = 0.69) | 1.02 ± 0.39*† (d = 2.5, r = 0.73) | 0.12 ± 0.39 (d = 0.4, r = 0.63) | 0.61 ± 0.36*† (d = 1.3, r = 0.77) | 0.49 ± 0.25*† (d = 0.8, r = 0.90) |
| Peak Tskin (°C) | 0.31 ± 1.06 (d = 0.4, r = 0.26) | 3.44 ± 1.22 (d = 3.7, r = 0.22) | 4.58 ± 1.25* (d = 5.6, r = 0.12) | 3.13± 0.84 (d = 3.8, r = 0.53) | 4.27 ± 0.90* (d = 6.2, r = 0.40) | 1.14 ± 0.78* (d = 1.4, r = 0.66) |
| Mean Tre:Tsk (°C) | 0.14 ± 0.99 (d = 0.2, r = 0.81) | 2.80 ± 1.11 (d = 1.7, r = 0.61) | 3.92 ± 1.41* (d = 2.7, r = 0.20) | 2.66 ± 0.84* (d = 3.4, r = 0.68) | 3.77 ± 0.86* (d = 5.8, r = 0.18) | 1.11 ± 0.82 (d = 1.2, r = 0.68) |
| Peak HR (b.min−1) | 4 ± 8 (d = 0.2, r = 0.94) | 12 ± 12† (d = 0.6, r = 0.83) | 20 ± 11*† (d = 1.1, r = 0.84) | 8 ± 17† (d = 0.4, r = 0.71) | 16 ± 14*† (d = 0.8, r = 0.80) | 8 ± 9*† (d = 0.4, r = 0.90) |
| Sweat rate (L.hr−1) | 0.33 ± 0.27*† (d = 1.2, r = 0.46) | 0.58 ± 0.43*† (d = 1.3, r = 0.47) | 0.95 ± 0.51*† (d = 2.3, r = 0.32) | 0.26 ± 0.31† (d = 0.6, r = 0.86) | 0.62 ± 0.37*† (d = 1.7, r = 0.80) | 0.37 ± 0.37*† (d = 0.8, r = 0.76) |
| Peak RPE | 1 ± 1† (d = 0.0, r = 0.84) | 1 ± 1† (d = 0.0, r = 0.57) | 2 ± 1*† (d = 2.0, r = 0.80) | 1 ± 2† (d = 1.0, r = 0.15) | 1 ± 1*† (d = 2.0, r = 0.53) | 1 ± 1† (d = 1.0, r = 0.75) |
| Peak TSS | 0.5 ± 0.5 (d = 1.0, r = 0.61) | 1.1 ± 0.8† (d = 2.2, r = 0.13) | 1.8 ± 0.7*† (d = 3.6, r = 0.04) | 0.6 ± 0.5* (d = 1.2, r = 0.55) | 1.3 ± 0.5*† (d = 2.6, r = 0.54) | 1.3 ± 0.5*† (d = 1.4, r = 0.54) |
| Peak TC | 1 ± 1† (d = 1.0, r = 0.54) | 1 ± 1† (d = 1.0, r = 0.68) | 1 ± 1† (d = 2.0, r = 0.68) | 0 ± 1 (d = 0.0, r = 0.73) | 0 ± 1 (d = 1.0, r = 0.73) | 0 ± 1 (d = 1.0, r = 0.73) |
Note; *significant difference between trials (P<0.05), †difference above the a-priori pre-defined limits.
Physiological measures
Tre demonstrated a difference between conditions (F = 14.5, P<0.001) and over time (F = 146.5, P<0.001). Observation of an interaction effect (F = 13.1, P<0.001) and post-hoc analyses identified that from 20-mins onwards HOTSUIT was greater than TEMP and TEMPSUIT, and from 25-mins onwards HOTSUIT was greater than TEMP, TEMPSUIT and HOT. HOT was also greater than TEMP from 25-mins onwards. No difference was observed between TEMPSUIT and HOT at any time (P>0.05).
Tskin demonstrated a difference between conditions (F = 36.6, P<0.001) and over time (F = 93.4, P<0.001). Observation of an interaction effect (F = 11.6, P<0.001) and post-hoc analyses identified that from 5-mins onwards HOT and HOTSUIT were greater than TEMP and TEMPSUIT. From 15-mins onwards, HOTSUIT was also greater than HOT. Peak Tchest (F = 41.7, P<0.001), Tarm (F = 7.3, P<0.001), Tthigh (F = 15.3, P<0.001) and Tcalf (F = 60.3, P<0.001) differed between conditions. Post-hoc analyses identified a higher (P<0.05) Tchest in; HOTSUIT compared to TEMP, TEMPSUIT and HOT, in HOT compared to TEMP, and, in TEMPSUIT compared to TEMP. Tarm was higher in HOT and HOTSUIT compared to TEMP. No differences (P>0.05) were observed between TEMPSUIT and HOT for Tchest or Tarm. Tthigh and Tcalf were higher (P>0.05) in HOT and HOTSUIT compared to TEMP and TEMPSUIT.
The Tre:Tskin gradient demonstrated a difference between conditions (F = 72.6, P<0.001) and over time (F = 76.0, P<0.001). Observation of an interaction effect (F = 13.9, P<0.001) and post-hoc analyses observed that from 5-mins onwards HOT and HOTSUIT were greater than TEMP and TEMPSUIT. From 25-mins onwards HOTSUIT was also greater than HOT. At 30-mins, HOT and HOTSUIT were no longer different.
HR demonstrated a difference between conditions (F = 19.5, P<0.001) and over time (F = 491.2, P<0.001). Observation of an interaction effect (F = 11.7, P<0.001) and post-hoc analyses identified that from 5-mins onwards HOTSUIT was greater than TEMPSUIT and from 10-mins onwards HOTSUIT was greater than TEMP and TEMPSUIT. From 20-mins onwards HOT was greater than TEMPSUIT and at 30-mins HOTSUIT was greater than HOT.
Sweat rate demonstrated a difference between conditions (F = 10.3, P<0.001). A greater (P<0.05) sweat rate was observed within TEMPSUIT, HOT and HOTSUIT compared to TEMP.
Perceptual measures
RPE demonstrated a difference between conditions (F = 17.9, P<0.001) and over time (F = 93.4, P<0.001). Observation of an interaction effect (F = 11.6, P<0.001) and post-hoc analyses identified that from 5-mins onwards HOTSUIT was greater than TEMP. From 15-mins HOT was also greater than TEMP. No difference was observed between TEMP and TEMPSUIT, or TEMPSUIT and HOT.
TSS demonstrated a difference between conditions (F = 53.9, P<0.001) and over time (F = 105.0, P<0.001). Observation of an interaction effect (F = 11.9, P<0.001) and post-hoc analyses identified that from 5-mins onwards HOT and HOTSUIT were greater than TEMP and TEMPSUIT. TEMPSUIT was greater than TEMP from 10-mins onwards, and from 20-mins HOTSUIT was greater than HOT. At 30-mins, TEMP and TEMPSUIT were not different.
TC demonstrated a difference between conditions (F = 10.4, P<0.001) and over time (F = 43.1, P<0.001). Observation of an interaction effect (F = 7.0, P<0.001) and post-hoc analyses identified that from 20-mins HOTSUIT was greater than TEMP and TEMPSUIT and from 25-mins HOTSUIT was greater than TEMP, TEMPSUIT and HOT.
Mean and individual data for ΔTre, end Tskin, peak HR and sweat rate for each condition are displayed within Figure 3.
Figure 3.
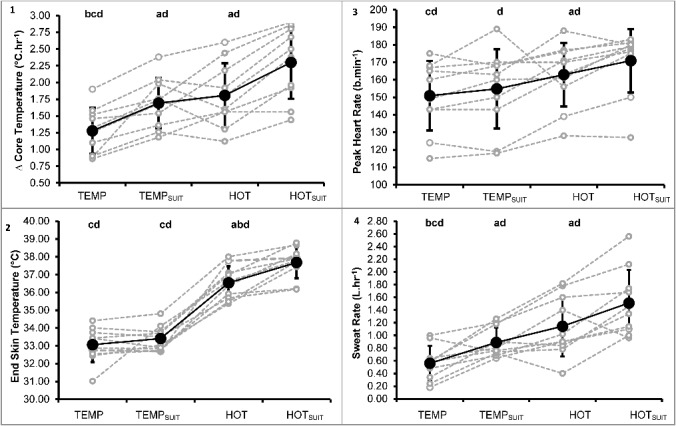
Mean ± SD (black marker and line) and individual responses (grey marker and lines) to TEMP, TEMPSUIT, HOT and HOTSUIT conditions at the end of exercise for ? core temperature (1), end skin temperature (2), peak heart rate (3) and sweat rate (4). Letters indicate statistical difference (P<0.05) whereby; a: vs. TEMP, b: vs. TEMPSUIT, c: vs. HOT, d: vs. HOTSUIT.
Discussion
Overview
A raised and maintained Tre, Tskin and an increased sweat rate have been identified as the primary stimuli for inducing heat adaptation [3,17]. Our data highlights that, when commencing equivalent exercise from a similar fluid balance (Uosm, Usg and NBM) and physiological state (Tre, Tskin and HR), wearing an upper-body vinyl ‘sauna’ suit can increase the magnitude of change in an individual's Tre and resultant sweat rate (Table 1, Figures 1 and 3). The increased Tre is greater than that during temperate exercise and is similar to that observed within hot conditions. Furthermore, the increase in physiological strain is enhanced by combining hot conditions and a vinyl suit, purporting a potential for increased efficiency during HA without the requirement to increase exercise intensity nor volume to achieve the same physiological strain.
Figure 1.
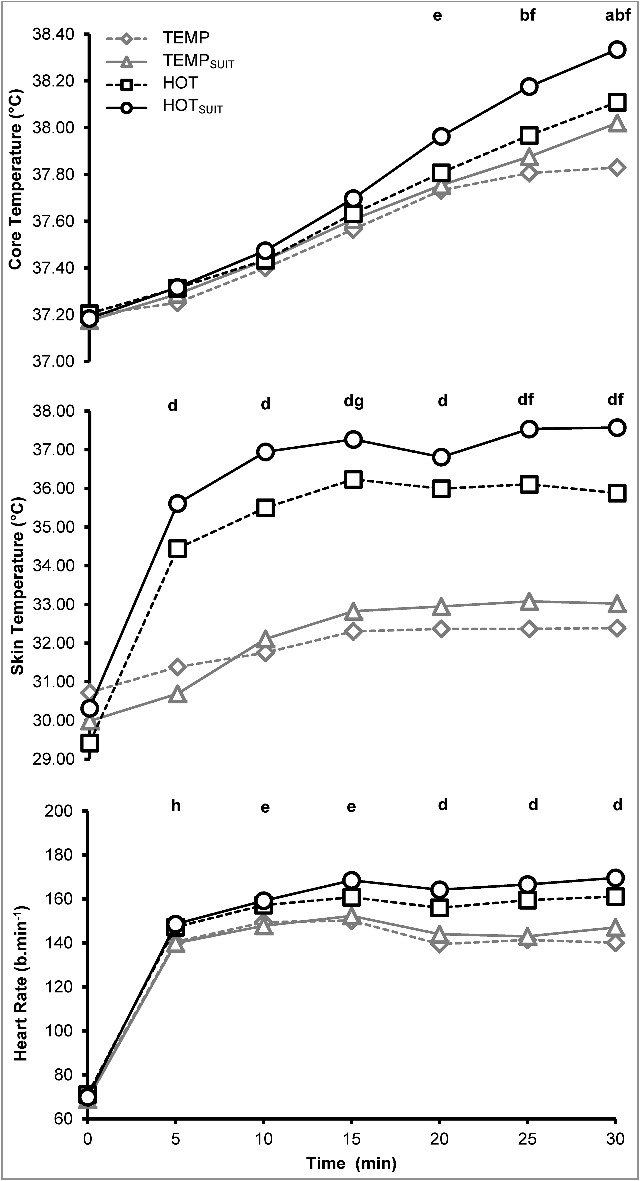
Mean physiological measurements, core temperature (Top), skin temperature (Middle) and heart rate (Bottom) during 30-mins of exercise in TEMP, TEMPSUIT, HOT and HOTSUIT conditions. SD has been removed for clarity. Letters indicate statistical difference (P<0.05) whereby; a: TEMP vs. TEMPSUIT, b: TEMP vs. HOT, c: TEMP vs. HOTSUIT, d: TEMP, TEMPSUIT vs. HOT, HOTSUIT, e: TEMP, TEMPSUIT vs. HOTSUIT, f: TEMP, TEMPSUIT, HOT vs. HOTSUIT, g: TEMPSUIT vs. HOTSUIT, h: HOT vs. HOTSUIT.
A primary aim of this experiment was to determine whether wearing an upper-body vinyl suit in temperate conditions would elicit equivalent physiological responses to potentiate heat adaptation as training in a hot environment. Whilst there were no differences (P>0.05) between TEMPSUIT and HOT for peak Tre, HR or sweat rate (Table 2), it is clear the HOT trial provided a larger physiological strain than temperate exercise without restricted heat loss (TEMP) (Figure 1 and 3). Further, no perceptual differences (P>0.05) were observed between TEMPSUIT and HOT for RPE or TC, with the only differences being Tskin, Tre:Tskin gradient and TSS (P<0.05 [Table 1 and 2]). The elevated Tskin between TEMPSUIT and HOT (∼3°C) likely reflected the higher ambient air temperature in the chamber, compared to the air temperature in the microclimate under the suit [35], which only covered the upper-body (∼60% of the BSA). Whilst much of the body was insulated by the upper-body sauna suit, the legs still represent ∼40% of the BSA [42,49] with an approximate 1.0 mg.cm−2.min−1 cutaneous water loss potential [38], which may have limited the benefit of TEMPSUIT. The elevation in TSS between TEMPSUIT and HOT (∼0.5 A.U.) is likely a result of the difference in Tskin [50].
In a similar experiment, eight trained athletes ran at 50% of their V̇O2max in hot conditions (40°C, 30% RH) in normal clothing for training, and in cool conditions (15°C, 50% RH) whilst wearing excess clothing [29]. Both approaches increased physiological strain index ([PSI] +5.8 and +4.5, respectively), though mean PSI was higher in hot conditions compared with overdressing in cool conditions (6.0 ± 1.0 vs. 5.2 ± 1.1, respectively). Unfortunately, based upon available data it is not possible to determine whether Tre or HR were lower or whether one measurement had a greater influence on the calculation of PSI. Nonetheless, these exploratory data are supportive of our HOT vs. TEMPSUIT comparison, with the authors suggesting that by adequately overdressing, athletes may be able to mimic heat stress and potentially obtain the benefits of heat adaptation in a cooler environment [29]. In line with the present experiment, recent data have reported the effects of wearing additional clothing (shorts, top, winter cycle jacket and gloves) vs. regular clothing (shorts and top only), with a greater increase in physiological strain when completing an 80-mins standardised cycling training session outdoors in temperate conditions (∼17°C, ∼82% RH) [30]. In spite of differences in training session duration which likely explain the magnitude of difference (ΔTre) in comparison to our data, Stevens et al. [30] noted a similar pattern of physiological differences to that of our comparisons between TEMP and TEMPSUIT with elevated mean Tre (theirs +0.4°C, ours +0.2°C) and sweat rate (both ∼+0.3 L.hr−1) alongside similar magnitudes of HR increase (theirs +3 b.min−1, ours +4 b.min−1), albeit without statistical difference in our data (Table 2). These exploratory data point to a potential benefit of “overdressing” and restricting heat loss, to elicit greater potentiating physiological stimuli, which may promote heat adaptation via attenuating evaporative cooling (Figure 3). Consequently, it is proposed that training in an upper-body sauna suit within temperate conditions (TEMPSUIT) confers a larger physiological strain compared to training without a sauna suit (TEMP). Furthermore, TEMPSUIT elicits similar increases in Tre, HR and sweat rate to that of training without a sauna suit in hot conditions (HOT).
Previous acute HA experiments utilising cycle ergometry in conditions of ∼40°C and 50% RH have identified that workloads of a comparable nature to this experiment (e.g. ∼1.4-2.0 W.kg−1) elicit rates of heat storage, that increase Tre by 1.0-1.9°C.hr−1 in a range of participants including trained athletes and recreationally active individuals, and both males [7,8,11,51] and females [34,52]. These data, which are similar to the current experiment (Table 1 and 2, Figures 1 and 3) give confidence that “overdressing” by utilising upper-body vinyl suits, or perhaps additional layers of regular clothing can elicit comparable physiological responses to experiments where heat adaptation has occurred. Additionally, the participants only wore an upper-body sauna suit; both alterations may have lessened the effectiveness of the TEMPSUIT in comparison to the HOT trial. Whilst the influence of restricted heat loss clothing during exercise in occupational contexts have been described [53,54], the use of sauna suits during training for performance has been less robustly investigated. Emerging data has reported the benefit of wearing a sauna suit during a 6-week training programme in temperate conditions (30-min sessions, 5 days per week) [31]. Physiological adaptations included; reductions in resting HR (−4 b.min−1), systolic (−2 mmHg) and diastolic blood pressure (−3 mmHg), and, an improved anaerobic threshold (+5.6% of V̇O2max) and V̇O2max (+4.3 mL.kg−1.min−1) [31]. These enhancements appear congruous with the magnitudes of adaptation associated with HA [26], albeit they were achieved over a considerably longer period than most HA protocols and did not include a comparable control group. Nonetheless, it might be proposed that the same dose of HA over more frequent (daily or twice-daily), longer exposures (∼90-mins) condensed into a shorter training period (7-14 days) and increasing the surface area of restricted heat loss (i.e. full-body sauna suit) would be effective at inducing the HA phenotype and thus requires further investigation. Likewise, the potential to shorten or complete training sessions across different locations will allow team/groups or individuals to implement heat alleviating strategies (e.g. HA), when previously restricted to attend warm-weather training camps or use heat chambers, due to logistical or monetary limitations.
A further aim of this study was to identify whether wearing an upper-body vinyl suit would enhance key potentiating stimuli in hot-dry conditions replicating a traditional HA session. As evidenced by the significantly greater physiological (Figure 1 and 3) and perceptual (Figure 2) responses to HOTSUIT (Table 2), and proposed by others, wearing additional clothing appears to be a potential viable strategy which may be utilised throughout training to enhance heat tolerance [28], in addition to the previously identified benefit as a priming stimuli for sweat adaptations [35]. Therefore, restricting heat loss during HA may present a more efficient method for attaining sufficient physiological stimuli, without increasing absolute exercise intensity. Further, although speculative, wearing sauna suits may offer supplementary perceptual, sudomotor and circulatory (e.g. skin blood flow) adaptations, imposed by the benefits of hot-wet conditions [18,55], which are recommended at the latter stages of HA [2,56]. This may support individuals exercising in either hot-wet or hot-dry conditions [57,58], however, despite the benefits of superior sweat loss capacity, an earlier onset of dehydration and cardiovascular strain may occur [59], especially if evaporative requirement is inhibited [60], thus hydration guidelines must be followed [61]. It is also acknowledged that a possible time-lag using rectal thermometry may have reduced the differences between the ΔTre across conditions, as opposed to using a more responsive index of core temperature (e.g. oesophageal [62]).
Figure 2.
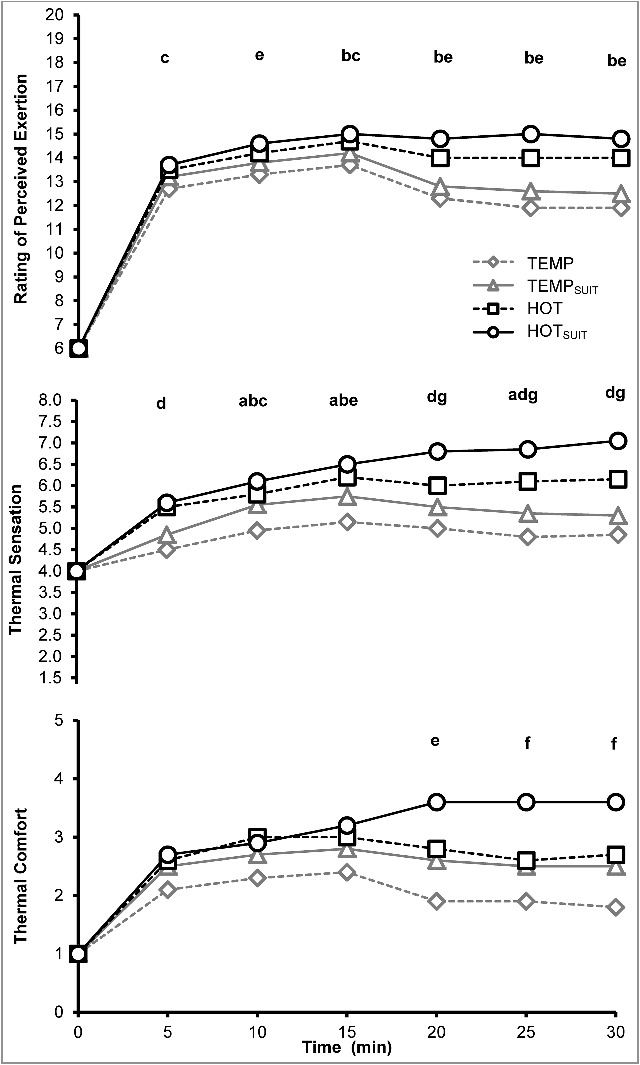
Mean perceptual measurements, rating of perceived exertion (Top), thermal sensation (Middle) and thermal comfort (Bottom) during 30-mins of exercise in TEMP, TEMPSUIT, HOT and HOTSUIT conditions. SD has been removed for clarity. Letters indicate statistical difference (P<0.05) whereby; a: TEMP vs. TEMPSUIT, b: TEMP vs. HOT, c: TEMP vs. HOTSUIT, d: TEMP, TEMPSUIT vs. HOT, HOTSUIT, e: TEMP, TEMPSUIT vs. HOTSUIT, f: TEMP, TEMPSUIT, HOT vs. HOTSUIT, g: HOT vs. HOTSUIT.
Practical application and future direction
Our data indicate that clothing which restricts sweat evaporation may be worn during exercise to enhance heat adaptation stimuli, however further work is required to elucidate the full potential of this method in both acute and chronic interventions using intensities and durations of exercise consistent with existing heat acclimation protocols. This may demonstrate its efficacy across exercise modalities (e.g. running/walking, rowing and cycling), both indoors and outdoors for athletic or occupational populations (e.g. firefighters and military), and for those individuals for whom heat tolerance is compromised (e.g. elderly or clinical populations), but access to heat training facilities is limited. Additional research is required to determine whether repeated restriction of evaporation via excessive/specific clothing can induce the HA phenotype to the same extent as a traditional chamber based protocol. Given the problems with accessing chamber facilities for large cohorts (e.g. team-sports, occupational or military personnel), the opportunity to overdress and train in temperate conditions to induce heat adaptation prior to competing in a warmer climate is appealing, although, we highlight the need for monitoring body temperature and hydration status, whilst also calculating fluid loss and individualising rehydration strategies for individuals adopting this technique.
Refinements to the exercise protocol (i.e. increased exercise intensity) and increasing the area of restricted heat loss (i.e. full-body sauna suit) may provide equivalent responses to exercising in hot conditions. Restricting whole-body water loss using a full-body sauna suit, the subsequent evaporation from limbs undergoing mechanical work and elevated self-generated air flow [63] may facilitate faster increases in Tre, helping to expedite HA. A further practical advancement would be to determine whether wearing restrictive clothing expedites HA when exercising at higher intensities, and therefore greater heat production, than those implemented in the present study is undertaken. Finally, sauna suits may assist in storing the heat generated from exercise, helping to maintain a higher body temperature. If these garments can expedite the time to achieving an elevated body temperature, this may reduce the amount of physical work that must be completed in each training session to achieve recommended guidelines for the maintenance of an elevated Tre (i.e. >38.5°C [7,32]). Previously, another ‘passive’ technique of HWI post-exercise, has been shown to be effective method of raising and maintaining Tre, to elicit heat adaptation [24]. Therefore, for those undertaking HA, overdressing will help to quickly raise body temperature and we highlight the potential to follow physical exertion with HWI to minimise the exercise requirement of HA, although further research is required to support this.
Conclusion
Exercising within temperate conditions whilst wearing an upper-body sauna suit induces a greater physiological strain (i.e. core temperature) and evokes a larger sweat loss in comparison to exercising without a sauna suit in the same conditions. In hot conditions, wearing a sauna suit further enhances physiological and perceptual strain. Wearing a full-body sauna suit during repeated training in temperate conditions may be a viable alternative to HA undertaken in environmental chambers, when a greater exercise intensity is used, with further research warranted. The use of a sauna suit during exercise in a hot environment may accelerate the attainment of important potentiating stimuli for heat adaptation and reduce the physical work, making HA more efficient.
Disclosure of Potential Conflicts of interest
The authors confirm there are no conflicts of interest.
Acknowledgement
The authors would like to thank the participants for their time and commitment to this study.
References
- [1].Casadio JR, Kilding AE, Cotter JD, et al.. From lab to real world: heat acclimation considerations for elite athletes. Sports Med. 2017;47(8):1467–1476. doi: 10.1007/s40279-016-0668-9. [DOI] [PubMed] [Google Scholar]
- [2].Racinais S, Alonso JM, Coutts AJ, et al.. Consensus recommendations on training and competing in the heat. Scand J Med Sci Sports. 2015;25:6–19. doi: 10.1111/sms.12467 doi: 10.1111/sms.12467. [DOI] [PubMed] [Google Scholar]
- [3].Sawka MN, Leon LR, Montain SJ, et al.. Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol. 2011;1:1883–1928. doi: 10.1002/cphy.c100082. [DOI] [PubMed] [Google Scholar]
- [4].Yamazaki F. Effectiveness of exercise-heat acclimation for preventing heat illness in the workplace. J UOEH. 2013;35:183–192. doi: 10.7888/juoeh.35.183. [DOI] [PubMed] [Google Scholar]
- [5].Patterson MJ, Stocks JM, Taylor NAS. Humid heat acclimation does not elicit a preferential sweat redistribution toward the limbs. Am J Physiol Regul Integr Comp Physiol. 2004;286:R512–R518. doi: 10.1152/ajpregu.00359.2003 doi: 10.1152/ajpregu.00359.2003. [DOI] [PubMed] [Google Scholar]
- [6].Buono MJ, Heaney JH, Canine KM. Acclimation to humid heat lowers resting core temperature. Am J Physiol. 1998;274:R1295–R1299. [DOI] [PubMed] [Google Scholar]
- [7].Gibson OR, Mee JA, Tuttle JA, et al.. Isothermic and fixed intensity heat acclimation methods induce similar heat adaptation following short and long-term timescales. J Therm Biol. 2015;49–50:55–65. doi: 10.1016/j.jtherbio.2015.02.005. [DOI] [PubMed] [Google Scholar]
- [8].James CA, Richardson AJ, Watt PW, et al.. Short-term heat acclimation improves the determinants of endurance performance and 5-km running performance in the heat. Appl Physiol Nutr Metab. 2016;42(3):285–294. doi: 10.1139/apnm-2016-0349. [DOI] [PubMed] [Google Scholar]
- [9].Lorenzo S, Halliwill JR, Sawka MN, et al.. Heat acclimation improves exercise performance. J Appl Physiol. 2010;109:1140–1147. doi: 10.1152/japplphysiol.00495.2010 doi: 10.1152/japplphysiol.00495.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sunderland C, Morris JG, Nevill ME. A heat acclimation protocol for team sports. Br J Sports Med. 2008;42:327–333. doi: 10.1136/bjsm.2007.034207. [DOI] [PubMed] [Google Scholar]
- [11].Willmott AG, Hayes M, Waldock KA, et al.. Short-term heat acclimation prior to a multi-day desert ultra-marathon improves physiological and psychological responses without compromising immune status. J Sports Sci. 2017;35(22):2249–2256. doi: 10.1080/02640414.2016.1265142. [DOI] [PubMed] [Google Scholar]
- [12].Amorim FT, Fonseca IT, Machado-Moreira CA, et al.. Insights into the role of heat shock proteins 72 to whole-body heat acclimation in humans. Temperature. 2015;2:499–505. doi: 10.1080/23328940.2015.1110655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yamazaki F. Importance of Heat Acclimation in the Prevention of heat illness during sports activity and work. Adv Exerc Sport Physiol. 2012;18:53–59. [Google Scholar]
- [14].Periard JD, Travers G, Racinais S, et al.. Cardiovascular adaptations supporting human exercise-heat acclimation. Auton Neurosci. 2016;196:52–62. doi: 10.1016/j.autneu.2016.02.002. [DOI] [PubMed] [Google Scholar]
- [15].Racinais S, Wilson MG, Gaoua N, et al.. Heat acclimation has a protective effect on the central but not peripheral nervous system. J Appl Physiol. 2017;123(4):816–824. doi: 10.1152/japplphysiol.00430.2017. [DOI] [PubMed] [Google Scholar]
- [16].Horowitz M. Heat acclimation, epigenetics, and cytoprotection memory. Compr Physiol. 2014;4:199–230. doi: 10.1002/cphy.c130025. [DOI] [PubMed] [Google Scholar]
- [17].Fox RH, Goldsmith R, Kidd DJ, et al.. Acclimatization to heat in man by controlled elevation of body temperature. J Physiol. 1963;166:530–347. doi: 10.1113/jphysiol.1963.sp007121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Regan JM, Macfarlane DJ, Taylor NA. An evaluation of the role of skin temperature during heat adaptation. Acta Physiol Scand. 1996;158:365–375. doi: 10.1046/j.1365-201X.1996.561311000.x. [DOI] [PubMed] [Google Scholar]
- [19].Buono MJ, Numan TR, Claros RM, et al.. Is active sweating during heat acclimation required for improvements in peripheral sweat gland function? Am J Physiol Regul Integr Comp Physiol. 2009;297:R1082–R1085. doi: 10.1152/ajpregu.00253.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Armstrong CG, Kenney WL. Effects of age and acclimation on responses to passive heat exposure. J Appl Physiol. 1993;75:2162–2167. doi: 10.1152/jappl.1993.75.5.2162. [DOI] [PubMed] [Google Scholar]
- [21].Pallubinsky H, Schellen L, Kingma BRM, et al.. Thermophysiological adaptations to passive mild heat acclimation. Temperature. 2017;4(2):176–186. doi: 10.1080/23328940.2017.1303562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Racinais S, Wilson MG, Périard JD. Passive heat acclimation improves skeletal muscle contractility in humans. Am J Physiol - Regul Integr Comp Physiol. 2017;312(1):R101–R107. [DOI] [PubMed] [Google Scholar]
- [23].Ruddock AD, Thompson SW, Hudson SA, et al.. Combined active and passive heat exposure induced heat acclimation in a soccer referee before 2014 FIFA World Cup. SpringerPlus. 2016;5(1):617. doi: 10.1186/s40064-016-2298-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Zurawlew MJ, Walsh NP, Fortes MB, et al.. Post‐exercise hot water immersion induces heat acclimation and improves endurance exercise performance in the heat. Scand J Med Sci Sports. 2015;26:745–754. doi: 10.1111/sms.12638. [DOI] [PubMed] [Google Scholar]
- [25].Scoon GSM, Hopkins WG, Mayhew S, et al.. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J Sci Med Sport. 2007;10:259–262. doi: 10.1016/j.jsams.2006.06.009. [DOI] [PubMed] [Google Scholar]
- [26].Tyler CJ, Reeve T, Hodges GJ, et al.. The effects of heat adaptation on physiology, perception and exercise performance in the heat: a meta-analysis. Sports Med. 2016;46(11):1699–1724. doi: 10.1007/s40279-016-0538-5. [DOI] [PubMed] [Google Scholar]
- [27].Periard JD, Racinais S, Timpka T, et al.. Strategies and factors associated with preparing for competing in the heat: a cohort study at the 2015 IAAF World Athletics Championships. Br J Sports Med. 2017;51:264–270. doi: 10.1136/bjsports-2016-096579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Dawson B. Exercise training in sweat clothing in cool conditions to improve heat tolerance. Sports Med. 1994;17:233–244. doi: 10.2165/00007256-199417040-00004. [DOI] [PubMed] [Google Scholar]
- [29].Steele J, Ely B, Minson C. Over-dressing during exercise in temperate environmental conditions mimics physiological strain of exercise in the heat. Int J Exerc Sci Conf Proc. 2015;8:18. [Google Scholar]
- [30].Stevens CJ, Plews DJ, Laursen PB, et al.. Acute physiological and perceptual responses to wearing additional clothing while cycling outdoors in a temperate environment: a practical method to increase the heat load. Temperature. 2017;4(4):414–419. doi: 10.1080/23328940.2017.1365108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Van der Velde SS, Pierre IA, Byrd BR, et al.. Effects of exercise training with a sauna suit on cardiovascular health: a proof-of-concept study. Int J Res Exerc Physiol. 2016;11:1–10. [Google Scholar]
- [32].Taylor NAS. Human Heat Adaptation. Compr Physiol. 2014;4:325–365. doi: 10.1002/cphy.c130022. [DOI] [PubMed] [Google Scholar]
- [33].Sawka MN, Burke LM, Eichner ER, et al.. American College of Sports Medicine position stand. Exercise and fluid replacement. Med Sci Sports Exerc. 2007;39:377–90. [DOI] [PubMed] [Google Scholar]
- [34].Mee JA, Gibson OR, Doust JJH, et al.. A comparison of males and females’ temporal patterning to short- and long-term heat acclimation. Scand J Med Sci Sports. 2015;25:250–258. doi: 10.1111/sms.12417. [DOI] [PubMed] [Google Scholar]
- [35].Mee JA, Peters S, Doust JH, et al.. Sauna exposure immediately prior to short-term heat acclimation accelerates phenotypic adaptation in females. J Sci Med Sport. 2018;21(2):190–195. doi: 10.1016/j.jsams.2017.06.024. [DOI] [PubMed] [Google Scholar]
- [36].World Medical Association World Medical Association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. PMID:24141714; doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- [37].Gibson OR, Willmott AG, James C, et al.. Power relative to body mass best predicts change in core temperature during exercise-heat stress. J Strength Cond Res. 2017;31(2):403–414. [DOI] [PubMed] [Google Scholar]
- [38].Taylor NA, Machado-Moreira CA, Wijngaart L van den, et al.. Regional variations in transepidermal water loss, eccrine sweat gland density, sweat secretion rates and electrolyte composition in resting and exercising humans. Extrem Physiol Med. 2013;2:4. doi: 10.1186/2046-7648-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Durnin JV, Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974;32:77–97. doi: 10.1079/BJN19740060. [DOI] [PubMed] [Google Scholar]
- [40].Siri WE. The gross composition of the body. Adv Biol Med Phys. 1956;4:239–280. doi: 10.1016/B978-1-4832-3110-5.50011-X. [DOI] [PubMed] [Google Scholar]
- [41].Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med. 1916;17:863–871. doi: 10.1001/archinte.1916.00080130010002. [DOI] [PubMed] [Google Scholar]
- [42].Ramanathan NL. A new weighting system for mean surface temperature of the human body. J Appl Physiol. 1964;19:531–3. doi: 10.1152/jappl.1964.19.3.531. [DOI] [PubMed] [Google Scholar]
- [43].Cuddy JS, Hailes WS, Ruby BC. A reduced core to skin temperature gradient, not a critical core temperature, affects aerobic capacity in the heat. J Therm Biol. 2014;43:7–12. doi: 10.1016/j.jtherbio.2014.04.002. [DOI] [PubMed] [Google Scholar]
- [44].Dion T, Savoie FA, Asselin A, et al.. Half-marathon running performance is not improved by a rate of fluid intake above that dictated by thirst sensation in trained distance runners. Eur J Appl Physiol. 2013;113:3011–20. doi: 10.1007/s00421-013-2730-8. [DOI] [PubMed] [Google Scholar]
- [45].Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14:377–81. doi: 10.1249/00005768-198205000-00012. [DOI] [PubMed] [Google Scholar]
- [46].Zhang H, Huizenga C, Arens E, et al.. Thermal sensation and comfort in transient non-uniform thermal environments. Eur J Appl Physiol. 2004;92:728–33. doi: 10.1007/s00421-004-1137-y. [DOI] [PubMed] [Google Scholar]
- [47].Toner MM, Drolet LL, Pandolf KB. Perceptual and physiological responses during exercise in cool and cold water. Percept Mot Skills. 1986;62:211–20. doi: 10.2466/pms.1986.62.1.211. [DOI] [PubMed] [Google Scholar]
- [48].Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale (NJ): Erlbaum; 1988. [Google Scholar]
- [49].Cross A, Collard M, Nelson A, et al.. Body segment differences in surface area, skin temperature and 3D displacement and the estimation of heat balance during locomotion in hominins. PLoS One. 2008;3:e2464. doi: 10.1371/journal.pone.0002464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Gagge AP, Stolwijk JA, Saltin B. Comfort and thermal sensations and associated physiological responses during exercise at various ambient temperatures. Environ Res. 1969;2:209–229. doi: 10.1016/0013-9351(69)90037-1. [DOI] [PubMed] [Google Scholar]
- [51].Willmott AGB, Gibson OR, Hayes M, et al.. The effects of single versus twice daily short term heat acclimation on heat strain and 3000 m running performance in hot, humid conditions. J Therm Biol. 2016;56:59–67. doi: 10.1016/j.jtherbio.2016.01.001. [DOI] [PubMed] [Google Scholar]
- [52].Mee JA, Gibson OR, Tuttle JA, et al.. Leukocyte Hsp72 mRNA transcription does not differ between males and females during heat acclimation. Temperature. 2016;3:549–556. doi: 10.1080/23328940.2016.1214336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Aoyagi Y, McLellan TM, Shephard RJ. Effects of 6 versus 12 days of heat acclimation on heat tolerance in lightly exercising men wearing protective clothing. Eur J Appl Physiol Occup Physiol. 1995;71:187–96. doi: 10.1007/BF00854978. [DOI] [PubMed] [Google Scholar]
- [54].McLellan TM, Aoyagi Y. Heat strain in protective clothing following hot-wet or hot-dry heat acclimation. Can J Appl Physiol. 1996;21:90–108. doi: 10.1139/h96-009. [DOI] [PubMed] [Google Scholar]
- [55].Shvartz E, Bhattacharya A, Sperinde SJ, et al. Sweating responses during heat acclimation and moderate conditioning. J Appl Physiol. 1979;46(4):675–680. [DOI] [PubMed] [Google Scholar]
- [56].Périard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25(S1):20–38. [DOI] [PubMed] [Google Scholar]
- [57].Eichna LW, Bean WB, Ashe WF, et al. Performance in relation to environmental temperature, reactions of normal young men to hot, humid (simulated jungle) environment. Bulletin Johns Hopkins Hosp. 1945;76(1):25–58. [Google Scholar]
- [58].Fox RH, Goldsmith R, Hampton IF, et al. Heat acclimatization by controlled hyperthermia in hot-dry and hot-wet climates. J Appl Physiol. 1967;22(1):39–46. [DOI] [PubMed] [Google Scholar]
- [59].González‐Alonso J, Calbet JA, Nielsen B. Muscle blood flow is reduced with dehydration during prolonged exercise in humans. J Physiol. 1998;513(3):895–905. doi: 10.1111/j.1469-7793.1998.895ba.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Gagnon D, Jay O, Kenny GP. The evaporative requirement for heat balance determines whole-body sweat rate during exercise under conditions permitting full evaporation. J Physiol. 2013;591(11):2925–2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Maughan RJ, Shirreffs SM. Development of individual hydration strategies for athletes. Int J Sport Nutr Exerc Metab. 2008;18(5):457–472. doi: 10.1123/ijsnem.18.5.457. [DOI] [PubMed] [Google Scholar]
- [62].Mündel T, Carter JM, Wilkinson DM, et al.. A comparison of rectal, oesophageal and gastro‐intestinal tract temperatures during moderate‐intensity cycling in temperate and hot conditions. Clin Physiol Funct Imaging. 2016;36(1):11–16. doi: 10.1111/cpf.12187. [DOI] [PubMed] [Google Scholar]
- [63].Deren TM, Coris EE, Casa DJ, et al.. Maximum heat loss potential is lower in football linemen during an NCAA summer training camp because of lower self-generated air flow. J Strength Cond Res. 2014;28:1656–1663. doi: 10.1519/JSC.0000000000000427. [DOI] [PubMed] [Google Scholar]


