Abstract
Objective
The aim of this study was to document long-term symptoms and functional results following war-related knee disarticulation, trans-femoral amputation, and hip disarticulation.
Methods
An observational cross-sectional study was conducted in a 7-day recreational camp in Iran. One thousand patients with unilateral hip disarticulation, trans-femoral amputation and knee disarticulation due to war-related injuries were invited to undergo a thorough physical examination. Among the invited persons, 58.7% (587 subjects) responded to our invitations. A complete examination related to phantom pain, phantom sensation, stump pain, back pain, and sound limb joints pain with a self-constructed questionnaire was performed. In addition, Amputee Mobility Predictor (AMP) instrument with a prosthesis was completed to assess the function of patients.
Results
The mean duration of time since amputation was 22 years. The most common symptoms reported by participants were phantom sensation (82%), back pain (69%), and phantom pain (63%). In addition, total scores of AMP with a prosthesis in persons with knee disarticulation and trans-femoral amputations were 20.8 and 28, respectively.
The knee disarticulation was associated with higher scores of AMP with a prosthesis compared to transfemoral amputation (p < 0.01).
Conclusion
The results of this study showed that patients with lower limb amputation suffer from significant clinical and functional problems. The findings may be useful to adopt new strategies in planning rehabilitation programs to improve quality of life and health status of patients with war-related lower limb amputation.
Level of Evidence
Level IV, Therapeutic study.
Keywords: Traumatic injury, Veterans, Back pain, Artificial limbs, Prosthesis
Introduction
The Iraq–Iran war, lasting from September 1980 to August 1988, left more than 250,000 dead, and 615,000 injured.1 Combat injuries predominantly affect the limbs2 and can frequently result in traumatic amputation or unsalvageable, complex limb injuries. The Iranian Veterans and Martyrs Affairs Foundation (VMAF) holds a database of all Iranian military and civilian casualties from the Iran–Iraq conflict. According to VMAF database, 11,570 Iranian survivors underwent lower limb amputations,3 1469 of which were unilateral knee disarticulations, trans-femoral amputations and hip disarticulations.
Transfemoral amputation is one of the most common levels of amputation during both war and peace.4 This lower extremity amputation alters the ability of a person profoundly.5 Long-term health issues include back pain, joint pain, osteoarthritis, and phantom limb pain.6 Phantom limb symptoms are one of the most commonly reported complaints following amputation.7 The phantom sysmptoms range from pain to sensation. The phantom symptoms are results of damage to the peripherial nervous system. 8 Phantom pain is defined as the pain in the missing portion of the limb, and phantom sensation defined as the persisting presence of the missing limb.8, 9 Different studies have reported a wide range of prevalence for this condition, reported as occurring in 4%–85% of people with amputations.10, 11, 12, 13, 14, 15
To adjust to amputation and long-term consequences such as phantom symptoms and functions, rehabilitation is considered as a fundamental step.
However, incomplete understanding of health issues limits the potential of rehabilitation for persons with amputation.6 This can present challenges for prosthetists, therapists, and physicians that care for patients with knee disarticulation and trans-femoral amputations. There have been few published studies concerning long-term problems faced by people with lower limb amputations following trauma such as war, but the majority of research is focused on transtibial amputations.16, 17 Furthermore, few studies have examined through and above knee amputations, such as tans-femoral amputations, were limited by small sample sizes.18 In this study, we address this gap in the research by characterizing the pain and function in war veterans with knee disarticulation and trans-femoral amputations and examining the factors associated with pain and function in this group.
Methods
This was a cross-sectional study conducted in a seven-day recreational camp in 2007. The VMAF database was searched for individuals who underwent knee disarticulation, trans-femoral amputation or hip disarticulation following injuries sustained during the Iran–Iraq War. According to VMAF data, there were 1469 veterans with unilateral trans-femoral amputation, disarticulation through knee and hip joint, in the database. Patients with recorded perceptual or cognitive impairments were excluded from the study, which limited our sample. As only thirty-three of the patients were female, they were also excluded. This cross-sectional study was approved by and registered with the ethics committee of the affiliated institute (registration code, 86D101).
The remaining one thousand patients were invited to a seven-day recreational camp, for further clinical consideration for inclusion in the study. Of the one thousand amputees that were invited to the camp, 587 (58.7%) responded to our invitation and consented to attend the camp and participate in this study. The structure of the recreational camp and follow-up used for this study has been previously described in detail.19
At the camp, all participants were examined by a prosthetist and invited to complete an extensive questionnaire including demographic data, employment history, and participation in sport and other recreational activities. The questionnaire, which was used and validated in previous studies,12, 19 specifically enquired about amputation-related symptoms such as phantom pain, phantom sensation, stump pain, stump length, back pain, pain in contralateral limb joints, and prosthesis usage.
For evaluating the basic function of participants in this study, additional information related to ambulatory potential of amputees was obtained by the Amputee Mobility Predictor (AMP) instrument.11 The AMP is a clinical, reliable and valid tool for objectively assessing mobility and potential functional ambulation of a person with lower limb amputation. The AMP was used in this study to evaluate the function of patients with a prosthesis (AMPPRO). The total score range from 0 to 42 for AMPPRO. There was potential for a 5 point increase in the total score, if the subject used an assistive device for items 14 to 20.11 For progressive assessment of a subject with amputation, twenty-one items in AMP are organized with a rising intensity of difficulty. The higher score is related to the higher ambulatory potential of lower-limb amputees.
Stump length in trans-femoral amputation was measured as the length of femur bone, rounded to the nearest centimeter, from greater trochanter to the end of remained soft tissue. The stump length was categorized as short, moderate, and long if it was less than 3 inches (7.62 cm), 3–8 inches (7.62–20.32 cm), and more than 8 inches (20.32 cm) length from the greater trochanter, respectively.
Phantom pain was defined as perceived pain from the missing portion of the limb, and phantom sensation was defined as the feelings perceived to be originating from the missing portion of the limb.12 This was defined dichotomously as “yes/no.”
Statistical analyses were performed using SPSS (Release 18 for Windows, 2009, Chicago, SPSS Inc). Data are presented as mean, standard deviation, frequency, and percentage for descriptions. The associations between dichotomous variables were performed by the use of chi-square test. The threshold for significance was 0.05.
Results
All 587 participants had knee disarticulation, transfemoral amputation or hip disarticulation. The level of amputation for all participants is shown in Table 1. The mean age at the time of amputation was 21.5 years (SD 6.14, range = 1–53). The mean age of participants at time of recruitment to the study was 43.5 years (SD 6.48, range = 16–78). The mean period of follow-up from amputation was 22 years post-injury (SD 3.96). The characteristics and reported symptoms related to amputation are reported in Table 1.
Table 1.
Characteristics of participants with knee disarticulation, transfemoral, and hip disarticulation (total n = 587).
| Characteristic | Distribution |
|---|---|
| Age at time of study, mean (SDa) years | 43 (6.48) |
| Time since amputation (SDa) years | 22 (3.96) |
| Do sport activity | 51% |
| Employment status | 27% |
| Level of amputation | |
| Knee disarticulation | 16% |
| Trans-femoral amputation | 78% |
| Hip disarticulation | 5% |
| Bilateral amputation | 1% |
| Prosthesis use at the time of survey | 78% |
| Phantom pain prevalence | 63% |
| Phantom sensation prevalence | 82% |
| Stump pain prevalence | 49% |
| Back pain prevalence | 69% |
| Contralateral joints pain prevalence | 67% |
| Stump lengthb in trans-femoral amputation, mean (SDa) cm | 30 (8.98) |
| Short | 28% |
| Moderate | 44% |
| Long | 27% |
Standard deviation.
Short stump is defined as the stump with less than 7.62 cm, moderate with 7.62–20.32 cm, and long with more than 20.32 cm length from the greater trochanter.
Out of 94 participants with knee disarticulation, 84% were currently using a limb prosthesis at the time of the study. Also, 77% out of 458 participants with transfemoral amputation, and 28% out of 29 participants with hip disarticulation were using their prosthesis at the time of the study. AMP was used for objectively considering the basic function of participants. The total mean score of AMPPRO in participants with unilateral amputations was 32 (SD 9.17). Total mean score of AMPPRO in participants with knee disarticulation, trans-femoral amputation, and hip disarticulation were 34.7, 32.8, and 31.7 (SD 7.66, 7.30, and 8.69), respectively.
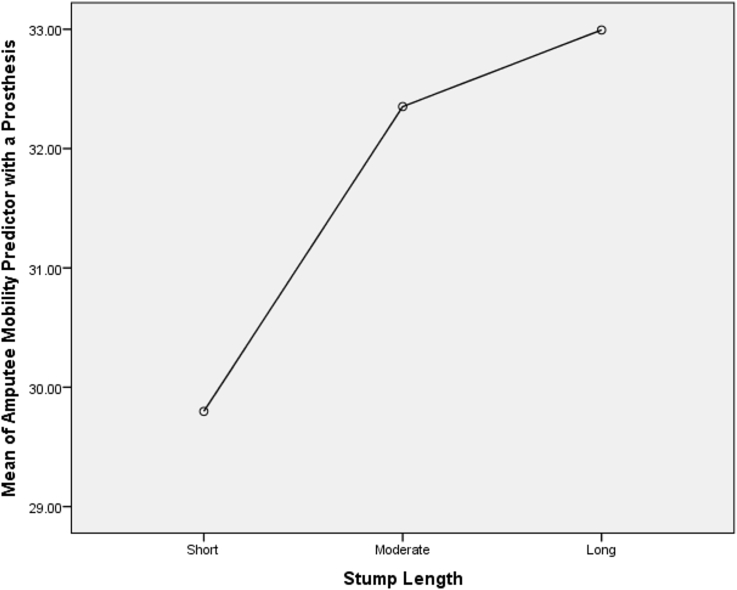
Stump length in trans-femoral amputation was significantly associated with increasing in the potential functional ambulation of participants (p = 0.014, One-way ANOVA). Fig. 1 shows the total mean score of AMPPRO according to the length of stump in trans-femoral amputation. In addition, participants with knee disarticulation had significantly higher scores of AMPPRO than those with trans-femoral amputations (p = 0.016, Independent samples t-test).
Fig. 1.
Total score of amputee mobility predictor with a prosthesis in participants with trans-femoral amputations according to length of the stump (total n = 353) (The stump length was categorized as short, moderate, and long if it had less than 7.62 cm, 7.62–20.32 cm, and more than 20.32 cm length from the greater trochanter, respectively).
Discussion
The results of this study demonstrated the high level of disability and ongoing symptoms experienced by patients for decades following traumatic wartime injury resulting in knee disarticulation, trans-femoral amputation and hip disarticulation. In addition, low levels of potential functional ambulation and high prevalence of phantom pain and sensations were demonstrated in more proximal level of amputation.
The prevalence of long-term consequences after lower limb amputation has received little attention in the medical literature. The most available evidence was limited to the transtibial amputation or upper limb amputation.12, 20, 21, 22, 23, 24, 25, 26 Phantom pain was reported by 63% of participants in our study which is similar to the findings of Yari et al.'s study (73%) in a 23-year follow-up in 46 patients with hip disarticulation or hemi-pelvectomy.21 The reported phantom pain in our study was higher than lower level of amputation such as transtibial amputation.24 It has been previously argued that the severity of phantom pain and phantom sensation gradually decreases over time.27 However, despite the 22-year follow-up in this study, a significant majority of participants still report phantom symptoms. This is a concerning finding as van der Schans et al. in 2002 demonstrated that amputees who experienced phantom pain had a poorer quality of life than those who did not.26
For obvious reasons, casualties of war are often young and healthy adults who participate in military conflict. Similarly, the participants of this study had a mean age at the time of injury of 21, which is in line with the existing literature describing battle-casualties. The high prevalence of contra-lateral limb pain and the younger age at time of injury may relate to a greater level of mobility and therefore reliance on the retained limb in younger and otherwise fitter patients.
The symptomatic pain could be suggestive of early degenerative diseases such as osteoarthritis of the hip and knee joints.28, 29 Stresses on the joints of the contralateral limb may be associated with the resultant disability. Such stresses may be raised from abnormalities of gait, hopping and stumbling behaviors common in young amputees.28 The reported pain in the current study was higher than those previously reported in amputees with lower level of amputations such as transtibial amputation.20 This finding was expected however, previous studies have shown that patients with above knee amputations had threefold risk of contra-lateral knee osteoarthritis than those with below-knee amputations.29
Lower limb amputees are at higher risk for back pain than general population.30, 31 The reported back pain in this study was 69% which was higher than the 23% prevalence of back pain in general population in rural areas.32 This higher prevalence may be due to spinal asymmetry when mobilizing or para-spinal muscle atrophy due to general reduced mobility or a combination.31, 33 However, apart from all these considerations, pain management is needed to reduce dependency and increase performance. As it was shown in vertebral pain, especially lumbosacral pain, bilateral lower limb amputations was associated with higher dependency in activities of daily living.34
According to previous studies, people with amputations have low levels of function.35, 36 Age, balance, physical condition of the non-amputated leg, and muscle power of lower extremity play important role in general functioning of a patient with lower limb amputation.35 Amputation level is described as an important predictor in functional ability of people. The results of this study support these previous findings. One possible reason for this predictive relationship is that it is more difficulty to maintain balance on the unaffected leg because of greater body mass loss. Persons with trans-femoral amputations are at a greater risk of falling because of amputation consequences such as joint and back pain.37 The effect of knee prosthesis mechanisms on balance confidence and function in lower limb amputations proved, for instance, the microprocessor controlled knee mechanisms, improved the balance characteristics, therefore reduced risk of falling.38 However, the details of prosthesis mechanisms were not included as part of the questionnaire in this study.
The authors acknowledge the weaknesses and shortcomings of this study. As only half of the eligible invited patients participated, there may be a selection bias significantly influencing the results. Similarly, the exclusion of patients with cognitive difficulties, although necessary because of the nature of the outcome measures, means that this group of patients has not been evaluated in this study. The selection of the study population was based on VMAF database of predominantly military patients, and the authors; therefore, caution against direct extrapolation or comparison to either wholly military or civilian populations. Therefore, the external validity of the results limited to patients with amputations due to war trauma. Despite these limitations, the authors believe that the large numbers of participants and long follow-up in this study make it an important contribution to the literature describing the consequence of knee disarticulation, transfemoral amputation, and hip disarticulation following trauma.
Conclusion
This study has demonstrated that patients with knee disarticulation, transfemoral amputation, and hip disarticulation following war injury have a significant amount of functional impairment and high-levels of pain for decades following their injury. The results of this descriptive study can be used in future investigations to identify and mitigate risk factors for additional problems in this population, and also to better direct rehabilitation services for addressing the main disabling problems faced by this group of patients.
Conflict of interest
All authors report no conflicts of interest.
Acknowledgement
This study was funded by Veterans and Martyrs Affair Foundation (VMAF), and Janbazan Medical and Engineering Research Center (JMERC).
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Hiro D. Routledge; New York: 1991. The Longest War: The Iran-Iraq Military Conflict. [Google Scholar]
- 2.Penn-Barwell J.G., Roberts S.A.G., Midwinter M.J. Improved survival in UK combat casualties from Iraq and Afghanistan: 2003–2012. J Trauma Acute Care Surg. 2015;78:1014–1020. doi: 10.1097/TA.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 3.Zargar M., Araghizadeh H., Soroush M.R. Iranian casualties during the eight years of Iraq-Iran conflict. Rev Saúde Pública. 2007;41:1065–1066. doi: 10.1590/s0034-89102007000600025. [DOI] [PubMed] [Google Scholar]
- 4.Dougherty P.J. Long-term follow-up of unilateral transfemoral amputees from the Vietnam war. J Trauma Acute Care Surg. 2003;54:718–723. doi: 10.1097/01.TA.0000046260.16866.A9. [DOI] [PubMed] [Google Scholar]
- 5.Hafner B.J., Willingham L.L., Buell N.C. Evaluation of function, performance, and preference as transfemoral amputees transition from mechanical to microprocessor control of the prosthetic knee. Arch Phys Med Rehabil. 2007;88:207–217. doi: 10.1016/j.apmr.2006.10.030. [DOI] [PubMed] [Google Scholar]
- 6.Robbins C.B., Vreeman D.J., Sothmann M.S. A review of the long-term health outcomes associated with war-related amputation. Mil Med. 2009;174:588–592. doi: 10.7205/milmed-d-00-0608. [DOI] [PubMed] [Google Scholar]
- 7.Giummarra M.J., Gibson S.J., Georgiou-Karistianis N. Central mechanisms in phantom limb perception: the past, present and future. Brain Res Rev. 2007;54:219–232. doi: 10.1016/j.brainresrev.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 8.Bosmans J.C., Geertzen J.H., Post W.J. Factors associated with phantom limb pain: a 31/2-year prospective study. Clin Rehabil. 2010;24:444–453. doi: 10.1177/0269215509360645. [DOI] [PubMed] [Google Scholar]
- 9.Subedi B., Grossberg G.T. Phantom limb pain: mechanisms and treatment approaches. Pain Res Treat. 2011;2011:1–8. doi: 10.1155/2011/864605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aldington D., Small C., Edwards D. A survey of post-amputation pains in serving military personnel. J R Army Med Corps. 2014;160:38–41. doi: 10.1136/jramc-2013-000069. [DOI] [PubMed] [Google Scholar]
- 11.Gailey R.S., Roach K.E., Applegate E.B. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee's ability to ambulate. Arch Phys Med Rehabil. 2002;83:613–627. doi: 10.1053/apmr.2002.32309. [DOI] [PubMed] [Google Scholar]
- 12.Modirian E., Shojaei H., Soroush M.R. Phantom pain in bilateral upper limb amputation. Disabil Rehabil. 2009;31:1878–1881. doi: 10.1080/09638280902810976. [DOI] [PubMed] [Google Scholar]
- 13.Pohjolainen T. A clinical evaluation of stumps in lower limb amputees. Prosthet Orthot Int. 1991;15:178–184. doi: 10.3109/03093649109164285. [DOI] [PubMed] [Google Scholar]
- 14.Rasulić L., Ivanović S., Bascarević V. Phantom pain and posttraumatic pain conditions. Acta Chir Iugosl. 2003;51:71–80. doi: 10.2298/aci0404069r. [DOI] [PubMed] [Google Scholar]
- 15.Shaikh J., Mohamm A., Varudkar A. Complications and outcome of amputations at tertiary care hospital in Aurangabad district of Maharashtra: an observational study. Trauma. 2015;78:80–82. [Google Scholar]
- 16.Dougherty P.J. Transtibial amputees from the Vietnam war. Twenty-eight-year follow-up. J Bone Jt Surg Am. 2001;83:383–389. doi: 10.2106/00004623-200103000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Ebrahimzadeh M.H., Hariri S. Long-term outcomes of unilateral transtibial amputations. Mil Med. 2009;174:593–597. doi: 10.7205/milmed-d-02-8907. [DOI] [PubMed] [Google Scholar]
- 18.Ebrahimzadeh M.H., Fattahi A.S. Long-term clinical outcomes of Iranian veterans with unilateral transfemoral amputation. Disabil Rehabil. 2009;31:1873–1877. doi: 10.1080/09638280902810968. [DOI] [PubMed] [Google Scholar]
- 19.Masoumi M., Esfandiari E., Mousavi B. Quality of life in war-related hip disarticulation in Iran. Acta Orthop Traumatol Turc. 2014;48:527–532. doi: 10.3944/AOTT.2014.13.0036. [DOI] [PubMed] [Google Scholar]
- 20.Ebrahimzadeh M.H., Rajabi M.T. Long-term outcomes of patients undergoing war-related amputations of the foot and ankle. J Foot Ankle Surg. 2007;46:429–433. doi: 10.1053/j.jfas.2007.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Yari P., Dijkstra P.U., Geertzen J.H. Functional outcome of hip disarticulation and hemipelvectomy: a cross-sectional national descriptive study in The Netherlands. Clin Rehabil. 2008;22:1127–1133. doi: 10.1177/0269215508095088. [DOI] [PubMed] [Google Scholar]
- 22.Edwards W.T., Jensen M.P., Robinson L.R. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81:1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 23.Kooijman C.M., Dijkstra P.U., Geertzen J.H. Phantom pain and phantom sensations in upper limb amputees: an epidemiological study. Pain. 2000;87:33–41. doi: 10.1016/S0304-3959(00)00264-5. [DOI] [PubMed] [Google Scholar]
- 24.Penn-Barwell J.G. Outcomes in lower limb amputation following trauma: a systematic review and meta-analysis. Injury. 2011;42:1474–1479. doi: 10.1016/j.injury.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Rayegani S.M., Aryanmehr A., Soroosh M.R. Phantom pain, phantom sensation, and spine pain in bilateral lower limb amputees: results of a national survey of Iraq-Iran war victims' health status. JPO J Prosthet Orthot. 2010;22:162–165. 110.1097/JPO.1090b1013e3181eb1093c1098c. [Google Scholar]
- 26.van der Schans C.P., Geertzen J.H., Schoppen T. Phantom pain and health-related quality of life in lower limb amputees. J Pain Symptom Manag. 2002;24:429–436. doi: 10.1016/s0885-3924(02)00511-0. [DOI] [PubMed] [Google Scholar]
- 27.Petri R.P., Jr., Aguila E. The military upper extremity amputee. Phys Med Rehabil Clin N Am. 2002;13:17–43. doi: 10.1016/s1047-9651(03)00070-6. [DOI] [PubMed] [Google Scholar]
- 28.Norvell D.C., Czerniecki J.M., Reiber G.E. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil. 2005;86:487–493. doi: 10.1016/j.apmr.2004.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kulkarni J., Adams J., Thomas E. Association between amputation, arthritis and osteopenia in British male war veterans with major lower limb amputations. Clin Rehabil. 1998;12:348–353. doi: 10.1191/026921598672393611. [DOI] [PubMed] [Google Scholar]
- 30.Ehde D.M., Smith D.G., Czerniecki J.M. Back pain as a secondary disability in persons with lower limb amputations. Arch Phys Med Rehabil. 2001;82:731–734. doi: 10.1053/apmr.2001.21962. [DOI] [PubMed] [Google Scholar]
- 31.Kulkarni J., Gaine W., Buckley J. Chronic low back pain in traumatic lower limb amputees. Clin Rehabil. 2005;19:81–86. doi: 10.1191/0269215505cr819oa. [DOI] [PubMed] [Google Scholar]
- 32.Davatchi F., Tehrani Banihashemi A., Gholami J. The prevalence of musculoskeletal complaints in a rural area in Iran: a WHO-ILAR COPCORD study (stage 1, rural study) in Iran. Clin Rheumatol. 2009;28:1267–1274. doi: 10.1007/s10067-009-1234-8. [DOI] [PubMed] [Google Scholar]
- 33.Smith D.G., Ehde D.M., Legro M.W. Phantom limb, residual limb, and back pain after lower extremity amputations. Clin Orthop Relat Res. 1999;361:29–38. doi: 10.1097/00003086-199904000-00005. [DOI] [PubMed] [Google Scholar]
- 34.Ashraf A., Shojaee H., Mousavi B. Impact of pain in vertebral column on activities of daily living in the Iranian amputees with bilateral lower limb amputation. Disabil Rehabil. 2012;34:869–872. doi: 10.3109/09638288.2011.623756. [DOI] [PubMed] [Google Scholar]
- 35.Schoppen T., Boonstra A., Groothoff J.W. Physical, mental, and social predictors of functional outcome in unilateral lower-limb amputees. Arch Phys Med Rehabil. 2003;84:803–811. doi: 10.1016/s0003-9993(02)04952-3. [DOI] [PubMed] [Google Scholar]
- 36.Greive A., Lankhorst G. Functional outcome of lower-limb amputees: a prospective descriptive study in a general hospital. Prosthet Orthot Int. 1996;20:79–87. doi: 10.3109/03093649609164423. [DOI] [PubMed] [Google Scholar]
- 37.Miller W.C., Speechley M., Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputees. Arch Phys Med Rehabil. 2001;82:1031–1037. doi: 10.1053/apmr.2001.24295. [DOI] [PubMed] [Google Scholar]
- 38.Kaufman K.R., Levine J.A., Brey R.H. Energy expenditure and activity of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Arch Phys Med Rehabil. 2008;89:1380–1385. doi: 10.1016/j.apmr.2007.11.053. [DOI] [PMC free article] [PubMed] [Google Scholar]