Abstract
Introduction:
Nipple-sparing mastectomy (NSM) is increasingly used for breast cancer risk reduction and treatment. Prior small studies with variable control for baseline characteristics suggest superior satisfaction with NSM. The aim of this study was to compare patient satisfaction following NSM and total mastectomy (TM) utilizing the BREAST-Q patient-reported outcome measure in a well-characterized patient population.
Methods:
Patients at a single institution undergoing NSM or TM with immediate tissue expander/implant reconstruction who completed a follow-up BREAST-Q from 2007–2017 were identified by retrospective review of a prospective database. Baseline characteristics were compared, and linear mixed models were used to analyze associations with BREAST-Q scores over time.
Results:
Of 1866 eligible patients, 219 (12%) underwent NSM, and 1647 (88%) underwent TM. Median time from baseline to BREAST-Q was 658 days. Patients having NSM were younger, more likely to be white, and had lower BMI. They more often had prophylactic surgery, bilateral mastectomies, lower-stage disease, and less often received chemotherapy/radiation than patients having TM. On multivariable analysis, after controlling for relevant clinical variables, there was no difference in satisfaction with breasts or satisfaction with outcome overall between NSM and TM patients. Psychosocial well-being and sexual well-being were significantly higher in the NSM group. After additionally controlling for pre-operative BREAST-Q score in a subset of patients (72 NSM; 443 TM), only psychosocial well-being remained significantly higher in NSM patients.
Conclusion:
Patient-reported outcomes should be discussed with women weighing the risks and benefits of NSM to provide a better understanding of expected quality of life.
Keywords: nipple-sparing mastectomy, total mastectomy, breast cancer, risk reduction, patient-reported outcomes, BREAST-Q
INTRODUCTION
Nipple-sparing mastectomy (NSM) is increasingly performed for breast cancer treatment and prophylaxis.1 Initially described as a subcutaneous mastectomy in the 1960s,2–4 this technique has been refined over time and now accounts for a growing proportion of mastectomies. Reported advantages of NSM compared to total mastectomy (TM) include improved cosmesis, body image, and nipple sensation.5 Potential disadvantages include retained breast tissue behind the nipple-areolar complex (NAC), or elsewhere on the skin flaps or chest wall due to lack of surgical exposure, and an increased risk of mastectomy skin flap necrosis.6 National Comprehensive Cancer Network (NCCN) guidelines state that NSM may be considered in carefully selected patients with early-stage, biologically favorable, peripherally located invasive cancer or ductal carcinoma in situ (DCIS).5
The primary issues to consider when recommending NSM are oncologic safety and cosmetic outcome.7 Short-term oncologic safety is promising, with reported local recurrence rates of 3–6% at 5 years--comparable to local recurrence rates seen with traditional mastectomy.8–11 However, the long-term risk of local recurrence or new primary cancers is uncertain, particularly in high-risk women, such as those with BRCA mutations.
The impetus for performing NSM is improved cosmetic outcome. Dissatisfaction with the appearance of the nipple is a common complaint after TM and reconstruction, and preservation of the NAC results in a more natural appearing breast following reconstruction.12–14 NSM is reported to result in better patient satisfaction than TM; however, studies examining this outcome have been limited by small sample size and variable control for differences in patient and disease characteristics among NSM and TM patients.13,15–18 The aim of this study was to compare patient satisfaction following NSM and TM with expander/implant reconstruction utilizing a validated patient-reported outcome measure in a well-characterized patient population.
METHODS
Following Institutional Review Board (IRB) approval, retrospective review of a prospectively maintained database of women undergoing mastectomy between 2007 and 2017 at a single institution was performed. Women were eligible for study inclusion if they underwent NSM or TM with immediate tissue expander/implant reconstruction and completed at least 1 postoperative BREAST-Q survey.
The BREAST-Q is a validated patient-reported outcome measure of satisfaction and health-related quality of life.19,20 It contains 6 domains, including 3 quality-of-life domains and 3 satisfaction domains. For the purposes of this study, we examined psychosocial well-being, sexual well-being, satisfaction with breasts, and satisfaction with outcome. Women undergoing mastectomy with reconstruction were prospectively asked to complete BREAST-Q surveys preoperatively, and at each subsequent follow-up visit. BREAST-Q scores are transformed onto a scale from 0 to 100, with higher scores representing better outcomes.
The decision to perform NSM or TM was at the discretion of the breast surgical oncologist, plastic surgeon, and patient. Patients with clinical evidence of tumor involving the NAC, and those with extensive intraductal carcinoma in the subareolar space were not eligible for NSM. The surgical technique for NSM has been described previously.13
Major complications were defined as any postoperative event that necessitated hospital admission or re-operation, or mastectomy skin flap necrosis greater than 10 cm. Minor complications were those managed in the office that did not require re-operation. Individual patient data were collected by retrospective review of prospectively maintained institutional databases.
Patients were stratified by mastectomy type (NSM vs. TM) and were analyzed with respect to age, body mass index (BMI), race, marital status, unilateral or bilateral mastectomy, indication for surgery (cancer or prophylactic), breast cancer stage, chemotherapy, radiation, postoperative complications, and preoperative BREAST-Q score.
Medians and interquartile ranges were calculated for continuous variables, and categorical variables were summarized as numbers and percentages. Between-group differences at baseline were tested using the Kruskal-Wallis test for continuous variables and Fisher’s exact test for categorical variables. Individual patient trajectories over time with locally weighted scatterplot smoothing (LOESS) curves overlaid were plotted for the satisfaction with breast, psychosocial well-being, sexual well-being, and satisfaction with outcome subscales of the BREAST-Q.
Linear mixed models were used to analyze associations with BREAST-Q scores over follow-up time, incorporating a random intercept and slope for each patient to account for the correlation between scores from an individual patient over time. Days from surgery to each BREAST-Q survey were calculated and analyzed longitudinally to maximize statistical power. Multivariable analysis adjusted for covariates determined a priori including age, unilateral vs. bilateral mastectomy, chemotherapy, and radiotherapy as well as baseline score if applicable. A p-value < 0.05 was considered statistically significant. All statistical analyses were conducted in R version 3.4.2 (R Core Development Team, Vienna, Austria).
RESULTS
Patient Population
During the study period, 4724 women underwent mastectomy with tissue expander/implant reconstruction. One-thousand, eight hundred and sixty-nine completed at least one post-operative BREAST-Q survey and met initial eligibility criteria. Two patients having unilateral NSM with contralateral TM and 1 patient requiring NAC excision for carcinoma involving the nipple margin were excluded, leaving an analytic sample of 1866: 219 NSM and 1647 TM patients. Patient and disease characteristics are outlined in Table 1. NSM patients were younger, had lower body mass index (BMI) and were more often white. NSM patients more commonly had prophylactic surgery and underwent bilateral mastectomy than TM patients. TM patients had more advanced-stage cancers and were more likely to receive chemotherapy or radiotherapy. Complications, primarily minor infections and limited mastectomy skin flap necrosis, were more common in the NSM group (minor, 15% vs. 10%; major, 4% vs. 3%, p = 0.046).
TABLE 1.
Clinicopathologic and treatment characteristics by mastectomy type
| Nipple-Sparing Mastectomy (n = 219) |
Total Mastectomy (n = 1647) |
p-value | |
|---|---|---|---|
| Age (median, range) | 44 (23–70) | 48 (20–78) | < 0.001 |
| BMI (median, range) | 22 (17–36) | 24 (15–51) | < 0.001 |
| Race (n, %) | < 0.001 | ||
| White | 200 (91%) | 1318 (80%) | |
| Black | 1 (1%) | 117 (7%) | |
| Asian | 10 (5%) | 94 (6%) | |
| Hispanic | 0 (0%) | 29 (2%) | |
| Unknown/other | 8 (4%) | 89 (5%) | |
| Marital status | 0.004 | ||
| Married/partnered | 175 (80%) | 1213 (74%) | |
| Single | 30 (14%) | 287 (17%) | |
| Divorced/separated | 14 (6%) | 116 (7%) | |
| Widowed | 0 (0%) | 31 (2%) | |
| Indication (n, %) | < 0.001 | ||
| Cancer | 168 (77%) | 1553 (94%) | |
| Prophylactic | 51 (23%) | 94 (6%) | |
| Bilateral mastectomy (n, %) | 174 (79%) | 1012 (61%) | < 0.001 |
| Pathologic stage (n, %) | < 0.001 | ||
| 0 | 35 (21%) | 257 (17%) | |
| I | 98 (59%) | 735 (47%) | |
| II/III | 32 (19%) | 563 (36%) | |
| Chemotherapy | 57 (26%) | 791 (48%) | < 0.001 |
| Postmastectomy radiation therapy | 9 (4%) | 353 (21%) | < 0.001 |
| Complications | 0.046 | ||
| None | 179 (82%) | 1444 (88%) | |
| Minor | 32 (15%) | 160 (10%) | |
| Major | 8 (4%) | 43 (3%) |
Outcomes
Median time from surgery to follow-up BREAST-Q was 658 days (interquartile range [IQR] 442–1189). Over time, scores in the satisfaction with breasts domain and satisfaction with outcome decreased, while psychosocial well-being did not change over time and sexual well-being increased over time. Despite these trends, on univariable analysis, NSM patients had consistently higher BREAST-Q scores in all domains (Fig. 1).
Fig. 1.
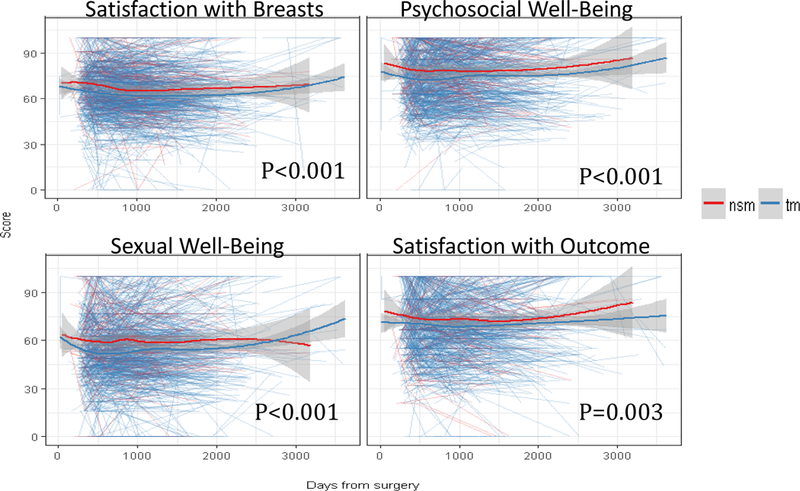
BREAST-Q scores over time
NSM, nipple-sparing mastectomy; TM, total mastectomy
In the multivariable analysis of BREAST-Q satisfaction with breasts, there was no significant difference in scores between patients undergoing NSM and TM (Table 2). Younger age, lower BMI, bilateral mastectomy, and not receiving chemotherapy or radiation were significantly associated with better satisfaction with breast scores. Even after adjustment for other variables, satisfaction with breasts decreased significantly over time.
TABLE 2.
Multivariable analysis: satisfaction with breasts, psychosocial well-being, sexual well-being, and satisfaction with outcome
BMI, body mass index; NSM, nipple-sparing mastectomy; TM, total mastectomy
| Estimate | Standard Error | p-value | |
|---|---|---|---|
| Satisfaction with breasts | |||
| Age | −0.149 | 0.042 | < 0.001 |
| BMI | −0.167 | 0.077 | 0.030 |
| Unilateral vs. bilateral mastectomy | −3.450 | 0.832 | < 0.001 |
| Prophylactic vs. cancer | −0.809 | 1.484 | 0.585 |
| Chemotherapy | −3.045 | 0.869 | < 0.001 |
| Radiation | −5.607 | 1.088 | < 0.001 |
| Days from surgery | −0.002 | 0.000 | < 0.001 |
| NSM vs. TM | 0.994 | 1.248 | 0.426 |
| Psychosocial well-being | |||
| Age | 0.113 | 0.049 | 0.021 |
| BMI | −0.278 | 0.089 | 0.002 |
| Unilateral vs. bilateral mastectomy | 0.317 | 0.968 | 0.743 |
| Prophylactic vs. cancer | 1.905 | 1.723 | 0.269 |
| Chemotherapy | −3.045 | 1.011 | < 0.001 |
| Radiation | −2.382 | 1.266 | 0.060 |
| Days from surgery | 0.001 | 0.000 | 0.049 |
| NSM vs. TM | 3.450 | 1.451 | 0.018 |
| Sexual well-being | |||
| Age | −0.132 | 0.055 | 0.016 |
| BMI | −0.379 | 0.101 | < 0.001 |
| Unilateral vs. bilateral mastectomy | 1.001 | 1.086 | 0.356 |
| Prophylactic vs. cancer | −2.125 | 1.920 | 0.269 |
| Chemotherapy | −4.126 | 1.133 | < 0.001 |
| Radiation | −3.212 | 1.422 | 0.024 |
| Days from surgery | 0.001 | 0.001 | 0.012 |
| NSM vs. TM | 3.997 | 1.619 | 0.014 |
| Satisfaction with outcome | |||
| Age | −0.220 | 0.050 | 0.000 |
| BMI | −0.189 | 0.092 | 0.041 |
| Unilateral vs. bilateral mastectomy | −0.596 | 0.999 | 0.551 |
| Prophylactic vs. cancer | 1.695 | 1.781 | 0.341 |
| Chemotherapy | −0.870 | 1.045 | 0.405 |
| Radiation | −5.437 | 1.311 | < 0.001 |
| Days from surgery | −0.001 | 0.000 | 0.032 |
| NSM vs. TM | 0.928 | 1.499 | 0.536 |
In contrast, NSM was significantly associated with improved psychosocial well-being. Older age, lower BMI, and not receiving chemotherapy were also significantly associated with improved psychosocial well-being. Psychosocial well-being scores improved significantly over time (Table 2).
Similarly, NSM patients had significantly better sexual well-being after adjustment for other variables. Paralleling what was seen for psychosocial well-being, lower BMI and not receiving chemotherapy were associated with higher scores in the sexual well-being domain, and sexual well-being scores increased significantly over time (Table 2). However, younger age was associated with improved sexual well-being compared to the finding of older age being associated with improved psychosocial well-being.
Findings for overall satisfaction with outcome resembled those seen for satisfaction with breasts. There was no significant difference between NSM and TM, and overall satisfaction with outcome decreased significantly over time. Younger age, lower BMI, and not receiving radiation were associated with higher scores (Table 2).
Subset Analysis of Patients with Preoperative BREAST-Q Scores
Seventy-two NSM patients and 443 TM patients completed a preoperative BREAST-Q assessment. Patients with available preoperative scores were slightly younger (47 vs. 48 years of age, p = 0.035), more often underwent bilateral mastectomy (68% vs. 62%, p = 0.028), and less frequently had higher-stage disease (stage II or III, 27% vs. 34%, p = 0.032) than those who had not completed a preoperative BREAST-Q. There was no difference in BMI, race, marital status, surgical indication (cancer vs. benign), mastectomy type (NSM vs. TM), receipt of chemotherapy or radiation, or complications in patients who filled out preoperative BREAST-Q surveys vs. those who did not. There was no significant difference in preoperative BREAST-Q scores between NSM and TM patients, though median scores were higher in NSM patients in all domains (Fig. 2).
Fig. 2.
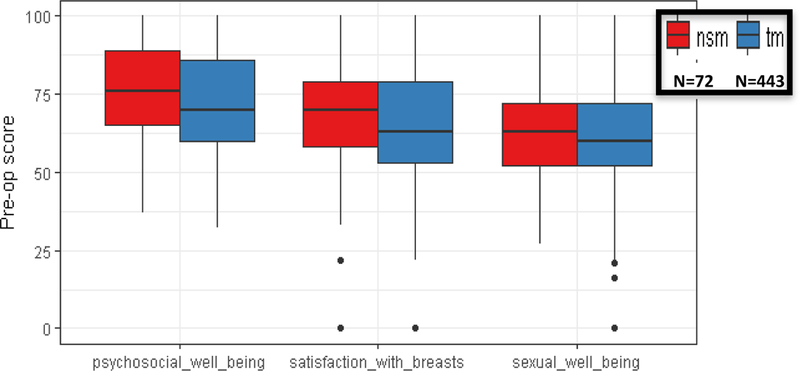
Preoperative BREAST-Q scores, nipple-sparing mastectomy (n = 72) vs. total mastectomy (n = 443)
NSM, nipple-sparing mastectomy; TM, total mastectomy
In multivariable analysis, after controlling for preoperative BREAST-Q score and other clinical features, no significant differences between NSM and TM were observed in satisfaction with breasts or overall satisfaction with outcome. Psychosocial well-being was significantly improved among NSM as compared to TM. Sexual well-being did not differ significantly between NSM and TM patients, though the effect size was in the direction of improved scores for NSM versus TM over time (effect size, −4.49, p = 0.067). These results parallel the findings in the total cohort, not controlling for preoperative BREAST-Q scores (Table 3).
TABLE 3.
Multivariable analysis, controlling for pre-operative BREAST-Q score
| Satisfaction with Breasts |
Psychosocial Well-Being |
Sexual Well-Being |
Satisfaction with Outcome |
|||||
|---|---|---|---|---|---|---|---|---|
| Estimate | p-value | Estimate | p-value | Estimate | p-value | Estimate | p-value | |
| Controlling for pre-op score (n = 515) |
1.877 | 0.374 | 4.869 | 0.035 | 4.488 | 0.067 | 3.353 | 0.184 |
| Total cohort (n = 1866) | 0.994 | 0.426 | 3.450 | 0.018 | 3.997 | 0.014 | 0.928 | 0.536 |
DISCUSSION
Early publications reported improved satisfaction among patients who underwent nipple reconstruction following traditional mastectomy,12,21 and it is now generally accepted that NSM is associated with a better cosmetic outcome than TM and reconstruction, leading to an increased patient demand for the procedure. In a study from the Mayo clinic, the proportion of patients undergoing mastectomy and reconstruction who had NSM increased from 23.7% in 2009 to 39.7% in 2014 (p = 0.004).1
As the indications for NSM expand in the absence of long-term oncologic outcome data, patient-reported outcomes assessing satisfaction with NSM in multiple domains are increasingly important to allow patients to assess the risks and benefits of the procedure. Our study provides a number of pertinent findings in this regard. First, patients undergoing NSM and TM differ significantly in baseline characteristics, such as age and BMI, as well as in cancer stage and treatment received; all features which may impact satisfaction. Failure to control for these differences may result in erroneous conclusions regarding the superiority of NSM. This point is illustrated in our study where utilizing a validated patient-reported outcome measure, we found no difference in satisfaction with breasts or satisfaction with overall outcome in NSM vs. TM patients after adjusting for relevant clinical variables.
Several previous studies have reported improved patient satisfaction following NSM compared with TM; however, control for baseline patient characteristics, disease features, and treatment is variable. Didier et al. utilized a novel questionnaire and compared 310 women who underwent NSM with 143 women who had a TM with subsequent nipple-areolar complex reconstruction. At 1 year, NSM patients reported improved body image, better satisfaction with nipple appearance and sensitivity, and a decreased sense of mutilation. However, while these groups differed at baseline, no adjustment was made for clinical or pathologic variables.22 More recently, Metcalfe et al. utilized multiple questionnaires to evaluate satisfaction in BRCA carriers undergoing prophylactic mastectomy. Their sample consisted of 137 women: 53 nipple-or areola-sparing mastectomy patients, and 84 skin-sparing mastectomy patients. There was no difference in perceived breast cancer risk, decision regret, or cancer-related distress, anxiety, or depression between the groups. After adjusting for time from surgery, weight and income, they found improved satisfaction with breasts, satisfaction with outcome, and sexual well-being in the nipple-/areola-sparing mastectomy group. While this is a more homogeneous group of patients undergoing prophylactic surgery, it is a relatively small sample size with no control for preoperative satisfaction scores.23 Satteson et al. performed a systematic review and meta-analysis comparing NSM to TM with nipple reconstruction. Nine studies including NSM patients were identified, containing satisfaction data from 473 patients, and found higher satisfaction scores in NSM patients. There was no control for other relevant variables in this group.24
Not all reports have found an advantage of NSM. A small study comparing prophylactic mastectomy with immediate implant reconstruction, including 20 women with NSM and 25 women with skin-sparing mastectomy and reconstructed NAC, found no difference in patient satisfaction as measured by BREAST-Q or a body image scale.25
In contrast to the lack of improved satisfaction with breasts or overall outcome, domains which intuitively seem most likely to be improved by NSM, we found that psychosocial well-being was higher, and that there was evidence for improved sexual well-being, though this effect did not reach statistical significance among patients with preoperative BREAST-Q scores. This has previously been suggested to reflect a greater sense of normalcy and self-confidence maintained by NSM patients,13 and despite decreased or absent nipple sensation, NSM patients may feel more sexually attractive, resulting in improved sexual well-being. Similar to the findings in our study, a prior report from our institution utilizing the BREAST-Q to compare 52 NSM patients with 202 patients who underwent skin-sparing mastectomy with nipple reconstruction reported higher psychosocial and sexual well-being scores in NSM patients, but no difference in satisfaction with breasts or satisfaction with outcome. There was no collection of preoperative BREAST-Q scores in this population.13
Two small studies prospectively utilized the BREAST-Q patient-reported outcome measure preoperatively to assess satisfaction longitudinally following NSM. In a study of 39 women undergoing NSM, satisfaction with breasts and psychosocial well-being were higher at 2 years postoperatively than at baseline.15 In the second, 28 patients undergoing NSM had decreased satisfaction with breasts, psychosocial, and sexual well-being scores initially, that subsequently returned to baseline after 1 year.26 These studies, coupled with the findings of our study, emphasize the importance of the time period of assessment in outcomes. While it is not surprising that outcomes are worse in the early post–treatment period where patients may still be suffering the sequelae of chemotherapy and radiotherapy, and scars have not begun to fade, our study found that satisfaction with breasts and overall outcome diminishes over time in both NSM and TM patients. This may reflect a lack of satisfaction with implant-based reconstructions over time, but emphasizes that retrospective comparisons between NSM and TM patients with variable lengths of follow-up have limited validity.
Strengths of this study include the evaluation of a relatively large cohort of NSM patients with the use of a validated patient-reported outcome measure. There was adjustment for differences in baseline patient characteristics, disease features, and treatment in this well-characterized patient population. In a subset of patients, there was also control for preoperative BREAST-Q score, allowing for a more reliable comparison between groups.
Limitations include the retrospective nature of the study. However, the BREAST-Q information was collected at the time of treatment, and the database utilized for patient identification and clinical variables is prospectively maintained. Patients were not randomized, and so selection bias exists in who received NSM or TM, although this reflects real-world clinical practice and differences were controlled for in the statistical model. Additionally, not every patient who underwent mastectomy during the study period completed a BREAST-Q survey. There may be undetected differences in women who chose to complete the BREAST-Q and those who did not, although these differences would be expected to affect NSM and TM patients similarly. Lastly but importantly, the study was underpowered to detect differences in outcomes between NSM and TM due to the small size of the NSM group.
In conclusion, the decision to perform NSM vs. TM should be individualized, taking the patient’s preferences into account. It is imperative to provide patients with information regarding oncologic safety, complications, cosmetic outcome, as well as patient satisfaction, and set realistic expectations. Quality-of-life outcomes after NSM should be discussed with patients weighing the risks and benefits of this procedure.
Synopsis:
Patient satisfaction following nipple-sparing mastectomy (NSM) and total mastectomy was compared utilizing the BREAST-Q patient-reported outcome measure. We found enhanced psychosocial and sexual well-being following NSM, but no difference in satisfaction with breasts or satisfaction with overall outcome.
Acknowledgments
Disclosures: The preparation of this manuscript was funded in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center, and this study has been accepted for presentation in podium format at the 19th Annual Meeting of the American Society of Breast Surgeons, May 2–6, 2018, Orlando, FL. Dr. Monica Morrow is a consultant for Genomic Health. Dr. Pusic is a co-developer of the BREAST-Q and receives royalties when the questionnaire is used in for-profit industry-sponsored clinical trials.
Footnotes
AUTHORS’ DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST
The preparation of this manuscript was funded in part by NIH/NCI Cancer Center Support Grant No. P30 CA 0087348 to Memorial Sloan Kettering Cancer Center, and this study has been accepted for presentation in podium format at the 19th Annual Meeting of the American Society of Breast Surgeons, May 2–6, 2018, Orlando, FL. Dr. Monica Morrow is a consultant for Genomic Health. Dr. Pusic is a co-developer of the BREAST-Q and receives royalties when the questionnaire is used in for-profit industry-sponsored clinical trials.
REFERENCES
- 1.Krajewski AC, Boughey JC, Degnim AC, Jakub JW, Jacobson SR, Hoskin TL, Hieken TJ. Expanded Indications and Improved Outcomes for Nipple-Sparing Mastectomy Over Time. Ann Surg Oncol 2015;22(10):3317–23. [DOI] [PubMed] [Google Scholar]
- 2.Freeman BS. Complications of subcutaneous mastectomy with prosthetic replacement, immediate or delayed. South Med J 1967;60(12):1277–80. [DOI] [PubMed] [Google Scholar]
- 3.Freeman BS. Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Reconstr Surg Transplant Bull 1962;30:676–82. [DOI] [PubMed] [Google Scholar]
- 4.Freeman BS. Technique of subcutaneous mastectomy with replacement; immediate and delayed. Br J Plast Surg 1969;22(2):161–6. [DOI] [PubMed] [Google Scholar]
- 5.Network NCC. NCCN Clinical Practice Guidelines in Oncology: Breast Cancer 2018.
- 6.Matsen CB, Mehrara B, Eaton A, Capko D, Berg A, Stempel M, Van Zee KJ, et al. Skin Flap Necrosis After Mastectomy With Reconstruction: A Prospective Study. Ann Surg Oncol 2016;23(1):257–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rusby JE, Smith BL, Gui GP. Nipple-sparing mastectomy. Br J Surg 2010;97(3):305–16. [DOI] [PubMed] [Google Scholar]
- 8.Galimberti V, Vicini E, Corso G, Morigi C, Fontana S, Sacchini V, Veronesi P. Nipple-sparing and skin-sparing mastectomy: Review of aims, oncological safety and contraindications. Breast 2017;34 Suppl 1:S82–s4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jakub JW, Peled AW, Gray RJ, Greenup RA, Kiluk JV, Sacchini V, McLaughlin SA, et al. Oncologic Safety of Prophylactic Nipple-Sparing Mastectomy in a Population With BRCA Mutations: A Multi-institutional Study. JAMA Surg 2017. [DOI] [PMC free article] [PubMed]
- 10.de Alcantara Filho P, Capko D, Barry JM, Morrow M, Pusic A, Sacchini VS. Nipple-sparing mastectomy for breast cancer and risk-reducing surgery: the Memorial Sloan-Kettering Cancer Center experience. Ann Surg Oncol 2011;18(11):3117–22. [DOI] [PubMed] [Google Scholar]
- 11.Petit JY, Veronesi U, Lohsiriwat V, Rey P, Curigliano G, Martella S, Garusi C, et al. Nipple-sparing mastectomy--is it worth the risk? Nat Rev Clin Oncol 2011;8(12):742–7. [DOI] [PubMed] [Google Scholar]
- 12.Wellisch DK, Schain WS, Noone RB, Little JW 3rd., The psychological contribution of nipple addition in breast reconstruction. Plast Reconstr Surg 1987;80(5):699–704. [DOI] [PubMed] [Google Scholar]
- 13.Wei CH, Scott AM, Price AN, Miller HC, Klassen AF, Jhanwar SM, Mehrara BJ, et al. Psychosocial and Sexual Well-Being Following Nipple-Sparing Mastectomy and Reconstruction. Breast J 2016;22(1):10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jabor MA, Shayani P, Collins DR Jr., Karas T, Cohen BE Nipple-areola reconstruction: satisfaction and clinical determinants. Plast Reconstr Surg 2002;110(2):457–63; discussion 64–5. [DOI] [PubMed] [Google Scholar]
- 15.Howard MA, Sisco M, Yao K, Winchester DJ, Barrera E, Warner J, Jaffe J, et al. Patient satisfaction with nipple-sparing mastectomy: A prospective study of patient reported outcomes using the BREAST-Q. J Surg Oncol 2016;114(4):416–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mesdag V, Regis C, Tresch E, Chauvet MP, Boulanger L, Collinet P, Giard S. Nipple sparing mastectomy for breast cancer is associated with high patient satisfaction and safe oncological outcomes. J Gynecol Obstet Hum Reprod 2017;46(8):637–42. [DOI] [PubMed] [Google Scholar]
- 17.Bailey CR, Ogbuagu O, Baltodano PA, Simjee UF, Manahan MA, Cooney DS, Jacobs LK, et al. Quality-of-Life Outcomes Improve with Nipple-Sparing Mastectomy and Breast Reconstruction. Plast Reconstr Surg 2017;140(2):219–26. [DOI] [PubMed] [Google Scholar]
- 18.Platt J, Zhong T. Patient-Centered Breast Reconstruction Based on Health-Related Quality-of-Life Evidence. Clin Plast Surg 2018;45(1):137–43. [DOI] [PubMed] [Google Scholar]
- 19.Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 2009;124(2):345–53. [DOI] [PubMed] [Google Scholar]
- 20.Cano SJ, Klassen AF, Scott AM, Pusic AL. A closer look at the BREAST-Q((c)). Clin Plast Surg 2013;40(2):287–96. [DOI] [PubMed] [Google Scholar]
- 21.Little JW 3rd. Nipple-areola reconstruction. Clin Plast Surg 1984;11(2):351–64. [PubMed] [Google Scholar]
- 22.Didier F, Radice D, Gandini S, Bedolis R, Rotmensz N, Maldifassi A, Santillo B, et al. Does nipple preservation in mastectomy improve satisfaction with cosmetic results, psychological adjustment, body image and sexuality? Breast Cancer Res Treat 2009;118(3):623–33. [DOI] [PubMed] [Google Scholar]
- 23.Metcalfe KA, Cil TD, Semple JL, Li LD, Bagher S, Zhong T, Virani S, et al. Long-Term Psychosocial Functioning in Women with Bilateral Prophylactic Mastectomy: Does Preservation of the Nipple-Areolar Complex Make a Difference? Ann Surg Oncol 2015;22(10):3324–30. [DOI] [PubMed] [Google Scholar]
- 24.Satteson ES, Brown BJ, Nahabedian MY. Nipple-areolar complex reconstruction and patient satisfaction: a systematic review and meta-analysis. Gland Surg 2017;6(1):4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van Verschuer VM, Mureau MA, Gopie JP, Vos EL, Verhoef C, Menke-Pluijmers MB, Koppert LB. Patient Satisfaction and Nipple-Areola Sensitivity After Bilateral Prophylactic Mastectomy and Immediate Implant Breast Reconstruction in a High Breast Cancer Risk Population: Nipple-Sparing Mastectomy Versus Skin-Sparing Mastectomy. Ann Plast Surg 2016;77(2):145–52. [DOI] [PubMed] [Google Scholar]
- 26.Peled AW, Duralde E, Foster RD, Fiscalini AS, Esserman LJ, Hwang ES, Sbitany H. Patient-reported outcomes and satisfaction after total skin-sparing mastectomy and immediate expander-implant reconstruction. Ann Plast Surg 2014;72 Suppl 1:S48–52. [DOI] [PubMed] [Google Scholar]


