Significance
Wellbeing falters without sound mental health. Scholars have recently indicated that the impacts of climate change are likely to undermine mental health through a variety of direct and indirect mechanisms. Using daily meteorological data coupled with information from nearly 2 million randomly sampled US residents across a decade of data collection, we find that experience with hotter temperatures and added precipitation each worsen mental health, that multiyear warming associates with an increased prevalence of mental health issues, and that exposure to tropical cyclones, likely to increase in frequency and intensity in the future, is linked to worsened mental health. These results provide added large-scale evidence to the growing literature linking climate change and mental health.
Keywords: climate, mental health, natural disasters, psychology, weather
Abstract
Sound mental health—a critical facet of human wellbeing—has the potential to be undermined by climate change. Few large-scale studies have empirically examined this hypothesis. Here, we show that short-term exposure to more extreme weather, multiyear warming, and tropical cyclone exposure each associate with worsened mental health. To do so, we couple meteorological and climatic data with reported mental health difficulties drawn from nearly 2 million randomly sampled US residents between 2002 and 2012. We find that shifting from monthly temperatures between 25 °C and 30 °C to >30 °C increases the probability of mental health difficulties by 0.5% points, that 1°C of 5-year warming associates with a 2% point increase in the prevalence of mental health issues, and that exposure to Hurricane Katrina associates with a 4% point increase in this metric. Our analyses provide added quantitative support for the conclusion that environmental stressors produced by climate change pose threats to human mental health.
Social, economic, and physical systems are critical determinants of psychological wellbeing (1). By disrupting these systems, climate change is likely to exacerbate known risk factors for mental disorders (2). Mental health difficulties are already common and costly (3). Nearly one-half of Americans will experience mental illness in their lifetime (4), with anxiety, stress-related, and mood disorders comprising the majority of diagnoses (5). These psychological disorders worsen overall health (6, 7), diminish productivity (8), and reduce quality of life (3, 9). Even subclinical levels of distress can impair psychological (10, 11) and immunological (12) functioning, reducing the ability to cope with adversity.
Over the past decade, scholars have highlighted the direct and indirect threats that climate change poses to mental health (13, 14). Warming is likely to amplify the frequency and intensity of natural disasters (15), which often cause physical injury, psychological trauma, infrastructure damage, and societal disruption in affected regions. Gradual changes in climate are also expected to alter human systems in costly ways. Rising temperatures amplify risks to human physical health (16), harm economic activity (17), spur social conflict (18), and produce forced migration (19). Some communities are already experiencing disruption of livelihood and associated grief in the face of ecological losses (20). While the precise magnitude of these climate-induced adversities is difficult to estimate, the theoretical relationship between climate change and mental health risk is compelling (2, 21).
Empirical investigations of this relationship have primarily focused on discrete climatic events and weather extremes. For example, exposure to hurricanes and floods is associated with symptoms of acute depression as well as posttraumatic stress disorder (22–27). Furthermore, both heat and drought amplify the risk of suicide (28–30), and psychiatric hospital visits increase during hotter temperatures (31–33). Those with preexisting mental health conditions and lower socioeconomic status are among the most vulnerable to these adverse environmental conditions (21). However, population-level impacts have been difficult to characterize, as most investigations have been qualitative, local in scale, or limited to only the most severe mental health outcomes. Although we are beginning to understand the ways in which weather influences other psychological phenomena, such as cognition (34), emotional expression (35), and sleep (36), large-scale quantification of the mental health risks posed by climate change is lacking (2).
To begin to address this gap, we report on the relationship between historical climatic conditions and the mental health of 2 million randomly sampled US residents between 2002 and 2012 (study materials are available on Harvard’s Dataverse: https://doi.org/10.7910/DVN/OVQY76). Our measure of individuals’ reported mental health is drawn from the Center for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System (BRFSS) between 2002 and 2012 (37). Respondents answered the following question: “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 d was your mental health not good?”
We code responses to this question as one if respondents indicate mental health difficulties over the period and zero otherwise (see Data). This measure has been shown to possess both psychometric test–retest reliability (38) and convergent validity with other standard measures of mental health status (39, 40). While not a direct measure of psychiatric disorders, this item has a number of strengths. First, it is to our knowledge the best large-scale, randomly sampled measure of individual mental health status in the United States. Second, the measure is spatially and temporally referenced in a manner that enables precise pairing with meteorological data. Third, it is likely able to capture both clinical and subclinical distress across a wide set of possible symptoms (5) and unlike measures of health care utilization, can account for the substantial portion of US adults who fail to seek treatment (41).
We combine our mental health data with meteorological data and empirical tools drawn from the climate econometrics literature to investigate the historical relationship between climatic variations and human mental health. These historical relationships can aid in estimating the magnitude of the risks that climate change poses to mental health. Following the theoretical framework of Bourque and Cunsolo Willox (14), we examine three selected types of environmental stressors likely to be produced by climate change: short-run meteorological exposure, multiyear warming, and acute exposure to natural disasters. We examine three questions.
First, anthropogenic warming is likely to present humans with increasingly extreme meteorological conditions in any given year (42). Do recently experienced meteorological stressors affect individuals’ reported mental health? Additionally, are those who are most vulnerable to mental health challenges more affected by such meteorological stress (14)? In our sample, more vulnerable populations include those with lower incomes, those who experience a higher average burden of mental health problems (43), and those who may be less able to smooth adverse temperatures (44) as well as women, who are more susceptible to the mental health difficulties captured by our measure (4). To examine this set of questions, we use pooled cross-sectional analyses, leveraging exogenous meteorological variation to examine the effect of short-run (past 30 d) weather exposure on individuals’ mental health outcomes (Pooled Cross-Section and SI Appendix, Fig. S2) (45).
Second, climate change is also likely to increase the rates of year-over-year and decade-over-decade warming of local climates and the chronic stressors that such warming produces (14, 46). Does longer-term warming have detrimental impacts on individual mental health over time? To examine this question, we use the long-differences approach (47), examining the association between spatial variation in multiyear warming and longer-run changes in mental health (Long Differences and Fig. 3B).
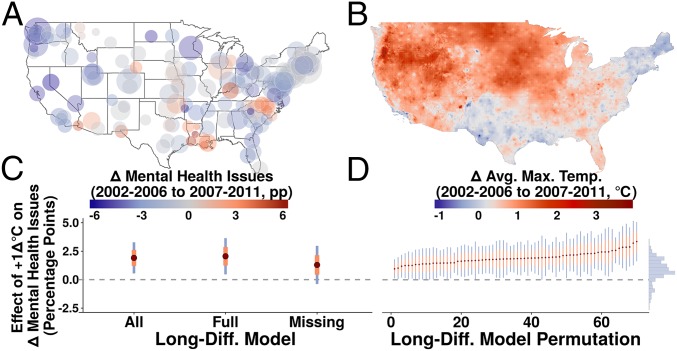
Fig. 3.
Longer-term warming and rates of mental health issues. A presents the change in prevalence of mental health issues between 2002–2006 and 2007–2011. Points are scaled by the number of respondents from each city. B plots the change in grid cell average maximum temperatures over this same period. C plots the coefficient estimates from the long-differences model, including all observations, the model excluding cities missing any years, and the model including only the cities missing 1 or more years in our sample, respectively. D plots the results of a permutation of all possible long-differences combinations in our data where the difference between periods is at least 5 y. The coefficient estimates from this process with 95% confidence intervals that do not contain zero are points in D. We display all coefficient estimates from this permutation process in the histogram to the right in D. Orange error lines represent one SE, and blue lines represent 95% confidence intervals.
Third, climate change is also likely to amplify the frequency and intensity of acute climatic events, like tropical cyclones (14, 15). Does direct exposure to costly tropical cyclones worsen individual mental health outcomes? To examine this question, we use a difference-in-differences approach, leveraging the landfall of Hurricane Katrina to examine the association between tropical cyclone exposure and our measure of reported mental health outcomes (Difference-in-Differences) (48).
Results
Short-Run Weather Exposure.
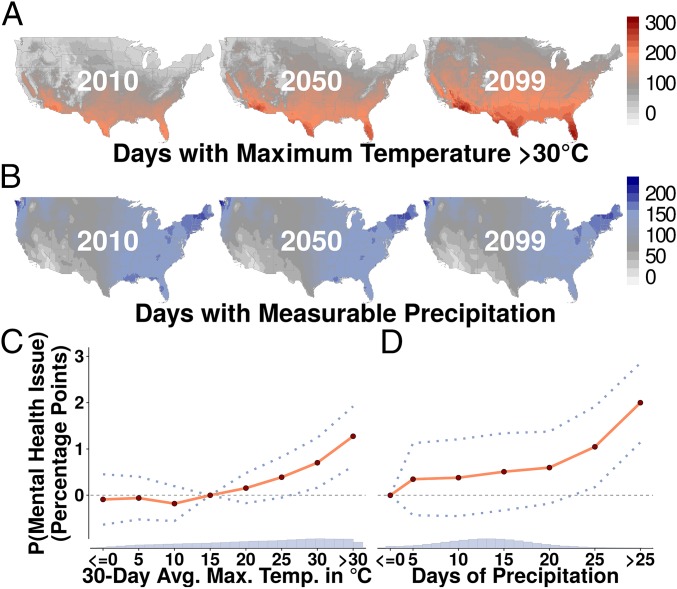
The results of estimating our pooled cross-sectional regression indicate that exogenous increases in monthly temperature (Fig. 1C and SI Appendix, Fig. S2) and added precipitation days (Fig. 1D) each amplify the monthly probability of experiencing mental health issues (Pooled Cross-Section and SI Appendix, Table S1). Average maximum temperatures greater than 30 °C amplify the probability of mental health issues by over 1% point compared with 10 °C to 15 °C (coefficient: 1.275, P < 0.001, n = 1,961,743). Months with greater than 25 d of precipitation increase the probability of mental health issues by 2% points compared with zero monthly precipitation days (coefficient: 2, P < 0.001, n = 1,961,743). Putting scale to the magnitude of this estimated relationship, a uniform shift from monthly temperatures between 25 °C and 30 °C to averages greater than 30 °C, if extrapolated across the current population of the United States over a 30-d period, would produce almost 2 million additional individuals reporting mental health difficulties.
Fig. 1.
Higher temperatures and precipitation increase risk of mental health issues. A presents projections of warming in the United States along the RCP8.5 high-emissions scenario. The annual number of days with maximum temperatures C is projected to markedly increase over this century. B plots the projected number of annual days with measurable precipitation (1 mm). C draws from nearly 2 million respondents’ reports of monthly mental health issues between 2002 and 2012. It plots the predicted probability of reporting any mental health issues for each 30-d average maximum temperature bin. The probability of mental health issues steadily increases past C to C. D depicts that precipitation days increase the probability of mental health issues. Dotted lines represent 95% confidence intervals.
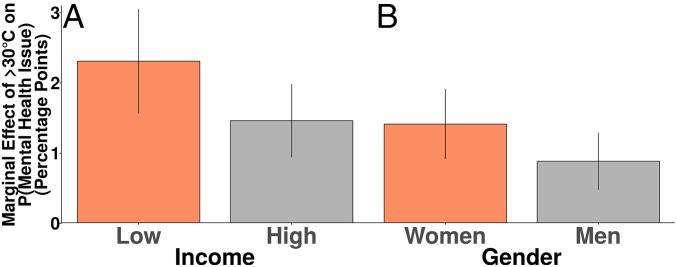
To examine if poorer respondents are more sensitive to temperature, we stratify our sample along income quartiles and estimate regressions for the lowest and highest quartiles (SI Appendix, Table S8). Fig. 2A shows that the negative effect of temperatures greater than 30 °C on the probability of mental health issues is larger for low-income respondents (coefficient: 2.309, P = 0.002, n = 438,518). This is 1.6 times the effect observed among the highest-income adults in the sample (coefficient: 1.458, P = 0.005, n = 509,608).
Fig. 2.
Heat effects are more acute among low-income respondents and among women. A displays the marginal effects produced by splitting the sample between the first and fourth quartiles of income. Those with incomes in the first quartile have amplified probabilities of reporting mental health issues in response to higher temperatures. B stratifies the sample by gender. The effects of higher temperatures on mental health issues are larger among women. All marginal effects are significant at the level. Error bars are SEM.
Fig. 2B shows that the negative effect of temperatures greater than 30 °C on the probability of mental health difficulties is largest for women (coefficient: 1.41, P = 0.005, n = 1,211,220). This is 1.6 times the effect observed among men in our sample (coefficient: 0.879, P = 0.031, n = 750,523). Combining these insights, the effect observed in the subsample of low-income women (coefficient: 2.742, P = 0.002, n = 300,570) is approximately two times the magnitude of the effect observed in the high-income men in the sample (coefficient: 1.373, p = 0.03, n = 235,098).
Looking forward, we observe that days with temperatures that exceed 30 °C are likely to become more common in the future (Fig. 1A), particularly in the US South. Changes in precipitation are projected with less certainty (Fig. 1B). Our examination of these projections indicates that any climate change-induced alteration in US mental health outcomes would be more likely due to changes in future temperature distributions than the smaller magnitude projected shifts in precipitation days (Climatic Data).
Multiyear Warming.
To investigate the effects of multiyear warming on mental health, we use the long-differences approach (28, 45, 47), leveraging spatial variation in city-level changes between the years 2002–2006 and 2007–2011 (Fig. 3B) to identify the relationship between multiyear warming and longer-term changes in mental health outcomes (Fig. 3A).
Fig. 3C presents the results of estimating our long-differences equation (Long Differences and SI Appendix, Table S9). Across the cities in our sample that have representation in both periods, we find that a 1 °C increase in average maximum temperatures associates with an approximately 2% point increase in prevalence of reported mental health difficulties (coefficient: 1.913, p = 0.007, n = 156). This estimate is slightly larger if we include only the cities that have subjects across each year in the sample (coefficient: 2.055, p = 0.014, n = 78), while cities that are missing some years produce a smaller estimate (coefficient: 1.293, P = 0.134, n = 78), possibly due to attenuation from added measurement error (48).
To ensure that our estimates are not sensitive to our specific choice of preperiod and postperiod, we estimate our regression across all possible combinations of years in the sample where the preperiod is at least 5 y before the postperiod (SI Appendix, Fig. S8). This procedure results in 278 unique estimates. We depict the estimates with 95% confidence intervals that do not include zero as points in Fig. 3D and display the distribution of all estimates in the histogram on the right. The median estimate from this permutation procedure suggests that a multiyear 1 °C increase in maximum temperatures produces a 0.8% point increase in prevalence of mental health issues.
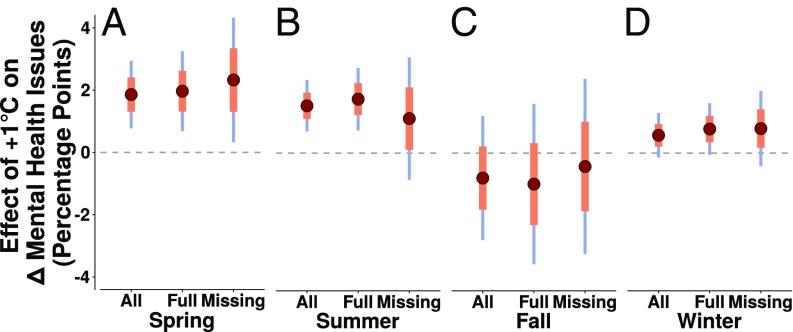
Furthermore, we observe that multiyear warming during the spring and summer has the largest effects on the prevalence of mental health issues compared with warming that occurred during fall and winter months. We display the estimated effects from these by-season models in Fig. 4 (SI Appendix, Table S13).
Fig. 4.
Multiyear warming and prevalence of mental health problems across the seasons of the year. A plots the results of estimating the long-differences model for spring, B plots the results of estimating the long-differences model for summer, C plots the results of estimating the long-differences model for fall, and D pots the results of estimating the long-differences model for winter. Orange error lines represent one SE, and blue lines represent 95% confidence intervals.
Natural Disaster.
To examine the relationship between tropical cyclone exposure and mental health, we make use of the catastrophic landfall of Hurricane Katrina in late August 2005. Hurricane Katrina resulted in one of the worst disasters in US history and affected millions of individuals along the US Gulf Coast (49).
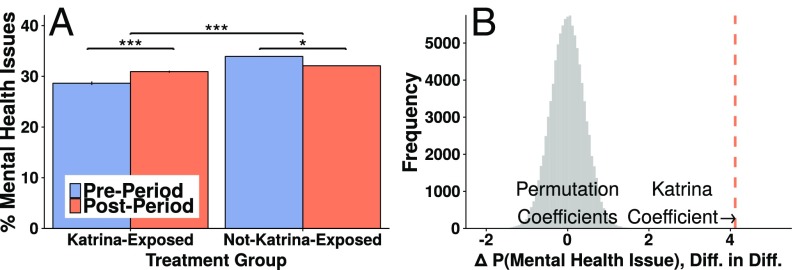
Fig. 5A shows that nondisaster areas observed a decrease in reports of mental health issues in the period after Katrina compared with the pre-Katrina period (Difference-in-Differences and SI Appendix, Table S14). Cities with declared disasters observed an increase in reports of mental health issues over this same period. The difference-in-differences estimate indicates that Katrina exposure increased the occurrence of mental health issues by approximately 4% points compared with nondisaster areas (coefficient: 4.12, p = 0.007, n = 1,961,743). Fig. 5B indicates that the coefficient estimate from our difference-in-differences regression falls substantially outside the distribution of coefficients estimated on 100,000 placebo regressions with randomly permuted group assignments.
Fig. 5.
Worsened mental health in areas affected by Hurricane Katrina. A depicts the mean prevalence of mental health difficulties for the Katrina-exposed and non—Katrina-exposed groups before and after Hurricane Katrina landfall. Locales not exposed to Katrina observed a drop in rates of mental health issues, while locales exposed to Katrina experienced an increase. The difference-in-differences estimate indicates that Hurricane Katrina exposure associates with an increase in prevalence of mental health issues. All differences are significant at . Error bars are SEM. B plots the results of randomly permuting 100,000 treatment status assignments and conducting our difference-in-differences regression for each permutation. The true difference-in-differences estimate falls substantially outside the distribution of permutation coefficients.
Discussion
By spatially and temporally linking individuals’ reports of mental health difficulties to the environmental exposures that they experienced, we show that short-term weather, multiyear warming, and tropical cyclone exposure each relate to worsened mental health outcomes. The effect of shifting from average monthly temperatures between 25 °C and 30 °C to averages greater than 30 °C on the probability of mental health difficulties (+0.5% points) is approximately one-quarter the size of the association between 1 °C of 5-y warming and the prevalence of mental health issues (+2% points), which is, in turn, one-half the size of the association between exposure to Hurricane Katrina and occurrence of mental health difficulties (+4% points).
A number of considerations are important to the interpretation of our results. First, an optimal measure would contain added information on the nature and severity of each individual’s particular mental health symptoms. Future studies should investigate the risks posed by climate change to specific psychiatric and neurobehavioral symptoms, such as substance use and psychosis. Varied psychopathology, subclinical distress, and chronic stress each confer unique risks and treatment needs.
Second, our data consist of a randomly sampled, pooled cross-section of respondents. An ideal source of data would track the same individuals over time to enable controlling for individual-specific characteristics and more precisely monitoring mental health responses to climatic factors over time. This limitation is notable in the case of our Hurricane Katrina analysis, where results may be partially attributable to selection out of affected areas.
Third, we do not uncover the causally mediating factors underlying our results. Exposure to more extreme meteorological conditions may produce physiological stressors that precipitate poor mental health, such extremes may initiate inflammatory processes that worsen mental health, or the effects may run entirely through reductions in health maintenance behaviors, like exercise (50) and sleep (36). Future studies and advances in climate econometric methods (45) are needed to investigate causal mediation in this setting.
Fourth, measurement error exists between the temperatures that we observe and the temperatures that respondents actually experienced, attenuating the magnitude of our estimates (48). This added measurement error suggests that our temperature-related estimates may represent a lower bound of the effects of temperature on mental health.
Fifth, we observe that the mental health of low-income individuals may be most harmed by a changing climate. However, our data are from a wealthy country with a temperate climate. Regions with less-temperate climates, insufficient resources (51), and greater reliance on ecological systems may see more severe effects of climate change on mental health (28).
Sixth, we examine three selected types of environmental adversity likely to be produced by climate change. As a result, our estimates only represent a sampling of the possible risks that climate change poses to mental health. Unfortunately, clear historical analogs for other climate-induced environmental stressors—like inundation from sea-level rise—are more difficult to measure. Nonetheless, it is vital for future large-scale empirical studies to investigate the many additional ways that climate change might harm mental health.
Seventh, while robust to many tests (Methods), we cannot definitively rule out unobserved heterogeneity with respect to our long-differences and difference-in-differences estimation procedures. As a result, care is warranted with respect to the causal interpretation of these estimates.
Eighth, we measure the direct effect of exposure to environmental stressors on self-reported mental health. Worry about climate change itself may exacerbate these environmental impacts on mental wellbeing (52, 53). Moreover, interactive effects between exposure to climatic stressors and other social stressors may modify these effects.
Ninth, our observed effects may not persist into the future. Humans may adapt technologically and physiologically to warmer climates to minimize the impact of warming on mental health (44). Individuals may also adapt via psychological coping mechanisms, such as avoidance, seeking social support (54), or fostering mental preparedness (55).
Ultimately, if observed relationships from the recent past persist, added climate change may amplify the society-wide mental health burden in the face of the acute environmental threats produced by warming in natural systems. Given the vital role that sound mental health plays in personal, social, and economic wellbeing—as well as in the ability to address pressing personal and social challenges—our findings provide added evidence that climatic changes pose substantial risks to human systems.
Methods
Data.
We dichotomize our BRFSS measure of mental health difficulties, as recall of mental health difficulties may be susceptible to memory limitations given the interaction of psychological distress and cognitive functioning (56), adding error to the 30-d measure (48). Supporting this, the distribution of the answers to our mental health variable presents a clustering at weeks of the month as well as at 5-d intervals, although the true underlying distribution is likely continuous (SI Appendix, Fig. S9). Whether or not a person experienced any mental health difficulties over the past 30 d (our dichotomized measure) is likely more reliable. SI Appendix, Fig. S1 plots respondents over time.
We use gridded (at ∼4 km) daily temperature and precipitation from the PRISM Climate Group (57) and average daily cloud cover, relative humidity, and wind speed from the National Centers for Environmental Prediction Reanalysis II project (58). Global circulation model projections use NASA Earth Exchange’s maximum temperature and precipitation projections for 2010, 2050, and 2099 (59) from 21 of the Coupled Model Intercomparison Project Phase 5 (CMIP5) models (60) run on Representative Concentration Pathway 8.5 (RCP8.5) (high-emission scenario) (61). SI Appendix, Figs. S10 and S11 presents the spatial and temporal distributions of these projected changes.
Pooled Cross-Section.
Our relationship of interest is the marginal effect of recent meteorological conditions on the probability of experiencing mental health issues. We model this as
| [1] |
In this pooled cross-sectional linear probability model, indexes individuals, indexes cities, indexes states, indexes calendar days, and indexes calendar years. Our dependent variable is binary and represents whether respondents in city in state on calendar day within calendar year reported experiencing any days of poor mental health over the 30 d before their interview date.
and represent the 30-d average of daily maximum temperatures and number of precipitation days over the same 30-d window as respondents’ reported mental health, respectively. We control for average diurnal temperature range, percentage of cloud cover, relative humidity, and wind speed, which are represented via , as failure to do so may bias our primary estimates (45). Bold terms in equations denote matrices.
We use separate indicator variables for each 5 °C 30-d average maximum temperature bin and for each 5-d bin of precipitation days, which are represented by and , respectively. This allows for flexible estimation of a nonlinear relationship between our main meteorological variables and mental health outcomes (50). We omit the 10 °C to 15 °C maximum temperature and 0–5 precipitation days indicator variables and interpret our estimates as the change in probability of reporting recent mental health issues associated with a particular temperature or precipitation day range relative to these baselines.
To ensure that time-invariant city-specific factors do not bias our estimates of the effect of weather on mental health outcomes, we include —representing nonparametric city fixed effects—in Eq. 1 (48). Furthermore, there may be unobserved daily considerations or region-specific time trends influencing our mental health outcomes that could spuriously correlate with the weather. To control for these potential confounds, we include and in Eq. 1, representing calendar date and state-by-year fixed effects, respectively.
Our empirical identifying assumption is that the remaining variation in 30-d maximum temperature and precipitation is as good as random after conditioning on these fixed effects (45, 62) (SI Appendix, Fig. S2). The estimated coefficients from and from this estimation can thus be interpreted as the causal effects of maximum temperature and precipitation days on the 30-d occurrence of mental health issues (45, 62). We adjust for spatial and serial correlation in by using heteroskedasticity-robust SEs clustered at the state level (48). We omit nonclimatic control variables from Eq. 1 because of their potential to generate posttreatment bias in our parameters of interest (18, 45).
Our estimates are robust to varying functional form specification of our main meteorological variables. SI Appendix, Fig. S3 shows that results are robust to varying the size of our temperature and precipitation bins. SI Appendix, Fig. S4 and Table S2 shows that results are robust to modeling average maximum temperatures with a quadratic and precipitation days linearly. SI Appendix, Fig. S5 and Table S3 shows that results are robust to using the full distribution of daily maximum temperatures over the period (63). Coefficient estimates in this model represent the effect on probability of reporting mental health issues of having 1 additional day of the 30-d window falling in the specified maximum temperature bin.
Our estimates are also robust to varying control variable inclusion. SI Appendix, Table S1 shows that results are robust to progressively dropping meteorological controls. SI Appendix, Table S4 shows that our functional forms persist even when choosing less stringent sets of fixed effects (although we prefer our primary fixed effects specification, as it controls for the most confounding variation). SI Appendix, Table S5 shows that our results are robust to varying inclusion of demographic controls. We model our demographic controls with nonparametric bins and introduce them as fixed effects into the estimation. Of note, our sample size in these regressions varies, as not all respondents answered each question.
Furthermore, SI Appendix, Fig. S6 shows that our results are not driven by any one particular state’s respondents, SI Appendix, Fig. S7 indicates that our results are not entirely driven by any one census division, and SI Appendix, Table S6 shows that our results are robust to aggregating to the city-day unit of analysis and weighting regressions by the number of respondents on each city-day. Finally, one might be concerned that meteorological factors produce differential rates of response to the BRFSS survey in ways that limit the external validity of our findings. SI Appendix, Table S7 presents minimal evidence of the effect of meteorology on sample collection, indicating a low threat of sample selection bias driven by the meteorological variables that we use. Finally, our pooled cross-sectional results are robust to using the count of mental health days outcome variable in the context of both an ordinary least squares and a negative binomial model (SI Appendix, Table S19). In the negative binomial model, we substitute year-month, day-of-week, and city-level fixed effects for computational tractability (to our knowledge, no package exists in R to estimate the size of our full fixed effects matrix in a negative binomial model).
Long Differences.
To model the relationship between multiyear changes in average maximum temperatures and multiyear changes in average mental health outcomes, we take the mean of our dependent and independent variables over two separate periods, a and b, with period a falling temporally before period b (45, 47). Our main model uses data from period a (2002–2006) to period b (2007–2011) for each city. For example, for our mental health issues outcome measure, , we calculate as and similarly, for the and over the same period. This results in the below equation for period a:
| [2] |
In Eq. 2, indexes cities, indexes states, and represents city-level fixed effects that control for time-invariant city-specific factors. Calculating the same metrics for period b results in the below equation:
| [3] |
Then, differencing Eqs. 2 and 3 results in
| [4] |
In Eq. 4, the city-level, time-invariant fixed effects () terms drop out (and are thus not potential confounds). Thus, the long-differences approach implicitly controls for time-invariant city factors in the way that we explicitly control for them in the pooled cross-sectional regressions. We are left with our long-differences model:
| [5] |
from Eq. 5 provides an estimate of multiyear warming on multiyear change in rates of individuals reporting mental health issues. In Eq. 5, represents changes in other meteorological variables. We weight the regression by the number of respondents in a city for statistical efficiency and again, cluster our errors at the state level. Unbiasedness of requires that city-level changes in mean maximum temperature between our two periods are uncorrelated with unobserved time-varying variables that alter our mental health outcomes of interest (47).
SI Appendix, Table S9 shows that results are robust to excluding those cities with missing observations in either period a or period b. SI Appendix, Table S10 shows that results are robust to using percentage change in maximum temperature from baseline rather than absolute level of temperature change.
Furthermore, given that unobserved time-varying variables could confound our estimation, SI Appendix, Table S11 shows that our long-differences results persist across a varied set of demographic controls calculated using the BRFSS demographics questions. Adding to these results is SI Appendix, Table S12, where we use demographic variables drawn from the US Census Bureau to externally measure changes in demographic composition of cities. Our results are robust to the inclusion and varied specification of these controls as well. However, as these demographic variables may themselves be driven by longer-term changes in meteorological variables and thus, serve as “bad controls,” we prefer the specifications that exclude demographic controls (45). Finally, our long-differences results are also robust to using the count of mental health days outcome variable (SI Appendix, Table S19).
Difference-in-Differences.
We leverage the landfall of Hurricane Katrina to estimate the relationship between disaster exposure and mental health outcomes using a difference-in-differences design (48):
| [6] |
In Eq. 6, represents an individual’s mental health as in Eq. 1. We retain indices from earlier equations and again cluster our errors at the state level. is equal to one for the post-Katrina period in our data (from August 24, 2005 to February 1, 2012) and zero otherwise. is equal to one if city received a federal disaster declaration in response to Hurricane Katrina and zero otherwise. represents the interaction of these two terms. Our estimate of interest, , represents the relationship between a city’s experience with Hurricane Katrina and residents’ subsequent mental health outcomes. Unbiasedness of requires the assumption of no contemporaneous shocks and that disaster affected areas were trending similarly to nondisaster areas before hurricane landfall (48).
SI Appendix, Table S14 indicates that results are robust to using a Katrina exposure indicator variable coupled with city and date fixed effects. This specification more flexibly controls for time-invariant city-specific factors as well as any idiosyncratic temporal factors. Furthermore, SI Appendix, Table S15 shows that results are robust to the inclusion of a varied set of respondent-level demographic controls to attempt to control for possible bias induced by unobserved heterogeneity (48). However, as these demographic variables may be affected by Katrina exposure, we prefer the specifications that exclude demographic controls (45). SI Appendix, Table S16 displays that our results are robust to aggregating to the city-day and weighting the regression by number of respondents per city-day.
We also explore alternative selection rules for Katrina-exposed and non–Katrina-exposed groups. SI Appendix, Table S17 shows that results are robust to using only neighboring nondisaster declaration cities from states that geographically border the states that had cities with disaster declarations as the control group. Furthermore, not all cities in the sample are represented in both pre- and post-Katrina periods. SI Appendix, Table S18 shows that results are robust to selecting respondents from only those cities with representation in the sample both before and after landfall. Finally, our difference-in-differences results are robust to using the count of mental health days outcome variable (SI Appendix, Table S19).
Supplementary Material
Acknowledgments
We thank our anonymous reviewers for their constructive feedback on this manuscript.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Data deposition: The study materials are available on Harvard’s Dataverse: https://doi.org/10.7910/DVN/OVQY76.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1801528115/-/DCSupplemental.
References
- 1.Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26:392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- 2.Berry HL, Waite TD, Dear KB, Capon AG, Murray V. The case for systems thinking about climate change and mental health. Nat Clim Change. 2018;8:282–290. [Google Scholar]
- 3.Whiteford HA, et al. Global burden of disease attributable to mental and substance use disorders: Findings from the global burden of disease study 2010. Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moussavi S, et al. Depression, chronic diseases, and decrements in health: Results from the world health surveys. Lancet. 2007;370:851–858. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 7.Prince M, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 8.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 9.Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162:1171–1178. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- 10.Lewinsohn PM, Solomon A, Seeley JR, Zeiss A. Clinical implications of “subthreshold” depressive symptoms. J Abnorm Psychol. 2000;109:345–351. [PubMed] [Google Scholar]
- 11.Marshall RD, et al. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry. 2001;158:1467–1473. doi: 10.1176/appi.ajp.158.9.1467. [DOI] [PubMed] [Google Scholar]
- 12.Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: Implications for health. Nat Rev Immunol. 2005;5:243–251. doi: 10.1038/nri1571. [DOI] [PubMed] [Google Scholar]
- 13.Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: A causal pathways framework. Int J Public Health. 2010;55:123–132. doi: 10.1007/s00038-009-0112-0. [DOI] [PubMed] [Google Scholar]
- 14.Bourque F, Cunsolo Willox A. Climate change: The next challenge for public mental health? Int Rev Psychiatry. 2014;26:415–422. doi: 10.3109/09540261.2014.925851. [DOI] [PubMed] [Google Scholar]
- 15.Webster PJ, Holland GJ, Curry JA, Chang H-R. Changes in tropical cyclone number, duration, and intensity in a warming environment. Science. 2005;309:1844–1846. doi: 10.1126/science.1116448. [DOI] [PubMed] [Google Scholar]
- 16.Watts N, et al. The Lancet countdown: Tracking progress on health and climate change. Lancet. 2017;389:1151. doi: 10.1016/S0140-6736(16)32124-9. [DOI] [PubMed] [Google Scholar]
- 17.Burke M, Hsiang S, Miguel E. Global non-linear effect of temperature on economic production. Nature. 2015;527:235–235. doi: 10.1038/nature15725. [DOI] [PubMed] [Google Scholar]
- 18.Hsiang SM, Burke M, Miguel E. Quantifying the influence of climate on human conflict. Science. 2013;341:1235367. doi: 10.1126/science.1235367. [DOI] [PubMed] [Google Scholar]
- 19.Bohra-Mishra P, Oppenheimer M, Hsiang SM. Nonlinear permanent migration response to climatic variations but minimal response to disasters. Proc Natl Acad Sci USA. 2014;111:9780–9785. doi: 10.1073/pnas.1317166111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cunsolo A, Ellis NR. Ecological grief as a mental health response to climate change-related loss. Nat Clim Change. 2018;8:275–281. [Google Scholar]
- 21.Clayton S, Manning C, Hodge C. Beyond Storms & Droughts: The Psychological Impacts of Climate Change. American Psychological Association and ecoAmerica; Washington, DC: 2014. [Google Scholar]
- 22.Kessler RC, et al. Trends in mental illness and suicidality after Hurricane Katrina. Mol Psychiatry. 2008;13:374–384. doi: 10.1038/sj.mp.4002119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.La Greca AM, Silverman WK, Lai B, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. J Consulting Clin Psychol. 2010;78:794–805. doi: 10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- 24.Pietrzak RH, et al. Resilience in the face of disaster: Prevalence and longitudinal course of mental disorders following Hurricane Ike. PLoS One. 2012;7:e38964. doi: 10.1371/journal.pone.0038964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bei B, et al. A prospective study of the impact of floods on the mental and physical health of older adults. Aging Ment Health. 2013;17:992–1002. doi: 10.1080/13607863.2013.799119. [DOI] [PubMed] [Google Scholar]
- 26.Boscarino JA, et al. Mental health outcomes at the Jersey shore after hurricane sandy. Int J Emerg Ment Health. 2013;15:147–158. [PubMed] [Google Scholar]
- 27.Jermacane D, et al. The English national cohort study of flooding and health: The change in the prevalence of psychological morbidity at year two. BMC Public Health. 2018;18:330. doi: 10.1186/s12889-018-5236-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carleton TA. Crop-damaging temperatures increase suicide rates in India. Proc Natl Acad Sci USA. 2017;114:8746–8751. doi: 10.1073/pnas.1701354114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hanigan IC, Butler CD, Kokic PN, Hutchinson MF. Suicide and drought in New South Wales, Australia, 1970–2007. Proc Natl Acad Sci USA. 2012;109:13950–13955. doi: 10.1073/pnas.1112965109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burke M, et al. Higher temperatures increase suicide rates in the United States and Mexico. Nat Clim Change. 2018;8:723–729. [Google Scholar]
- 31.Hansen A, et al. The effect of heat waves on mental health in a temperate Australian city. Environ Health Perspect. 2008;116:1369–1375. doi: 10.1289/ehp.11339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang X, Lavigne E, Ouellette-kuntz H, Chen BE. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J Affective Disord. 2014;155:154–161. doi: 10.1016/j.jad.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 33.Chan EY, et al. Association between ambient temperatures and mental disorder hospitalizations in a subtropical city: A time-series study of Hong Kong special administrative region. Int J Environ Res Public Health. 2018;15:754. doi: 10.3390/ijerph15040754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zivin JG, Hsiang SM, Neidell M. Temperature and human capital in the short and long run. J Assoc Environ Resource Economists. 2018;5:77–105. [Google Scholar]
- 35.Baylis P, et al. Weather impacts expressed sentiment. PloS One. 2018;13:e0195750. doi: 10.1371/journal.pone.0195750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Obradovich N, Migliorini R, Mednick SC, Fowler JH. Nighttime temperature and human sleep loss in a changing climate. Sci Adv. 2017;3:e1601555. doi: 10.1126/sciadv.1601555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System. US Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta: 2017. [Google Scholar]
- 38.Andresen EM, Catlin TK, Wyrwich KW, Jackson-Thompson J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. 2003;57:339–343. doi: 10.1136/jech.57.5.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moriarty DG, Zack MM, Kobau R. The centers for disease control and prevention’s healthy days measures–Population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1:37. doi: 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kroenke K, et al. The phq-8 as a measure of current depression in the general population. J Affective Disord. 2009;114:163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 41.Substance Abuse and Mental Health Services Administration 2016. Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health, HHS Publication No. SMA 17-5044, NSDUH Series H-52 (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD)
- 42.Fischer E, Knutti R. Anthropogenic contribution to global occurrence of heavy-precipitation and high-temperature extremes. Nat Clim Change. 2015;5:560–564. [Google Scholar]
- 43.Dohrenwend BP, et al. Socioeconomic status and psychiatric disorders: The causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 44.Barreca A, Clay K, Deschenes O, Greenstone M, Shapiro JS. Adapting to climate change: The remarkable decline in the US temperature-mortality relationship over the twentieth century. J Polit Economy. 2016;124:105–159. [Google Scholar]
- 45.Hsiang S. Climate econometrics. Annu Rev Resource Econ. 2016;8:43–75. [Google Scholar]
- 46.Smith SJ, Edmonds J, Hartin CA, Mundra A, Calvin K. Near-term acceleration in the rate of temperature change. Nat Clim Change. 2015;5:333–336. [Google Scholar]
- 47.Burke M, Emerick K. Adaptation to climate change: Evidence from US agriculture. Am Econ J Econ Policy. 2016;8:106–140. [Google Scholar]
- 48.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. MIT Press; Cambridge, MA: 2010. [Google Scholar]
- 49.Lambrew JM, Shalala DE. Federal health policy response to Hurricane Katrina: What it was and what it could have been. JAMA. 2006;296:1394–1397. doi: 10.1001/jama.296.11.1394. [DOI] [PubMed] [Google Scholar]
- 50.Obradovich N, Fowler JH. Climate change may alter human physical activity patterns. Nat Hum Behav. 2017;1:0097. [Google Scholar]
- 51.Bhugra D, et al. The WPA-Lancet psychiatry commission on the future of psychiatry. Lancet Psychiatry. 2017;4:775–818. doi: 10.1016/S2215-0366(17)30333-4. [DOI] [PubMed] [Google Scholar]
- 52.Searle K, Gow K. Do concerns about climate change lead to distress? Int J Clim Change Strateg Management. 2010;2:362–379. [Google Scholar]
- 53.Clayton S, Manning C, Krygsman K, Speiser M. Mental Health and Our Changing Climate: Impacts, Implications, and Guidance. American Psychological Association and ecoAmerica; Washington, DC: 2017. [Google Scholar]
- 54.Kaniasty K. Predicting social psychological well-being following trauma: The role of postdisaster social support. Psychol Trauma Theor Res Pract Policy. 2012;4:22–33. [Google Scholar]
- 55.Reser JP, Swim JK. Adapting to and coping with the threat and impacts of climate change. Am Psychol. 2011;66:277. doi: 10.1037/a0023412. [DOI] [PubMed] [Google Scholar]
- 56.Kizilbash AH, Vanderploeg RD, Curtiss G. The effects of depression and anxiety on memory performance. Arch Clin Neuropsychol. 2002;17:57–67. [PubMed] [Google Scholar]
- 57.Di Luzio M, Johnson GL, Daly C, Eischeid JK, Arnold JG. Constructing retrospective gridded daily precipitation and temperature datasets for the conterminous United States. J Appl Meteorol Climatology. 2008;47:475–497. [Google Scholar]
- 58.Kanamitsu M, et al. NCEP–DOE AMIP-II reanalysis (R-2) Bull Am Meteorol Soc. 2002;83:1631–1644. [Google Scholar]
- 59.Thrasher B, Maurer EP, McKellar C, Duffy P. Technical note: Bias correcting climate model simulated daily temperature extremes with quantile mapping. Hydrol Earth Syst Sci. 2012;16:3309–3314. [Google Scholar]
- 60.Taylor KE, Stouffer RJ, Meehl GA. An overview of CMIP5 and the experiment design. Bull Am Meteorol Soc. 2012;93:485–498. [Google Scholar]
- 61.Riahi K, et al. RCP 8.5—a scenario of comparatively high greenhouse gas emissions. Clim Change. 2011;109:33–57. [Google Scholar]
- 62.Carleton TA, Hsiang SM. Social and economic impacts of climate. Science. 2016;353:aad9837. doi: 10.1126/science.aad9837. [DOI] [PubMed] [Google Scholar]
- 63.Deschênes O, Greenstone M. Climate change, mortality, and adaptation: Evidence from annual fluctuations in weather in the US. Am Econ J Appl Econ. 2011;3:152–185. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.