Abstract
Background:
Perceived stress and psychological distress are associated with more cigarette craving and withdrawal, higher nicotine dependence, and less success during quit attempts. Low income smokers have disproportionately higher rates of smoking and may be particularly vulnerable to the effects of stress on smoking dependence. The aim of the current study was to assess if lower income smokers have a stronger association between stress and nicotine dependence than higher income smokers.
Methods:
Data were obtained from the Pennsylvania Adult Smoking Study, which included 351 daily smokers. Subjects completed PhenX Toolkit and other self-report measures of socioeconomic factors, the 10-item Perceived Stress Scale, Kessler Psychological Distress Scale (K6), Fagerstrom Test for Nicotine Dependence (FTND), and the Hooked on Nicotine Checklist (HONC). Moderation analyses using linear regression examined income-related differences in the association between stress and nicotine dependence.
Results:
Income groups were categorized by an annual household income of $50,000 based on visual-inspection of scatter plots of income by nicotine dependence. Compared to higher income smokers, lower income smokers had significantly higher mean levels of nicotine dependence on the FTND [3.74 vs. 4.79, p<.001], perceived stress [15.63 vs. 17.95, p=.004], and psychological distress [5.30 vs. 6.86, p=.001], respectively. There were interaction effects, such that lower income smokers had a strong, positive associations between FTND and perceived stress (B=−0.11, CI= −0.17 – −0.04, p=.002) and psychological distress (B=−0.13, CI= −0.25 – −0.02, p=.022) whereas no association was found in higher income smokers. No significant moderation effects were found for the HONC or when income groups were categorized by U.S. federal poverty level.
Conclusions:
The results highlight that the relationship between increasing stress and FTND was found in lower but not higher income groups. Future research should examine socioeconomic environmental and psychosocial factors that may facilitate increased smoking during stress-induced craving.
Keywords: Dependence, Distress, Income, Nicotine, Socioeconomic, Stress
1. Introduction
Stress and smoking share a cyclical relationship. Stress triggers cigarette craving for smokers, which creates the illusion that smoking in turn relieves stress (1-3). This has been shown in laboratory tasks where acute stress induces cigarette craving and negative affect (2). Heavy smokers show stronger physiological reactivity to stress compared to light smokers and non-smokers (2). Self-reported chronic stress has been linked to more impulsive decision making that could contribute to less control over smoking behavior (2). Smokers often report that cessation is difficult because they lose their primary source of stress relief (3, 4).
Perceived stress, the subjective appraisal of a life event, is determined by the perceived severity of the event and the resources available for coping with the event (5). There are few studies on the relationship between perceived stress and tobacco use and dependence. Perceived stress has been found to be a risk factor for tobacco use among adolescents (1). Heavy adult smokers (>16 cigarettes per day) report higher levels of perceived stress than light smokers (2). Perceived stress has also been linked to more self-reported withdrawal symptoms among smokers, especially among women (6).
Similar to perceived stress, psychological distress has been associated with higher smoking prevalence, nicotine dependence, and lower rates of cessation (7). In the U.S., the rates of smoking among individuals with high self-reported non-specific psychological distress in the last 30 days were over 30% in 2014 which were more than double the rates for individuals with no psychological distress (8, 9). Higher psychological distress is associated with greater overall nicotine dependence, including shorter time to the first cigarette of the day and stronger smoking urges (7). One study found that psychological distress was not related to interest in quitting or a history of quit attempts; however, distress has been associated with lower rates of success among those that do attempt to quit (10, 11).
The rates of smoking in the U.S. are disproportionately high among individuals of low socioeconomic status (12). In the U.S., 26% of those below the poverty level were smokers in 2015 compared to 14% of those at or above the poverty level (13). In addition to higher rates of smoking, socioeconomic disadvantage has been linked to higher levels of nicotine dependence (14), which may be one factor driving poorer smoking cessation outcomes globally (12, 15).
Individuals of low socioeconomic status (SES) report more perceived stress (16, 17) and psychological distress (18) than those of high SES. Prior research has identified stress as one pathway linking low SES with poor health outcomes like all-cause mortality (17, 19). Low SES conditions may reduce the capacity and resources to manage stress and contribute to poor health behaviors like smoking (20, 21); however, the research examining this link is limited and findings have been mixed (6, 22). One study found that among smokers, lower income was associated with higher levels of perceived stress, but less cigarettes smoked per day (6). Another study found poor neighborhood conditions to contribute to more stress and negative affect, which in turn reduced self-efficacy for controlling smoking behaviors during a quit attempt (22). Similarly, financial stress, as measured by inability to pay bills, was associated with more desire to quit smoking, but lower rates of quit attempts and less success among those who did attempt to quit (23, 24). In the International Tobacco Control survey, U.S. smokers reported the highest rates of financial stress (13%) and the lowest rates of quit attempts (33%) and successful quitting (26%) compared to smokers in the UK, Australia, and Canada (23). This study also found the highest levels of nicotine dependence among low income smokers (23).
It is unclear if SES affects the relationship between psychological stress and nicotine dependence. The relationship between stress and nicotine dependence can be difficult to interpret using measures such as the Fagerström Test for Nicotine Dependence (FTND) since lower SES may be related to higher dependence, but less average cigarettes per day due to financial limitations (25). Therefore, the aim of the current study was to determine if the association between stress and smoking dependence differed for smokers with varying income levels. This model takes into account detailed income data that may influence dependence outcomes more than education level, another commonly used indicator of SES. Further, we examined the independent and interactive effects of income and stress on nicotine dependence severity among adult smokers using two measures of dependence. These measures included behavioral as well as cognitive dependence factors to examine for differences in the effect of income and stress on varying aspects of nicotine dependence, not just cigarettes per day. We expected perceived stress and psychological distress to show a stronger positive association with nicotine dependence for low income smokers compared to high income smokers.
2. Methods
2.1. Participant recruitment
Data for the current study was collected between June 2012 and April 2014 for the Pennsylvania Adult Smoking Study (PASS) (26). PASS was designed to examine pathways between socioeconomic status and smoke exposure through smoking topography, biomarkers, and stress. Smokers from 14 counties throughout central Pennsylvania who were 18 years of age or older and not currently pregnant were recruited for the study. Participants were only required to smoke at least 1 cigarette per day for the past year to accommodate low income volunteers who may smoke a low number of cigarettes due to financial constraints, but continue to have high levels of dependence and smoking-related health problems (27). Prisoners and volunteers without mental capacity to provide informed consent were not eligible for the study.
Participants were recruited through radio advertisements, internet and social media, word of mouth, and flyers posted in local stores that sell tobacco products (i.e., tobacco shops, gas stations). In total, 352 participants enrolled in the study and one of these participants did not complete the protocol. All study procedures were approved by the Penn State College of Medicine Institutional Review Board (Hershey, Pennsylvania).
2.2. Procedures
Preliminary eligibility was determined via telephone interview. All eligible and interested participants completed two at-home study visits. All data for the current study was collected at the first visit. The second home visit was conducted as a follow-up visit to collect study-related materials from the participant. Participants gave written informed consent and were administered questionnaires by a trained interviewer. The questionnaires included questions on sociodemographic factors, medical history, tobacco use and exposure, nicotine dependence, and stress. The questionnaires included items from version 5.1 of the Consensus Measures of Phenotypes and Exposures (PhenX) Toolkit (March 23, 2012). Prior data from PASS demonstrating the effect of smoking topography on nicotine metabolites, a hypothesized link to poor smoking outcomes among low SES smokers, was reported previously and describes the procedural details of measures not used in the current analysis (26).
2.3. Measures
2.3.1. Socioeconomic status.
To determine income status, participants were asked to provide their best estimate of their total income from all family members living in their household before taxes in the prior year. For the 38 participants that chose ‘I don’t know’ to this income question, they were prompted to choose if their household income was above or below $20,000. These participants were then further prompted to choose between income options binned into $1000 increments if below $20,000 and $5000 increments if above $20,000. The highest value of each chosen bin was used in all analyses as the reported total household annual income.
2.3.2. Nicotine dependence.
The Fagerström Test for Nicotine Dependence (FTND) is a 6-item measure focused on behavioral indices of nicotine dependence (e.g., “How many cigarettes a day do you smoke?”). Scores ranged from low (0) to high (10) dependence severity (25). Internal consistency of the FTND scale for the current study was low (Cronbach’s α = 0.63), which was expected based on prior research with the FTND and likely due to the small number of items (25). The Hooked on Nicotine Checklist (HONC) is a 10-item measure with scores ranging from low (0) to high (10) dependence severity (28). Whereas FTND is a good measure of nicotine intake, HONC measures a different dimension of nicotine dependence; loss of autonomy. The items inquire about past recall of withdrawal symptoms (e.g., “Did you feel more irritable because you couldn’t smoke?”) and difficulty with prior quit attempts (e.g., “Have you ever tried to quit, but couldn’t?”). The HONC had good internal consistency among the current sample (Cronbach’s α=0.73).
2.3.4. Perceived stress.
The Perceived Stress Scale (PSS) is a 10-item questionnaire widely used to measure the appraised stress attributed to various life situations in the past month (5). Responses are measured on a Likert scale ranging from “Never” to “Very Often” and are summed to calculate a total score ranging from 0 to 40. Internal consistency of the PSS for the current sample was good (Cronbach’s α = 0.91).
2.3.5. Psychological distress.
The Kessler Psychological Distress Scale (K6) is a 6-item measure of anxiety and depressive symptoms in the past 30 days (29). It is highly correlated with mental disorders diagnosed using the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (30). Response options range from “None of the time” to “All of the time” and are summed to create a total score ranging from 0 to 24. Internal consistency of the K6 scale for the current study was good (Cronbach’s α = 0.86).
2.4. Analyses
2.4.1. Data cleaning.
Of the 351 participants who completed the protocol, 18 were excluded for missing data on income, nicotine dependence, or stress. The final sample for analysis was 333.
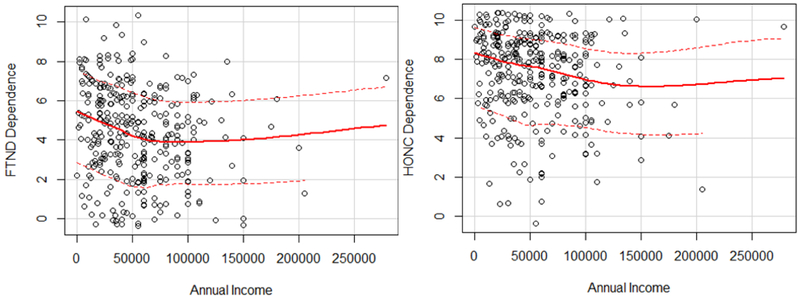
We aimed to create income groups that were meaningful in relation to dependence outcomes. To do this, we visually inspected scatter plots of income by dependence scores (Figure 1). This method has been done in prior research to interpret non-linear associations between health outcomes and income (31). For the FTND score in particular, income values around $50,000 appeared to be associated with a meaningful difference in dependence. Lower income participants were categorized as those with a household annual income ≤ $50,000 and higher income participants with > $50,000. Income was used as a continuous variable for correlations and t-tests.
Figure 1.
Scatter plots of annual household income by FTND and HONC dependence. Each scatter plot includes a non-parametric regression line with loess smoothing (solid line) and lines of positive and negative squared residuals of the mean fit values (dashed lines). Points were jittered by a factor of 2.
Continuous income values were positively skewed and square root transformations were used to improve the distribution normality for the correlation analyses with income. All analyses were conducted using RStudio version 1.0.153.
2.4.2. Descriptive statistics.
Descriptive statistics were calculated for the total sample and by income group. T-tests and chi-square analyses were used to compare demographic, nicotine dependence, and stress variables across income categories. Pearson’s correlations were used to examine the association between income as a continuous variable, measures of dependence, and self-reported perceived stress and psychological distress.
2.4.3. Moderation.
Moderation analyses were conducted with linear models in the Mod function to examine the interaction effect of income group (lower and higher) with continuous total scores on the PSS and K6 scales. Dependence scores from the FTND and HONC were regressed onto income, stress, and their interaction term in separate models. Plots of the interaction simple slopes for the association of PSS and K6 with FTND scores are displayed by income group. Income category in the linear regression equations was dummy coded such that 0 indicates ≤ $50,000 and 1 indicates > $50,000.
2.4.4. Post-hoc analyses.
After completing the main analyses, two relevant questions remained. First, were there significant interaction effects on some dependence behaviors, but not others? Second, would there be similar results if the income categories were created using the U.S. federal household poverty line? The individual FTND item scores were regressed onto income, stress, and their interaction in moderation analyses. A second set of moderation analyses were conducted to examine if the same interaction effects were found for income groups split at the federal income poverty level determined by participants’ self-reported household income and the number of people living in the home (32).
3. Results
3.1. Participant characteristics
Participant characteristics are displayed by lower and higher income groups in Table 1. The overall sample (n=333) was 57% female and 86% white with an average age of 38.01 years (SD=11.53). Ages ranged from 18 to 66 years. Participants began smoking at an average age of 16.87 years (SD=4.63) and reported smoking a mean of 16.45 cigarettes per day (SD=8.03). Over three quarters of the sample reported at least one quit attempt in their lifetime (77%). The sample had a median income of $45,000 (Interquartile range=$51,000). There were no differences by income group ($50,000 cutoff) in age, gender, or race. Low income participants had significantly less education, and lower rates of home ownership, bank savings account, and health insurance. There were no significant differences in age of smoking initiation, cigarettes per day, or past history of quit attempts. Low income smokers had significantly higher scores on both measures of dependence, which was expected given that this association was used to define a cut-point for the income groups. Low income smokers had significantly higher self-reported stress and distress.
Table 1.
Participant demographics and smoking characteristics by income group
| Total sample (n=333) |
Low income (n=184) |
High income (n=149) |
Effect Size | p-value | |
|---|---|---|---|---|---|
| Demooraphics | |||||
| Age, M(SD) | 38.01 (11.53) | 37.78 (11.43) |
38.28 (11.68) | d=0.04 | .696 |
| Female, N(%) | 189 (57) | 110 (60) | 79 (53) | V=0.06 | .260 |
| Caucasian, N(%) | 288 (86) | 154 (84) | 134 (90) | V=0.08 | .135 |
| Socioeconomic | |||||
| Income, M(SD) | $53,698.97 (38,500.84) |
$27,042.20 (14,114.35) |
$86,617.40 (33,233.92) |
NA | NA |
| Income, Range | $0-$279,000 | $0- $50,000 |
$52,000 - $279,000 | NA | NA |
| Years education, M(SD) | 15.34 (2.06) | 14.96 (2.07) |
15.80 (1.96) | d=0.42 | <.001 |
| Home ownershipa, N(%) | 131 (39) | 51 (28) | 80 (54) | V=0.26 | <.001 |
| Savings account, N(%) |
191 (57) | 74 (45) | 117 (79) | V=0.38 | <.001 |
| Health Insurance, N(%) |
245 (74) | 119 (65) | 126 (85) | V=0.22 | <.001 |
| Smoking | |||||
| Cigarettes per day, M(SD) | 16.45 (8.03) | 17.15 (8.36) |
15.59 (7.53) | d=0.20 | .076 |
| Age of initiation, M(SD) | 16.87 (4.63) | 16.46 (4.12) |
17.38 (5.16) | d=0.20 | .078 |
| Quit attempt, N(%) | 255 (77) | 143 (78) | 112 (75) | V=0.02 | .677 |
| FTND, M(SD) | 4.32 (2.29) | 4.79 (2.35) | 3.74 (2.09) | d=0.47 | <.001 |
| HONC, M(SD) | 7.28 (2.12) | 7.60 (2.02) | 6.89 (2.18) | d=0.34 | .002 |
| Stress | |||||
| Perceived Stress, M(SD) | 16.91 (7.40) | 17.95 (7.46) |
15.63 (7.13) | d=0.32 | .004 |
| Distress, M(SD) | 6.16 (4.47) | 6.86 (4.84) | 5.30 (3.82) | d=0.36 | .001 |
Note:
High income n=148; FTND = Fagerström Test for Nicotine Dependence; HONC = Hooked on Nicotine Checklist; d= Cohen’s d; V= Cramer’s V; p-values refer to significance of t-tests and χ2 analyses.
3.2. Associations between income, stress, and nicotine dependence
Correlations among all primary study variables were conducted with the total sample. There were significant negative correlations between self-reported annual household income and dependence on the FTND (r= −.16, p= .003) and the HONC (r= − .17, p= .002). There were significant negative correlations between self-reported annual household income and perceived stress (r=− .14, p= .013) and psychological distress (r= −.17, p= .002). There were significant positive correlations between perceived stress and dependence on the FTND (r= .22, p< .001) and the HONC (r= .41, p< .001). There were significant positive correlations between psychological distress and dependence on the FTND (r= .19, p< .001) and the HONC (r= .35, p< .001).
3.3. Moderation analyses
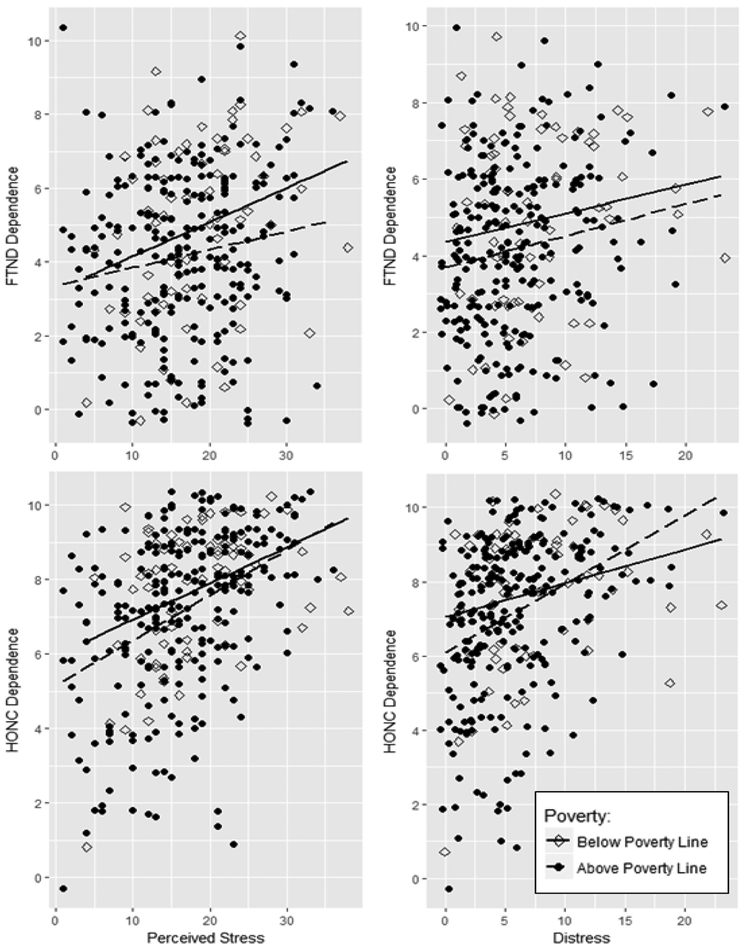
There was a significant interaction effect between perceived stress and income on FTND scores, such that lower income was associated with a stronger positive relationship between perceived stress and FTND dependence than higher income (B= − 0.11, CI= −0.17 – −0.04, p= .002) (Table 2). The same significant interaction effect was found between psychological distress and income on FTND scores, such that lower income was associated with a stronger positive relationship between psychological distress and FTND dependence than those with higher income (B= −0.13, CI= −0.– −.02, p= .022). There were no significant interaction effects between perceived stress or psychological distress and income on HONC dependence scores. The interaction simple slopes of perceived stress and psychological distress with FTND and HONC scores for each group are displayed in Figure 2.
Table 2.
Nicotine dependence measures regressed onto the interaction of income group and perceived stress and distress
| Unstandardized estimate (B) |
95% Confidence Interval |
p-value | R2(Adj.R2) | Low Income Slope |
High Income Slope |
|
|---|---|---|---|---|---|---|
| FTND | ||||||
| Stress x income |
−0.11 | −0.17 – −0.04 | .002 | 0.11 (0.10), p<001 |
0.10, p<.001 |
−0.01, p=0.88 |
| Distress x income |
−0.13 | −0.25 – −0.02 | .022 | 0.08 (0.08), p<.001 |
0.12, p<.001 |
−0.01, p=0.800 |
| HONC | ||||||
| Stress x ?income |
0.01 | −0.05 –0.06 | .851 | 0.18 (0.17), p<.001 |
0.11, p<.001 |
0.12, p<.001 |
| Distress x income |
0.03 | −0.08 –0.13 | .607 | 0.13 (0.12), p<.001 |
0.14, p<.001 |
0.17, p<.001 |
Note: FTND= Fagerström Test for Nicotine Dependence; HONC = Hooked on Nicotine Checklist
Figure 2.
Plots of the simple slopes of the associations between perceived stress or distress and dependence measured by the FTND or HONC. Lower income group (≤$50,000) slopes are displayed with a solid line and higher income group (>$50,000) slopes with a dashed line. Points were jittered by a factor of two.
3.4. Post-hoc analyses
3.4.1. Moderation analyses of individual FTND items.
In post-hoc analyses, we examined interaction effects on each item of the FTND to identify which smoking behaviors were most susceptible to stress by income interaction effects. There were significant interaction effects of income and perceived stress (B= −0.02, 95% CI= −0.03 – −0.01, p= .003) as well as psychological distress (B= −0.03, 95% CI= −0.06 – −0.01, p= .006) on smoking more after waking; perceived stress (−0.28, 95% CI= −0.51 – −0.04, p= .023) on average cigarettes per day; and perceived stress on difficulty refraining from smoking in restricted areas (B= −0.01, 95% CI= −0.02 – −0.01, p= .038). For each significant interaction lower income smokers had a stronger positive association between stress and levels of smoking behavior indicative of more dependence. There were no interaction effects on smoking during illness, hating to give up the first cigarette of the day, and the time to smoking the first cigarette of the day.
3.4.2. Moderation analyses wth poverty level.
We aimed to determine if study effects would remain the same if the federal household poverty level was used as an income cut-point rather than the data-derived value of $50,000. The sample was grouped by poverty level based on their self-reported annual household income as described above, and the self-reported number of persons living in the household. Participants were categorized as living in poverty with an annual household income < $12,060 for a household size of 1, < $16,240 for a household size of 2, < $20,420 for a household size of 3, < $24,600 for a household size of 4, < $28,780 for a household size of 5, < $32,960 for a household size of 6, < $37,140 for a household size of 7, and < $41,320 for a household size of 8. Poverty category in the linear regression equations was dummy coded such that 0 indicates below the poverty level and 1 indicates above the poverty level. Among the total sample, 69 participants reported a household income below the federal poverty level and 264 participants were above the federal poverty level. Participants below the poverty level, compared to those above the poverty level, had higher mean nicotine dependence scores on the FTND (4.91 vs. 4.17, 95% CIdiff= 0.11 – 1.38, p=.022) and HONC (7.72 vs. 7.17, 95% CIdiff= 0.04 – 1.07, p=.034) and higher mean levels of psychological distress (7.48 vs. 5.81,95% CIdiff= 0.36 – 2.97, p=.013), respectively. There were no significant differences in mean perceived stress between the poverty groups (18.23 vs. 16.57, 95% CIdiff= −0.31 – 3.63, p=.097), respectively. We then regressed nicotine dependence scores onto the interaction of perceived stress and psychological distress and federal poverty groups. No interactions were significant. (Table 3, Figure 3)
Table 3.
Nicotine dependence measures regressed onto the interaction of poverty group and perceived stress and distress
| Unstandardized estimate (B) |
95% Confidence Interval |
p-value | R2(Adj.R2) | Below Poverty Slope |
Above Poverty Slope |
|
|---|---|---|---|---|---|---|
| FTND | ||||||
| Stress × poverty | −0.04 | −0.13–0.04 | .291 | 0.06 (0.05),p<001 | 0.08, p=.002 |
0.04, p=0.089 |
| Distress × poverty | 0.01 | −0.12 – 0.13 | .905 | 0.04 (0.03), p=.003 | 0.08, p=.030 |
0.08, p=0.040 |
| HONC | ||||||
| Stress × poverty | 0.02 | −0.05 – 0.09 | .500 | 0.18 (0.17), p<001 |
0.11, p<.001 | 0.13, p<.001 |
| Distress × poverty | 0.09 | −0.02 – 0.20 | .097 | 0.13 (0.12), p<.001 | 0.13, p<.001 | 0.20, p<.001 |
Note: FTND= Fagerström Test for Nicotine Dependence; HONC = Hooked on Nicotine Checklist
Figure 3.
Plots of the simple slopes of the associations between perceived stress or distress and dependence measured by the FTND or HONC. Slopes for participants below the poverty level are displayed with a solid line and those above the poverty level with a dashed line. Points were jittered by a factor of two.
4. Discussion
The current study found nicotine dependence, stress, and the association between nicotine dependence and stress to differ by income categories above and below $50,000. Our results support prior research showing links between income and smoking prevalence and dependence (13, 14). By using detailed income data and inspecting for non-linear associations, we identified $50,000 as a meaningful annual household income that may serve as a more sensitive cut-off for identifying smoking-related group differences than the commonly used federal poverty level.
Previous models propose that low SES individuals experience more stress, which contributes to higher smoking rates and poor cessation outcomes (22), however the reasons for this link are still unclear. In our sample, low income participants did report higher mean levels of perceived stress and psychological distress than high income participants. However, many of the higher income participants also reported high levels of stress. Yet, for this group, more stress was not associated with higher levels of nicotine dependence on a behavioral dependence measure. In fact, dependence rates slightly decreased at higher levels of stress and distress for higher income participants. Alternatively, the same high levels of stress were associated with more behavioral dependence for the low income smokers. Thus, lower income may not just be associated with more stress, but also less resilience to stress. Resilience to stress, rather than the amount of stress, may be more predictive of smoking outcomes for low income smokers and should be examined in future research.
We did not find significant moderation effects of income on the relationship between stress and dependence measured with the HONC. HONC dependence scores increased with higher perceived stress and psychological distress for all smokers in our study, regardless of income. The HONC measures dependence by asking smokers to recall craving and withdrawal symptoms (28). Thus, higher income smokers appeared to be buffered against an increase in dependence-related smoking behaviors, but not against their recall of cigarette craving or withdrawal symptoms like concentration difficulty and irritability. While both income groups showed positive associations between stress and smoking urges on the HONC, more stress was associated with more smoking on the FTND for the low income group only.
This suggests that there is something unique about the behavioral smoking responses to stress for low income smokers compared to high income smokers, regardless of craving. Our findings lend support for prior research that did not find craving to mediate the association between stress and smoking cessation (22). Instead, self-efficacy to abstain from smoking during the quit attempt was a significant mediator (22). Similarly, the current study found that low income smokers showed strong positive links between stress and self-reported ability to refrain from smoking in restricted areas, which was not found for high income smokers.
It is possible that resilience factors buffer higher income smokers from the effects of perceived stress and distress on their smoking behavior. There are many potential individual, environmental, and structural factors that could contribute to the risk and resilience of smoking behavior to stress (19, 33). Low income neighborhoods often have fewer home and workplace smoking restrictions, more cigarette advertisements to serve as smoking cues, and easier access to cigarette vendors (34-36). For these reasons, low income smokers may be presented with more smoking cues and find it easier to cope with stressors by smoking rather than by other less accessible means, like exercise, social support, relaxation, or purchasing goods or services to alleviate the stressor.
Siahpush and colleagues found a relationship between income and smoking dependence using the Heaviness of Smoking Index as the measure of dependence (HSI) (37). The HSI uses two items from the FTND, the number of cigarettes per day and the time to first cigarette. We found a significant stress by income moderation effect on the number of cigarettes per day, but not the time to first cigarette. This was surprising given that the time to first cigarette has been recognized as one of the strongest predictors of nicotine dependence, quitting success, and even genetic heritability for smoking (38-40). Given the link between stress and dependence, it is possible that low income participants smoked more to cope with stressors throughout the day, not because of a physiological urgency first thing in the morning. This may suggest stronger psychological dependence on the negatively reinforcing effects of nicotine, rather than stronger physiological dependence marked by early morning withdrawal symptoms. It should be noted that because of financial constraints, lower income smokers might be expected to smoke fewer CPD. Therefore the current finding that low income participants smoked more CPD may even underestimate the extent to which smoking-related coping occurs.
In line with this hypothesis, laboratory studies have shown that acute stress reduces smokers’ ability to resist smoking and increases the rewarding effects of smoking (41). The influence of stress on smoking may be stronger for low income smokers, however this has not yet been examined. Future research measuring craving, withdrawal, and smoking motivations in the laboratory during acute stress or throughout the day (e.g., ecological momentary assessment) could shed light on the complex association between stress and smoking behavior for smokers of low SES. Research in this area could inform cessation techniques that provide education and practice focused on identifying, mitigating, and coping with stressors.
4.1. Limitations
The current study was preliminary in that it aimed to establish the link between stress and dependence across income. For this reason, broad definitions of stress and distress were used. These, however, provided limited specificity to our understanding of the etiologies and types of stressors most closely linked to smoking behaviors. Prior research has shown that interpersonal relationship, financial, and neighborhood stressors account for more variance in current smoking status than other types of stressors among African Americans (42), and these may also be important predictors for nicotine dependence. The current study was conducted with smokers in central Pennsylvania who were primarily Caucasian. Therefore the results may not generalize to smokers in other countries or low income racial and ethnic minorities in the U.S. who may experience co-occurring class and minority stressors. Future research could work towards narrowing our definitions of stress and dependence to identify points for intervention and specifying intervention strategies for specific populations.
This was a cross-sectional study that could not infer causation. Although we are hypothesizing that lower income creates a vulnerability to stress-related increases in nicotine dependence and smoking behavior, it is possible that psychological distress may create a vulnerability to both lower income and higher nicotine dependence. There is some evidence that treating psychological distress can improve economic outcomes, while there is less evidence that intervening on economic factors improves psychological outcomes (43). Thus, prospective research may be better able to determine if causal directions do exist and what level of intervention would produce the most benefit.
The link between stress and smoking behavior can also be investigated in a laboratory setting to observe affect and stress-induced cigarette craving and seeking behaviors. Experimental studies designed to mimic real-world experiences can provide more control over conditions and avoid issues of recall bias from self-reported smoking behavior while not incurring the time and monetary costs of longitudinal observational research. No studies have examined how the stress to smoking link differs for smokers of low and high SES. This could help determine if low SES smokers have less reserve, or capacity to manage stress through means other than smoking, or if environmental factors, like cigarette access or lack of regulations is a more likely cause of the stress-related increases in dependence observed for low SES smokers in the current study.
4.2. Conclusion
The current study highlights the role of income in understanding how stress relates to smoking behavior. Future research could benefit from examining further which stressors are most influential and the mechanisms through which stress has its effect on smoking behavior. Smoking cessation treatments for low income populations may be improved by placing a stronger emphasis on stress management.
Highlights.
Lower income, especially below $50,000, was related to higher nicotine dependence.
Lower income was associated with more perceived stress and psychological distress.
More perceived stress and distress was associated with higher nicotine dependence.
More stress was linked to higher nicotine dependence for low income smokers.
Stress and nicotine dependence were not associated for high income smokers.
Acknowledgements:
We would like to thank A. Stennett, J. Gramley, and J. Derk for their help with data collection. This work was presented at the 24th Annual Meeting of the Society for Research on Nicotine and Tobacco, Baltimore, Maryland, February, 21–24, 2018.
Role of Funding Sources:
This research was supported by the National Institute on Drug Abuse grant R01DA026815 and in part by the National Center for Advancing Translational Sciences grants UL1TR000127, UL1TR002014, and KL2TR002015. The funding sources were not involved in the design or conduct of the study; the data collection, management, analysis, or interpretation; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication. The contents of this paper are the sole responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the National Center for Advancing Translational Sciences.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest:
None declared.
References
- 1.Leventhal AM, Urman R, Barrington-Trimis JL, Goldenson NI, Gallegos K, Chou CP, et al. Perceived stress and poly-tobacco product use across adolescence: Patterns of association and gender differences. Journal of psychiatric research. 2017;94:172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carim-Todd L, Mitchell SH, Oken BS. Impulsivity and Stress Response in Nondependent Smokers (Tobacco Chippers) in Comparison to Heavy Smokers and Nonsmokers. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2016;18(5):547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4:e006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robles Z, Garey L, Hogan J, Bakhshaie J, Schmidt NB, Zvolensky MJ. Examining an underlying mechanism between perceived stress and smoking cessation-related outcomes. Addictive behaviors. 2016;58:149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 6.Lawless MH, Harrison KA, Grandits GA, Eberly LE, Allen SS. Perceived stress and smoking-related behaviors and symptomatology in male and female smokers. Addictive behaviors. 2015;51:80–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hagman BT, Delnevo CD, Hrywna M, Williams JM. Tobacco use among those with serious psychological distress: results from the national survey of drug use and health, 2002. Addictive behaviors. 2008;33(4):582–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrence D, Williams JM. Trends in Smoking Rates by Level of Psychological Distress-Time Series Analysis of US National Health Interview Survey Data 1997–2014. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2016;18(6):1463–70. [DOI] [PubMed] [Google Scholar]
- 9.Zvolensky MJ, Jardin C, Wall MM, Gbedemah M, Hasin D, Shankman SA, et al. Psychological distress among smokers in the United States: 2008 to 2014. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lawrence D, Mitrou F, Zubrick SR. Non-specific psychological distress, smoking status and smoking cessation: United States National Health Interview Survey 2005. BMC Public Health. 2011;11:256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cosci F, Corlando A, Fornai E, Pistelli F, Paoletti P, Carrozzi L. Nicotine dependence, psychological distress and personality traits as possible predictors of smoking cessation. Results of a double-blind study with nicotine patch. Addictive behaviors. 2009;34(1):28–35. [DOI] [PubMed] [Google Scholar]
- 12.Hiscock R, Judge K, Bauld L. Social inequalities in quitting smoking: what factors mediate the relationship between socioeconomic position and smoking cessation? Journal of public health. 2011. ;33(1):39–47. [DOI] [PubMed] [Google Scholar]
- 13.Jamal A, King BA, Neff LJ, Whitmill J, Babb SD, Graffunder CM. Current cigarette smoking among adults - United States, 2005–2015. Centers for Disease Control and Prevention, 2016. [DOI] [PubMed] [Google Scholar]
- 14.Siahpush M, McNeill A, Borland R, Fong GT. Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco control. 2006;15 Suppl 3:iii71–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Federico B, Costa G, Kunst AE. Educational inequalities in initiation, cessation, and prevalence of smoking among 3 Italian birth cohorts. American journal of public health. 2007;97(5):838–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen S, Janicki-Deverts D. Who's Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091. Journal of Applied Social Psychology. 2012;42(6):1320–34. [Google Scholar]
- 17.Redmond N, Richman J, Gamboa CM, Albert MA, Sims M, Durant RW, et al. Perceived stress is associated with incident coronary heart disease and all-cause mortality in low- but not high-income participants in the Reasons for Geographic And Racial Differences in Stroke study. Journal of the American Heart Association. 2013;2(6):e000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sareen J, Afifi TO, McMillan KA, Asmundson GJG. Relationship between household income and mental disorders. Arch Gen Psychiatry. 2011;68(4):419–27. [DOI] [PubMed] [Google Scholar]
- 19.Baum A, Garofalo JP, Yali AM. Socioeconomic status and chronic stress: Does stress account for SES effects on health?. Annals of the New York Academy of Sciences. 1999;896:131–44. [DOI] [PubMed] [Google Scholar]
- 20.Harwood GA, Salsberry P, Ferketich AK, Wewers ME. Cigarette smoking, socioeconomic status, and psychosocial factors: Examining a conceptual framework. Public Health Nursing. 2007;24(4):361–71. [DOI] [PubMed] [Google Scholar]
- 21.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129(1):10–51. [DOI] [PubMed] [Google Scholar]
- 22.Businelle MS, Kendzor DE, Reitzel LR, Costello TJ, Cofta-Woerpel L, Li Y, et al. Mechanisms linking socioeconomic status to smoking cessation: a structural equation modeling approach. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2010;29(3):262–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siahpush M, Yong HH, Borland R, Reid JL, Hammond D. Smokers with financial stress are more likely to want to quit but less likely to try or succeed: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction. 2009;104(8):1382–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kendzor DE, Businelle MS, Costello TJ, Castro Y, Reitzel LR, Cofta-Woerpel LM, et al. Financial strain and smoking cessation among racially/ethnically diverse smokers. American journal of public health. 2010;100(4):702–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–27. [DOI] [PubMed] [Google Scholar]
- 26.Krebs NM, Chen A, Zhu J, Sun D, Liao J, Stennett AL, et al. Comparison of Puff Volume With Cigarettes per Day in Predicting Nicotine Uptake Among Daily Smokers. American journal of epidemiology. 2016;184(1):48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248:107–23. [DOI] [PubMed] [Google Scholar]
- 28.Wellman RJ, DiFranza JR, Savageau JA, Godiwala S, Friedman K, Hazelton J. Measuring adults' loss of autonomy over nicotine use: the Hooked on Nicotine Checklist. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2005;7(1):157–61. [DOI] [PubMed] [Google Scholar]
- 29.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–76. [DOI] [PubMed] [Google Scholar]
- 30.Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. International journal of methods in psychiatric research. 2010;19 Suppl 1:4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rehkopf DH, Berkman LF, Coull B, Krieger N. The non-linear risk of mortality by income level in a healthy population: US National Health and Nutrition Examination Survey mortality follow-up cohort, 1988–2001. BMC Public Health. 2008;8:383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Department of Health and Human Services. Annual update of the HHS Poverty Guidelines. Department of Health and Human Services, 2017. [Google Scholar]
- 33.Unger JB, Cruz T, Shakib S, Mock J, Shields A, Baezconde-Garbanati L, et al. Exploring the cultural context of tobacco use: a transdisciplinary framework. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2003;5 Suppl 1:S101–17. [DOI] [PubMed] [Google Scholar]
- 34.Barbeau EM, Wolin KY, Naumova EN, Balbach E. Tobacco advertising in communities: associations with race and class. Preventive medicine. 2005;40(1):16–22. [DOI] [PubMed] [Google Scholar]
- 35.Shavers VL, Fagan P, Jouridine Alexander LA, Clayton R, Doucet J, Baezconde-Garbanati L. Workplace and home smoking restrictions and racial/ethnic variation in the prevalence and intensity of current cigarette smoking among women by poverty status, TUS-CPS 1998–1999 and 2001–2002. Journal of Epidemiology & Community Health. 2006;60 (Supplement 2):ii34–ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laws MB, Whitman J, Bowser DM, Krech L. Tobacco availabiity and point of sale marketing in demographically contrasting districts of Massachusetts. Tobacco control. 2002;11 (Suppl II):ii71–ii3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction. 1989;84:791–800. [DOI] [PubMed] [Google Scholar]
- 38.Baker TB, Piper ME, McCarthy DE, Bolt DM, Smith SS, Kim SY, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2007;9 Suppl 4:S555–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fagerström K Time to first cigarette; the best single indicator of tobacco dependence?. Monaldi Archives for Chest Disease. 2003;59(1):91–4. [PubMed] [Google Scholar]
- 40.Haberstick BC, Timberlake D, Ehringer MA, Lessem JM, Hopfer CJ, Smolen A, et al. Genes, time to first cigarette and nicotine dependence in a general population sample of young adults. Addiction. 2007;102(4):655–65. [DOI] [PubMed] [Google Scholar]
- 41.McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison EL, Lavery M, et al. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. Journal of psychopharmacology. 2011;25(4):490–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Slopen N, Dutra LM, Williams DR, Mujahid MS, Lewis TT, Bennett GG, et al. Psychosocial stressors and cigarette smoking among African American adults in midlife. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2012;14(10):1161–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. The Lancet. 2011;378(9801):1502–14. [DOI] [PubMed] [Google Scholar]