Abstract
The prognostic relevance of masked uncontrolled hypertension (MUCH) is incompletely clear and its global impact on cardiovascular outcomes and mortality has not been assessed. The aim of this study was to perform a meta-analysis on the prognostic value of MUCH. We searched for articles assessing outcome in patients with MUCH compared to those with controlled hypertension and reporting adjusted hazard ratio and 95% confidence interval. We identified six studies using ambulatory blood pressure monitoring (12610 patients with 933 events) and five using home blood pressure measurement (17742 patients with 394 events). The global population included 30352 patients who experienced 1327 events. Selected studies had cardiovascular outcomes and all-cause mortality as primary outcome and the main result is a composite of these events. The overall adjusted hazard ratio was 1.80 (95% confidence interval 1.57–2.06) for MUCH versus controlled hypertension. Subgroup meta-analysis showed that adjusted hazard ratio was 1.83 (95% confidence interval 1.52–2.21) in studies using ambulatory blood pressure monitoring and 1.75 (95% confidence interval 1.38–2.20) in those using home blood pressure measurement. Risk was significantly higher in MUCH than in controlled hypertension independently of follow-up length and types of studied events. MUCH was at significantly higher risk than controlled hypertension in all ethnic groups, but the highest hazard ratio was found in studies including Black patients. Risk of cardiovascular events and all-cause mortality is significantly higher in patients with MUCH than in those with controlled hypertension. MUCH detected by ambulatory or home blood pressure measurement appear to convey similar prognostic information.
Keywords: ambulatory blood pressure, cardiovascular risk, controlled hypertension, home blood pressure, hypertension, masked hypertension, masked uncontrolled hypertension, mortality
INTRODUCTION
Some individuals have normal clinic blood pressure (BP) but high out-of-office BP. This phenomenon has been named white coat normotension1, isolated ambulatory or home hypertension2, reverse white-coat hypertension3 and lastly masked hypertension by Pickering et al. in 20024.
It has been detected in untreated subjects5,6 and treated or mixed populations7–28. In specifically treated patients, this phenomenon has been described more than 10 years ago7–10,15 and later renamed masked uncontrolled hypertension (MUCH)16,29–31.
Among prospective studies7–28 including patients with MUCH, some11–14,22,27 did not evaluate cardiovascular risk in untreated and treated subjects analysed separately, some8,10,15,18,20,21,24,26,28 reported significant higher risk and some7,9,16,17,23 not significant higher risk in patients with MUCH when compared to those with normal clinic and out-of-office BP (controlled hypertension, CH), and others19,25 reported different results depending on comorbidities.
Thus, the prognostic value of MUCH is not yet clear. To the best of our knowledge, previous reviews and meta-analyses5,6,32–36 concerning masked hypertension evaluated untreated, treated or mixed populations analysed together and an analysis specifically assessing the prognostic value of MUCH is still lacking.
In addition, MUCH can be detected by using either ambulatory BP monitoring 7,9–16,18,19,21,23,24,26–28 or home BP measurement8,17,20,22,25. Though MUCH detected by ambulatory BP monitoring or home BP recording are not completely the same entity14, globally these methods describe a similar phenomenon, that is normal clinic and high out-of-office BP.
The aim of this study was to perform a meta-analysis on the prognostic value of MUCH diagnosed by ambulatory BP monitoring and home BP measurement.
METHODS
The study was performed in accordance with the recommendations of the Meta-analysis of Observational Studies in Epidemiology Group.37 Original studies were approved by the institutional review committees and subjects gave informed consent. The data that support the findings of this study are available from the authors upon reasonable request.
Search Strategy
We conducted a literature search through PubMed, Web of science and Cochrane Library for articles evaluating cardiovascular outcome in patients with MUCH in comparison with those with CH up to April 20, 2018. The terms used to identify studies were “white coat normotension”, “isolated ambulatory hypertension”, “isolated home hypertension”, “reverse white-coat hypertension”, “masked hypertension”, “masked uncontrolled hypertension” and “prognosis” or “cardiovascular risk” or “cardiovascular outcome” or “cardiovascular events”. Two reviewers (A.M.P. and F.C.) independently screened titles and abstracts to identify eligible studies. Disagreement between the two reviewers was resolved by a third reviewer. Reference lists of included articles were also examined for additional studies. If necessary, supplementary data were obtained through personal contact with the investigators of the selected studies.
Eligibility criteria
Inclusion criteria for entry in the present meta-analysis were: 1) full-text paper published in a peer-reviewed journal; 2) any language of publication; 3) study on adult population; 4) use of ambulatory BP monitoring or home BP recording; 5) prospective study; 6) follow-up of at least 1 year; 7) assessment of cardiovascular outcome and mortality (any endpoint, that is, composite or separate endpoints) in MUCH compared with CH; 8) availability of adjusted hazard ratio (HR) and 95% confidence interval (CI) between MUCH and CH.
Study selection, data extraction and quality evaluation
The first literature search identified 1659 studies from various databases and 857 studies after removing duplicates. Of these, 31 were eligible after revision of titles and abstracts.5–28,32–36,38,39 Seven studies5,6,32–36 were excluded because they were previous narrative reviews and/or reviews including untreated, treated or mixed populations analysed together, 3 studies11,14,27 were excluded because untreated and treated patients were analysed together (one of them27 evaluated patients with chronic kidney disease), 2 studies38,39 were excluded because they were included in another report20 and 1 study21 was excluded because it evaluated hypertensive patients with chronic kidney disease (only a few studies specifically assessed populations with diabetes and chronic kidney disease; hence, due to the relatively small number of patients and events of these specific subpopulations, we did not include them in this meta-analysis). Thus, 18 studies7–10,12,13,15–20, 22–26,28 were included. Of these selected studies, 7 were joined in a single report9,12,13,15,18,19,23 according to the data provided by the International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes (IDACO) investigators (L.T. and J.A.S.) and 2 others10,26 were joined in a single report according to updated data (2013) provided by the authors of Chieti-Pescara Study (S.D.P., A.M.P., F.C.). Also for some other studies data were provided by the authors: D.L.C., M.L.D.B. and D.A.D.B. for the Office versus Ambulatory pressure (OvA) Study7, I.Z.B-D for the Hadassah Study16, W.V. for the Dallas Heart Study22, J.R.B. and L.M.R. for the Spanish Registry Study28. Finally, 11 studies/joined data were selected for meta-analysis, 6 for MUCH detected by ambulatory BP monitoring7,16,24,28, joined data of IDACO Study9,12,13,15,18,19,23 and joined data of Chieti-Pescara Study10,16, and 5 for MUCH detected by home8,17,20,22,25 BP measurement. Selection of publications is summarized in Figure 1.
Figure 1.
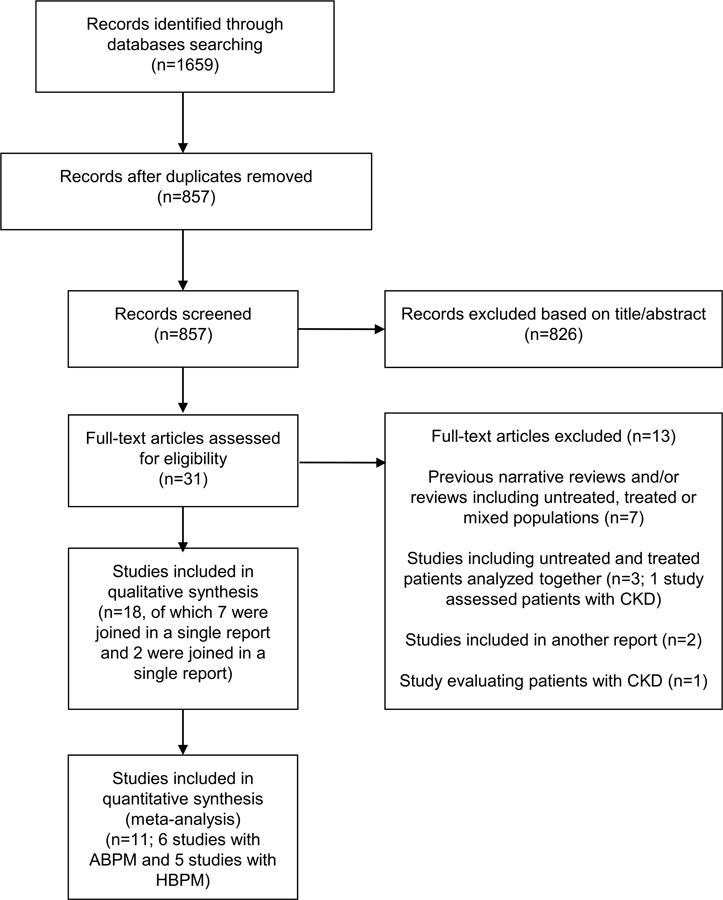
Flow chart showing selection of publications. ABPM, ambulatory blood pressure monitoring; CKD, chronic kidney disease; HBPM, home blood pressure measurement.
Two reviewers (A.M.P. and F.C.) independently extracted relevant data from selected studies. Disagreement between the two reviewers was resolved by a third reviewer.
The quality of included studies was assessed using the Newcastle-Ottawa scale.40 This scale evaluates cohort studies based on: 1) selection (representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at start of study; maximum 4 stars), 2) comparability (comparability of cohorts on the basis of the design or analysis; maximum 2 stars) and 3) outcome (assessment of outcome, follow-up length, adequacy of follow up of cohorts; maximum 3 stars). The total maximum score can be 9.
Statistical Analysis
To address confounding from other risk factors, we used the adjusted HR and 95% CI of the individual studies to calculate the overall adjusted HR and 95% CI, as also previously performed.5,33,34 We used the random effects model.41 Tests of heterogeneity were performed using the Cochrane Q statistic and I2 statistic.42 Subgroup meta-analysis, which is equivalent to meta-regression with categorical (or categorized) variables, was also performed to analyze potential sources of heterogeneity.43 Individual studies were removed one at a time to evaluate the influence of that study on the pooled estimate. A funnel plot, Begg and Mazumdar44 rank correlation test and Egger’s45 regression test for funnel plot asymmetry were used to examine the likely presence of publication bias and small-study effect. Potential adjustment for missing studies was approached by Duval and Tweedie’s trim and fill method.46 Statistical significance was defined as P < 0.05 (2-tailed tests). Analyses were done using the Comprehensive Meta-Analysis software version 2 (Biostat, Englewood, NJ).
RESULTS
Main characteristics of studies using ambulatory BP monitoring are reported in Table 1. The pooled population consisted of 12610 patients who experienced 933 events. All the studies defined MUCH as clinic BP < 140/90 mmHg and daytime BP > 135/85 mmHg. Mean follow-up ranged from 4.7 to 11 years. Four studies evaluated fatal and nonfatal cardiovascular events (stroke, coronary artery disease, heart failure and peripheral revascularization in three studies and stroke and coronary artery disease in one study) and two studies evaluated all-cause mortality.
Table 1.
Main characteristics of selected studies using ambulatory blood pressure monitoring
| Patients | MUCH Definition | FU (years) | Events | Type of Event | |||
|---|---|---|---|---|---|---|---|
| Study | CH | MUCH | CH | MUCH | |||
| OvA Study 20037 | 146 | 143 | Day BP≥135/85 mmHg | 5 | 7 | 9 | Fatal/Nonfatal CVE |
| Chieti-Pescara Study 2005–201710,26 | 523 | 215 | Day BP≥135/85 mmHg | 10 | 79 | 69 | Fatal/Nonfatal CVE |
| IDACO Study 2005–20179,12,13,15,18,19,23 | 528 | 236 | Day BP≥135/85 mmHg | 11 | 147 | 93 | Fatal/Nonfatal CVE |
| Hadassah Study 200816 | 360 | 268 | Day BP≥135/85 mmHg | 7.7 | 23 | 29 | All-Cause Mortality |
| Jackson Heart Study 201624 | 272 | 135 | Day BP≥135/85 mmHg | 8.2 | 16 | 22 | Fatal/nonfatal CVE |
| Spanish Registry Study28 | 7406 | 2378 | Day BP≥135/85 mmHg | 4.7 | 273 | 166 | All-Cause Mortality |
BP, blood pressure; CH, controlled hypertension; CVE, cardiovascular events (stroke, coronary artery disease, heart failure and peripheral revascularization for OvA, Chieti-Pescara and IDACO Studies; stroke and coronary artery disease for Jackson Heart Study); FU, follow-up (mean); IDACO, International Database on Ambulatory blood pressure in relation to Cardiovascular Outcomes; MUCH, masked uncontrolled hypertension; OvA, Office versus Ambulatory pressure. Data of the OvA, IDACO, Hadassah and Spanish Registry Studies are provided by the authors. Data of the Chieti Pescara Study, provided by the authors, come from the overall database of treated hypertensive patients at baseline (2264 patients) which includes patients aged≥60 years reported in Ref. 26, those aged < 60 years reported in Ref. 10 and other patients aged < 60 years of the database (data of patients aged≥and < 60 years are equally updated to 2013); the cutoff of daytime BP to define MUCH was chosen for homogeneity with other studies. Data of the Jackson Heart Study are published data. Daytime BP recording interval: OvA Study (30 minutes), Chieti-Pescara Study (15 minutes), IDACO Study (15–30 minutes), Hadassah Study (20 minutes), Jackson Heart Study (20 minutes) and Spanish Registry Study (20 minutes).
Main characteristics of studies using home BP recording are reported in Table 2. The pooled population consisted of 17742 patients who experienced 394 events. All the studies defined MUCH as clinic BP < 140/90 mmHg and home BP > 135/85 mmHg. Mean follow-up ranged from 2 to 9.4 years. All the studies evaluated fatal and nonfatal cardiovascular events (stroke, coronary artery disease and heart failure in three studies and stroke and coronary artery disease in two studies). Globally, we included 30352 patients who experienced 1327 events.
Table 2.
Main characteristics of selected studies using home blood pressure recording
| Patients | MUCH Definition | FU (years) | Events | Type of Event | |||
|---|---|---|---|---|---|---|---|
| Study | CH | MUCH | CH | MUCH | |||
| SHEAF Study 20048 | 685 | 462 | Home BP >135/85 mmHg | 3.2 | 26 | 41 | Fatal/Nonfatal CVE |
| J-HEALTH Study 200817 | 689 | 566 | Home BP >135/85 mmHg | 3.5 | 5 | 9 | Fatal/Nonfatal CVE |
| IDHOCO Study 201420 | 328 | 232 | Home BP >135/85 mmHg | 8.3 | 57 | 66 | Fatal/Nonfatal CVE |
| Dallas Heart Study 201522 | 171 | 122 | Home BP >135/85 mmHg | 9.4 | 17 | 37 | All-Cause Mortality |
| HONEST Study 201725 | 8608* | 5879* | Home BP >135/85 mmHg | 2.0 | 64† | 75† | Fatal/nonfatal CVE |
BP, blood pressure; CH, controlled hypertension; CVE, cardiovascular events (stroke, coronary artery disease and heart failure for SHEAF, IDHOCO and Dallas Heart Studies; stroke and coronary artery disease for J-HEALTH and HONEST Studies); FU, follow-up (mean); HONEST, Home blood pressure measurement with Olmesartan Naive patients to Establish Standard Target blood pressure; IDHOCO, International Database on HOme blood pressure in relation to Cardiovascular Outcome; J-HEALTH, Japan Hypertension Evaluation with Angiotensin II antagonist Losartan THerapy); MUCH, masked uncontrolled hypertension; SHEAF, Self-measurement of blood pressure at Home in the Elderly: Assessment and Follow-up.
Patients without diabetes mellitus (including those with chronic kidney disease) plus patients with diabetes mellitus (including those with chronic kidney disease)
the event number is calculated considering the event rate per 1000 person/years in each group, the number of patients in each group and the mean duration of follow-up (data are extracted from Figure 4a of the manuscript).25 Data of the Dallas Heart Study are provided by the authors. Data of the SHEAF, J-HEALTH and IDHOCO Studies are published data. Home BP in the SHEAF Study: 3 consecutive readings in the morning and in the evening for a 4-day period. Home BP in the J-HEALTH Study: 1 reading in the morning (each month, usually on the day of attending hospital) during 6 months of treatment (thereafter patients were categorized in various subgroups). Home BP in the IDHOCO Study (including five studies): 2 consecutive readings in the morning and in the evening on 7 consecutive days in one study; 1 reading in the morning for 4 weeks in one study; 2 consecutive readings in the morning and in the evening for 3 days in one study; 3 consecutive readings in the morning and in the evening for 5 consecutive days in one study; mean of all morning measurements in one study. Home BP in the Dallas Heart Study: mean of the third to fifth BP measurements. Home BP in the HONEST Study: 2 consecutive readings in the morning on 2 different days at 4 and 16 weeks, and 6, 12, 18 and 24 months.
Other characteristics of studies are reported in Table S1 (please see http://hyper.ahajournals.org.). All of them assessed general hypertensive populations; indeed, studies or sub-analyses evaluating specific populations such as those with diabetes or chronic kidney disease were not included. The prognostic value of MUCH was evaluated across various ethnicities. A similar set of covariates, including main cardiovascular risk factors, was used in multivariate analysis in the majority of studies and some studies used additional covariates. According to the Newcastle-Ottawa scale, all the included studies were of high quality (Table S2) (please see http://hyper.ahajournals.org.).
Figure 2 gives the adjusted HR and 95% CI of the individual studies and of the overall analysis between MUCH and CH. The overall adjusted HR was 1.80 (95% CI 1.57–2.06), P=0.0001, for MUCH versus CH. The degree of heterogeneity of the HR estimates across the studies (I2 and τ) were modest and statistically non‐significant (p=0.20 for the Q statistic). To further explore this aspect, subgroup meta-analysis was performed according to the method of BP measurement, follow-up length, type of event and ethnicity (Table 3). The adjusted HR was 1.83 (95% CI 1.52–2.21) for studies using ambulatory BP monitoring and 1.75 (95% CI 1.38–2.20) for studies using home BP measurement with no significant difference between subgroups. Risk was significantly higher in MUCH than in CH in both studies with a mean follow-up shorter and longer than 5 years and in both studies evaluating different types of composite events and all-cause mortality, and no significant difference was found among specific subgroups (Table 3). As far as ethnicity, we found some heterogeneity among subgroups. Indeed, though MUCH was always at significantly higher risk than CH, the lowest HR was found in studies including Asian patients only and the highest HR was found in studies including Black patients (Table 3). If one study25, in which categorization of patients by home BP was somehow different from others, was excluded the results regarding overall analysis and subgroup analysis by BP measurement method, follow-up length and types of events did not substantially change; on the contrary, there was no more heterogeneity among ethnic subgroups. Sensitivity analysis indicated that none of the studies had a significant influential effect on the overall estimate in both the global analysis (Figure S1) (please see http://hyper.ahajournals.org.) and the analysis evaluating studies with ambulatory BP monitoring and home BP measurement separately (Figure S2) (please see http://hyper.ahajournals.org.). When we explored for publication bias and small-study effect, the Begg and Mazumdar and Egger’s tests did not attain statistical significance (all 2-tailed P > 0.5). However, when we applied Duval and Tweedie’s trim and fill method, one study appeared missing to the left side of the mean effect and the imputed point estimate was 1.76, 95% CI 1.52–2.03, (Figure S3) (please see http://hyper.ahajournals.org.).
Figure 2.
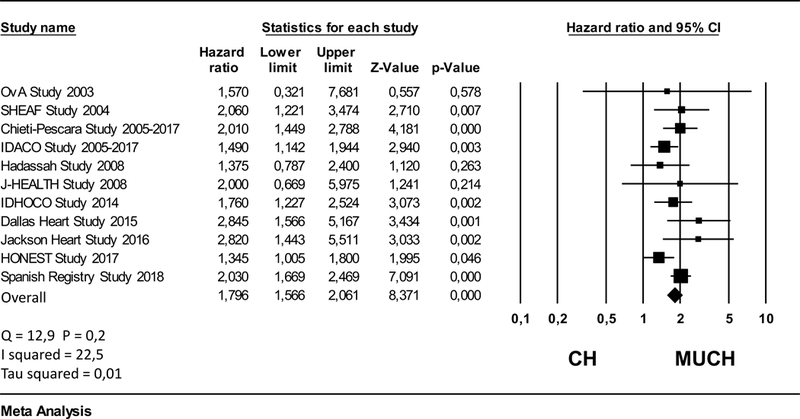
Forest plot showing the adjusted hazard ratio and 95% confidence interval (CI) between patients with masked uncontrolled hypertension (MUCH) and those with controlled hypertension (CH). Data of the OvA, Chieti-Pescara, IDACO, Hadassah, Spanish Registry and Dallas Heart Studies are provided by the authors. Data of the HONEST Study are extracted from Figures 4a and 4b of the manuscript25; they are a pooled estimate of values of MUCH patients without diabetes mellitus (including those with chronic kidney disease) and of MUCH patients without chronic kidney disease (including those with diabetes mellitus). Data of the SHEAF, J-HEALTH, IDHOCO and Jackson Heart Studies are published data.
Table 3.
Random effects meta-analysis according to the method of blood pressure measurement, follow-up length, type of composite event and ethnicity in the comparison between masked uncontrolled hypertension and controlled hypertension
| Variable | Studies | Subjects/Events | Adjusted HR (95% CI) |
P |
|---|---|---|---|---|
| Method of BP measurement | ||||
| ABPM*,†,‡,§,║,¶ | 6 | 12610/933 | 1.83 (1.52−2.21) | 0.75 |
| HBPM#,**,††,‡‡,§§ | 5 | 17742/394 | 1.75 (1.38−2.20) | |
| Mean follow-up length | ||||
| ≤ 5 years*,¶,#,**,§§ | 5 | 26962/672 | 1.77 (1.41−2.22) | 0.82 |
| ≥ 5 years†,‡,§,║,††,‡‡ | 6 | 3390/655 | 1.83 (1.49−2.24) | |
| Type of composite event | ||||
| Stroke + CAD + HF + PR*,†,‡ | 3 | 1791/404 | 1.70 (1.27−2.27) | 0.76 |
| Stroke + CAD + HF #,††,‡‡ | 3 | 2000/241 | 2.06 (1.49−2.84) | |
| Stroke + CAD║,**,§§ | 3 | 16149/191 | 1.64 (1.16−2.31) | |
| All-cause mortality§,¶ | 2 | 10412/491 | 1.85 (1.36−2.51) | |
| Ethnicity | ||||
| Caucasian only*,†,§,¶,# | 5 | 12586/719 | 1.96 (1.69−2.29) | 0.02 |
| Asian only**,§§ | 2 | 15742/153 | 1.38 (1.04−1.83) | |
| Black included║,‡‡ | 2 | 700/92 | 2.83 (1.81−4.42) | |
| Caucasian, Asian, Hispanic‡,†† | 2 | 1324/363 | 1.58 (1.28−1.96) | |
ABPM, ambulatory blood pressure monitoring; CAD, coronary artery disease; CI, confidence interval; HBPM, home blood pressure measurement; HF, heart failure; HR, hazard ratio; PR, peripheral revascularization.
OvA Study;
Chieti-Pescara Study;
IDACO Study;
Hadassah Study;
Jackson Heart Study (included 100% Black patients);
Spanish Registry Study;
SHEAF Study;
J-HEALTH Study;
IDHOCO Study;
Dallas Heart Study (included 50% Black patients);
HONEST Study.
DISCUSSION
This meta-analysis shows that risk of cardiovascular events and all-cause mortality is significantly higher in patients with MUCH than in those with CH. Moreover, MUCH detected by ambulatory BP monitoring or home BP measurement appear to convey similar prognostic information, though some differences exist across the studies.
To the best of our knowledge, this is the first meta-analysis specifically evaluating the prognostic value of MUCH. Indeed, previous ones evaluated the prognostic value of masked hypertension in untreated patients5,6 or untreated, treated and mixed populations analysed together33,34,36. Fagard and Cornelissen33, executed a meta-analysis of seven studies. The adjusted HR of masked hypertension versus normotension was 2.0 (95% CI 1.58–2.52). The aim of the study was to include subjects coming from the same population and the authors had to select reports evaluating untreated, treated8,10 or mixed cohorts that were analysed together in the meta-analysis. Bobrie et al34, performed a meta-analysis of six studies. Compared with normotension, the overall adjusted HR was 1.92 (95% CI 1.51–2.44) for masked hypertension. Among selected studies, one had been performed in untreated subjects, two8,10 in treated subjects and three in mixed populations that were analysed together in the meta-analysis. Palla et al36, published a meta-analysis in which the impact of masked hypertension in comparison with normotension in treated subjects was also evaluated. Four studies9,11,19,20 for cardiovascular events and three studies19,20,24 for mortality were included. Compared with normotension, the odds ratio was 2.03 (95% CI 1.52–2.72) concerning cardiovascular events and 1.44 (1.03–2.01) concerning mortality for masked hypertension. However, the selected studies were substantially heterogeneous; indeed, among them one included a mixed population11and one included selected populations19. Moreover, other studies evaluating patients with MUCH were not included.7,8,10,16,17,22,25 Finally, the odds ratio, and not the adjusted HR, was calculated. The abovementioned meta-analyses33,34,36 have been of relevance in trying to address the prognostic value of masked hypertension in untreated and treated subjects. However, compared with them33,34,36 our study included only treated patients comprising those with MUCH and CH and analysed studies that were homogeneous about hypertensive population type. Moreover, we had the opportunity to pool together the data obtained directly by the authors of various studies. This aspect makes our meta-analysis the largest available about the prognostic value of MUCH.
MUCH could depend on various conditions including smoking habit, alcohol consumption, BP response to physical activity, psychological stress, some comorbidities, different effect of therapy on office and out-of-office BP (it has been reported that a 3 mmHg office systolic BP reduction equates approximately to 2 mmHg out-of-office systolic BP reduction), clinic BP recorded at peak of antihypertensive effect, insufficient prescribed doses and incomplete adherence to treatment.30–32,35 Whatever the reason the first purpose is to identify MUCH which is associated with increased cardiovascular risk and then to control out-of-office BP by correcting potential factors contributing to MUCH in the patient.
Recent guidelines47 recommend measurement of out-of-office BP for confirmation and management of hypertension, given the superiority of out-of-office BP over clinic BP in predicting prognosis. The findings of the present study further support the relevance of out-of-office BP in the prognostic stratification of patients. At present, however, studies showing the superiority of out-of-office BP control over clinic BP control in reducing cardiovascular risk are still lacking.
The present study has some limitations. First, the set of events evaluated in the single studies was not exactly the same; however, when subgroup meta-analysis was performed taking into account the type of cardiovascular events and all-cause-mortality, the risk was always significantly higher in patients with MUCH. Second, a minority of subjects (less than 0.5% of the global population) has been included in both the IDACO9,12,13,15,18,19,23 and International Database of HOme blood pressure in relation to Cardiovascular Outcome20 studies; however, given the relatively small number of patients, we think this aspect has not significantly affected the results. Third, data of the Home blood pressure measurement with Olmesartan Naive patients to Establish Standard Target blood pressure (HONEST) study25 were extrapolated from the manuscript. Fourth, the HONEST study25 used a categorization of patients by home BP that was somehow different from other studies; however, if that study was excluded from analysis the overall result did not substantially change.
PERSPECTIVES
This meta-analysis shows that patients with MUCH have significantly higher risk of cardiovascular events and all-cause mortality than those with CH and that MUCH detected by ambulatory BP monitoring or home BP measurement appear to convey prognostic information of similar magnitude. Thus, every effort should be made to detect this condition and to identify the best therapeutic approach. In such a context, future studies are needed, such as the MASked-unconTrolled hypERtension management based on office BP or on out-of-office (ambulatory) BP measurement (MASTER) Study48, to evaluate whether out-of-office BP control improves cardiovascular outcome in these patients.
Supplementary Material
NOVELTY AND SIGNIFICANCE
What Is New?
• This is the first meta-analysis evaluating cardiovascular outcome and mortality in patients with MUCH.
• The present study pooled together data obtained in a very large population (30352 patients) experiencing many events (1327).
What Is Relevant?
• This study provides evidence that in treated patients with normal clinic BP the evaluation of out-of-office BP is of relevance for risk stratification.
• This study supports that future randomized trials should be conducted to evaluate whether out-of-office BP control improves outcome in patients with MUCH.
Summary
• This meta-analysis shows that risks of cardiovascular events and all-cause mortality are significantly higher in patients with MUCH than in those with CH. MUCH detected by ambulatory BP monitoring or home BP measurement appear to convey similar prognostic information.
Acknowledgments
SOURCES OF FUNDING
Sante D. Pierdomenico, Anna M. Pierdomenico and Francesca Coccina have no sources of funding.
Wanpen Vongpatanasin is supported by the UT Southwestern O’Brien Kidney Center, the Pak Center of Mineral Metabolism and Clinical Research, and R01 HL133179. The Dallas Heart Study was funded by the Donald W. Reynolds Foundation and was partially supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award Number UL1TR001105.
To be completed online.
Footnotes
CONFLICT OF INTEREST
None.
REFERENCES
- 1.Liu JE, Roman MJ, Pini R, Schwartz JE, Pickering TG, Devereux RB. Cardiac and arterial target organ damage in adults with elevated ambulatory and normal office blood pressure. Ann Intern Med1999;131:564–572. [DOI] [PubMed] [Google Scholar]
- 2.Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G. Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] study). Circulation 2001;104:1385–1392. [DOI] [PubMed] [Google Scholar]
- 3.Wing LM, Brown MA, Beilin LJ, Ryan P, Reid CM; ANBP2 Management Committee and Investigators. Second Australian National Blood Pressure Study. ‘Reverse white-coat hypertension’ in older hypertensives. J Hypertens 2002;20:639–644. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension 2002;40:795–796. [DOI] [PubMed] [Google Scholar]
- 5.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta-analysis. Am J Hypertens 2011;24:52–58. [DOI] [PubMed] [Google Scholar]
- 6.Asayama K, Thijs L, Li Y, et al. ; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes (IDACO) Investigators. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension 2014;64:935–942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, Gheeraert PJ, Missault LH, Braun JJ, Six RO, Van Der Niepen P, O’Brien E. Prognostic value of ambulatory blood-pressure recordings in patients with treated hypertension. N Engl J Med 2003;348:2407–2415. [DOI] [PubMed] [Google Scholar]
- 8.Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 2004;291:1342–1349. [DOI] [PubMed] [Google Scholar]
- 9.Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 2005;46:508–515. [DOI] [PubMed] [Google Scholar]
- 10.Pierdomenico SD, Lapenna D, Bucci A, Di Tommaso R, Di Mascio R, Manente BM, Caldarella MP, Neri M, Cuccurullo F, Mezzetti A. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens 2005;18:1422–1428. [DOI] [PubMed] [Google Scholar]
- 11.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens 2005;19:801–807. [DOI] [PubMed] [Google Scholar]
- 12.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study. Am J Hypertens 2006;19:243–250 [DOI] [PubMed] [Google Scholar]
- 13.Ingelsson E, Bjorklund K, Lind L, Arnlov J, Sundstrom J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. [DOI] [PubMed] [Google Scholar]
- 14.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006;47:846–853. [DOI] [PubMed] [Google Scholar]
- 15.Hansen TW, Kikuya M, Thijs L, Björklund-Bodegård K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA; IDACO Investigators. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens 2007; 25:1554–1564. [DOI] [PubMed] [Google Scholar]
- 16.Ben-Dov IZ, Kark JD, Mekler J, Shaked E, Bursztyn M. The white coat phenomenon is benign in referred treated patients: a 14-year ambulatory blood pressure mortality study. J Hypertens 2008;26:699–705. [DOI] [PubMed] [Google Scholar]
- 17.Shimada K, Fujita T, Ito S, Naritomi H, Ogihara T, Shimamoto K, Tanaka H, Yoshiike N. The importance of home blood pressure measurement for preventing stroke and cardiovascular disease in hypertensive patients: a sub-analysis of the Japan Hypertension Evaluation with Angiotensin II Antagonist Losartan Therapy (J-HEALTH) study, a prospective nationwide observational study. Hypertens Res 2008;31:1903–1911. [DOI] [PubMed] [Google Scholar]
- 18.Franklin SS, Thijs L, Hansen TW, et al. ; International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension 2012;59:564–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Franklin SS, Thijs L, Li Y, et al. ; International Database on Ambulatory blood pressure in Relation to Cardiovascular Outcomes Investigators. Masked hypertension in diabetes mellitus: treatment implications for clinical practice. Hypertension 2013;61:964–971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stergiou GS, Asayama K, Thijs L, Kollias A, Niiranen TJ, Hozawa A, Boggia J, Johansson JK, Ohkubo T, Tsuji I, Jula AM, Imai Y, Staessen JA; International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators. Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertension 2014;63:675–682. [DOI] [PubMed] [Google Scholar]
- 21.Minutolo R, Gabbai FB, Agarwal R, Chiodini P, Borrelli S, Bellizzi V, Nappi F, Stanzione G, Conte G, De Nicola L. Assessment of achieved clinic and ambulatory blood pressure recordings and outcomes during treatment in hypertensive patients with CKD: a multicenter prospective cohort study. Am J Kidney Dis 2014;64:744–752. [DOI] [PubMed] [Google Scholar]
- 22.Tientcheu D, Ayers C, Das SR, McGuire DK, de Lemos JA, Khera A, Kaplan N, Victor R, Vongpatanasin W. Target organ complications and cardiovascular events associated with masked hypertension and white-coat hypertension: analysis from the Dallas Heart Study. J Am Coll Cardiol 2015;66:2159–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Satoh M, Asayama K, Kikuya M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: The Ohasama Study. Hypertension 2016;67:48–55. [DOI] [PubMed] [Google Scholar]
- 24.Booth JN 3rd, Diaz KM, Seals SR, Sims M, Ravenell J, Muntner P, Shimbo D. Masked hypertension and cardiovascular disease events in a prospective cohort of blacks: The Jackson Heart Study. Hypertension 2016;68:501–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kushiro T, Kario K, Saito I, Teramukai S, Sato Y, Okuda Y, Shimada K. Increased cardiovascular risk of treated white coat and masked hypertension in patients with diabetes and chronic kidney disease: the HONEST Study. Hypertens Res 2017;40:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pierdomenico SD, Pierdomenico AM, Coccina F, Porreca E. Prognosis of masked and white coat uncontrolled hypertension detected by ambulatory blood pressure monitoring in elderly treated hypertensive patients. Am J Hypertens 2017;30:1106–1111. [DOI] [PubMed] [Google Scholar]
- 27.Wang C, Zhang J, Li Y, Ma X, Ye Z, Peng H, Lou T. Masked hypertension, rather than white-coat hypertension, has a prognostic role in patients with non-dialysis chronic kidney disease. Int J Cardiol 2017;230:33–39. [DOI] [PubMed] [Google Scholar]
- 28.Banegas JR, Ruilope LM, de la Sierra A, Vinyoles E, Gorostidi M, de la Cruz JJ, Ruiz-Hurtado G, Segura J, Rodríguez-Artalejo F, Williams B. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med 2018;378:1509–1520. [DOI] [PubMed] [Google Scholar]
- 29.Banegas JR, Ruilope LM, de la Sierra A, de la Cruz JJ, Gorostidi M, Segura J, Martell N, García-Puig J, Deanfield J, Williams B. High prevalence of masked uncontrolled hypertension in people with treated hypertension. Eur Heart J 2014;35:3304–3312. [DOI] [PubMed] [Google Scholar]
- 30.Franklin SS, O’Brien E, Thijs L, Asayama K, Staessen JA. Masked hypertension: a phenomenon of measurement. Hypertension 2015;65:16–20. [DOI] [PubMed] [Google Scholar]
- 31.Franklin SS, O’Brien E, Staessen JA. Masked hypertension: understanding its complexity. Eur Heart J 2017;38:1112–1118. [DOI] [PubMed] [Google Scholar]
- 32.Pickering TG, Eguchi K, Kario K. Masked hypertension: a review. Hypertens Res 2007;30:479–488. [DOI] [PubMed] [Google Scholar]
- 33.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 2007;25:2193–2198. [DOI] [PubMed] [Google Scholar]
- 34.Bobrie G, Clerson P, Ménard J, Postel-Vinay N, Chatellier G, Plouin PF. Masked hypertension: a systematic review. J Hypertens 2008;26:1715–1725. [DOI] [PubMed] [Google Scholar]
- 35.Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens 2014;28:521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palla M, Saber H, Konda S, Briasoulis A. Masked hypertension and cardiovascular outcomes: an updated systematic review and meta-analysis. Integr Blood Press Control 2018;11:11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 38.Stergiou GS, Baibas NM, Kalogeropoulos PG. Cardiovascular risk prediction based on home blood pressure measurement: the Didima study. J Hypertens. 2007;25:1590–1596. [DOI] [PubMed] [Google Scholar]
- 39.Hänninen MR, Niiranen TJ, Puukka PJ, Johansson J, Jula AM. Prognostic significance of masked and white-coat hypertension in the general population: the Finn-Home Study. J Hypertens 2012;30:705–712. [DOI] [PubMed] [Google Scholar]
- 40.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 41.Egger M, Smith GD, Phillips AN. Meta-analysis: principles and procedures. BMJ 1997;315:1533–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Stat Med 2002; 21:1559–1573. [DOI] [PubMed] [Google Scholar]
- 44.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–1101. [PubMed] [Google Scholar]
- 45.Egger M, Smith GD, Schneider M, Minder C. Bias in metaanalysis detected by a simple, graphical test. BMJ 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Duval S, Tweedie R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc 2000;95:89–98. [Google Scholar]
- 47.Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:e13–e115. [DOI] [PubMed] [Google Scholar]
- 48.Parati G, Agabiti Rosei E, Bakris G, et al. Masked-uncontrolled hypertension management based on office BP or on out-of-office (ambulatory) BP measurement (MASTER): study protocol. J Hypertens 2017;35 (e-Supplement 2):e190 (Abstract). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


