Abstract
The current study sought to test the role of family support as a buffer of life stress for depressive symptoms in a sample of young adults at low- and high-risk for depression based on a previous history of depression. Ninety seven young adults, 54 with remitted depression and 43 without prior history of depression, completed reports of family relationships, disruptive life events, and depressive symptoms at baseline and every 2 months for 10 months. Results revealed significant interactions between family environment and life events predicting Beck Depressive Inventory (BDI) scores at baseline, such that individuals with better family support were buffered from risk associated with life stress, and this was true even after accounting for a previous history of depression. Longitudinal analyses utilizing the PHQ-9 as a depressive symptom measure did not find significant associations with family environment, but did find that more stressful events at baseline were associated with increasing levels of symptoms over time. Exploratory analyses suggest that discrepant findings for baseline versus longitudinal analyses may be due to differences in symptom measurement and to associations between family environment and cognitive features of depression. These findings provide qualified support for the continued relevance of families as stress buffers in young adulthood across a spectrum of risk for depression.
Keywords: Remitted depression, families, stressful life events, depressive symptoms
Depression is one of the most prevalent forms of psychopathology, with estimates that between 16–42% of individuals meet criteria for the disorder before the age of 32 (Kessler et al., 2005; Moffitt et al., 2009). The impairment and disability associated with depression makes it one of the leading causes of global disease burden (Üstün, Ayuso-Mateos, & Chatterji, 2004), with the disorder accounting for the most years lost to disability of any illness (World Health Organization, 2009). Individuals with depression are at heightened risk for somatic health problems (Penninx, Milaneschi, Lamers, & Vogelzangs, 2013), lower educational attainment (Fletcher, 2008), and suicide (J. Angst, Angst, & Stassen, 1999). For these reasons, understanding factors that contribute to the onset and course of depressive symptoms is critical for developing interventions and reducing suffering.
An individual’s social environment, and particularly his or her family environment, is believed to play one of the key roles in the development and trajectory of depression (Hammen, Shih, & Brennan, 2004; Sheeber, Hops, & Davis, 2001). Individuals from more conflictual, less supportive families are at increased risk for depressive symptoms (Epkins & Harper, 2016; Sheeber, Hops, Alpert, & Davis, 1997). Indeed, meta-analytic work demonstrates that low levels of parental warmth and high levels of parental aversiveness, withdrawal, and overinvolvement are each reliably related to youth depression (McLeod, Wood, & Weisz, 2007). Conversely, more positive family environments appear to be protective against mental health problems, consistent with the social buffering hypothesis (Cohen & Wills, 1985; Wilcox, 1981). Here, having closer parent-child relationships has been found to buffer adolescents from depressive symptoms in the face of interpersonal problems, such as bullying (DeLay, Hafen, Cunha, Weber, & Laursen, 2013; Herman-Stahl & Petersen, 1996). Further supporting the causal role of parenting, intervention studies have demonstrated that improvements in parenting lead to better psychological profiles in children, including fewer depressive symptoms and better self-regulation (Brody et al., 2005; Compas et al., 2010; Connell & Dishion, 2008).
One way in which positive family environments may relate to offspring’s mental health is by acting as a buffer during experiences of negative life events. The stress associated with such events as romantic breakups, academic or professional failures, or experiences with crime have been robustly associated with higher rates of depression across the lifespan (Bouma, Ormel, Verhulst, & Oldehinkel, 2008; Monroe & Harkness, 2005; Risch, Herrell, Lehner, Liang, & Merikangas, 2009). Here, researchers have explored both the number of events an individual experiences as well as the amount of disruption they experience as a result of such events as related, but separate, indices of this stress (Newcomb, Huba, & Bentler, 1981). For individuals who experience such events, however, a supportive family environment may lessen the impact. For example, Ge et al. (2009) found that parent-child closeness buffered adolescents from the effects of stressful events on their depressive symptoms 3 years later. This may occur by parents providing emotional support or helping with problem-solving during difficult periods. It is also possible that positive relationships preventatively create more adaptive psychological profiles for children, perhaps by increasing children’s self-esteem, such that stressful events are experienced as less threatening. To wit, several studies have pointed to cognitively-facilitated processes, like self-image, as key mediators of links between parenting and youth depressive symptoms (Garber, Robinson, & Valentiner, 1997; Plunkett, Henry, Robinson, Behnke, & Falcon, 2007).
Although most research on associations between parenting and offspring depression focuses on children and adolescents (Restifo & Bögels, 2009), it is also important to consider how such family environments may continue to affect offspring into young adulthood. Abundant work documents the long term effects of early family experiences (Repetti, Taylor, & Seeman, 2002), supporting the possibility that family characteristics may continue to predict depressive symptoms even once offspring have grown and moved away from home. Indeed, Galambos, Barker, and Kahn (2006) found that less conflict in parent-child relationships not only predicted lower depression symptomatology at baseline when offspring were 18 years old, but also predicted a steeper decline in depressive symptoms across the following seven years. This is notable given the normative developmental experiences of increasing autonomy that occur during this emerging adulthood period. Indeed, capitalizing on the college transition that many young adults undertake, Moreira and Telzer (2015) found that greater family cohesion prior to college buffered students from increases in depressive symptoms two months into their first semester. Similarly, work by Levens, Elrahal, & Sagui (2016) revealed that family support was protective against depressive symptoms in offspring during the college transition, but that this was only true if students were perceived as being low in stress reactivity (itself a marker of reduced vulnerability to depression). It remains unclear, however, whether buffering processes would continue to predict depressive symptoms across all types of stressors for this age group. Also unknown is whether these patterns would be observed in those at heightened risk for depression.
One group of individuals who are at greater risk for future depressive symptoms are those with a previous history of depression. Up to 80% of individuals who have previously experienced a depressive episode will meet full criteria for at least one other episode in their lifetime and that nearly all will experience subsyndromal episodes (Judd, 1997). The majority of research on depressive symptoms and family environment in community samples, however, fails to assess prior history of depression and thus to distinguish between those with greater or lesser risk. Here, studies utilizing individuals with remitted depression provide an important comparison group. Comparing remitted individuals to those without a prior history of depression allows researchers to overcome concerns of reporting bias associated with active depression (Chilcoat & Breslau, 1997) while also exploring relative vulnerability to future symptoms.
To address these gaps in the literature, the current study tested the interaction between family environment and life stress predicting depressive symptoms at baseline and across a 10-month period using a sample of young adults with remitted depression (rMDD) or no history of depression. Specifically, we hypothesized that individuals who experienced more negative life events or who reported greater life disruption associated with negative events would show higher levels of depressive symptoms than those with less life stress. We predicted that these associations would be buffered, however, if individuals reported coming from a more positive family environment. We also tested whether vulnerability to depression, as evidenced by having previously experienced at least one depressive episode, would account for any observed associations. Lastly, we conducted exploratory analyses to identify which symptoms of depression were most associated with the family environment.
Method
Participants
As part of a larger study, young adults with remitted MDD (rMDD) or with no history of psychopathology were recruited at two universities in the United States through university and community flyers, internet and public transportation advertisements. All study activities were approved by the Institutional Review Board at the University of Illinois-Chicago (protocol number 2012–0568). Interested individuals who met criteria via a phone screen were invited for a baseline diagnostic interview, which included the Diagnostic Interview for Genetic Studies (DIGS; Nurnberger et al., 1994), from which inclusion and exclusion criteria were further assessed and confirmed. Screening questions and structured interviews were identical for both potential rMDD and potential Health Control (HC) individuals. Individuals with rMDD were required to have a history of at least one major depressive episode and a score of less than 7 on the Hamilton Depression Rating Scale (Hamilton, 1960). Diagnosis of MDD history was determined with DIGS. HC individuals were required to have never met criteria for any Axis I or II psychiatric disorder (including MDD), based on responses to the DIGS and to have no first-degree relatives with a history of psychiatric illness, based on the DIGS, and the Family Interview for Genetic Studies (Maxwell, 1992). Exclusion criteria for either group included a history of substance abuse or dependence within the previous six months, according to responses on the DIGS, or a score of more than 7 on the Hamilton Depression Rating Scale. Only participants with complete data on the primary variables of interest at baseline (e.g., measures of demographics, family environment, life stress, and depressive symptoms) were included in the current study. There were no differences in study variables for participants who were enrolled in the larger project but who did not have complete data compared to those with complete data. The final sample included 54 individuals with rMDD and 43 HC. Sixty-three percent of the sample identified as White and 68% were female. Individuals were between 18- and 23-years-old (M=20.89, SD=1.63), were free of medication for at least the past 30 days, and had on average 14.51 years of education. Participants were compensated $40 for the initial clinical interview and then $10 per time point for completing questionnaires.
Procedure
Following the phone screen and confirmatory diagnostic interview, individuals who met inclusion criteria completed self-report questionnaires assessing their family environment, history of stressful life experiences, and depressive symptoms during a baseline laboratory visit. Following this visit, they completed online self-report measures of depressive symptoms every two months for ten months, resulting in a total of six assessments. On average, participants completed 4.21 assessments, with over 87 percent of participants completing two or more assessments.
Measures
Depressive Symptoms.
During the baseline assessment, participants completed the Beck Depression Inventory-II (BDI; Beck, Steer, & Brown, 1996), a widely-used measure of depressive symptoms that probes for the extent to which an individual has experienced 21 symptoms in the previous week (α=.91, current sample). It contains both cognitive (8 item) and noncognitive (13 item) subscales. At baseline and then for every two months, participants also completed the Patient Health Questionnaire-9 (PHQ-9; Kroenke, Spitzer, & Williams, 2001), a nine-item screen that assesses each of the nine DSM-IV criteria for a depressive episode within the past two weeks (α=.85, current sample). (To minimize participant burden, the BDI was not administered at follow-up sessions.) The reliability and validity of both measures have been robustly documented (Aben, Verhey, Lousberg, Lodder, & Honig, 2011; Löwe, Kroenke, Herzog, & Gräfe, 2004).
Family Environment.
At baseline, participants also reported on their family environment using the Family Adaptability and Cohesion Evaluation Scale (Olson, Portner, Bell, & Tiesel, 1991). This 30-item measure assesses the extent to which individuals are supportive of and engaged with their family members. It involves participants rating items from 0 to 5 for the extent to which statements are characteristic of their families, such as “Family members discuss problems and feel good about the solutions” and “In our family, everyone shares responsibility.” The measure yields two subscales corresponding to Adaptability and Cohesion, which were highly correlated in the present study (r=.84, p<.001). Consequently, the total FACES score was used, with higher scores reflecting a more optimal family environment (α=.80 all items, current sample).
Stressful Life Events.
Participants also reported on their experiences of stressful life events during the baseline visit using the Life Event Occurrences Survey (LEOS; McKee, Maciejewski, Falba, & Mazure, 2003), which probes for whether or not 32 potentially stressful events occurred in the previous six months. Examples of events include physical assault, separation from a romantic partner, or trouble with a boss. If an event did occur, participants also reported on the amount of disruption that occurred due to the event, rating from 0 (“no disruption in daily living”) to 3 (“resulted in severe changes to daily living lasting at least 3 days”). This measure has been used in both clinical and community samples (McKee et al., 2003; Saunders et al., 2014). In the current study, the sum of total events experienced and the sum of disruption ratings were computed separately.
Demographic Information.
During the baseline assessment, participants also reported on their age, gender, race/ethnicity, and years of education, which were included as covariates in all analyses.
Data Analytic Plan
Descriptive statistics were computed for the main study variables.
Next, multiple regression analyses were run in which BDI scores were predicted by family environment, number of stressful life events, and their interaction, along with demographic covariates of age, gender, racial minority status, and years of education. This was repeated in a second model, substituting amount of disruption associated with life events for the total number of life events. Variables were mean-centered prior to the creation of the interaction term. Finally, given that our sample included both individuals with and without a history of depression, both models were rerun to probe whether findings might be due to differences attributable to being in the HC or rMDD group. To test this, depression history status was added as a dummy code.
Turning to changes in depressive symptoms over time, we next conducted a series of growth curve models using Hierarchical Linear and Nonlinear Modeling (HLM) software (Version 6.08; Raudenbush, Bryk, & Congdon, 2004), in which changes in PHQ-9 scores over visits were modeled by family environment, number of life events, and their interaction, repeating analyses to explore disruption associated with life events in place of total number of events. Given that time was centered with baseline=0, the prediction of the intercept in each model reflects associations amongst family environment, life stress, and their interaction for baseline PHQ-9 scores (paralleling the multiple regression analyses examining BDI scores). In this way, Level 1 was composed of an intercept term, months since baseline, and an error term, whereas Level 2 was composed of family environments, number life events, the interaction between life events and family environment, participant age, gender, minority status, years of education, and an error term.
These analyses were then re-run accounting for rMDD vs HC membership. An example of a model is presented below:
Level 1: PHQ-9ti = π0i + π1i*(Months since baselineti) + eti
Level 2: π0i = β00 + β01 (Agei) + β02 (Educationi) + β03 (Minority Statusi) + β04 (Femalei) + β05 (Depression Groupi) + β06 (Family Enviornmenti) + β07 (Number Stressful Eventsi) + β08 (Family Environment*Number Eventsi) + r0i
π1i = β10 + β11(Agei) + β12(Educationi) + β13 (Minority Statusi) + β14 (Femalei) + β15 (Depression Groupi) + β16 (Family Enviornmenti) + β17 (Number Stressful Eventsi) + β18 (Family Environment*Number Eventsi) + r1i
Lastly, after identifying diverging patterns of results for the BDI versus PHQ-9 pertaining to family environment, post-hoc analyses probed associations between family environment with individual items on the BDI to explore whether family relationships were more associated with cognitive constructs which are primarily assessed on the BDI as opposed to the PHQ-9. To examine additional support for this interpretation, regression analyses were re-run predicting to the Cognitive and Noncognitive subscales of the BDI.
Results
Descriptive statistics for all study variables are presented in Table 1. Notably, all participants were high school graduates and young, suggesting that findings are best considered within that developmental framework.
Table 1.
Descriptive Statistics for Full Sample, Remitted Depressed, and Healthy Control Groups
| Full sample | Healthy Controls |
Remitted Depressed |
||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | t | p | |
| Age | 20.89 | 1.63 | 20.61 | 1.72 | 21.11 | 1.53 | −1.53 | .13 |
| Education | 14.50 | 1.45 | 14.51 | 1.50 | 14.50 | 1.42 | 0.04 | .97 |
| % Female | 68% | 67% | 69% | −.11 | .91 | |||
| % White | 63% | 72% | 59% | −1.31 | .19 | |||
| Family Environment |
108.11 | 20.64 | 118.60 | 15.56 | 99.76 | 20.48 | 5.15 | <.01 |
| Number Stressful Events |
3.69 | 2.65 | 2.95 | 1.93 | 4.28 | 3.00 | −2.63 | .01 |
| Disruption from Stressful Events |
4.01 | 4.81 | 2.37 | 3.33 | 5.31 | 5.40 | −3.29 | <.01 |
| BDI (baseline) | 3.67 | 5.81 | .93 | 1.65 | 5.85 | 6.94 | −5.04 | <.01 |
| PHQ-9 (baseline) | 2.65 | 3.83 | 1.14 | 2.25 | 3.87 | 4.39 | −3.93 | <.01 |
Family Environment, Stressful Life Experiences, and Baseline BDI Scores
Regression analyses probing the interaction between family environment and number of stressful life events, controlling for participant age, gender, ethnicity, and years of education, revealed significant simple effects of both family environment (b=−.10, SE=.03, p<.001) and stressful events (b=.76, SE=.20, p<.001), qualified by a trend level interaction (b=−.02, SE=.01, p=.05), such that for participants from lower-quality support families (1 SD below the mean), there was a significant association between the number of stressful events they experienced and their BDI scores (b = 1.19, t= 5.93, p<.001), whereas that association was only marginally significant for participants 1 SD above the mean (b =.34, t=1.67, p=.10; see Figure 1).
Figure 1. Interaction between Total Stressful Events and Family Environment Predicting BDI Scores at Baseline.
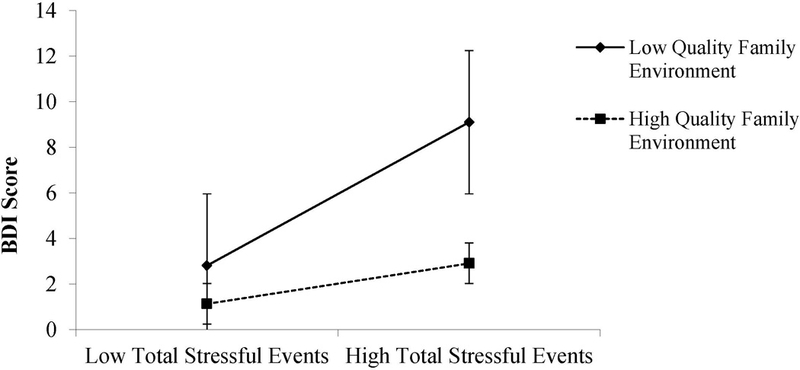
Note. Family environment and stressful events variables are plotted at 1 SD above (‘high’) and 1 SD below (‘low’) the sample means of those variables.
These analyses were repeated, examining participants’ ratings of disruption due to life events instead of total number of events. This revealed similar patterns, where lower-quality support (b=−.07, SE=.02, p=.007) and greater disruption (b=.57, SE=.10, p<.001) exerted simple effects and an interactive effect (b=−.01, SE=.00, p=.01) on BDI symptoms. Plotting scores at 1 standard deviation above and below the mean of family environment quality demonstrated that the association between disruption and BDI symptoms was stronger for participants reporting lower quality family environments (b =.79, t=6.54, p<.001) than higher quality family environment (b .34, t=2.35, p=.02) as displayed in Figure 2.
Figure 2. Interaction between Disruption from Stressful Events and Family Environment Predicting BDI Scores at Baseline.
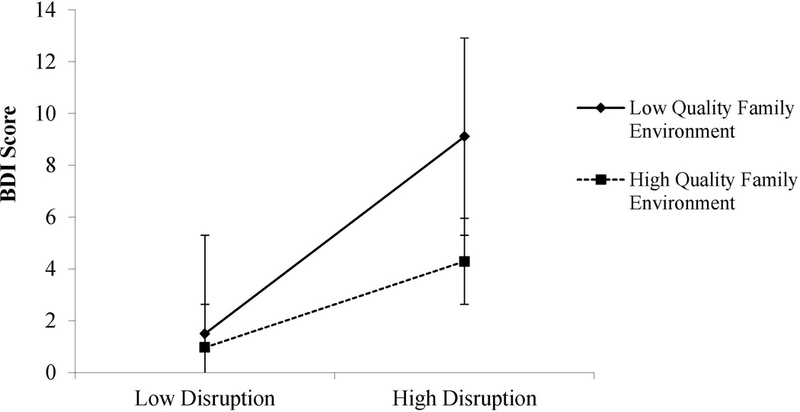
Note. Family environment and disruption variables are plotted at 1 SD above (‘high’) and 1 SD below (‘low’) the sample means of those variables.
Predicting Baseline BDI Scores Accounting for Group Membership
To assess whether associations between life stress variables, family environment, and BDI scores were due to differences between participants with rMDD versus no history of depression, analyses were re-run while including a dummy code indicating remitted depression status. For the regression model assessing family environment and total number of stressful events, the findings were the same. For the model of BDI scores predicted by disruption and family environment, the simple effect of family environment quality diminished slightly to marginal significance (b=−.05, SE=.03, p=.06), but disruption and the interaction between disruption and family environment remained significant contributors to depressive symptom scores. Full models are presented in Table 2. Together, these findings suggest that higher-quality family environment reduces the magnitude of the association between life stress experiences and depressive symptoms, above and beyond contributions of depression vulnerability1.
Table 2.
Results of Multiple Regression Predicting BDI Scores, Covarying Depression Group
| Predictor variable | R | R2 | F | Sig. | b | SE | p |
|---|---|---|---|---|---|---|---|
| Model with Number Stressful Events | .58 | .34 | 5.55 | <.00 1 |
|||
| Age | .17 | .55 | .76 | ||||
| Education | .19 | .61 | .75 | ||||
| Minority Status | −.06 | 1.10 | .96 | ||||
| Female | −.70 | 1.10 | .53 | ||||
| Depression Group | 2.63 | 1.20 | .03 | ||||
| Family Environment | −.07 | .03 | .01 | ||||
| Stressful Events | .65 | .20 | <.0 1 |
||||
| Family x Stressful Events | −.02 | .01 | .05 | ||||
| Model with Disruption from Events | .69 | .48 | 10.09 | <.00 1 |
|||
| Age | .28 | .48 | .57 | ||||
| Education | .10 | .54 | .85 | ||||
| Minority Status | .07 | .97 | .94 | ||||
| Female | −.94 | .98 | .34 | ||||
| Depression Group | 2.119 | 1.06 | .05 | ||||
| Family Environment | −.05 | .03 | .06 | ||||
| Disruption from Events | .52 | .10 | <.0 1 |
||||
| Family x Disruption | −.01 | .001 | .01 |
PHQ Scores at Baseline and Over Time
The intraclass correlation coefficient for the unconditional model revealed that 61% of the variance in PHQ-9 scores was due to between-participant features and 39% of the variance was due to within-person features. Modeling the trajectory of PHQ-9 scores over 5 time points from family environment, total stressful events, and their interaction revealed that family environment ratings significantly predicted baseline PHQ scores (i.e., the intercept; b=−.04, SE=.02, p=.03) , while the number of stressful events significantly predicted the slope of symptoms over time (b=.05, SE=.02, p=.01). There were no other simple effects or interactions. In other words, coming from a higher-quality family environment predicted lower depressive symptoms at baseline, but were not significantly related to the trajectory of symptoms over time. In contrast, having experienced more stressful events in the 6 months prior to baseline was not associated with baseline symptoms but predicted increasing depressive symptomatology over time.
Repeating this model substituting disruption associated with stressful life events for total number of events determined that family environment (b=−.03, SE=.02, p=.07) and disruption (b=.16, SE=.09, p=.07) were each marginally associated with baseline PHQ scores, but there was no significant interaction nor were there significant effects of family environment, disruption, nor their interaction on the slope of symptoms over time.
To determine whether observed associations might be accounted for by remitted depression status, associations were re-run accounting for history of depression. In the model examining total number of events, the contribution of family environment on baseline PHQ-9 scores was no longer significant (b=−.02, SE=.02, p=.37), but number of stressful events continued to significantly predict higher scores over time (b=.05, SE=.02, p=.01), presented in Figure 3. In the model examining disruption associated with stressful events, neither family environment nor disruption were related to baseline scores (b=−.01, SE=.02, p=.49; b=.12, SE=.08, p=.16, respectively), suggesting that those initial associations may be due to differences associated with remitted depression. Full results are presented in Table 3.
Figure 3. Association Between Number of Stressful Life Events at Baseline and PHQ Scores Over Time.
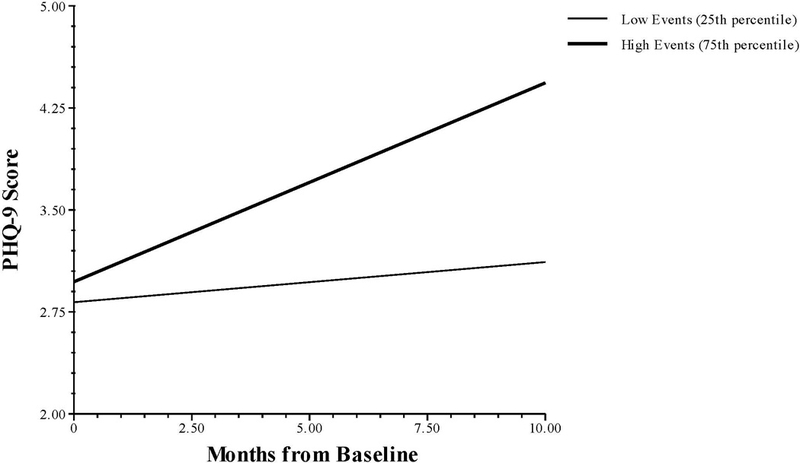
Note. Graph presents results of association between number of events and time since baseline for PHQ scores holding all other variables at their means.
Table 3.
Results of Multilevel Model Predicting PHQ-9 Scores Over Time, Covarying Depression Group
| Fixed Effect | Coefficient | SE | p |
|---|---|---|---|
| Model including Number of Stressful Life Events | |||
| For Intercept (Baseline), π0 | |||
| Intercept, β00 | 1.85 | 0.68 | 0.01 |
| Age, β01 | 0.19 | 0.34 | 0.59 |
| Education, β02 | −0.25 | 0.44 | 0.47 |
| Minority Status, β03 | −0.14 | 0.77 | 0.84 |
| Female, β04 | −0.06 | 0.77 | 0.94 |
| Depression Group, β05 | 2.44 | 0.84 | <0.01 |
| Family Environment, β06 | −0.02 | 0.02 | 0.37 |
| Stressful Events, β07 | 0.00 | 0.16 | 0.99 |
| Family x Events, β08 | 0.00 | 0.01 | 0.97 |
| For Time slope, π1 | |||
| Intercept, β10 | 0.05 | 0.10 | 0.59 |
| Age, β11 | −0.09 | 0.05 | 0.07 |
| Education, β12 | 0.14 | 0.06 | 0.02 |
| Minority Status, β13 | 0.05 | 0.11 | 0.68 |
| Female, β14 | −0.02 | 0.10 | 0.83 |
| Depression Group, β15 | −0.01 | 0.12 | 0.95 |
| Family Environment, β16 | 0.00 | 0.00 | 0.73 |
| Stressful Events, β17 | 0.05 | 0.02 | 0.01 |
| Family x Events, β18 | 0.00 | 0.00 | 0.89 |
| Model including Disruption from Stressful Life Events | |||
| For Intercept (Baseline), π0 | |||
| Intercept, β00 | 2.04 | 0.07 | 0.01 |
| Age, β01 | 0.22 | 0.34 | 0.53 |
| Education, β02 | −0.29 | 0.34 | 0.40 |
| Minority Status, β03 | −0.11 | 0.69 | 0.87 |
| Female, β04 | −0.13 | 0.78 | 0.87 |
| Depression Group, β05 | 2.23 | 0.91 | <0.01 |
| Family Environment, β06 | −0.01 | 0.02 | 0.49 |
| Disruption from Events, β07 | 0.12 | 0.08 | 0.16 |
| Family x Disruption, β08 | 0.00 | 0.00 | 0.68 |
| For Time slope, π1 | |||
| Intercept, β10 | 0.01 | 0.11 | 0.92 |
| Age, β11 | −0.10 | 0.05 | 0.04 |
| Education, β12 | 0.17 | 0.06 | 0.01 |
| Minority Status, β13 | 0.06 | 0.13 | 0.65 |
| Female, β14 | −0.02 | 0.11 | 0.84 |
| Depression Group, β15 | −0.04 | 0.13 | 0.72 |
| Family Environment, β16 | 0.00 | 0.00 | 0.64 |
| Disruption from Events, β17 | 0.01 | 0.01 | 0.47 |
| Family x Disruption, β18 | 0.00 | 0.00 | 0.38 |
Exploratory Analyses: Symptom Profiles Associated with Family Environment Ratings
Given that differences in the associations between family environment ratings were more robustly predictive of BDI scores than PHQ-9 scores, we conducted post-hoc analyses to see whether family environment ratings were more strongly associated with constructs assessed on the BDI than the PHQ-9, namely, cognitive features of depression. After using a Bonferroni adjustment for multiple comparison (changing significance to p<.002), family environment was significantly associated with the items regarding guilty feelings (r=−.37, p<.001), self-dislike (r=−.37, p<.001), and self-criticalness (r=−.35, p<.001). Of note, these items reflect cognitive features of depression, which are largely not assessed on the PHQ-9. Correlations for all items are presented in Table 4.
Table 4.
Bivariate correlations between Family Environment score and BDI items
| BDI Item Construct |
Pearson correlation with Family Environment |
p-value |
|---|---|---|
| Sadness | −.06 | .57 |
| Pessimism | −.22 | .03 |
| Past Failure | −.27 | <.01 |
| Loss of Pleasure | −.27 | <.01 |
| Guilty Feelings | −.37 | <.001* |
| Punishment Feelings | −.30 | <.01 |
| Self-Dislike | −.37 | <.001* |
| Self-Criticalness | −.35 | <.001* |
| Suicidal Ideation | −.21 | .04 |
| Crying | −.01 | .93 |
| Agitation | −.23 | .03 |
| Loss of Interest | −.31 | <.01 |
| Indecisiveness | −.24 | .02 |
| Worthlessness | −.14 | .18 |
| Loss of Energy | −.20 | .06 |
| Changes in Sleep | −.12 | .24 |
| Irritability | −.22 | .03 |
| Appetite | −.27 | <.01 |
| Concentration | −.23 | .02 |
| Tiredness | −.26 | .01 |
| Diminished Libido | −.05 | .63 |
indicates statistical significance after Bonferroni adjustment
To examine further support for the possibility that family environment may particularly relate to cognitive features of depression, prior regression models were re-run predicting the Cognitive and Noncognitive subscales of the BDI separately. Using either the number of stressful life events or disruption due to life events as an indicator of life stress, cognitive symptoms of depression were significantly predicted by family environment, life stress, and their interaction, as displayed in Table 5. Indeed, the model including number of life events accounted for 37% of the variance in Cognitive symptom scores, while the model including disruption due to life events accounted for 52% of the variance. Covarying for group membership did not alter the pattern of results. In contrast, noncognitive symptoms of depression measured on the BDI showed significant main effects of both family environment and life stress (using either indicator), but no interactive effect. The effect of family environment on noncognitive symptoms was no longer significant once controlling for depression history group membership. Notably, this pattern for noncognitive symptoms roughly parallels findings for the PHQ-9, albeit using cross-sectional, rather than longitudinal, data.
Table 5.
Multiple regression results predicting Cognitive and Noncognitive symptom subscales of the BDI.
| Predictor variable | R | R2 | F | Sig. | b | SE | p |
|---|---|---|---|---|---|---|---|
| Model Cognitive with Number Stressful Events |
.61 | .40 | 6.44 | <.001 | |||
| Age | −.30 | .29 | .31 | ||||
| Education | .54 | .33 | .10 | ||||
| Minority Status | −.01 | .59 | .99 | ||||
| Female | −.54 | .69 | .36 | ||||
| Depression Group | .88 | .64 | .17 | ||||
| Family Environment | −.04 | .02 | <.01 | ||||
| Stressful Events | .37 | .11 | <.01 | ||||
| Family x Stressful Events | −.02 | .01 | <.01 | ||||
| Model Cognitive with Disruption from Events |
.73 | .53 | 12.18 | <.001 | |||
| Age | −.22 | .25 | .39 | ||||
| Education | .46 | .28 | .11 | ||||
| Minority Status | .05 | .51 | .93 | ||||
| Female | −.68 | .51 | .19 | ||||
| Depression Group | .61 | .55 | .28 | ||||
| Family Environment | −.03 | .01 | .02 | ||||
| Disruption from Events | .26 | .05 | <.01 | ||||
| Family x Disruption | −.01 | .00 | <.01 | ||||
| Model Noncognitive with Number Stressful Events |
.52 | .27 | 4.00 | <.001 | |||
| Age | .27 | .33 | .16 | ||||
| Education | −.34 | .37 | .36 | ||||
| Minority Status | −.05 | .67 | .94 | ||||
| Female | −.16 | .67 | .81 | ||||
| Depression Group | 1.75 | .73 | .02 | ||||
| Family Environment | −.03 | .02 | .10 | ||||
| Stressful Events | .27 | .12 | .03 | ||||
| Family x Stressful Events | .00 | .01 | .88 | ||||
| Model Noncognitive with Disruption from Events |
.59 | .38 | 5.83 | <.001 | |||
| Age | .50 | .311 | .12 | ||||
| Education | −.36 | .35 | .31 | ||||
| Minority Status | .03 | .63 | .97 | ||||
| Female | −.26 | .63 | .68 | ||||
| Depression Group | 1.513 | .68 | .03 | ||||
| Family Environment | −.02 | .02 | .30 | ||||
| Disruption from Events | .26 | .07 | <.01 | ||||
| Family x Disruption | .001 | .001 | .92 |
Discussion
The current study provides qualified support for the role of positive family environments in buffering individuals from depressive symptoms in response to life stress. Specifically, we found that individuals who reported better family environments showed weaker associations between the number of or amount of disruption from stressful life events and their depressive symptoms at baseline, consistent with a social buffering hypothesis (Cohen & Wills, 1985; Wilcox, 1981). Notably, these associations were evident in a sample of individuals in emerging adulthood, a developmental period typically characterized by the diminished influence of families relative to increasing emphasis on autonomy and peer relationships (Fraley & Davis, 1997; Roisman, Masten, & Coatsworth, 2004). Furthermore, these associations were largely independent of any effects associated with a prior history of depression, suggesting that buffering processes can operate for individuals across the spectrum of vulnerability. When examining symptoms over 12-months using a different self-report measure of depression, however, this buffering pattern did not emerge. Rather, a more positive family environment predicted fewer symptoms on the PHQ at baseline, but did not predict the trajectory of depressive symptoms, and these effects appeared to be accounted for by whether an individual had a history of depression. In contrast, the number of stressful life events experienced did not predict symptoms at baseline, but did predict increases in depressive symptoms over time. Although similar associations were present for models examining disruption due to life stress, these associations were not significant once accounting for depression history.
There are several possible explanations for the diverging findings at baseline versus longitudinal assessments. One possibility is that differences are due to the unique composition of items on the Beck Depression Inventory (collected only at baseline) versus the PHQ-9 (collected at all time points). Although both measures include the symptoms outlined in the DSM-IV criteria for major depression, the BDI devotes significantly more attention to cognitive features of depression, such as self-criticism or feelings of guilt. Indeed, it is precisely these cognitive aspects that may be particularly influenced by an individual’s family environment. For example, Plunkett et al. (2007) demonstrated that parental support had a significant indirect effect on children’s depressive symptoms by affecting children’s self-esteem. Similarly, Garber, Robinson, & Valentiner (1997) found that the effects of maternal acceptance and maternal control on children’s depressive symptoms were partially mediated by children’s self-worth. Indeed, our post-hoc examination of associations between family environment and individual items on the BDI, as well as in regression analyses predicting Cognitive versus Noncognitive symptom subscales, found that associations were most robust for cognitive symptoms. Although further work is need, this pattern is consistent with the proposal that parenting may contribute to children developing important schemas for themselves that in turn may leave them more or less vulnerable to depressive processes. Specifically, more adaptable and cohesive families may support children in developing resilient views of themselves that then protect them when they experience stressful life events. Moreover, through effects on cognitive processes, it would not be surprising that family environments could continue to exert effects on offspring even into adulthood.
An alternative explanation for the different patterns of findings is that associations between family environment, stress, and depressive symptoms depend primarily on concurrent functioning. Thus, the effects of family and stress measured at baseline on depressive symptoms would dissipate overtime, supplanted by more recent stressful experiences or changes in family relationship. This is consistent with results of work by Galambos, Barker, and Krahn (2006), which revealed that conflict with parents predicted young adults’ self-esteem at baseline, but not their trajectory of self-esteem over time. Of course, it may also be the case that the baseline associations in the current study reflect state-dependent functioning that simultaneously biases the perceptions of family life, stress, and depressive symptoms. However, the symptom load in these adolescents with remitted depression was quite low. In a related manner, longitudinal work by Moos, Cronkite, and Moos (1998) found no evidence for depressive symptoms predicting decrements in social relationships, but did find support for changes in family functioning predicting changes in depression. For these reasons, it is less likely that our patterns of results are due to reversed direction of effects; however, further work is needed to investigate that possibility.
There are important limitations to acknowledge in the current work. First, responses to the BDI were obtained only at baseline, whereas the PHQ-9 was utilized at each time point. This reliance solely on the PHQ-9 for longitudinal assessment of depressive symptoms was done to minimize participant burden; however, as noted earlier, this makes our findings for baseline versus longitudinal assessments difficult to interpret, particularly with the stronger effects observed for cognitive symptoms (only in BDI). Another limitation is that family environment and life stress experiences were assessed only at baseline. Measures of these constructs over time would allow for an analysis of the role of intervening stressful life events or changes in family functioning on depressive symptoms and would also allow for an understanding of the directionality of effects. Additionally, although history of depression and current remission status were determined by clinical interview (including a corroborative interview with a parent to determine group membership), all measures in the current study were assessed using self-report questionnaires, leading to the possibility that associations are enhanced due to shared method variance or reporter bias. Lastly, it is important to note that the participant’s family-of-origin was never specified in the measure of family environment. However, given the age and educational status of the participants, it is likely that the overwhelming majority of respondents were reporting on the cohesion and adaptability of their relationships with their parents and siblings, rather than with their spouse or children of their own. Future work would benefit from greater clarity around focal relationships.
In the context of these limitations, the current work raises several important questions for future work. For example, if positive family environments help impart healthier self-views in individuals, when do these effects first emerge and how long might they last once offspring enter adulthood? As many individuals marry and begin families of their own, it would be worthwhile to determine when cognitive processes that were shaped by their own childhood relationships cede to marital and caretaking dynamics. It is possible that emerging adulthood represents a key inflection point for these interpersonal influences. Similarly, direct assessment of cognitive factors holds the potential to illuminate key mediators of the proposed stress-buffering function on family relationships in emerging adults. Another question is how families may contribute to depression remission and relapse. The current work suggests that family processes do not seem to operate fundamentally differently in individuals with a history of remitted depression versus those without. However, it is possible that individuals who have achieved remission—compared to those who continue to be depressed—have more supportive families that facilitate recovery. A comparison of these processes across never-depressed, remitted depressed, and actively depressed individuals would be fruitful. Finally, it is unclear what other factors in the lives of young adults contribute to the variance in depressive symptoms not explained by life stress and family environment. Given the age and other demographic features of participants in our study, it is likely that developmentally-salient experiences within other types of social relationships (such as friends, classmates, and romantic partners) or within academic or professional pursuits may also contribute to depressive symptoms in this age group. Moreover, intrapersonal factors (neuroticism, reward processing, drive) can also play a critical role in buffering the effects of stress.
In summary, the current work provides qualified support for the possibility that family environments may buffer individuals from the negative sequelae of stressful life events, even into adulthood and regardless of whether an individual has a history of depression. If family environments continue to affect the mental health outcomes through influences on self-evaluative processes, then this has important clinical implications for the treatment of depression during emerging adulthood. Given that most university students and young adults in these areas live away from home, parents and siblings likely have little involvement in the recovery process even when individuals do seek treatment for symptoms. However, if the family environment is a source of positive support for a patient, then efforts to include families in treatment should be pursued, such as through telemedicine or coaching the patient on how to best access family help. In contrast, if the family environment is a detrimental force on patient functioning, then targeting the cognitive processes most vulnerable to negative influence may be particularly effective in reducing symptoms. Furthermore, given that our observed patterns were true regardless of whether participants had no history of depression or had remitted depression, this suggests that similar family processes might be considered and included within preventative efforts. With these implications in mind, the current work affirms the importance of family experiences for mental health symptomatology in emerging adults with and without vulnerability to depression.
Acknowledgments
Grant funding was provided by the National Institute of Mental Health (NIMH), RO1 091811: Identification of Neurobiological Intermediate Phenotypes in Major Depressive Disorder (MINDS), 07/17/2015, Scott A. Langenecker, PhD.
Footnotes
There were also no significant three-way interaction effects of family environment, life stress (number of events or disruption), and group membership predicting BDI or PHQ-9 scores (at baseline or over time).
The ideas and analyses appearing in the current manuscript have not been previously disseminated, including at conferences or on listservs or websites.
Contributor Information
Erika M. Manczak, Department of Psychiatry and Behavioral Sciences, Stanford University
Kristy A. Skerrett, Department of Psychiatry, University of Illinois-Chicago
Laura B. Gabriel, Department of Psychiatry, University of Illinois-Chicago and Department of Psychiatry, University of Michigan
Kelly A. Ryan, Department of Psychiatry, University of Michigan
Scott A. Langenecker, Department of Psychiatry, University of Illinois-Chicago
References:
- Aben I, Verhey F, Lousberg R, Lodder J, & Honig A (2011). Validity of the Beck Depression Inventory, Hospital Anxiety And Depression Scale, SCL-90, and Hamilton Depression Rating Scale as screening instruments for depression in stroke patients. Psychosomatics, 43(5), 386–393. [DOI] [PubMed] [Google Scholar]
- Angst J, Angst F, & Stassen HH (1999). Suicide risk in patients with major depressive disorder. Journal of Clinical Psychiatry, 60, 57–62. [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bouma EMC, Ormel J, Verhulst FC, & Oldehinkel AJ (2008). Stressful life events and depressive problems in early adolescent boys and girls: The influence of parental depression, temperament and family environment. Journal of Affective Disorders, 105(1–3), 185–193. [DOI] [PubMed] [Google Scholar]
- Brody GH, Murry VM, McNair L, Chen Y-F, Gibbons F, Gerrard M, & Wills TA (2005). Linking changes in parenting to parent–child relationship quality and youth self‐control: The Strong African American Families Program. Journal of Research …, 15(1), 47–69. [Google Scholar]
- Chilcoat HD, & Breslau N (1997). Does psychiatric history bias mothers’ reports? An application of a new analytic approach. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 971–979. [DOI] [PubMed] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357. [PubMed] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, et al. (2010). Coping and parenting: Mediators of 12-month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology, 78(5), 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, & Dishion TJ (2008). Reducing depression among at-risk early adolescents: Three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology, 22(4), 574–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLay D, Hafen CA, Cunha JM, Weber LND, & Laursen B (2013). Perceptions of parental support buffer against depression for Brazilian youth with interpersonal difficulties. International Journal of Behavioral Development, 37(1), 29–34. [Google Scholar]
- Epkins CC, & Harper SL (2016). Mothers’ and fathers’ parental warmth, hostility/rejection/neglect, and behavioral control: Specific and unique relations with parents’ depression versus anxiety symptoms. Parenting, 16(2), 125–145. [Google Scholar]
- Fletcher JM (2008). Adolescent depression: Diagnosis, treatment, and educational attainment. Health Economics, 17(11), 1215–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraley RC, & Davis KE (1997). Attachment formation and transfer in young adults’ close friendships and romantic relationships. Personality and Individual Differences, 4, 131–144. [Google Scholar]
- Galambos NL, Barker ET, & Krahn HJ (2006). Depression, self-esteem, and anger in emerging adulthood: Seven-year trajectories. Developmental Psychology, 42(2), 350–365. [DOI] [PubMed] [Google Scholar]
- Garber J, Robinson N, & Valentiner D (1997). The relation between parenting and adolescent depression self-worth as a mediator. Journal of Adolescent Research, 12(1), 12–33. [Google Scholar]
- Ge X, Natsuaki MN, Neiderhiser JM, & Reiss D (2009). The longitudinal effects of stressful life events on adolescent depression are buffered by parent–child closeness. Development and Psychopathology, 21(02), 621. [DOI] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry, 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Shih JH, & Brennan PA (2004). Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology, 72(3), 511–522. [DOI] [PubMed] [Google Scholar]
- Herman-Stahl M, & Petersen AC (1996). The protective role of coping and social resources for depressive symptoms among young adolescents. Journal of Youth and Adolescence, 25(6), 733–753. [Google Scholar]
- Judd LL (1997). The clinical course of unipolar major depressive disorders. Archives of General Psychiatry, 50, 989–991. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merkangas K, & Walter E (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ‐9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levens SM, Elrahal F, & Sagui SJ (2016). The role of family support and perceived stress reactivity in predicting depression in college freshman. Journal of Social and Clinical Psychology, 35(4), 342–355. [Google Scholar]
- Löwe B, Kroenke K, Herzog W, & Gräfe K (2004). Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). Journal of Affective Disorders, 81(1), 61–66. [DOI] [PubMed] [Google Scholar]
- Maxwell ME (1992). Family Interview for Genetic Studies (FIGS): A manual for FIGS. Clinical Neurogenetics Branch, Intramural, NIMH, Bethesda, MD. [Google Scholar]
- McKee SA, Maciejewski PK, Falba T, & Mazure CM (2003). Sex differences in the effects of stressful life events on changes in smoking status. Addiction, 98, 847–855. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, & Weisz JR (2007). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27(2), 155–172. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, & Poulton R (2009). How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine, 40(06), 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM, & Harkness KL (2005). Life Stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review, 112(2), 417–445. [DOI] [PubMed] [Google Scholar]
- Moos RH, Cronkite RC, & Moos BS (1998). The long-term interplay between family and extrafamily resources and depression. Journal of Family Psychology, 12(3), 326–343. [DOI] [PubMed] [Google Scholar]
- Moreira JFG, & Telzer EH (2015). Changes in family cohesion and links to depression during the college transition. Journal of Adolescence, 43(C), 72–82. [DOI] [PubMed] [Google Scholar]
- Newcomb MD, Huba GJ, & Bentler PM (1981). A multidimensional assessment of stressful life events among adolescents: Derivation and correlates. Journal of Health and Social Behavior, 22(4), 400–415. [Google Scholar]
- Nurnberger JI, Blehar MC, Kaufmann CA, York-Cooler C, Simpson SG, Harkavy-Friedman J, et al. (1994). Diagnostic interview for genetic studies: rationale, unique features, and training. Archives of General Psychiatry, 51, 849–859. [DOI] [PubMed] [Google Scholar]
- Olson DHL, Portner J, Bell R, & Tiesel JW (1991). Faces II
- Olson DH, McCubbin HI, Barnes HL, Larsen A, Muxen M, & Wilson M (1989). Families: What Makes Them Work Los Angeles, CA: Sage Publishing. [Google Scholar]
- Penninx B, Milaneschi Y, Lamers F, & Vogelzangs N (2013). Understanding the somatic consequences of depression: biological mechanisms and the role of depression symptom profile. BMC Medicine, 11(129), 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plunkett SW, Henry CS, Robinson LC, Behnke A, & Falcon PC III. (2007). Adolescent perceptions of parental behaviors, adolescent self-esteem, and adolescent depressed mood. Journal of Child and Family Studies, 16(6), 760–772. [Google Scholar]
- Repetti RL, Taylor SE, & Seeman T (2002). Risky families: Family social environments and mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. [PubMed] [Google Scholar]
- Restifo K, & Bögels S (2009). Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review, 29(4), 294–316. [DOI] [PubMed] [Google Scholar]
- Risch N, Herrell R, Lehner T, Liang K, & Merikangas KR (2009). Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression. JAMA, 301(23), 2462–2471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roisman GI, Masten AS, & Coatsworth JD (2004). Salient and emerging developmental tasks in the transition to adulthood. Child Development, 75(1), 123–133. [DOI] [PubMed] [Google Scholar]
- Saunders EFH, Nazir R, Kamali M, Ryan KA, Evans S, Langenecker S, et al. (2014). Gender differences, clinical correlates, and longitudinal outcome of bipolar disorder with comorbid migraine. The Journal of Clinical Psychiatry, 75(05), 512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeber L, Hops H, & Davis B (2001). Family processes in adolescent depression. Clinical Child and Family Psychology Review, 4(1), 19–35. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, & Davis B (1997). Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology, 25(4), 333–344. [DOI] [PubMed] [Google Scholar]
- Üstün TB, Ayuso-Mateos JL, & Chatterji S (2004). Global burden of depressive disorders in the year 2000. The British Journal of Psychiatry, 184, 386–392. [DOI] [PubMed] [Google Scholar]
- Wilcox BL (1981). Social support, life stress, and psychological adjustment: A test of the buffering hypothesis. American Journal of Community Psychology, 9(4), 371–386. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2009). Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks, 1–70.


