Abstract
Background
Tobacco and alcohol consumption are known causes of cancer. We set out to estimate the absolute numbers and proportions of cancer attributable to smoking and high alcohol consumption in Germany in 2018.
Methods
Numbers and proportions (population-attributable fractions, PAF) were calculated by sex and age group for ages 35 to 84 years based on population projections, national cancer incidence and exposure data, and published relative risks.
Results
For the year 2018 we estimated the smoking-attributable cancer burden to be 85 072 cases (men 58 760, women 26 312), corresponding to 19% of all incident cancers. The highest PAF was seen for lung cancer: 89% of male and 83% of female lung cancer cases are attributable to smoking. The cancer burden attributable to high alcohol consumption was estimated to be 9588 (men 8117, women 1471) cases (2% of all incident cancers). The highest PAF were observed for cancer of the oral cavity and pharynx (men 34%, women 6%) and squamous cell carcinoma of the esophagus (men 30%; women 5%).
Conclusions
A considerable proportion of cancer cases are attributable to smoking and high alcohol consumption. More rigorous prevention efforts are required to achieve significant reductions in the prevalence of these risk factors and the attributable cancer burden.
Health authorities in the USA recognized smoking as a cause of lung cancer and laryngeal cancer as early as in 1964. Since then, evidence of a causal link between smoking and several other cancer sites has accumulated, and today smoking is known as the leading avoidable cancer risk factor, causally associated with 12 different types of cancer (1).
Alcohol consumption was first concluded to be carcinogenic to humans by the International Agency for Research on Cancer (IARC) in 1988 (2). According to the Continuous Update Project (CUP) of the World Cancer Research Fund (WCRF), alcohol consumption increases the risk for six types of cancer (3).
Our aim in carrying out this study was to provide projections of the cancer burden attributable to the risk factors smoking and high alcohol consumption in Germany for the year 2018. Due to a lack of epidemiological data on the role of lifestyle cancer risk factors at young and very old ages, we restricted our estimates to the age range of 35 to 84 years.
Methods
Projection of cancer cases
We estimated the number of site-specific cancers for each age and sex group for the year 2018 by multiplying the most recent age- and sex-specific incidence rates available from the German cancer registries (for the year 2014 [4]), by age- and sex-specific population projections for Germany for the year 2018 (5) (eTables 1 and 2).
Estimation of the smoking-attributable cancer burden
The strong association between smoking and lung cancer allows estimating the smoking-attributable fraction of lung cancer by means of an established indirect method (6), without having to make assumptions about latency periods. This method requires knowledge of lung cancer rates in never smokers and of relative risks (RR) of cancers causally linked to smoking, for smokers compared to never smokers. Such data were not available for Germany, so we used published pooled data from large contemporary cohorts provided by the American Cancer Society for the period 2000 to 2010: age- and sex-specific lung cancer mortality rates per 100 000 persons were reported by Thun et al. (14), and multivariably adjusted age- and sex-specific relative mortality risks for lung cancer and other smoking-caused cancers combined, derived from the same cohorts, were published in a recent report by US health authorities (1).
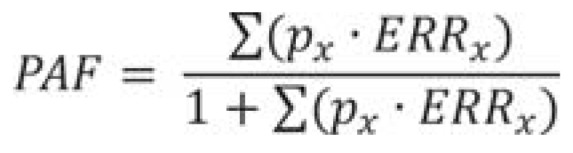
By applying the age- and sex-specific lung cancer rates in never smokers to the age- and sex-specific population projections for Germany for the year 2018, we calculated the number of cancer cases that would be expected in the absence of smoking as a risk factor. The number of lung cancer cases attributable to smoking was then calculated by subtracting these cases from the overall number projected for 2018. For other cancers caused by smoking, data on rates among never smokers were not available, so we used the commonly applied Levin’s formula for the calculation of population-attributable fractions (PAF) (5):
where px is the proportion of the population at exposure level (here: prevalence of ever smokers) ERRx and is the excess relative risk associated with exposure level x calculated as (RR –1). Here, we used not the observed smoking prevalence from a population survey, but rather a notional (theoretical) prevalence of ever smoking in the German population that was derived by inserting the calculated attributable fractions of lung cancer and the relative risks for lung cancer in smokers in the above formula and solving it for px separately for each sex and age group. This notional prevalence can be regarded as the ever smoking prevalence that would be necessary in the German population to produce the cancer incidence in 2018 if the relative risks of the American cohorts pertained (15).
Estimation of the alcohol-attributable cancer burden
To provide estimates of cancer cases caused by excess alcohol intake, PAF were calculated considering cancers determined as causally related to consumption of alcohol by the IARC (16). Data on the prevalence of alcohol consumption in Germany were obtained from the German Health Interview and Examination Survey for Adults for the period 2008 to 2011 (DEGS1 2008–2011) (17).
Estimation of the average alcohol consumption in the population was based on a validated food frequency questionnaire (18). Self-reported information on amount and frequency of alcohol consumption was combined and converted into average grams of pure alcohol per day (eSupplement A). For PAF estimation, alcohol consumption was categorized into “below recommended limits” (<10 g pure alcohol per day in women or <20 g pure alcohol per day in men) and “above recommended limits” (=10 g/d in women or =20 g/d in men) (19).
RR estimates concerning the association between alcohol consumption and site-specific cancer incidence were taken from meta-analyses of cohort studies, conducted by the WCRF, when available. The mean amount of pure alcohol consumed in grams per day (g/d) by those who stayed within the recommended limits was defined as the optimum exposure level.
For each age and sex group, we computed the PAF associated with the absolute difference of the mean exposure level for those with alcohol consumption above versus those with alcohol consumption at or below recommended limits using the above-mentioned Levin’s formula (eSupplement B).
As in similar previous studies, we assumed a 10-year latency period between exposure and cancer incidence. By applying the age- and sex-specific PAF to the projected cancer incidences for Germany for the year 2018, we calculated the number of cancer cases that would be expected if individuals with alcohol consumption above recommended limits reduced their alcohol intake to the levels of those who adhere to recommended limits.
Sensitivity analyses
Methods of sensitivity analyses are described in eSupplement C.
Results
Smoking-attributable cancer burden
In most age groups the risk for lung cancer in smokers is around 20 or more times higher than in never smokers, and for other cancers about twice as high (eTable 3). While we projected 52 914 lung cancer cases in 2018 in the German population aged 35 to 84 (men 34 410, women 18 504), only 7056 cases were projected to occur in the absence of smoking (men 3962, women 3094) (table 1). Accordingly, 89% of lung cancer cases among men and 83% among women would be attributable to smoking (overall 45 858 cases; men 30 448, women 15 410).
Table 1. Lung cancer cases attributable to smoking by sex and age group, Germany, 2018.
| Age (years) | Lung cancer cases projected for 2018 | Lung cancer cases expected in absence of smoking in 2018 | Smoking-attributable lung cancer cases | PAF (%) |
| Men | ||||
| 35–54 | 2890 | 434 | 2456 | 85 |
| 55–64 | 9136 | 775 | 8361 | 92 |
| 65–74 | 11 492 | 926 | 10 566 | 92 |
| 75–84 | 10 982 | 1827 | 9065 | 83 |
| Total | 34 410 | 3962 | 30 448 | 88 |
| Women | ||||
| 35–54 | 2268 | 423 | 1845 | 81 |
| 55–64 | 5358 | 478 | 4880 | 91 |
| 65–74 | 6000 | 785 | 5215 | 87 |
| 75–84 | 4878 | 1409 | 3469 | 71 |
| Total | 18 504 | 3095 | 15 409 | 83 |
PAF, population-attributable fraction
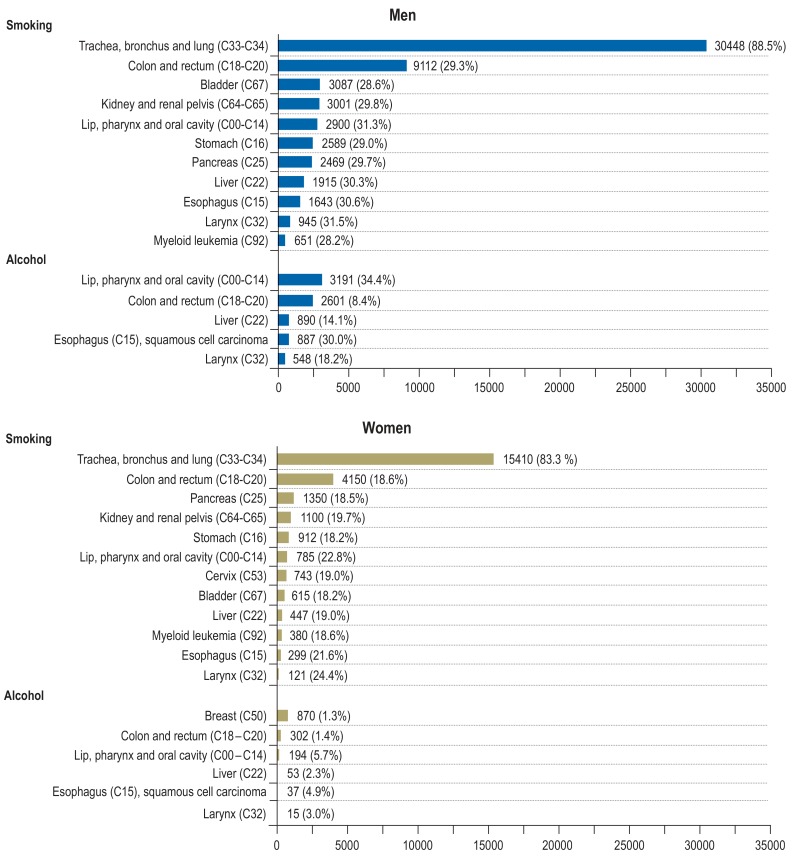
For all other cancers, the PAF was around 30% in men and 20% in women, which translated to 39 214 cancer cases (men 28 312, women 10 902) (Figure, eTables 4 and 5). Overall, according to our estimates for 2018, 85 072 out of 440 373 projected cancer cases (eTables 4 and 5), i.e., 19.3%, would be attributable to smoking (men 58 760 cases, 24.7%; women 26 312 cases, 13.0%).
Figure.
The sensitivity analysis based on empirical smoking prevalence from DEGS1 2008–2011 (eTable 6) yielded a very similar estimate of 86 000 smoking-attributable cancer cases (eTable 7).
Alcohol-attributable cancer burden
According to DEGS1 2008–2011, 18.7% of men and 12.9% of women aged 25 to 74 years were estimated to drink alcohol at levels above the recommended limits, with an average intake of 44.6 g/d for men and 20.2 g/d for women (table 2). Dose–response meta-analyses of alcohol consumption and site-specific cancer risk found risk increases of 7–29% per 10 g/d (for the larynx, per 12.5 g/d) increase in pure alcohol intake (eFigure).
Table 2. Prevalence of alcohol consumption below and above recommended limits according to the DEGS1 survey (2008–2011): mean pure alcohol intake in grams per day among men and women aged 25–74 years.
| Prevalence (%) and mean (m) for alcohol consumption below and above recommended limits | ||||||||||||
| 25–34 years | 35–44 years | 45–54 years | 55–64 years | 65–74 years | Total | |||||||
| Exposure | % | m | % | m | % | m | % | m | % | m | % | m |
| Men | ||||||||||||
| Below recommended limits (<20 g/d) | 86 | 6.8 | 85 | 5.6 | 78 | 6.2 | 81 | 6.3 | 76 | 5.7 | 81 | 6.1 |
| Above recommended limits (≥ 20 g/d) | 14 | 57.7 | 15 | 38.4 | 22 | 47.3 | 19 | 38.0 | 24 | 43.2 | 19 | 44.6 |
| Women | ||||||||||||
| Below recommended limits (<10 g/d) | 89 | 2.3 | 86 | 2.3 | 88 | 2.4 | 83 | 2.2 | 90 | 1.9 | 87 | 2.2 |
| Above recommended limits (≥ 10 g/d) | 11 | 16.9 | 14 | 23.3 | 12 | 18.8 | 17 | 20.8 | 10 | 19.8 | 13 | 20.2 |
The greatest PAF for alcohol consumption were estimated for cancer of the oral cavity and pharynx (men 34%, women 6%) and squamous cell carcinoma of the esophagus (men 30%, women 5%). The attributable cancer burden was greater among men than women, with much higher PAF for all cancer sites. Overall, PAF ranged from 8% to 34% in men and from 1% to 6% in women, which in sum translated to 9588 cancer cases (men 8177, women 1471), corresponding to 2.2% (men 3.4%, women 0.7%) of all cancer cases (eTables 8 and 9). The cancer sites contributing most to this excess were cancer of the oral cavity and pharynx in men, with 3191 cancer cases, and breast cancer in women, with 870 cases.
Sensitivity analyses using the 95% confidence limits of risk estimates on the association of alcohol and cancer indicated a potential range of 7000 to 12 300 cancer cases attributable to alcohol (eTable 10).
Discussion
Of around 440 000 cancer cases expected in 2018, about 85 000 and 9500 cases are estimated to be attributable to smoking and alcohol consumption, respectively, which corresponds to 19% and 2% of cancers. Especially lung cancer is largely attributable to smoking, with a PAF of 80 to 90%. Generally, the attributable cancer burden was estimated to be considerably greater among men, both in relative and in absolute terms.
Smoking-attributable cancer burden
Tobacco smoke is a complex mixture of more than 5000 chemicals, including carcinogenic substances, with no risk-free level of exposure (20). The health consequences of the cumulative exposure to carcinogens of tobacco smoke are enormous, particularly for the lung but also for other organs (1). Our estimations of the smoking-attributable cancer burden are based on expected cancer incidence in the complete absence of smoking. It is, however, important to keep in mind that even if smoking were eliminated today, it would take decades until no further cancer caused by smoking occurred. Former smokers still have an increased risk of cancer, even though the excess risk declines with increasing time since smoking cessation (21).
The total number of smoking-attributable cancer cases was estimated to be more than twice as high in men than in women, which mostly reflects the higher prevalence of smoking among men, especially in recent decades (22, 23). Our results are quite consistent with a previous study for Germany, which estimated 72 208 cancer cases to be attributable to smoking in 2008; 55 057 cases in men and 17 151 cases in women. Our estimates are slightly higher for men (58 760 vs. 55 057), and markedly higher for women (26 312 vs. 17 151) (24). This might be due to our use of more recent risk estimates, as sex differences in relative risks of smoking have been decreasing over time and are now rather negligible (14).
We found that overall, 19% of cancer cases are attributable to smoking, which is substantially higher than comparable estimates for England (14.7%, [10]) or Australia (13.4%, [11]), two countries that have achieved strong declines in smoking in recent years through comprehensive tobacco control strategies (25, 26).
For Germany, a modeling study demonstrated that significant reductions in smoking prevalence and the attributable disease burden could be achieved by strengthening tobacco control policies in line with recommendations of the World Health Organization, such as raising taxes, banning tobacco advertising, and enhancing cessation support (27).
Alcohol-attributable cancer burden
The major constituent of alcoholic beverages, ethanol, and its metabolite acetaldehyde have been classified as carcinogenic to humans (28). While there are more cancer sites causally associated with alcohol consumption in women, the total number of alcohol-attributable cancer cases was estimated to be more than five times higher in men than in women. In addition to a higher prevalence of alcohol consumption above the recommended limits among men, the greater average amount of alcohol consumed by men in each age group contributes to this inequality.
Instead of an unrealistic zero exposure (total absence of alcohol consumption), we sought to arrive at an achievable target value by setting the reference exposure level to the mean amount of alcohol consumed by those who adhere to recommended limits. However, it is important to note that there is no safe level of alcohol consumption with regard to cancer risk (29).
Overall, our projections of cancer site-specific PAF and corresponding excess cases are lower than those from a previous study (30), which estimated that approximately 8700 cancer cases among men and 4900 cases among women were attributable to alcohol in Germany in 2010. Our lower estimates can be explained by the fact that we did not consider the cancer burden due to light drinking and used more recent risk estimates from prospective studies.
A study estimating the alcohol-attributable burden of cancer incidence in eight European countries found that PAF varied across countries because of differences in alcohol exposure (31). Results from modeling studies demonstrate that alcohol consumption could be influenced by public health policies and interventions such as pricing and taxation (32).
Strengths and limitations
We provide up-to-date estimates of the cancer burden attributable to smoking and alcohol consumption in Germany, based on the latest relative risk estimates from cohort studies as well as the most recent population projections and cancer registry data. Sensitivity analyses revealed substantial numbers of attributable cancer cases across all scenarios in a comparable range.
Due to a lack of up-to-date risk estimates from prospective cohort studies, we did not consider synergistic interactions between smoking and alcohol consumption, although there is some evidence of such an effect for head and neck cancer (33). For the estimation of the smoking-attributable cancer burden we had to rely on lung cancer rates in never smokers and relative risk estimates from a US population. We also had to use relative risk estimates for cancer mortality from the same population, but these tend to be similar to those for cancer incidence (21).
Furthermore, with respect to the estimation of the alcohol-attributable cancer burden, PAF depend on the reliability of self-reported alcohol drinking and the definition of exposure categories. Potential changes in prevalence of smoking or alcohol consumption over the past 10 years in the considered age groups should be small and therefore not affect our estimates substantially.
When calculating PAF, we restricted our estimates to cancer types with currently sufficient or convincing evidence as stated by pertinent authorities, but new evidence might confirm other causal links in the future. For example, there is evidence that the risk of gastric cancer is associated with increased alcohol consumption, but this association was observed only for high alcohol intakes (=45 g/d) (34). A causal association between smoking and breast cancer has also been postulated (35). Given these limitations, our PAF and cancer burden projections are likely to be underestimates and can thus be considered conservative.
Conclusion
Of around 440 000 cancer cases to be expected in Germany in 2018, approximately 85 000 and 9500 cases are estimated to be attributable to smoking and alcohol consumption, respectively, corresponding to 19% and 2% of all cancer cases. Given the still significant prevalence of smoking and alcohol consumption in this country, there is huge potential for cancer prevention by intensifying efforts to reduce smoking rates and alcohol use.
Two other articles in this issue of Deutsches Ärzteblatt International present the topics “Cancers Due to Infection and Selected Environmental Factors” and “Cancers Due to Excess Weight, Low Physical Activity and Unhealthy Diet”, respectively (36, 37).
BOX. Population-attributable fraction (PAF).
This concept was developed in the early 1950s and is widely used in epidemiological studies (7, 8). A PAF expresses by what proportion the prevalence or incidence of a disease could be reduced if the whole population were shifted to a more favorable level of a risk factor for that disease. In a seminal article series, Parkin et al. used the PAF concept to estimate the fraction of cancers occurring in the United Kingdom that are attributable to lifestyle and environmental risk factors (9). This was followed by similar work in other countries (e.g., [10, 11]), and we present here for the first time such estimates for Germany.
The limitations and pitfalls in the interpretation of PAF estimates have been described in detail elsewhere (7, 12). One important aspect of this concept is that while the PAF for a single causal risk factor cannot be more than 100%, in the event of shared responsibility of several causes for a disease—as is usually the case for cancer—the PAF of these causes can add up to more than 100% (7, 13). Thus, PAF cannot be simply added up across causes, but can, however, be combined to estimate a joint PAF assuming independence of risk factors (13), as was done for the estimates presented in the article by Gredner et al. in this issue of Deutsches Ärzteblatt International. Even though it would unarguably take several years before reductions in cancer risk factors would lead to reduced cancer incidence, the PAF is nevertheless considered a valuable quantitative appraisal of their population impact (9).
As with all epidemiological models, our PAF estimations are based on assumptions, which may not hold true in all cases. Here, for instance, this applies to the assumption of a 10-year latency period between exposure and cancer incidence, or the assumption of independence of risk factors. However, while all presented results need to be understood as estimates, we are confident that our projections regarding the potential for prevention at population level are reasonably conservative and reflect the best of current knowledge.
Figure.
Estimated number and population-attributable fraction (PAF) of site-specific incident cancer cases attributable to smoking and high alcohol consumption among men and women in Germany for the year 2018.
Key Messages.
We used population-attributable fractions (PAF) to estimate the proportion of cancer incidence attributable to the risk factors smoking and high alcohol consumption.
According to our estimates, around one in five cancer cases is due to smoking and around one in 50 cases is due to high alcohol consumption, pointing to a large potential for prevention.
Although our projections are based on assumptions and epidemiological data that entail some uncertainties, we are confident that they are the best estimates possible on the basis of current knowledge and are reasonably conservative.
Public health policies and factors such as pricing and taxation can play an important role in reducing smoking and high alcohol consumption, and thus in cancer prevention.
Healthcare professionals can contribute to cancer prevention by advising and supporting their patients to quit smoking and reduce alcohol consumption.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Funding:
The study was funded by German Cancer Aid (Deutsche Krebshilfe), grant number 70112097.
References
- 1.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Atlanta (GA): 2014. The health consequences of smoking—50 years of progress: a report of the surgeon general. [PubMed] [Google Scholar]
- 2.International Agency for Research on Cancer. IARC. Lyon: 1988. IARC monographs on the evaluation of carcinogenic risks to humans. Alcohol drinking. [PMC free article] [PubMed] [Google Scholar]
- 3.World Cancer Research Fund International. World Cancer Research Fund International. London: 2017. Summary of global evidence on diet, weight, physical activity & what increases or decreases your risk of cancer. [Google Scholar]
- 4.Robert Koch Institute. German Centre for Cancer Registry Data: Database Query 2017. www.krebsdaten.de/Krebs/DE/Datenbankabfrage/datenbankabfrage_stufe1_node.html (last accessed on 12 December 2017) [Google Scholar]
- 5.Statistisches Bundesamt. www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/VorausberechnungBevoelkerung/BevoelkerungDeutschland2060_5124202159004.pdf;jsessionid=D06F3A9634A843F70E6D0D907E659818.InternetLive1?__blob=publicationFile (last accessed on14 December 2017) Wiesbaden, Germany: Bevölkerung Deutschlands bis 2060 - Ergebnisse der 13. koordinierten Bevölkerungsvorausberechnung. [Google Scholar]
- 6.Peto R, Lopez AD, Boreham J, Thun M, Heath C Jr. Mortality from tobacco in developed countries: indirect estimation from national vital statistics. Lancet. 1992;339:1268–1978. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 7.Greenland S. Concepts and pitfalls in measuring and interpreting attributable fractions, prevented fractions, and causation probabilities. Ann Epidemiol. 2015;25:155–161. doi: 10.1016/j.annepidem.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 8.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9:531–541. [PubMed] [Google Scholar]
- 9.Parkin DM, Boyd L, Walker LC. The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br J Cancer. 2011;105(2):S77–S81. doi: 10.1038/bjc.2011.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brown KF, Rumgay H, Dunlop C, et al. The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer. 2018;118:1130–1141. doi: 10.1038/s41416-018-0029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiteman DC, Webb PM, Green AC, et al. Cancers in Australia in 2010 attributable to modifiable factors: summary and conclusions. Aust N Z J Public Health. 2015;39:477–484. doi: 10.1111/1753-6405.12471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kowall B, Stang A. [Some caveats in the interpretation of population attributable risks] Gesundheitswesen. 2018;80:149–153. doi: 10.1055/s-0042-104584. [DOI] [PubMed] [Google Scholar]
- 13.Ezzati M, Hoorn SV, Rodgers A, et al. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet. 2003;362:271–280. doi: 10.1016/s0140-6736(03)13968-2. [DOI] [PubMed] [Google Scholar]
- 14.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–364. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parkin DM. 2 Tobacco-attributable cancer burden in the UK in 2010. Br J Cancer. 2011;105(2):S6–S13. doi: 10.1038/bjc.2011.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Secretan B, Straif K, Baan R, et al. A review of human carcinogens–Part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol. 2009;10:1033–1034. doi: 10.1016/s1470-2045(09)70326-2. [DOI] [PubMed] [Google Scholar]
- 17.Scheidt-Nave C, Kamtsiuris P, Gößwald A, et al. German health interview and examination survey for adults (DEGS)-design, objectives and implementation of the first data collection wave. BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haftenberger M, Heuer T, Heidemann C, Kube F, Krems C, Mensink GB. Relative validation of a food frequency questionnaire for national health and nutrition monitoring. Nutr J. 2010;9 doi: 10.1186/1475-2891-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burger M, Brönstrup A, Pietrzik K. Derivation of tolerable upper alcohol intake levels in Germany: a systematic review of risks and benefits of moderate alcohol consumption. Prev Med. 2004;39:111–127. doi: 10.1016/j.ypmed.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 20.Talhout R, Schulz T, Florek E, van Benthem J, Wester P, Opperhuizen A. Hazardous compounds in tobacco smoke. Int J Environ Res Public Health. 2011;8:613–628. doi: 10.3390/ijerph8020613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ordonez-Mena JM, Schottker B, Mons U, et al. Quantification of the smoking-associated cancer risk with rate advancement periods: meta-analysis of individual participant data from cohorts of the CHANCES consortium. BMC Med. 2016;14 doi: 10.1186/s12916-016-0607-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kotz D, Bockmann M, Kastaun S. The use of tobacco, e-cigarettes, and methods to quit smoking in Germany. Dtsch Arztebl Int. 2018;115:235–242. doi: 10.3238/arztebl.2018.0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulze A, Mons U. Trends in cigarette smoking initiation and cessation among birth cohorts of 1926-1970 in Germany. Eur J Cancer Prev. 2005;14:477–483. doi: 10.1097/01.cej.0000174777.98518.7e. [DOI] [PubMed] [Google Scholar]
- 24.Wienecke A, Barnes B, Lampert T, Kraywinkel K. Changes in cancer incidence attributable to tobacco smoking in Germany, 1999-2008. Int J Cancer. 2014;134:682–691. doi: 10.1002/ijc.28392. [DOI] [PubMed] [Google Scholar]
- 25.Department of Health England. Towards a smokefree generation—a tobacco control plan for England. 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/630217/Towards_a_Smoke_free_Generation_-_A_Tobacco_Control_Plan_for_England_2017-2022__2_.pdf (last accessed on 6 July 2018) [Google Scholar]
- 26.Intergovernmental Committee on Drugs Australia. National tobacco strategy 2012-2018. Canberra: Commonwealth of Australia. 2012 [Google Scholar]
- 27.Levy DT, Blackman K, Currie LM, Mons U. Germany SimSmoke: the effect of tobacco control policies on future smoking prevalence and smoking-attributable deaths in Germany. Nicotine Tob Res. 2013;15:465–473. doi: 10.1093/ntr/nts158. [DOI] [PubMed] [Google Scholar]
- 28.Pflaum T, Hausler T, Baumung C, et al. Carcinogenic compounds in alcoholic beverages: an update. Arch Toxicol. 2016;90:2349–2367. doi: 10.1007/s00204-016-1770-3. [DOI] [PubMed] [Google Scholar]
- 29.Rehm J, Shield K. Alcohol consumption. In: Stewart BW, Wild CP, editors. World Cancer Report 2014. Lyon IARC: 2014. [Google Scholar]
- 30.Wienecke A, Barnes B, Neuhauser H, Kraywinkel K. Incident cancers attributable to alcohol consumption in Germany, 2010. Cancer Causes Control. 2015;26:903–911. doi: 10.1007/s10552-015-0566-8. [DOI] [PubMed] [Google Scholar]
- 31.Schütze M, Boeing H, Pischon T, et al. Alcohol attributable burden of incidence of cancer in eight European countries based on results from prospective cohort study. BMJ. 2011;342 doi: 10.1136/bmj.d1584. d1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meier PS, Holmes J, Angus C, Ally AK, Meng Y, Brennan A. Estimated effects of different alcohol taxation and price policies on health inequalities: a mathematical modelling study. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1001963. e1001963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hashibe M, Brennan P, Chuang SC, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 2009;18:541–550. doi: 10.1158/1055-9965.EPI-08-0347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Cancer Research Fund International. The associations between food, nutrition and physical activity and the risk of stomach cancer. London: World Cancer Research Fund International 2015. www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports/stomach-cancer (last accessed on 3 March 2018) [Google Scholar]
- 35.Catsburg C, Miller AB, Rohan TE. Active cigarette smoking and risk of breast cancer. Int J Cancer. 2015;136:2204–2209. doi: 10.1002/ijc.29266. [DOI] [PubMed] [Google Scholar]
- 36.Gredner T, Behrens G, Stock C, Brenner H, Mons U. Cancers due to infection and selected environmental factors—estimation of the attributable cancer burden in Germany. Dtsch Arztebl Int. 2018;115:586–593. doi: 10.3238/arztebl.2018.0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Behrens G, Gredner T, Stock C, Leitzmann MF, Brenner H, Mons U. Cancers due to excess weight, low physical activity and unhealthy diet—estimation of the attributable cancer burden in Germany. Dtsch Arztebl Int. 2018;115:578–585. doi: 10.3238/arztebl.2018.0578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Lange C, Manz K, Rommel A, Schienkiewitz A, Mensink G. Alkoholkonsum von Erwachsenen in Deutschland: Riskante Trinkmengen, Folgen und Maßnahmen. J Health Monitoring. 2016 doi: 10.17886/RKI-GBE-2016-029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Tramacere I, Negri E, Bagnardi V, et al. A meta-analysis of alcohol drinking and oral and pharyngeal cancers Part 1: overall results and dose-risk relation. Oral Oncol. 2010;46:497–503. doi: 10.1016/j.oraloncology.2010.03.024. [DOI] [PubMed] [Google Scholar]
- E3.Vingeliene S, Chan D, Vieira A, et al. An update of the WCRF/AICR systematic literature review and meta-analysis on dietary and anthropometric factors and esophageal cancer risk. Ann Oncol. 2017;28:2409–2419. doi: 10.1093/annonc/mdx338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E4.Vieira AR, Abar L, Chan DSM, et al. Foods and beverages and colorectal cancer risk: a systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann Oncol. 2017;28:1788–1802. doi: 10.1093/annonc/mdx171. [DOI] [PubMed] [Google Scholar]
- E5.World Cancer Research Fund International. The associations between food, nutrition and physical activity and the risk of liver cancer. London: World Cancer Research Fund International 2015. www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports/liver-cancer (last accessed on 3 March 2018) [Google Scholar]
- E6.World Cancer Research Fund International. The associations between food, nutrition and physical activity and the risk of breast cancer. London: World Cancer Research Fund International 2017; www.wcrf.org/int/research-we-fund/continuous-update-project-findings-reports/breast-cancer (last accessed on 3 March 2018) [Google Scholar]
- E7.Islami F, Tramacere I, Rota M, et al. Alcohol drinking and laryngeal cancer: overall and dose-risk relation–a systematic review and meta-analysis. Oral Oncol. 2010;46:802–810. doi: 10.1016/j.oraloncology.2010.07.015. [DOI] [PubMed] [Google Scholar]