Abstract
Background
Irritable bowel syndrome with diarrhoea (IBS-D) comprises multiple troublesome symptoms and negatively impacts patients’ quality of life.
Objective
The objective of this article is to assess IBS-D patient burden and patient and healthcare professional (HCP) attitudes towards IBS.
Methods
Patients and HCPs from Australia, Canada, France, Germany, Italy, Spain and the United Kingdom completed internet-based surveys via market research panels. Attitudes to IBS-D-related statements were scored using seven-point Likert scales.
Results
The patient survey included 513 patients (70% female, mean age 40.9 years). Faecal urgency was reported as the most troublesome symptom (27%) and fatigue occurred on the most days per month (mean: 18); 61% of patients used ≥3 types of treatment daily or intermittently; 19% used antidepressants daily. Thirty-three per cent thought HCPs should listen and provide more support and 46% reported willingness to ‘try anything’ to help manage their IBS–D. The HCP survey included 366 primary care physicians and 313 gastroenterologists: A total of 70% and 65%, respectively, agreed it was important that IBS-D patients feel listened to and supported; 73% agreed their main aim was to improve quality of life; ∼30% expressed frustration at managing IBS-D.
Conclusion
IBS-D imposes a substantial burden on patients and HCPs. These findings point towards a need for improved patient-HCP communication.
Keywords: Irritable bowel syndrome, diarrhoea, faecal urgency, psychosocial morbidity, survey
Key summary
Established knowledge on this subject
Irritable bowel syndrome with diarrhoea (IBS-D) is a functional bowel disorder characterised by abdominal pain with diarrhoea and multiple other gastrointestinal symptoms.
IBS-D symptoms can range from mild and intermittent to severe and continuous and can impose a substantial negative impact on quality of life.
IBS-D patients may undergo long delays before seeking treatment or reaching a diagnosis.
Patient and healthcare professional (HCP) attitudes towards IBS-D and the wider health burden on patients are not well described.
Significant and/or new findings of this study
The most troublesome symptom reported by IBS-D patients was faecal urgency, rather than the characteristic symptoms of abdominal pain and diarrhoea.
Most IBS-D patients use multiple treatments regularly, including codeine, and report high rates of dissatisfaction with current treatments.
Although some IBS-D patients generally accept their condition, many reported a substantial psychological burden and would like more support from HCPs.
HCPs generally understand the high burden imposed by IBS-D on patients but find the condition challenging to manage; adherence to guidelines is low.
Introduction
Irritable bowel syndrome (IBS) is a functional bowel disorder characterised by abdominal pain with altered bowel habits.1 IBS affects ∼11% of adults globally,2 of whom around one-third experience diarrhoea as the predominant bowel symptom (IBS-D).1 IBS-D patients typically experience multiple troublesome symptoms, including urgency, bloating, diarrhoea and abdominal pain,1 which can vary from mild and intermittent to severe and continuous.3
IBS-D is considered to be a gut-brain interaction disorder4 and a range of treatment approaches have been proposed, including diet and lifestyle modifications, probiotics and fibre supplements and various prescription and over-the-counter medications.5 However, patients can undergo long delays before seeking treatment or being diagnosed, despite experiencing bothersome symptoms.6
IBS-D can affect patients’ quality of life considerably7 and imposes a substantial economic burden.8,9 However, the health impact of IBS-D on patients in relation to their symptom burden and attitudes towards their condition is less well described. The aim of this study was twofold: first, to assess the gastrointestinal and wider health burden on patients currently receiving IBS-D treatment, including the range of medications used and patient-perceived care shortfalls; and second, to evaluate attitudes and perspectives of treating healthcare professionals (HCPs) towards IBS-D among a sample of IBS-D patients and HCPs.
Materials and methods
Data collection
The study comprised two separate self-administered, internet-based surveys, one for IBS-D patients and one for treating HCPs. Participants were invited to complete the surveys via online market research panels provided by Survey Sampling International, using online banner and email advertising; consenting participants were randomly selected for inclusion. Respondents opted-in via email without knowing the subject beforehand. All survey questions were mandatory. Respondents received a small incentive in the form of points which could be redeemed for vouchers or PayPal credit.
Patients from Australia, Canada and the EU5 region (France, Germany, Italy, Spain and the United Kingdom (UK)) completed a 30-minute web-based structured questionnaire, starting with a panel of screening questions related to gastrointestinal conditions to determine eligibility. The survey, completed in January and February 2016, comprised 51 questions on patient experience, treatment behaviours and attitudes towards IBS-D and current and new treatments. The target sample size was 80 patients per country. The sample was boosted via a second provider (Lightspeed) to account for a shortfall in the original panel and to replace records rejected through quality control. The target sample size was not achieved in all countries (Australia, n = 76; Canada, n = 66; France, n = 43; Germany, n = 80; Italy, n = 85; Spain, n = 81; UK, n = 82).
The HCP survey included gastroenterologists and primary care physicians (PCPs) from the same seven countries, who completed a 40-minute web-based structured questionnaire between February and April 2016, including questions on attitudes to IBS-D concerning patients, management, therapies, treatment guidelines and goals. The target sample size was 45 HCPs per type per country.
Sample population
Patient eligibility criteria were strict, to ensure a representative cohort of IBS-D patients, and included: males and females aged 18–65 years; diagnosed with IBS-D by a HCP; symptoms of diarrhoea and abdominal pain, discomfort or spasm present for >1 year and within the past year; taken prescription or over-the-counter medications to help manage IBS-D in the past year; not diagnosed with chronic constipation, inflammatory bowel disease, coeliac disease, cancer, diverticulitis, ulcerative colitis, Crohn’s disease, pancreatitis or alcohol or drug abuse; not had a cholecystectomy; not affiliated with a pharmaceutical company; and not participated in IBS market research in the past three months. There were target maximum quotas for proportions of females (70%) and patients who had never seen a specialist gastroenterologist for their IBS-D (40%).
Screening criteria for the HCP survey were: 3–35 years’ experience; seen diagnosed IBS-D patients within the past three months; prescribed medication or recommended over-the-counter treatments for IBS-D patients; not affiliated with a pharmaceutical company; and not participated in IBS market research in the past three months. Gastroenterologists must have been consultant grade (or equivalent).
Statistical analysis
Categorical variables were summarised by descriptive statistics. Patient and HCP attitudes to statements relating to IBS-D were scored using seven-point Likert scales (1 = completely disagree; 4 = neither agree nor disagree; 7 = completely agree). Participants who answered 6 (agree) or 7 were considered to agree with the statement; those who answered 1 or 2 (disagree) were considered to disagree; those who answered 3–5 were classed as neither agreeing nor disagreeing.
Statistical Package for the Social Sciences software was used to analyse the patient sample. Two-tailed t tests were performed for the means and proportions from two independent samples (patients who had ever or never seen a gastroenterologist) to compare demographics, characteristics and attitudes data at a 5% risk level, with p < 0.05 denoting significance.
Results
Patient survey
Demographics and healthcare characteristics
Of 8627 patients screened, 513 were eligible; 315 (61%) had seen a gastroenterologist (Table 1), mean age was 40.9 years and 357 (70%) were female. The most commonly reported comorbidities were anxiety (37%), depression (27%) and migraine (26%).
Table 1.
Demographics, healthcare characteristics and reason for first HCP visit.
| Ever seen a gastroenterologist |
|||
|---|---|---|---|
| Total (N = 513)a | Yes (n = 315) | No (n = 198) | |
| Female, n (%) | 357 (70) | 220 (70) | 137 (69) |
| Mean age, years (SD) | 40.9 (11.6) | 41.7 (11.5) | 39.8 (11.6) |
| Most common comorbidities, n (%)b,c | |||
| Anxiety | 189 (37) | 109 (35) | 80 (40) |
| Depression | 137 (27) | 80 (25) | 57 (29) |
| Migraine | 133 (26) | 87 (28) | 46 (23) |
| Gastric reflux | 109 (21) | 84 (27)k | 25 (13) |
| Lactose intolerance | 69 (13) | 50 (16)k | 19 (10) |
| Diagnostic testing history, n (%)d,e | |||
| Blood tests | 403 (79) | 275 (87)k | 128 (65) |
| Stool tests | 322 (63) | 225 (71)k | 97 (49) |
| Endoscopy/colonoscopy | 304 (59) | 243 (77)k | 61 (31) |
| Food allergy tests | 205 (40) | 149 (47) | 56 (28) |
| Most common symptoms before treatment, n (%)f,g | |||
| Diarrhoea | 513 (100) | 315 (100) | 198 (100) |
| Stomach pain or discomfort | 399 (78) | 247 (78) | 152 (77) |
| Stomach cramps or spasm | 361 (70) | 223 (71) | 138 (70) |
| Bloating | 269 (52) | 175 (56) | 94 (47) |
| Urgency | 204 (40) | 122 (39) | 82 (41) |
| Mucus | 100 (19) | 71 (23)k | 29 (15) |
| Faecal incontinence | 88 (17) | 56 (18) | 32 (16) |
| Mean length of time with symptoms, years (SD)h | 9.8 (9.5) | 10.2 (9.9) | 9.1 (8.8) |
| Reason for first HCP visit, n (%)i,j | |||
| The condition was having a large impact on my quality of life | 253 (49) | 168 (53)k | 85 (43) |
| Increasing frequency of my symptoms | 245 (48) | 159 (50) | 86 (43) |
| I was worried about the length of time I’d had my symptoms for | 227 (44) | 150 (48) | 77 (39) |
| Increasing severity of my symptoms | 215 (42) | 151 (48)k | 64 (32) |
| Treatments I tried myself did not relieve the symptoms | 124 (24) | 77 (24) | 47 (24) |
| Fear of serious or life-threatening condition | 121 (24) | 86 (27)k | 35 (18) |
| I read information on the internet that made me suspect it was IBS | 113 (22) | 64 (20) | 49 (25) |
| A friend or family member advised me to go to an HCP | 111 (22) | 71 (23) | 40 (20) |
| Family history of cancer (eg bowel or stomach) | 52 (10) | 37 (12) | 15 (8) |
Australia, n = 76; Canada, n = 66; France, n = 43; Germany, n = 80; Italy, n = 85; Spain, n = 81; UK, n = 82; bBased on responses to the question: ‘Which of the following conditions, if any, have you been diagnosed with by a doctor?’; cReported in ≥10% of patients; dBased on responses to the question: ‘Which of the following tests have been carried out since you first experienced symptoms of IBS?’; eReported in ≥20% of patients; fBased on responses to the question: ‘Which, if any, of the following symptoms does your IBS include before you take any treatment, if you take any?’; gReported in ≥10% of patients in any group; hBased on responses to the question: ‘For how long have you experienced your IBS symptoms?’; iBased on responses to the question: ‘What made you decide to arrange your first appointment with a HCP about the symptoms of IBS you were experiencing?’; jReported in ≥10% of patients in any group; kp < 0.05 vs patients who had never seen a gastroenterologist.
HCP: healthcare professional; IBS: irritable bowel syndrome; SD: standard deviation.
IBS-D symptom burden
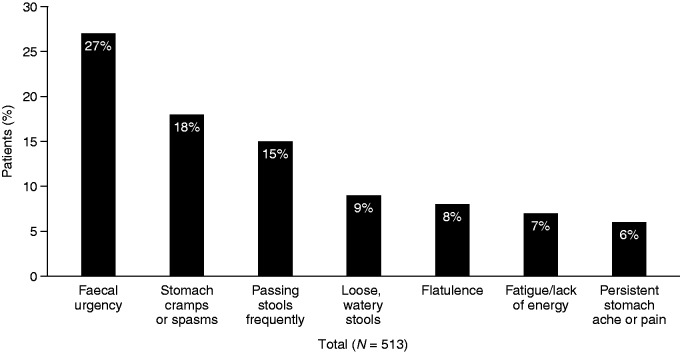
As well as diarrhoea (100%), the most common symptoms prior to treatment included stomach pain or discomfort (78%), stomach cramps or spasm (70%) and bloating (52%); 17% of patients reported faecal incontinence (Table 1). Mucus was reported in a significantly greater proportion of patients who had seen a gastroenterologist than those who had not (23% vs 15%; p < 0.05). Overall, the median symptom duration was six years (range 1– > 21 years; mean 9.8 years; standard deviation 9.5 years). Faecal urgency was regarded as the most troublesome symptom by 136 patients (27%) (Figure 1).
Figure 1.
Most troublesome symptoms currently experienced.a,b
aBased on the first selected response to the question: ‘Which of the symptoms you currently experience trouble you the most?’ (bloating was not included as a potential response); bReported in ≥5% of patients.
The most common reason for arranging a first appointment with an HCP was the large impact IBS-D was having on quality of life (49%). Of patients who had seen a gastroenterologist, 53% reported quality of life as the main reason for a first HCP appointment, compared to 43% of those who had not seen a gastroenterologist (p < 0.05) (Table 1). Other reasons (multiple responses were allowed) included increasing frequency of symptoms (48%), worry about duration of symptoms (44%) and increasing symptom severity (42%).
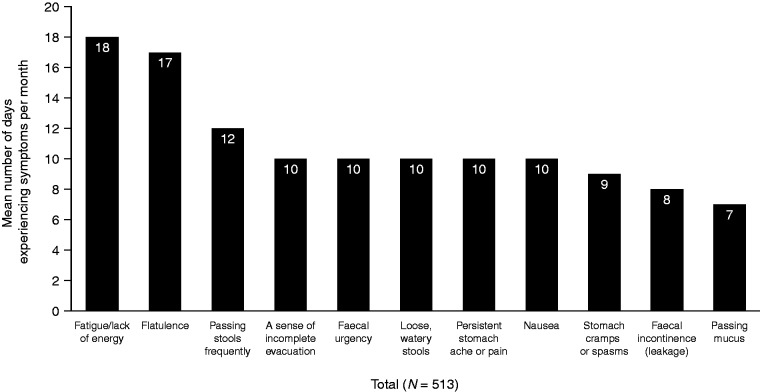
Over the preceding three months, 390 patients (76%) reported experiencing intermittent symptoms and 123 (24%) reported continuous symptoms. Symptoms that occurred on the most days per month on average were fatigue/lack of energy (18 days) and flatulence (17 days) (Figure 2). Patients who had previously seen a gastroenterologist reported significantly more frequent flatulence (18 vs 14 days per month; p < 0.05), sense of incomplete evacuation (12 vs 9 days per month; p < 0.05) and loose, watery stools (11 vs 9 days per month; p < 0.05), on average, than those who had not.
Figure 2.
Number of days experiencing symptoms per month.a
aBased on responses to the question: ‘In the past three months, how many days per month, on average, have you experienced each of your irritable bowel syndrome symptoms?’
Medication use
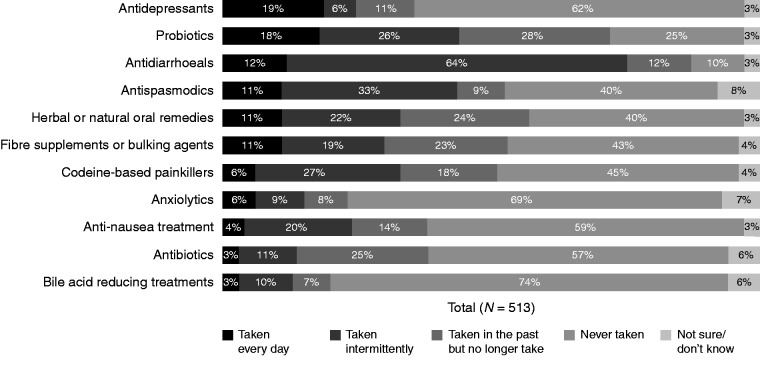
Overall, 498 (97%) patients reported using at least one type of medication intermittently or daily, and 315 (61%) reported using three or more (Supplementary Figure 1). In total, 372 patients (73%) reported currently using over-the-counter medication, either alone (n = 214, 42%) or with concurrent prescription medication (n = 158, 31%).
Antidiarrhoeal agents were the most commonly used medication type: intermittently in 326 (64%) and daily in 63 patients (12%) (Figure 3). Antidepressants were the most commonly used daily medication (n = 95, 19%), followed by probiotics (n = 92, 18%). Intermittent or daily use of codeine-based painkillers was reported by 168 patients (33%). Patients who had seen a gastroenterologist reported significantly higher daily use of antispasmodics (n = 43, 14% vs n = 15, 8%), bile acid sequestrants (n = 16, 5% vs n = 1, 1%), anti-nausea treatment (n = 18, 6% vs n = 2, 1%) and antibiotics (n = 12, 4% vs n = 1, 1%) than those who had not (all comparisons: p < 0.05).
Figure 3.
Current patterns of medication use.a
aBased on responses to the question: ‘Which best describes your use of each of the following treatments in the management of your irritable bowel syndrome?’
Percentages may not always total 100% due to rounding.
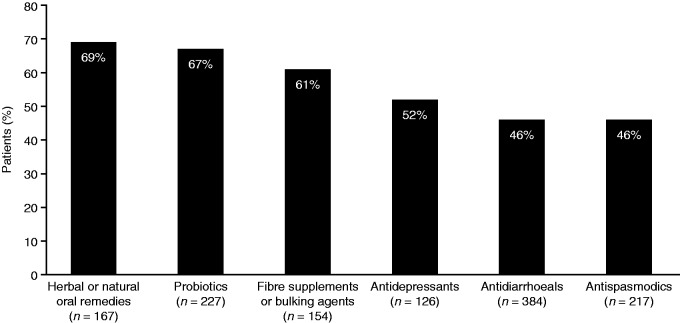
Treatment satisfaction
Overall, patients reported high levels of dissatisfaction with current IBS-D treatments (Figure 4), most commonly herbal or natural remedies (n = 115/167, 69%), probiotics (n = 151/227, 67%) and fibre supplements (n = 94/154, 61%). Additionally, 178 of 384 patients (46%) were dissatisfied with antidiarrhoeals.
Figure 4.
Patient dissatisfaction with current treatments.a
aResults included the proportion of patients answering 1 to 5 (completely disagree, slightly agree) in response to the question: ‘How satisfied are you overall with each of the treatments you are currently taking for your irritable bowel syndrome?’ (seven-point scale where 1=completely disagree and 7=completely agree).
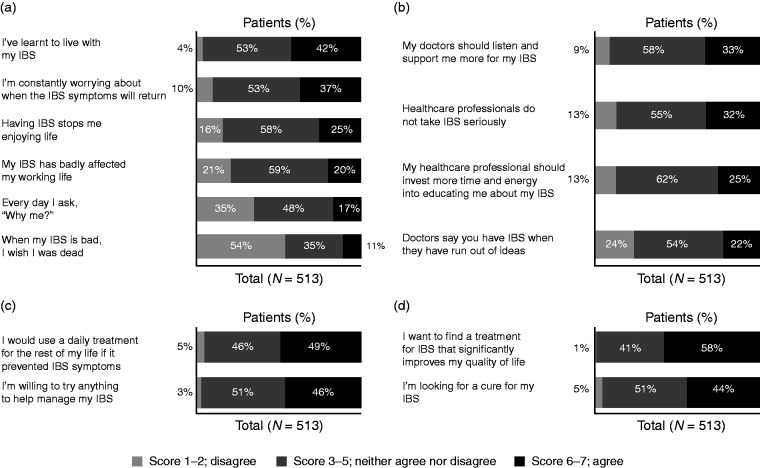
Patient attitudes towards IBS-D
Although 216 patients (42%) agreed that they had learned to live with IBS, 189 (37%) were worried about when their symptoms would return and 58 (11%) agreed that: ‘When my IBS is bad, I wish I was dead’ (Figure 5(a)).
Figure 5.
Patient attitudes towards: (a) IBS; (b) healthcare professionals and services; (c) current therapies; (d) treatment goals.
Percentages may not always total 100% due to rounding.
IBS: irritable bowel syndrome.
One-third of patients (n = 170, 33%) agreed that doctors should listen and provide more support and 165 (32%) agreed that HCPs do not take IBS seriously (Figure 5(b)).
Overall, 249 patients (49%) reported that they would use a daily treatment for the rest of their life if it prevented IBS symptoms and 237 (46%) reported willingness to ‘try anything’ (Figure 5(c)). Regarding treatment goals, 296 patients (58%) reported a desire for IBS treatment to significantly improve quality of life and 227 (44%) reported seeking a cure for their IBS (Figure 5(d)).
HCP survey
Sample size and caseload
Of 1460 HCPs screened, 643 were eligible and completed the survey: 366 PCPs and 313 gastroenterologists. On average over a three-month period, PCPs reported seeing 957 patients, including 84 with diagnosed or suspected IBS, of whom 27 had IBS-D (32%). Gastroenterologists reported an average caseload of 491 patients over three months, including 169 with diagnosed or suspected IBS, of whom 55 had IBS-D (33%).
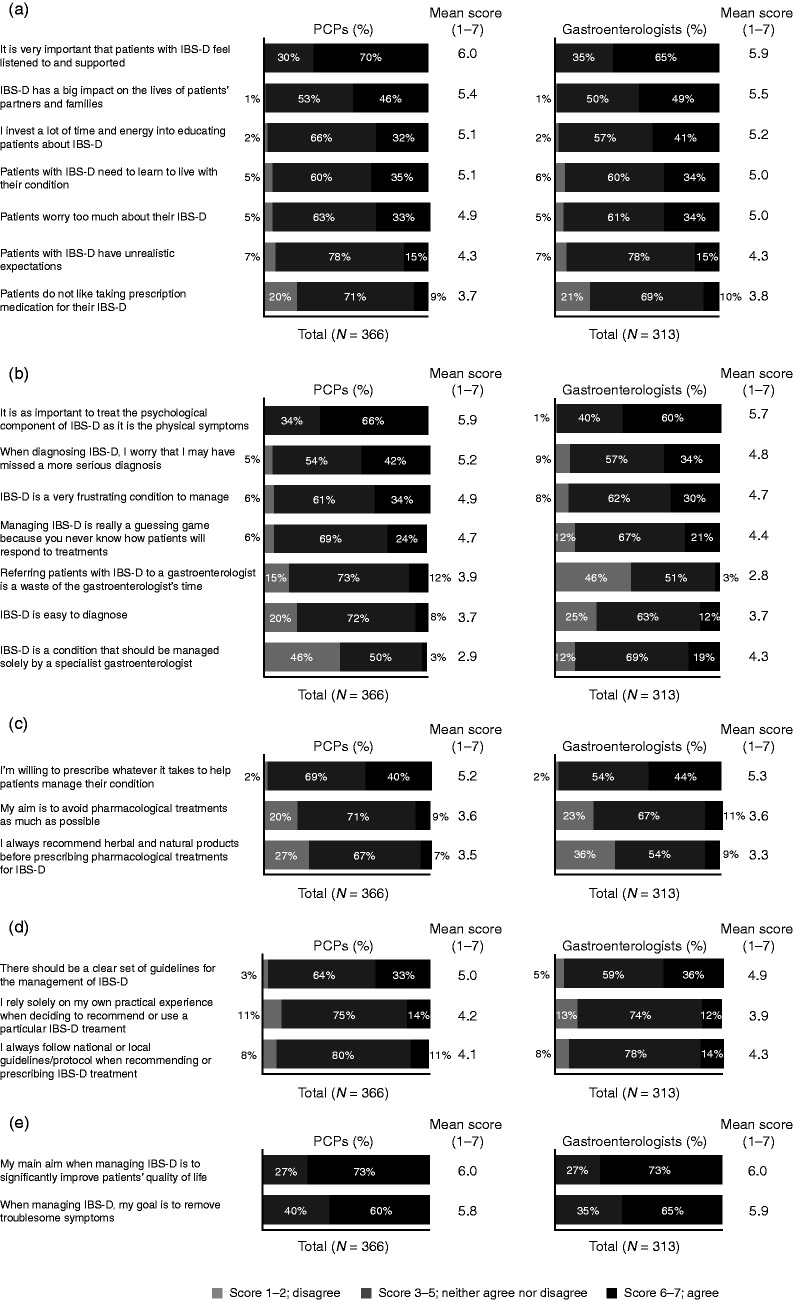
HCP attitudes towards IBS-D
Approximately two-thirds of PCPs and gastroenterologists agreed that IBS-D patients should feel listened to and supported, and none disagreed (Figure 6(a)). Approximately one-third agreed that IBS-D patients need to live with their condition (35% and 34%, respectively) and that they worry about it too much (33% and 34%, respectively).
Figure 6.
HCP attitudes towards: (a) IBS patients; (b) management of IBS; (c) current therapies; (d) treatment guidelines; (e) treatment goals.
Percentages may not always total 100% due to rounding.
HCP: healthcare professional; IBS: irritable bowel syndrome; IBS-D: irritable bowel syndrome with diarrhoea; PCP: primary care physician.
The psychological component of IBS-D was considered just as important to treat as the physical symptoms by 66% of PCPs and 60% of gastroenterologists (Figure 6(b)). Approximately one-third of PCPs and gastroenterologists agreed that IBS-D was very frustrating to manage (34% and 30%, respectively). Only 15% of PCPs disagreed that referring IBS-D patients to a gastroenterologist is a waste of the gastroenterologist’s time, compared to 46% of gastroenterologists (Figure 6(b)).
Similar proportions of PCPs (40%) and gastroenterologists (44%) reported willingness to try ‘whatever it takes’ to help patients manage their condition (Figure 6(c)). Approximately 10% of HCPs aimed to avoid pharmacological treatments as much as possible, and a similar proportion agreed that they would always recommend herbal and natural products before prescribing pharmacological treatments.
Approximately one-third of PCPs (33%) and gastroenterologists (36%) agreed that there should be a clear set of guidelines for the management of IBS-D (Figure 6(d)). When recommending or prescribing IBS-D treatment, 14% of PCPs and 12% of gastroenterologists reported relying solely on their own practical experience; only 11% of PCPs and 14% of gastroenterologists reported always following national and local guidelines.
Overall, 73% of PCPs and gastroenterologists agreed that their main aim when managing IBS-D is to significantly improve patients’ quality of life (mean score 6.0 each; none disagreed), and 60% of PCPs and 65% of gastroenterologists agreed that: ‘When managing IBS-D my goal is to remove troublesome symptoms’ (none disagreed) (Figure 6(e)).
Discussion
This survey-based study demonstrates the wide burden of IBS-D on patients and at the wider service level, and provides insights into HCP attitudes towards the condition. Patients expressed strong desires for improved symptom management and for HCPs to take them more seriously, yet HCPs generally recognised the large psychological and physical symptom burden. These results may point towards an unmet need for improved patient-physician communication10 and satisfactory pharmacological and supportive therapies,11–14 which may be aided by the Multi-Dimensional Clinical Profile, an innovative learning tool to assist HCPs with a patient-centred approach to managing functional gastrointestinal disorders, advocated by the Rome Foundation.15
IBS-D patients reported experiencing multiple troublesome symptoms for long durations. Given that the symptoms principally used to diagnose IBS-D are abdominal pain and diarrhoea,4 it is interesting that patients reported that their most troublesome and frequently occurring symptoms were faecal urgency and fatigue.
HCPs generally indicated that IBS-D was challenging to manage. Approximately one-third expressed a desire for clear guidelines, only 11%–14% indicated adherence to guidelines and a similar proportion reported using solely their own experience. These results represent a discrepancy between HCPs’ reported aims of improving symptoms and quality of life and the low reported adherence to evidence-based guidelines, which could imply either that current guidelines are inadequate or unclear, or that improved education is required. Low adherence to guidelines may partly account for the variety of prescription treatments used by patients.16,17 Antidiarrhoeals and antispasmodics were reportedly the most common pharmacological treatments taken daily or intermittently, consistent with current recommendations.18 Conversely, antidepressants are not recommended as first-line therapy,18 despite being reported as the most commonly used daily treatments for IBS-D, possibly reflecting the strong association of IBS with psychological comorbidities.19–22
More than one-half of patients reported currently or previously using codeine-based painkillers, higher than previous reports of narcotic use for IBS,13 suggesting a need to manage severe pain and diarrhoea. This is concerning as codeine is not recommended for treating diarrhoea because of gastroenterological side effects and increased probability of addiction with long-term use in chronic conditions;23 however, it is unclear whether codeine use was through self-medication or prescription. High codeine use and the large proportion of patients and HCPs ‘willing to try anything’ further highlights that IBS is challenging to manage.24
The reported regular use of multiple treatments, combined with low satisfaction, may suggest tolerability or effectiveness issues. Patients were least satisfied with herbal or natural therapies, possibly reflecting a lack of evidence for their efficacy.25 Notably, ∼10% of HCPs agreed that they would avoid pharmacological treatments as much as possible, highlighting low adherence to current treatment guidelines,17 which recommend dietary and lifestyle interventions18,26 followed by pharmacological treatment. Reasons for avoiding pharmacological treatment may include lack of awareness of available treatments, patient preferences or efficacy and safety concerns; the latter possibly indicates a need for improved treatment options.
Patients reported the impact of IBS-D on quality of life as the most common reason for first visiting an HCP about IBS-D, consistent with previous findings that IBS-D symptoms can reduce patients’ quality of life.3,7 Correspondingly, patients and HCPs strongly agreed that quality of life improvement should be the main treatment goal.
Patients reported mixed attitudes towards and general acceptance of their IBS, although, consistent with previous findings,13,27,28 results suggested that some patients experienced a substantial psychological burden (25% reported that IBS stops them enjoying life and 11% reported suicidal ideation). Results also suggested that patients perceived that HCPs underestimated the impact of IBS-D, yet HCPs generally recognised the psychological component, with the majority expressing an understanding that patients require support. These findings support previous reports of the communication gap between patients with functional gastrointestinal disorders and HCPs.10
Approximately one-third of the HCPs’ IBS caseload consisted of IBS-D patients, consistent with previous findings.1 However, the total PCP caseload consisted of proportionally more IBS patients than a previous report,29 which could suggest higher IBS-D prevalence than historically observed, increased willingness to visit an HCP or a sample selection bias. Many gastroenterologists agreed that referring patients to them was valuable, yet few PCPs concurred, suggesting that improved communication between specialties may permit more effective management.10 Including clear advice on when to refer patients to a gastroenterologist may be a consideration for future guidelines.
IBS-D patients were identified through the internet, representing the large demographic of patients who commonly seek information online.13,30,31 The prespecified quota of 60% of patients who had previously seen a gastroenterologist may indicate that those with more severe symptoms were overrepresented compared to previous reports.29 However, estimates of symptom severity can vary widely according to the type of population and method of assessment,32 and country-level health system differences may mean some patients had direct access to a specialist. Another possible limitation is that participants self-identified as having been diagnosed with IBS-D by an HCP. Overall, the large sample size of patients (n = 513) and HCPs (n = 643) fits with previous reports.6,14 However, the target patient quota was not achieved in all countries. Additionally, only gastroenterologists of at least consultant grade were included, possibly underrepresenting perspectives of younger HCPs. Other limitations include the large proportion of neutral responses for both surveys,33 and possible bias towards the most ‘agreeable’ answer, which may also depend on the visual order.34
This study highlights the substantial symptom burden on IBS-D patients and the impact that IBS-D exerts on quality of life. The complex treatment landscape of multiple therapies, low treatment satisfaction rates and low adherence to existing guidelines implies an unmet need for improved pharmacological and supportive therapies, together with clearer guidelines.35 This study also suggests that HCPs experience a degree of uncertainty and difficulty in managing IBS-D patients, and points towards a need for improved communication between HCPs and patients.
Acknowledgements
Editorial assistance in the writing and revision of the draft manuscript on the basis of detailed discussion and feedback from all the authors was provided by Helena Cant of Complete HealthVizion Inc and funded by Allergan plc.
Declaration of conflicting interests
Hans Törnblom has worked on advisory boards for Allergan plc, Almirall and Shire. Richard Goosey is an employee of Kantar Health, paid consultant of Allergan plc. Gwen Wiseman is a former employee of Allergan plc. Stephen Baker is an employee of Allergan plc. Anton Emmanuel has worked on advisory boards for Allergan plc, Almirall, Shire and Takeda.
Funding
This work was supported by Allergan plc but received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethics approval
Not applicable because this is a survey.
Informed consent
Not applicable because this is a survey.
References
- 1.Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology 2016; 150: 1393–1407. [DOI] [PubMed] [Google Scholar]
- 2.Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis. Clin Gastroenterol Hepatol 2012; 10: 712–721. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Chang L, Bellamy N, et al. Severity in irritable bowel syndrome: A Rome Foundation Working Team report. Am J Gastroenterol 2011; 106: 1749–1759. [DOI] [PubMed] [Google Scholar]
- 4.Schmulson MJ, Drossman DA. What is new in Rome IV. J Neurogastroenterol Motil 2017; 23: 151–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lacy BE. The science, evidence, and practice of dietary interventions in irritable bowel syndrome. Clin Gastroenterol Hepatol 2015; 13: 1899–1906. [DOI] [PubMed] [Google Scholar]
- 6.American Gastroenterological Association. IBS in America: Survey summary findings, http://ibsinamerica.gastro.org/files/IBS_in_America_Survey_Report_2015-12-16.pdf (2015, accessed 5 November 2016).
- 7.Buono JL, Carson RT, Flores NM. Health-related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual Life Outcomes 2017; 15: 35–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flores NM, Tucker C, Carson RT, et al. The humanistic and economic burden of irritable bowel syndrome with diarrhoea (IBS-D) by disease severity among patients in the EU5 region. Value Health 2016; 19: A514–A515. [Google Scholar]
- 9.Canavan C, West J, Card T. Calculating total health service utilisation and costs from routinely collected electronic health records using the example of patients with irritable bowel syndrome before and after their first gastroenterology appointment. Pharmacoeconomics 2016; 34: 181–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collins J, Farrall E, Turnbull DA, et al. Do we know what patients want? The doctor-patient communication gap in functional gastrointestinal disorders. Clin Gastroenterol Hepatol 2009; 7: 1252–1254. [DOI] [PubMed] [Google Scholar]
- 11.Camilleri M. Current and future pharmacological treatments for diarrhea-predominant irritable bowel syndrome. Expert Opin Pharmacother 2013; 14: 1151–1160. [DOI] [PubMed] [Google Scholar]
- 12.Hulisz D. The burden of illness of irritable bowel syndrome: Current challenges and hope for the future. J Manag Care Pharm 2004; 10: 299–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drossman DA, Morris CB, Schneck S, et al. International survey of patients with IBS: Symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J Clin Gastroenterol 2009; 43: 541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lacy BE, Rosemore J, Robertson D, et al. Physicians’ attitudes and practices in the evaluation and treatment of irritable bowel syndrome. Scand J Gastroenterol 2006; 41: 892–902. [DOI] [PubMed] [Google Scholar]
- 15.Drossman DA. Multi-dimensional clinical profile (MDCP): for the functional gastrointestinal disorders, 1st ed Raleigh: The Rome Foundation, 2015. [Google Scholar]
- 16.Olafsdottir LB, Gudjonsson H, Jonsdottir HH, et al. Irritable bowel syndrome: Physicians’ awareness and patients’ experience. World J Gastroenterol 2012; 18: 3715–3720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harkness EF, Harrington V, Hinder S, et al. GP perspectives of irritable bowel syndrome – an accepted illness, but management deviates from guidelines: A qualitative study. BMC Fam Pract 2013; 14: 92–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute for Health and Care Excellence. Irritable bowel syndrome in adults: Diagnosis and management, https://www.nice.org.uk/guidance/cg61/resources/irritable-bowel-syndrome-in-adults-diagnosis-and-management-pdf-975562917829 (2008, accessed 23 October 2017).
- 19.Van Oudenhove L. The link between affective and functional gastrointestinal disorders: Are we solving the psychobiological puzzle? Neurogastroenterol Motil 2008; 20: 1265–1267. [DOI] [PubMed] [Google Scholar]
- 20.Qin HY, Cheng CW, Tang XD, et al. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol 2014; 20: 14126–14131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grzesiak M, Beszłej JA, Mulak A, et al. The lifetime prevalence of anxiety disorders among patients with irritable bowel syndrome. Adv Clin Exp Med 2014; 23: 987–992. [DOI] [PubMed] [Google Scholar]
- 22.Fond G, Loundou A, Hamdani N, et al. Anxiety and depression comorbidities in irritable bowel syndrome (IBS): A systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci 2014; 264: 651–660. [DOI] [PubMed] [Google Scholar]
- 23.Quigley EMM, Fried M, Gwee KA, et al. World Gastroenterology Organisation global guidelines irritable bowel syndrome: A global perspective update September 2015. J Clin Gastroenterol 2016; 50: 704–713. [DOI] [PubMed] [Google Scholar]
- 24.Keefer L, Drossman DA, Guthrie E, et al. Centrally mediated disorders of gastrointestinal pain. Gastroenterology 2016; 150: 1408–1419. [DOI] [PubMed] [Google Scholar]
- 25.Chey WD, Maneerattaporn M, Saad R. Pharmacologic and complementary and alternative medicine therapies for irritable bowel syndrome. Gut Liver 2011; 5: 253–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKenzie YA, Bowyer RK, Leach H, et al. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet 2016; 29: 549–575. [DOI] [PubMed] [Google Scholar]
- 27.Miller V, Hopkins L, Whorwell PJ. Suicidal ideation in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol 2004; 2: 1064–1068. [DOI] [PubMed] [Google Scholar]
- 28.Ballou S, Bedell A, Keefer L. Psychosocial impact of irritable bowel syndrome: A brief review. World J Gastrointest Pathophysiol 2015; 6: 120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: Prevalence, characteristics, and referral. Gut 2000; 46: 78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Halpert A, Dalton CB, Palsson O, et al. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National survey on patient educational needs in IBS and development and validation of the Patient Educational Needs Questionnaire (PEQ). Am J Gastroenterol 2007; 102: 1972–1982. [DOI] [PubMed] [Google Scholar]
- 31.Halpert A, Dalton CB, Palsson O, et al. Patient educational media preferences for information about irritable bowel syndrome (IBS). Dig Dis Sci 2008; 53: 3184–3190. [DOI] [PubMed] [Google Scholar]
- 32.Lembo A, Ameen VZ, Drossman DA. Irritable bowel syndrome: Toward an understanding of severity. Clin Gastroenterol Hepatol 2005; 3: 717–725. [DOI] [PubMed] [Google Scholar]
- 33.Matell MS, Jacoby J. Is there an optimal number of alternatives for Likert-scale items? Effects of testing time and scale properties. J Appl Psychol 1972; 56: 506–509. [Google Scholar]
- 34.Friedman HH, Herskovitz PJ, Pollack S. The biasing effects of scale-checking styles on response to a Likert scale. Proceedings of the Section on Survey Research Methods 1993; 2: 792–795. [Google Scholar]
- 35.Lacy BE, Ford AC, Talley NJ. Quality of care and the irritable bowel syndrome: Is now the time to set standards? Am J Gastroenterol 2018; 113: 167–169. [DOI] [PubMed] [Google Scholar]