ABSTRACT
We aimed to identify factors such as pre-arthroscopy and intra-operative variables that were associated with failure of hip arthroscopy as a joint preserving operation. We performed a retrospective analysis of a database containing 344 consecutive hip arthroscopies performed at our institution. Forty-four hips were identified that underwent a subsequent arthroplasty procedure following their hip arthroscopy (cases). Sixty-six control hips (hip arthroscopy with no subsequent arthroplasty) were randomly selected from the same database. Cases and controls were matched for age, sex and follow-up (P = 0.59, 0.48, 0.10, respectively). Pre-operative radiographs/MRI scans plus intra-operative findings were analysed to identify factors associated with failure. Both a lower centre edge angle and higher acetabular index on pre-operative radiographs were associated with higher rates of failure (P < 0.001). The presence of any acetabular wear at operation was also associated with failure (P < 0.001). Highest rates of failure were seen in hips with both features of dysplasia on pre-operative radiographs and any intra-operative acetabular wear (relative risk: 5, odds ratio: 9.13, P < 0.001). Dysplastic features on pre-operative radiographs and the finding of acetabular wear at hip arthroscopy increase the risk of subsequent arthroplasty. Identification of these features pre-operatively with evolving imaging techniques would improve the results of hip arthroscopy as joint preserving surgery.
INTRODUCTION
Hip arthroscopy is rapidly becoming a more frequently performed procedure; the UK National Non-Arthroplasty Hip Registry reported a greater than doubling in the number of arthroscopies performed between 2012 and 2015 [1]. Similar trends have been observed in the United States [2]. Overall, hip arthroscopy has been shown to be a safe and successful intervention for a wide variety of indications [2–4]. Unfortunately, conversion to an ipsilateral total hip replacement (THR) following hip arthroscopy is necessary up to 16% of patients [5–7]. Identifying factors pre-operatively that might predict the need for subsequent arthroplasty would benefit both patient and surgeon.
Previous retrospective case series have focused upon determining why hip arthroscopy fails for a specific diagnosis, for example femoroacetabular impingement (FAI) [8–10]. There has been a lack of studies comparing cohorts of failed (requiring arthroplasty) and preserved hips following arthroscopy in patients that are matched for age and sex, regardless of initial diagnosis. Consequently, there remains the need to clarify factors that limit hip arthroscopy as an arthroplasty-sparing procedure without the aforementioned selection bias of a specific diagnosis.
In our single centre, case control study aimed to (i) identify features on pre-operative radiographs that might predict failure of arthroscopy and necessity for subsequent arthroplasty and (ii) determine intra-operative findings associated with the failure of hip arthroscopy as joint preserving surgery which may be identifiable on pre-operative imaging thus allowing surgeons in the future to better identify suitable patients for joint preserving surgery as well as inform both surgeon and patient of the likelihood of success of their arthroscopic hip surgery.
MATERIALS AND METHODS
This is a retrospective, case-controlled study performed at a single District General Hospital in the United Kingdom. The study was performed as a service evaluation and therefore did not require National Health Service (NHS) Research Ethics Committee, NHS/Health and Social Care (HSC) R&D Office or Health Research Authority (HRA) approval (http://www.hra.nhs.uk/research-community/before-you-apply/determine-whether-your-study-is-research/# sthash.UDz6enkk.dpuf).
A prospectively collected database of hip arthroscopy patients between 2008 and 2012 was reviewed. During this 5-year period, 344 hip arthroscopies were recorded, from which ‘cases’ were identified as having undergone hip arthroscopy and needing a subsequent, ipsilateral, hip arthroplasty procedure. A control cohort (patients who had a hip arthroscopy but no subsequent arthroplasty procedure) were selected being matched for age and sex. All patients, including those referred from regional hospitals, were followed up for a minimum of 2 years post-arthroscopy at the Royal Berkshire Hospital, with the length of follow-up being defined as the last clinical review.
Based on previous work by McCarthy et al. [11] investigating the failure rate of hip arthroscopy dependent on the degree of cartilaginous wear we calculated, we would need 10 hips in each group to detect a significant difference for individual factors (power = 0.8, α < 0.5). We decided on a ratio of 1:1.5 (cases: controls) for our study to ensure that our study was sufficiently powered. A total of 44 cases were identified and 66 controls were selected. The overall study population comprised 81 female patients (34 cases, 47 controls) and 29 male patients (10 cases, 19 controls).
All surgeries were performed by two very experienced hip arthroscopists who offer a tertiary referral service for hip arthroscopy in the United Kingdom. The patients included in this study are from their NHS practice only, which amounts to half of each of their practices. There was no significant difference in the rate of conversion to THR between surgeons.
Hip arthroscopy was performed with the patient supine with a specialized hip distractor table. Traction was first applied to the contralateral leg and then to the ipsilateral leg. The first portal (anterolateral) was sited under fluoroscopic guidance. An anterior portal was created under direct vision. The central compartment was assessed first. For patients with a CAM deformity of the femoral neck, an osteochondroplasty was performed with fluoroscopy used to assess adequate resection. Pincer resection was performed with or without a labral takedown depending on the size of deformity and planned correction of the centre edge angle (CEA). Labral pathology was addressed with knotless anchors for repairable tears or radiofrequency ablation for non-repairable tears. Labral repair was always carried out in preference to debridement. Isolated University College London Hospital (UCLH) grade 4a [12] chondral lesions were treated with microfracture. As our standard practice was to not carry out an inter-portal capsulotomy, the authors do not routinely carry out a capsular repair. At the end of the procedure, the joint was infused with local anaesthetic.
All patients had a standardized post-operative rehabilitation comprising overnight stay and physiotherapy; they were mobilized fully weight bearing, unless microfracture was performed, in which case, up to 3 weeks of protected weight bearing was instigated. Initial follow-up was at 6 weeks with subsequent reviews at 3 months, 6 months and 1 year post-operation. Additional follow-up was determined by patient symptoms. All patients were recommended to complete a 2-week course of non-steroidal anti-inflammatory medication as an analgesic and heterotopic ossification prophylaxis unless contra-indicated.
The primary outcome was the requirement for a hip arthroplasty operation (either hip resurfacing or THR) following a hip arthroscopy within the study follow-up period (minimum of 2 years). We analysed both pre-operative and intra-operative variables to identify factors that influenced this outcome.
For all patients, cases and controls, a supine anterior-posterior (AP), pre-operative, pelvic radiograph was obtained. The use of CT scan was on a patient-by-patient basis and not routine in our practice. Each radiograph was analysed by a single orthopaedic resident (OD) using HipMorf software [13] to obtain the acetabular index (AI), head extrusion index (HEI), lateral CEA of Wiberg and alpha angle (αA). Hips were graded for features of osteoarthritis using the Kellgren-Lawrence system [14]. Corresponding MRI scans, which were available for 35 (79.5%) cases and 43 (65.2%) controls were also reviewed for labral pathology, evidence of cartilage damage and FAI. MRI scans were not available for some patients who were referred from regional hospitals for tertiary opinions. These scans were performed locally being available only on compact disc, pre-dating our institutions digital archiving of scans. The pre-operative diagnosis was obtained for all patients from the operative notes.
Inter- and intra-observer error was checked by using a randomly selected sample of 10 hips, which were re-analysed by the primary author (O.D.) and by a hip preservation fellow (G.G.).
Intra-operative features were identified by scrutinising the surgical records (intra-operative photographs and operation notes). A record was made of the types of procedures performed (e.g. microfracture, osteochondroplasty, etc.), and the presence and location of any acetabular cartilage damage as per the UCHL grading system. Presence of femoral head damage was also recorded as was the presence and location of any labral pathology.
Comparison was made between cases and controls for differences in the presence, extent and location of acetabular wear found at the time of arthroscopy. The presence of labral pathology was also compared between the two groups. We compared the two groups for the difference in dysplastic features (defined as AI >10° and CEA <25°) [15] on pre-operative radiographs. Sub-group analysis for combined effect of dysplastic features and cartilaginous wear was also performed.
Non-parametric, bivariate, regression analyses using Mann–Whitney U-tests and Chi-squared tests were performed for all categorical variables to identify if there were links to increased hip arthroscopy failure. Significance was set at P < 0.05. All statistical analysis was performed using SPSS, version 13, software (IBM, New York, USA).
RESULTS
Cases and controls were matched for age (mean = 44.7 versus 44.2 years, P = 0.59), sex (males: females = 10:34 versus 19:47, P = 0.48) and length of follow-up (70.8 months versus 63.5 months, P = 0.10) (Table I).
Table I.
Cohort characteristics
| Cohort | Cases | Controls | P-value | ||
|---|---|---|---|---|---|
| Mean age (years) | 44.38 | 44.73 | 44.15 | 0.59 | |
| Gender | Male | 29 | 10 | 19 | 0.48 |
| Female | 81 | 34 | 47 | ||
| Follow-up (months) | 66.41 | 70.8 | 63.48 | 0.096 | |
Radiographic analysis had both excellent intra- (k: 0.73–0.85, P = 0.001–0.003) and inter- (k: 0.71–0.82, P = 0.002–0.005) observer reliability. Cases had a lower CEA compared with controls (mean = 19.0° versus 25.5°, P < 0.001), higher AI (mean = 10.2° versus 5.9°, P < 0.001) and higher HEI (mean = 0.46 versus 0.32, P < 0.001). There was no significant difference in the Kellgren-Lawrence grade for the operated hip between cases and controls on pre-operative radiographs (P = 0.84).
For the 78 patients (70.9%) whom had a pre-arthroscopy MRI available, the MRI did not reveal any significant relationship between pathology identified and failure of arthroscopy (Table II), except for the presence of a labral tear that was subsequently found to be irreparable at the time of arthroscopy doubled the risk of the hip failing (risk ratio: 2.1; odds ratio: 4.67; P = 0.01).
Table II.
Pre-operative MRI findings
| Pathology | Cohort | Cases | Controls | P-value |
|---|---|---|---|---|
| Labral tear | 53 | 20 | 33 | 0.1 |
| Acetabular articular wear | 29 | 18 | 11 | 0.1 |
| FAI | 20 | 8 | 12 | 0.1 |
MRIs were available for 35 (79.8%) of cases and 44 (65.2%) of controls).
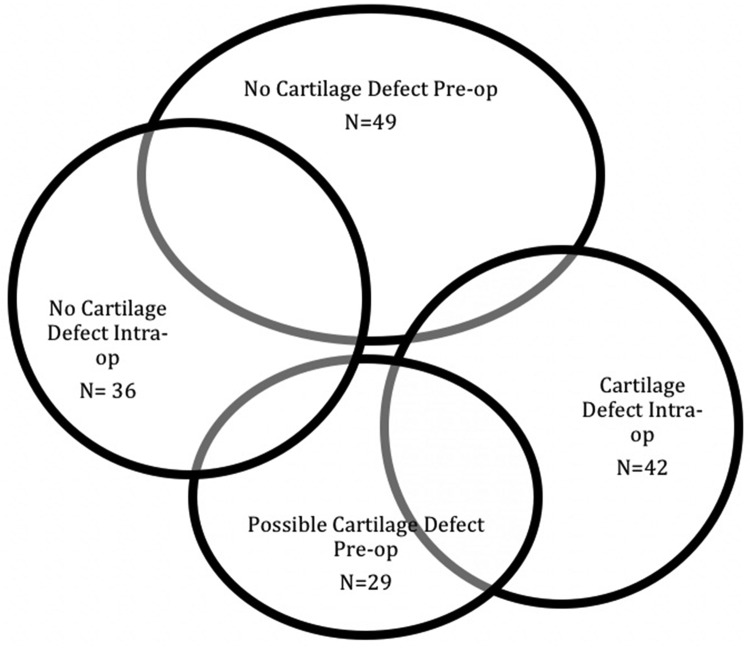
Comparison of pre-operative MRIs and the intra-operative findings revealed, 49 hips having no acetabular chondral damage pre-operatively with 31 of these hips having the same finding intra-operatively. In 18 cases acetabular wear was present on arthroscopy having not been identified on pre-operative MRI. Conversely, 29 MRIs showed a definite or possible cartilaginous lesion of the acetabulum, 24 of which were confirmed intra-operatively with only 5 hips having no acetabular wear (Fig. 1). The sensitivity and specificity of pre-arthroscopy MRI scans, in our series, for acetabular cartilaginous wear was 57.14% (CI: 40.96–72.28%) and 86.49% (71.23–95.46%), respectively.
Fig. 1.
Pre-operative MRI findings of acetabular cartilaginous wear compared with intra-operative findings of wear.
At arthroscopy presence of any acetabular cartilage wear (P < 0.001) and wear on the femoral head (P = 0.002) were both associated with increased risk of requiring subsequent arthroplasty. Cases had more extensive cartilaginous wear of the acetabulum than controls with a mean of 1.41 versus 0.58 UCHL zones [12]. There was a predominance of superior acetabular involvement in cases (mean = 0.89 versus 0.39 superior zones, P = 0.001). Thirty of the cases (68.1%) had at least 1 superior acetabular zone demonstrating wear compared with 19 (28.8%) of the controls.
Of the cases, 15 underwent a labral repair, 33 had an osteochondroplasty and 12 had a microfracture performed (compared with 31, 53 and 8, respectively for the control cohort). None of these interventions were found to significantly alter the risk for subsequent arthroplasty (Table III). Thirty-four and 43 other additional procedures were performed for cases and controls, respectively (Table IV); with no difference between the two groups (P = 0.2). Of note, one failed hip had an osteophytectomy, one an osteophytectomy and labral debridement and another two patients needed removal of loose bodies; none of the control cohort underwent any of these procedures.
Table III.
Operative findings and procedures performed at hip arthroscopy
| Cohort | Cases | Controls | P-value | ||
|---|---|---|---|---|---|
| Finding | Labral tear | 48 | 17 | 31 | 0.4 |
| Acetabular wear | 54 | 32 | 22 | <0.001 | |
| No. of hips with superior zone wear | 49 | 30 | 19 | <0.001 | |
| Femoral head wear | 41 | 24 | 17 | 0.002 | |
| Procedure | Labral Repair | 46 | 15 | 31 | 0.2 |
| Osteochondroplasty | 86 | 33 | 53 | 0.5 | |
| Microfracture | 20 | 12 | 8 | 0.0 | |
| Other | 77 | 33 | 44 | 0.2 | |
Table IV.
Other procedures performed at hip arthroscopy
| Procedure | Cohort | Cases | Controls | P-value |
|---|---|---|---|---|
| Synovectomy | 4 | 3 | 1 | 0.3 |
| Labral debridement | 45 | 17 | 29 | 0.57 |
| Rim-trim | 17 | 5 | 12 | 0.33 |
| Removal of loose body | 2 | 2 | 0 | — |
| Osteophytectomy | 1 | 1 | 0 | — |
| Labral debridement + osteophytectomy | 1 | 1 | 0 | — |
| Labral debridement + synovectomy | 3 | 2 | 1 | 0.34 |
| Rim-trim labral debridement | 3 | 2 | 1 | 0.34 |
Hips with both dysplastic features on pre-arthroscopy AP radiographs and also cartilaginous wear of the acetabulum at time of operation had the highest risk of failure in 21 (47.7%) of cases and only 6 (9%) of controls (P < 0.001). This represented a 5-fold increased risk of requiring a subsequent arthroplasty (odds ratio: 9.13, P < 0.001). The best chance for survival was seen in hips that had no dysplasia (defined as LCEA <25° and/or AI >10° [15, 16]) and no wear (relative risk = 5, odds ratio = 0.11, P < 0.001).
DISCUSSION
Our retrospective study of 110 patients confirms that the presence of cartilaginous wear and hip dysplasia predispose patients to early hip arthroplasty following arthroscopy, with the presence of both conferring a 5-fold increased risk of subsequent arthroplasty.
Wear in the superior zones of the acetabulum was more prevalent among our failed cohort of patients. This observation possibly results from the increased dysplastic features seen in our failed hips as resultant under-coverage will lead to rim loading and wear in superior zones [17, 18], particularly UCLH zone 2. This is contrary to Dwyer et al. [19], who reported that anterior acetabular wear increased the risk of needing an arthroplasty procedure but superior wear was not an independent risk factor.
Features of dysplasia on pre-operative radiographs seem to suggest limited success for hip arthroscopy; Larson et al. [20] showed that the more severe the dysplasia, the less the likelihood that arthroscopy can be effective as hip preserving surgery. This, however, appears to represent a point on a spectrum and we feel that hip arthroscopy still has a role in the management of patients with mild dysplasia although this needs further exploration [21].
Intra-operatively we found that the presence of chondral lesions was the feature most likely to predispose to failure of arthroscopy. The detection of these lesions on pre-operative MRI was limited; our series showed a sensitivity of 57.1% and specificity 86.5% for detection of acetabular wear. This is not dissimilar from previously reported rates of cartilage lesion detection [22–24], which similarly used 1.5-Tesla MRI scanners with a variety of unenhanced and enhanced techniques. With the continuing improvement of MRI modalities for imaging the hip, especially the use of dGEMERIC sequencing [25, 26], T2 mapping [26, 27] and 3-Tesla MRI [28], pre-operative identification of chondral pathology may be improved so helping to guide surgical treatment.
Haviv et al. [5] reported a retrospective case series of 564 hip arthroscopies with mean follow-up of 3.2 years and a 16% conversion rate to total hip arthroplasty. This study was claimed to demonstrate that patients with more significant degenerative changes had a shorter time interval to arthroplasty but 75% of patients with severe osteoarthritis did not require arthroplasty. Our study did demonstrate a significant correlation between degenerative changes at arthroscopy and the requirement for arthroplasty.
A review of six studies [5, 8, 9, 11, 29, 30] in 2013 by McCarthy and Mc Millan [31] concluded that OA was the biggest predictor of a failed hip arthroscopy. These same studies reported a wide range in conversion rate to THR from 9% [8, 30] to 37% [11]. Our series had a failure rate at the lower end of this range (12.8%). Egerton et al. [32] investigated the influence of cartilage wear on outcome scores following hip arthroscopies. Using the modified Harris hip score and non-arthritic hip score (NAHS), they described an overall improvement in both scoring systems following hip arthroscopy in 560 patients although this was less in patients with cartilage defects.
Acetabular dysplasia has been reported to negatively influence outcomes of hip arthroscopy. Ross et al. [33] looked at 30 hips that failed hip arthroscopy requiring peri-acetabular osteotomy. They found that that these patients had an average CEA of 14.7° and acetabular inclination of 16.3°. Other studies [19] have demonstrated some success with hip arthroscopy for mild dysplasia when the presence of cartilage wear did predict the need for THR at a mean interval of 2.7(±2.3) years.
Our study has some limitations. Our study was predominantly a single surgeon series and so may not be representative of the ‘global’ hip arthroscopy practice. Second, we have not been able to fully determine whether patients who went onto arthroplasty had any symptomatic improvement post-arthroscopy prior to their arthroplasty procedure. We have hip disability and osteoarthritis outcome scores (HOOS) and NAHS for 17 of the 44 cases but as this represents only 38.6% of the cases and lack control comparators so we did not include these in our final analysis. Where available for cases there was a fall in their HOOS scores post-arthroscopy but an improvement in their NAHS (−6.88 points and +8.67 points, respectively, Table V). HOOS has a minimal clinically important difference for hip arthroscopy of 9 and 6 for activities of daily living and sports, respectively [34]. Prospective collection of patient-reported outcome measures (PROMs) pre- and post-arthroscopy would overcome this limitation, as ultimately it is the patient who truly decides if a procedure is successful or not. Finally, performing a retrospective analysis meant determining a patient’s exact primary presenting symptom was not possible, for example a young patient with degenerative changes of the hip may have primarily complained of mechanical symptoms rather than pain thus indicating that a hip arthroscopy rather than an arthroplasty procedure would be of benefit. Features such as this could cause selection bias in our failed cases.
Table V.
PROMs for cases
| HOOS | HOOS-SF | NAHS | |
|---|---|---|---|
| Mean score pre-arthroscopy | 53.53 | 49.39 | 41.06 |
| Mean score post-arthroscopy | 46.65 | 41.76 | 47.41 |
| Mean change in score | −6.88 | −7.19 | +8.76 |
HOOS, hip disability and osteoarthritis outcome score; HOOS-SF, short form hip disability and osteoarthritis outcome score; NAHS, non-arthritic hip score.
This study demonstrates that both dysplastic features present on the pre-operative radiographs and articular wear present at arthroscopy greatly increase the risk of subsequent arthroplasty; the combination of dysplasia with articular wear incurs a 5-fold increased risk. Identifying these features pre-operatively will aim to improve the results of hip arthroscopy as joint preserving surgery; however, the limitations of pre-operative imaging techniques currently make this challenging.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Group NU. The Non-Arthroplasty Hip Registry 2016 Annual Report, British Hip Society, 2016. [Google Scholar]
- 2. Bozic KJ, Chan V, Valone FH.. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013; 28: 140–3. [DOI] [PubMed] [Google Scholar]
- 3. Lynch TS, Terry MA, Bedi A. et al. Hip arthroscopic surgery: patient evaluation, current indications, and outcomes. Am J Sports Med 2013; 41: 1174–89. [DOI] [PubMed] [Google Scholar]
- 4. Horner NS, Ekhtiari S, Simunovic N. et al. Hip arthroscopy in patients age 40 or older: a systematic review. Arthroscopy 2017; 33: 464–75.e3. [DOI] [PubMed] [Google Scholar]
- 5. Haviv B, O'Donnell J.. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. Sport Med Arthrosc Rehabil Ther Technol 2010; 2: 18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schairer WW, Nwachukwu BU, McCormick F. et al. Use of hip arthroscopy and risk of conversion to total hip arthroplasty: a population-based analysis. Arthroscopy 2016; 32: 587.. [DOI] [PubMed] [Google Scholar]
- 7. Harris JD, McCormick FM, Abrams GD. et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthrosc J Arthrosc Relat Surg 2013; 29: 589–95. [DOI] [PubMed] [Google Scholar]
- 8. Philippon MJ, Yen Y-M, Briggs KK. et al. Early outcomes after hip arthroscopy for femoroacetabular impingement in the athletic adolescent patient: a preliminary report. J Pediatr Orthop 2008; 28: 705–10. [DOI] [PubMed] [Google Scholar]
- 9. Philippon MJ, Schroder BG, Briggs KK.. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthrosc J Arthrosc Relat Surg 2012; 28: 59–65. [DOI] [PubMed] [Google Scholar]
- 10. Saadat E, Martin SD, Thornhill TS. et al. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med 2014; 42: 1487–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. McCarthy JC, Jarrett BT, Ojeifo O. et al. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res 2011; 469: 362–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Konan S, Rayan F, Meermans G. et al. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br 2011; 93: 332–6. [DOI] [PubMed] [Google Scholar]
- 13. Nicholls AS, Kiran A, Pollard TCB. et al. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum 2011; 63: 3392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kellgren JH, Lawrence JS.. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957; 16: 494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gala L, Clohisy JC, Beaulé PE.. Hip dysplasia in the young adult. J Bone Surg 2016; 98: 63–73. [DOI] [PubMed] [Google Scholar]
- 16. Byrd JWT, Jones KS.. Hip arthroscopy in the presence of dysplasia. Arthrosc J Arthrosc Relat Surg 2003; 19: 1055–60. [DOI] [PubMed] [Google Scholar]
- 17. Klaue K, Durnin CW, Ganz R.. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991; 73: 423–9. [DOI] [PubMed] [Google Scholar]
- 18. Ganz R, Leunig M, Leunig-Ganz K. et al. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466: 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dwyer MK, Lee JA, McCarthy JC.. Cartilage status at time of arthroscopy predicts failure in patients with hip dysplasia. J Arthroplasty 2015; 30: 121–4. [DOI] [PubMed] [Google Scholar]
- 20. Larson CM, Ross JR, Stone RM. et al. Arthroscopic management of dysplastic hip deformities: predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med 2016; 44: 447–53. [DOI] [PubMed] [Google Scholar]
- 21. Grammatopoulos G, Davies OLI, El-Bakoury A. et al. A traffic light grading system of hip dysplasia to predict the success of arthroscopic hip surgery. Am J Sports Med 2017; 45: 2891–900. [DOI] [PubMed] [Google Scholar]
- 22. Czerny C, Hofmann S, Neuhold A. et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 1996; 200: 225–30. [DOI] [PubMed] [Google Scholar]
- 23. Keeney JA, Peelle MW, Jackson J. et al. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res 2004; 429: 163–9. [DOI] [PubMed] [Google Scholar]
- 24. Knuesel PR, Pfirrmann CWA, Noetzli HP. et al. MR arthrography of the hip: diagnostic performance of a dedicated water-excitation 3D double-echo steady-state sequence to detect cartilage lesions. Am J Roentgenol 2004; 183: 1729–35. [DOI] [PubMed] [Google Scholar]
- 25. Bulat E, Bixby SD, Siversson C. et al. Planar dGEMRIC maps may aid imaging assessment of cartilage damage in femoroacetabular impingement. Clin Orthop Relat Res 2016; 474: 467–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bittersohl B, Miese FR, Dekkers C. et al. T2* mapping and delayed gadolinium-enhanced magnetic resonance imaging in cartilage (dGEMRIC) of glenohumeral cartilage in asymptomatic volunteers at 3 T. Eur Radiol 2013; 23: 1367–74. [DOI] [PubMed] [Google Scholar]
- 27. Ho CP, Surowiec RK, Ferro FP. et al. Subregional anatomical distribution of T2 values of articular cartilage in asymptomatic hips. Cartilage 2014; 5: 154–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Linda DD, Naraghi A, Murnaghan L. et al. Accuracy of non-arthrographic 3T MR imaging in evaluation of intra-articular pathology of the hip in femoroacetabular impingement. Skeletal Radiol 2017; 46: 299–308. [DOI] [PubMed] [Google Scholar]
- 29. Byrd JWT, Jones KS.. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res 2010; 468: 741–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Larson CM, Giveans MR, Taylor M.. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res 2011; 469: 1667–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McCarthy J, Mc Millan S.. Arthroscopy of the hip. Factors affecting outcome. Orthop Clin North Am 2013; 44: 489–98. [DOI] [PubMed] [Google Scholar]
- 32. Egerton T, Hinman RS, Takla A. et al. Intraoperative cartilage degeneration predicts outcome 12 months after hip arthroscopy hip. Clin Orthop Relat Res 2013; 471: 593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ross JR, Clohisy JC, Baca G. et al. Patient and disease characteristics associated with hip arthroscopy failure in acetabular dysplasia. J Arthroplasty 2014; 29: 160–3. [DOI] [PubMed] [Google Scholar]
- 34. Martin RL, Philippon MJ.. Evidence of reliability and responsiveness for the hip outcome score. Arthrosc J Arthrosc Relat Surg 2008; 24: 676–82. [DOI] [PubMed] [Google Scholar]