ABSTRACT
Periacetabular osteotomy (PAO) remains the gold standard procedure for joint preservation in symptomatic developmental dysplasia of the hip (DDH). Hip arthroscopy (HA) and open arthrotomy have been used to correct intra-articular pathology at the time of PAO, but there is limited data regarding differences in outcomes between these techniques when performed at the time of PAO. The aim of this study was to determine if short-term clinical outcomes differed between patients managed with HA versus arthrotomy to evaluate and treat intra-articular pathology at the time of PAO to discern if one technique is associated with better pain and functional results. Data were retrospectively reviewed from two surgeons at one institution managing DDH patients from September 2013 to December 2015. One surgeon treated patients with PAO and arthrotomy (N = 32), while the other performed PAO and HA (N = 39). There were 87% women, median age was 28 years and mean BMI was 25. Seventy-five percent of all patients received an intra-articular intervention. Patients completed 13 PROs at the pre-operative and 1-year post-operative clinical visits. Pre-operatively, there were no differences in any of the 13 PROs between patients treated with HA versus arthrotomy (P ≥ 0.076). Patients treated with PAO and arthrotomy experienced greater mean improvement in two out of the 13 PROs; the other 11 showed no differences. No treatment effect was observed for any of the 13 PROs using multivariable modelling that accounted for severity of dysplasia and degree of arthritis. Few differences were shown in short-term clinical outcomes between HA and arthrotomy at the time of PAO. This work highlights the need for a high quality randomized clinical trial to provide definitive guidance on whether hip preservation surgeons should address intra-articular pathology at the time of PAO for DDH and which technique best serves this purpose.
INTRODUCTION
The Bernese periacetabular osteotomy (PAO) remains the gold standard for treatment of symptomatic developmental dysplasia of the hip (DDH) in skeletally mature patients. First developed by Ganz in 1984, this technique utilizes four osteotomies to completely mobilize the acetabular fragment [1]. Although a technically demanding procedure, it allows for optimal correction in all planes and maintains integrity of the posterior column, enabling early weight bearing and mobilization. Several groups have confirmed the long-term efficacy of this joint preservation procedure with a recent report from the originating institution documenting survivorship up to 30 years after surgery [2]. Concomitant intra-articular pathology, primarily cartilage and labral damage, occurs with high prevalence in patients with DDH, presumed secondary to the inherent instability and altered biomechanics of the dysplastic hip [3, 4]. In addition, proximal femoral deformity often coexists in patients with dysplasia and may require treatment at the time of PAO to maintain normal range of motion following acetabular re-orientation.
Treatment of intra-articular pathology during PAO was first described with an arthrotomy [5]. This technique is facile and does not add significant time to a case nor does it require extra equipment and preparation. However, arthrotomy yields limited exposure to the joint and thus restricts access to appropriately diagnose and treat intra-articular structures. An alternative to arthrotomy is hip arthroscopy (HA), which has recently been described for the management of intra-articular disease during PAO [6]. Arthroscopy allows a comprehensive view of the intra-articular compartment and ability to address disease, but requires specialized training and equipment as well as additional preparation and case time, all while carrying a unique set of potential complications. Both techniques allow for femoral head neck junction osteochondroplasty in order to maintain range of motion after PAO.
Currently, there is insufficient evidence to confirm benefit from assessment and treatment of intra-articular pathology at the time of PAO, whether through open or arthroscopic techniques. Recently, a prospective report of 95 hips undergoing PAO without simultaneous interrogation of the joint showed that 27% of patients returned within 2 years and subsequently underwent arthroscopy to treat labral pathology or cam lesions [7]. Pre-operative magnetic resonance arthrogram (MRA) revealed labral pathology in 94% of all patients in that study, but not all patients required management as more than 70% of the hips did not require subsequent treatment of labral pathology, adding further data to the fact that the PAO is able to provide labral offloading and pain relief even in the presence of a labral tear. However, those that did require treatment after PAO had lower patient-reported outcome (PRO) scores at 2-year follow-up. While intuitive to address structural abnormalities and potential pain generators in patients with DDH, an arthrotomy or HA requires further disruption of the joint and may potentially lead to further instability, iatrogenic damage to intra-articular cartilage, adhesions or heterotopic ossification. It therefore remains unclear which patients are most likely to benefit from treatment of labral or cartilage disease and which technique is best suited for treatment. The aim of this study was to determine if short-term clinical outcomes differed between patients managed with HA versus arthrotomy to evaluate and treat intra-articular pathology at the time of PAO to discern if one technique is associated with better pain and functional results.
MATERIALS AND METHODS
This retrospective cohort study was conducted from September 2013 to December 2015 and was approved by our institutional review board. All patients were treated at Mayo Clinic, Rochester, Minnesota, by 1 of 2 senior hip preservation surgeons (R.T.T. and R.J.S.).
During this time period, a subset of patients scheduled to undergo PAO for DDH were treated with either simultaneous HA or arthrotomy. One surgeon treated all of their patients that met study inclusion criteria with PAO and HA, whereas the other surgeon treated all eligible patients with PAO and arthrotomy. Candidates for PAO had closed triradiate cartilage and symptomatic DDH defined by a lateral center-edge angle (LCEA) as described by Wiberg [8] of <25° and/or an acetabular index as described by Tönnis [9] of >10°. An anterior center-edge angle <25° was also considered dysplastic [10]. Patients were further considered if they were ≤50 years old and had Grade 0 or Grade 1 degenerative changes according to Tönnis [9]. No patients were included with previous surgery about the hip, isolated acetabular retroversion, neurogenic dysplasia, Legg-Calvé-Perthes or slipped capital femoral epiphysis. During the study period, 87 patients (89 hips) underwent PAO with the aforementioned criteria. PROs were completed both pre-operatively and 1 year post-operatively by 70 patients (71 hips) (80%), which comprised the final cohort.
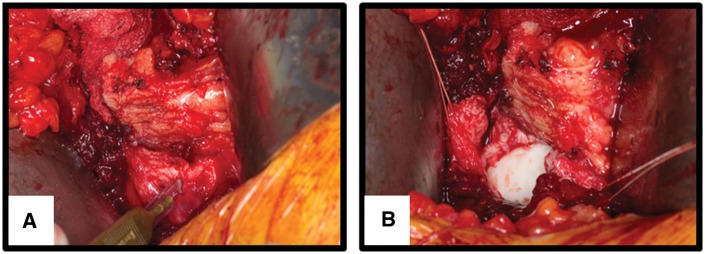
One surgeon (R.T.T.) treated all eligible patients with a PAO followed by open arthrotomy to address any visible intra-articular pathology (N = 32 hips) (Fig. 1). The second surgeon (R.J.S.) treated all eligible patients with HA prior to PAO to address any visible intra-articular pathology (N = 39) (Fig. 2). Patients underwent identical routine perioperative in-hospital care and post-operative follow-up per institutional protocol. The intra-articular treatments included labral repair, labral debridement, osteochondroplasty and acetabular or femoral chondroplasty. For the purposes of classification and sensitivity analyses, labral repair and femoral head–neck junction osteochondroplasty were considered to be ‘major’ interventions, whereas labral debridement and acetabular or femoral chondroplasty were considered to be ‘minor’ interventions. Major and/or minor interventions were performed on 53 hips (75%) overall, 38 hips (97%) in the HA group and 15 hips (47%) in the arthrotomy group (Table I). Major interventions were performed on 31 hips (44%) overall, 26 hips (67%) in the HA group and 5 hips (16%) in the arthrotomy group (Table I). A head and neck osteochondroplasty was performed prior to reorientation in 12 hips undergoing PAO and HA and 2 hips undergoing PAO and arthrotomy. All patients with a pre-operative cam deformity or elevated alpha angle had this addressed with osteochondroplasty. Pre-operative MRI was performed on 52 patients and demonstrated evidence of labral pathology in 47 patients (90%). Among those 47 patients, 36 (77%) had subsequent identification and treatment of the tear intraoperatively with either debridement or formal repair.
Fig. 1.
This intraoperative photograph demonstrates the open arthrotomy technique utilized following completion of the PAO (A). A labral tear is seen from 11:00 to 1:00, which was debrided before capsule closure (B).
Fig. 2.
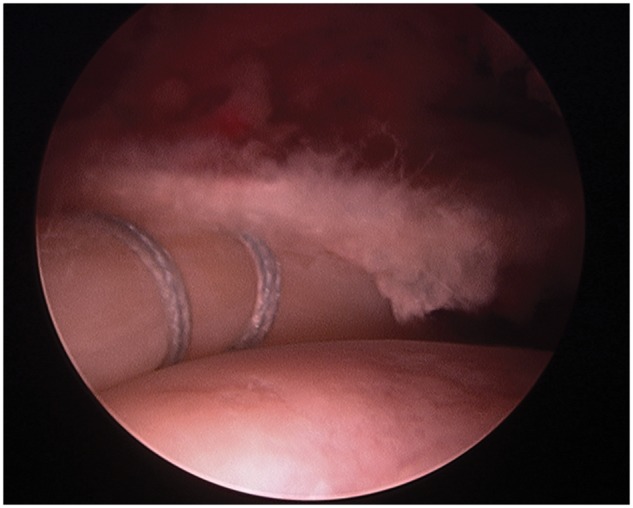
This intraoperative photograph demonstrates the arthroscopic technique utilized to assess intra-articular pathology, which identified a labral tear in this patient that was repaired before beginning the PAO.
Table I.
Demographics and patient characteristics
| Characteristic | Entire cohort (N = 71) | PAO+HA (N = 39) | PAO+arthrotome (N = 32) | P-Value |
|---|---|---|---|---|
| Gender | 0.968a | |||
| Female | 62 (87%) | 34 (87%) | 28 (88%) | |
| Male | 9 (13%) | 5 (13%) | 4 (13%) | |
| Age | 0.798b | |||
| Mean (SD) | 27.3 (7.2) | 27.1 (7.4) | 27.6 (7.1) | |
| Median | 27.8 | 26.6 | 28.9 | |
| Range | (15.2–41.7) | (15.2–41.3) | (15.3–41.7) | |
| Body mass index | 0.428b | |||
| Mean (SD) | 25.1 (4.9) | 25.5 (5.1) | 24.6 (4.7) | |
| Median | 24.3 | 25.0 | 23.7 | |
| Range | (16.9–39.2) | (16.9–38.1) | (18.3–39.2) | |
| Diagnosis | 0.406a | |||
| DDH alone | 67 (94%) | 36 (92%) | 31 (97%) | |
| DDH+retroversion | 4 (6%) | 3 (8%) | 1 (3%) | |
| Intra-articular intervention | <0.001a | |||
| Majorcand/or minord | ||||
| Intervention not performed | 18 (25%) | 1 (3%) | 17 (53%) | |
| Intervention performed | 53 (75%) | 38 (97%) | 15 (47%) | |
| Majorcintra-articular intervention | <0.0011 | |||
| No major intervention | 40 (56%) | 13 (33%) | 27 (84%) | |
| Major intervention | 31 (44%) | 26 (67%) | 5 (16%) |
aχ2.
bUnequal variance t test.
cLabral repair, Osteochondroplasty.
dLabral debridement, Chondroplasty.
DDH, developmental dysplasia of the hip; PAO, periacetabular osteotomy.
Patients filled out 13 PROs at the pre-operative and 1 year post-operative clinical visits as part of a prospectively collected hip preservation registry. PROs included the Harris Hip Score; UCLA Activity Score; all five subcomponents of the Hip Disability and Osteoarthritis Outcome Score (HOOS) [Pain, Symptom, Activities of Daily Living (ADL), Sports and Recreation, Quality of Life]; all four subcomponents of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (Pain, Stiffness, Physical, Total) and both subcomponents of the SF-12 (Physical and Mental).
There were 62 women (87%) and 9 men (13%), median age was 28 years (range 15–42 years) and mean BMI was 25.1 (range 16.9–39.2) (Table I). Four patients (6%) had concomitant acetabular retroversion and DDH (Table I). There were no major differences at the time of surgery between the HA and arthrotomy groups based on age, BMI or gender (Table I). All three radiographic measures, namely LCEA, Tönnis Grade and Tönnis angle differed between the two treatment groups. The open arthrotomy group had a lower mean LCEA (14.6 versus 17.6, P = 0.02) and lower Tönnis Grade (Grade 0: 81% versus 59%, P = 0.04), and a significantly higher mean Tönnis angle (20.1 versus 14.1 P < 0.001) than the HA group (Table II). In order to account for these differences, the association of surgical technique and the pre-operative to post-operative changes in PROs were analysed using multivariable models which included the three above-mentioned radiographic measures as adjusting covariates.
Table II.
Radiographic parameters
| Radiographic metric | Entire cohort (N = 71) | PAO+HA (N = 39) | PAO+arthrotomy (N = 32) | P-Value |
|---|---|---|---|---|
| LCEA (pre-operative) | 0.021a | |||
| N | 71 | 39 | 32 | |
| Mean (SD) | 16.3 (6.1) | 17.6 (5.8) | 14.6 (6.2) | |
| Median | 18.0 | 19.0 | 15.0 | |
| Range | (−3.0 to 25.0) | (-3.0 to 25.0) | (0.0 to 23.0) | |
| LCEA (post-operative) | 0.112a | |||
| N | 51 | 25 | 26 | |
| Mean (SD) | 31.5 (6.1) | 29.8 (4.9) | 33.2 (6.7) | |
| Median | 30.0 | 30.0 | 33.5 | |
| Range | (14.0 to 47.0) | (14.0 to 39.0) | (22.0 to 47.0) | |
| Tönnis angle (pre-operative) | <0.001a | |||
| N | 71 | 39 | 32 | |
| Mean (SD) | 16.8 (9.6) | 14.1 (10.6) | 20.1 (7.2) | |
| Median | 14.0 | 11.0 | 20.5 | |
| Range | (5.0 to 71.0) | (5.0 to 71.0) | (6.6 to 35.0) | |
| Tönnis angle (post-operative) | <0.001a | |||
| N | 51 | 25 | 26 | |
| Mean (SD) | 5.5 (5.6) | 2.2 (3.9) | 8.7 (5.1) | |
| Median | 5.0 | 0.0 | 8.7 | |
| Range | (0.0 to 20.0) | (0.0 to 16.0) | (0.0 to 20.0) | |
| Tönnis Grade (pre-operative) | 0.042b | |||
| 0 | 49 (69%) | 23 (59%) | 26 (81%) | |
| 1 | 22 (31%) | 16 (41%) | 6 (19%) | |
| Tönnis Grade (post-operative) | 0.189b | |||
| 0 | 45 (88%) | 20 (80%) | 25 (96%) | |
| 1 | 6 (12%) | 5 (20%) | 1 (4%) |
aWilcoxon.
bχ2.
PAO, periacetabular osteotomy; HA, hip arthroscopy.
The data are summarized using means and standard deviations for variables comprised of continuous data, and counts and percentages for categorical variables. Comparisons of the PROs between the pre-operative and 1-year follow-up time points for the entire cohort were performed using paired t-tests. Patients treated with HA were compared with those treated with open arthrotomy with respect to patient characteristics, including age, gender, body mass index and diagnosis (acetabular retroversion versus DDH) using two-sample t-tests for continuous data and χ2 tests for binary variables. Changes in the PROs from baseline (pre-operative) to 1-year follow-up were compared between the HA and open arthrotomy groups using two-sample t-tests. Similar analyses were performed to evaluate other factors such as gender, age group, body mass index and presence of acetabular retroversion. Univariate regression analysis was performed to explore relationships between radiographic parameters such as LCEA, Tönnis angle, Tönnis Grade and PROs. Subsequently, multivariable regression analysis was performed in order to account for differences in pre-operative radiographic measures between treatment groups. Specifically, the association of surgical technique and the pre-operative to 1-year follow-up change in PROs were adjusted for pre-operative LCEA, Tönnis angle and Tönnis Grade. These three radiographic parameters were incorporated into the models as adjusting covariates individually as well as simultaneously. All statistical tests were two-sided and P-values <0.05 were considered significant. The analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA) and R version 3.4.1 (R Core Team, 2017, R Core Team, Vienna, Austria).
RESULTS
Pre-operatively, there were no differences in any of the 13 PROs between patients treated with HA versus arthrotomy (P ≥ 0.076) (Table III). All PROs with the exception of SF-12 Mental subscale (P = 0.897) improved for the entire cohort post-operatively (P < 0.01) (Table IV). Patients treated with arthrotomy experienced a greater mean increase from baseline in HOOS Pain and HOOS Quality of Life; the other 11 PROs showed no difference between groups (Table V).Women demonstrated greater mean improvement than men in 7 of 13 PROs; the other 6 PROs showed no difference between groups (Table VI). There was no difference in PROs based on whether intra-articular intervention was performed (Table VII). Furthermore, no relationship was shown between the pre-operative and post-operative change in PROs based on the presence of concomitant acetabular retroversion, age or BMI. Multivariable analysis accounting for LCEA, Tönnis angle and Tönnis Grade showed no significant effect of surgical technique for any of the 13 PROs (P ≥ 0.061).
Table III.
Pre-operative PROs based on treatment algorithm
| Pre-operative score | PAO+HA (N=39) | PAO+ arthrotomy (N=32) | P-Value |
|---|---|---|---|
| UCLA score | 0.152a | ||
| Mean (SD) | 6.0 (2.7) | 6.9 (2.7) | |
| Median | 6.0 | 7.0 | |
| Range | (2.0 to 10.0) | (3.0 to 10.0) | |
| Harris hip score | 0.520a | ||
| Mean (SD) | 59.7 (15.8) | 62.3 (17.5) | |
| Median | 64.9 | 62.7 | |
| Range | (19.8 to 84.7) | (19.8 to 97.9) | |
| HOOS—Pain | 0.941a | ||
| Mean (SD) | 53.8 (17.3) | 54.2 (22.9) | |
| Median | 60.0 | 57.5 | |
| Range | (5.0 to 85.0) | (12.5 to 92.5) | |
| HOOS—Symptom | 0.653a | ||
| Mean (SD) | 51.3 (20.0) | 53.5 (20.7) | |
| Median | 55.0 | 55.0 | |
| Range | (5.0 to 100.0) | (0.0 to 90.0) | |
| HOOS—ADL | 0.926a | ||
| Mean (SD) | 66.1 (20.3) | 66.6 (24.3) | |
| Median | 68.4 | 72.8 | |
| Range | (13.2 to 95.6) | (23.5 to 100.0) | |
| HOOS—Sport/Rec | 0.498a | ||
| Mean (SD) | 37.3 (22.3) | 41.5 (26.5) | |
| Median | 37.5 | 40.6 | |
| Range | (0.0 to 81.3) | (0.0 to 87.5) | |
| HOOS—QOL | 0.909a | ||
| Mean (SD) | 28.5 (18.5) | 29.0 (18.2) | |
| Median | 25.0 | 31.3 | |
| Range | (0.0 to 62.5) | (0.0 to 62.5) | |
| WOMAC—Pain | 0.726a | ||
| Mean (SD) | 60.0 (18.5) | 58.1 (24.2) | |
| Median | 65.0 | 60.0 | |
| Range | (10.0 to 90.0) | (15.0 to 95.0) | |
| WOMAC—Stiffness | 0.862a | ||
| Mean (SD) | 51.0 (23.7) | 52.0 (26.0) | |
| Median | 50.0 | 50.0 | |
| Range | (0.0 to 100.0) | (0.0 to 100.0) | |
| WOMAC—Physical | 0.926a | ||
| Mean (SD) | 66.1 (20.3) | 66.6 (24.3) | |
| Median | 68.4 | 72.8 | |
| Range | (13.2 to 95.6) | (23.5 to 100.0) | |
| WOMAC—Total | 0.936a | ||
| Mean (SD) | 63.9 (19.2) | 63.5 (23.7) | |
| Median | 68.2 | 69.8 | |
| Range | (12.5 to 91.7) | (20.8 to 96.9) | |
| SF-12 physical | 0.076a | ||
| Mean (SD) | 35.6 (9.4) | 40.3 (12.0) | |
| Median | 34.2 | 42.1 | |
| Range | (19.6 to 52.6) | (17.4 to 61.0) | |
| SF-12 mental | 0.888a | ||
| Mean (SD) | 52.9 (9.5) | 53.3 (10.2) | |
| Median | 54.1 | 55.1 | |
| Range | (24.0 to 68.8) | (32.0 to 69.3) |
aUnequal variance t test.
PAO, periacetabular osteotomy; HA, hip arthroscopy; HOOS, Hip Disability and Osteoarthritis Outcome Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; ADL, Activity of Daily Living; QOL, quality of life.
Table IV.
Pre-operative versus 1-year follow-up PROs
| PRO metric | Pre-operative (N = 71) | Post-operative (N = 71) | P-Value |
|---|---|---|---|
| UCLA score | 0.006a | ||
| Mean (SD) | 6.4 (2.7) | 7.3 (2.2) | |
| Median | 6.0 | 7.0 | |
| Range | (2.0–10.0) | (3.0–10.0) | |
| Harris hip score | <0.001b | ||
| Mean (SD) | 60.9 (16.5) | 84.7 (16.2) | |
| Median | 63.8 | 91.3 | |
| Range | (19.8–97.9) | (34.1–100.1) | |
| HOOS—Pain | <0.001b | ||
| Mean (SD) | 54.0 (19.7) | 81.8 (18.9) | |
| Median | 57.5 | 86.3 | |
| Range | (5.0–92.5) | (17.5–100.0) | |
| HOOS—Symptom | <0.001b | ||
| Mean (SD) | 52.3 (20.2) | 74.8 (21.1) | |
| Median | 55.0 | 80.0 | |
| Range | (0.0–100.0) | (10.0–100.0) | |
| HOOS—ADL | <0.001a | ||
| Mean (SD) | 66.3 (22.0) | 88.0 (16.8) | |
| Median | 69.9 | 95.6 | |
| Range | (13.2–100.0) | (32.4–100.0) | |
| HOOS—Sports/Rec | <0.001b | ||
| Mean (SD) | 39.2 (24.1) | 72.4 (27.8) | |
| Median | 37.5 | 81.3 | |
| Range | (0.0–87.5) | (0.0–100.0) | |
| HOOS—QOL | <0.001b | ||
| Mean (SD) | 28.8 (18.2) | 67.0 (24.2) | |
| Median | 31.3 | 68.8 | |
| Range | (0.0–62.5) | (0.0–100.0) | |
| WOMAC—Pain | <0.001b | ||
| Mean (SD) | 59.2 (21.0) | 85.9 (17.2) | |
| Median | 65.0 | 90.0 | |
| Range | (10.0–95.0) | (25.0–100.0) | |
| WOMAC—Stiffness | <0.001a | ||
| Mean (SD) | 51.4 (24.6) | 77.6 (22.8) | |
| Median | 50.0 | 75.0 | |
| Range | (0.0–100.0) | (12.5–100.0) | |
| WOMAC—Physical | <0.001a | ||
| Mean (SD) | 66.3 (22.0) | 88.9 (16.2) | |
| Median | 69.9 | 95.6 | |
| Range | (13.2–100.0) | (32.4–100.0) | |
| WOMAC—Total | <0.001b | ||
| Mean (SD) | 63.8 (21.2) | 86.7 (16.9) | |
| Median | 68.8 | 92.7 | |
| Range | (12.5–96.9) | (29.2–100.0) | |
| SF-12 physical | <0.001b | ||
| Mean (SD) | 37.7 (10.8) | 48.6 (11.0) | |
| Median | 37.1 | 51.9 | |
| Range | (17.4–61.0) | (16.4–69.0) | |
| SF-12 mental | 0.897b | ||
| Mean (SD) | 53.1 (9.8) | 52.9 (10.4) | |
| Median | 54.6 | 56.7 | |
| Range | (24.0–69.3) | (14.9–68.2) |
aWilcoxon signed-rank test.
bPaired t test.
HOOS, Hip Disability and Osteoarthritis Outcome Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; ADL, Activity of Daily Living; QOL, quality of life.
Table V. .
PROs based on surgical technique
| Pre-op to post-op change | PAO+HA (N = 39) | PAO+ arthrotomy (N = 32) | P-Value |
|---|---|---|---|
| UCLA score | 0.788a | ||
| Mean (SD) | 0.9 (2.7) | 1.0 (2.4) | |
| Median | 1.0 | 0.0 | |
| Range | (−4.0 to 6.0) | (−4.0 to 6.0) | |
| Harris hip score | 0.351a | ||
| Mean (SD) | 22.1 (14.7) | 26.0 (18.6) | |
| Median | 22.0 | 23.7 | |
| Range | (−6.6 to 57.2) | (0.0 to 64.9) | |
| HOOS—Pain | 0.043a | ||
| Mean (SD) | 23.6 (19.3) | 34.7 (21.5) | |
| Median | 25.0 | 35.0 | |
| Range | (−20.0 to 65.0) | (−10.0 to 72.5) | |
| HOOS—Symptom | 0.192a | ||
| Mean (SD) | 18.4 (24.0) | 27.1 (18.9) | |
| Median | 20.0 | 25.0 | |
| Range | (−25.0 to 50.0) | (−10.0 to 70.0) | |
| HOOS—ADL | 0.137a | ||
| Mean (SD) | 17.0 (20.3) | 24.8 (20.2) | |
| Median | 15.4 | 22.1 | |
| Range | (−42.6 to 50.0) | (0.0 to 72.1) | |
| HOOS—Sport/Rec | 0.492a | ||
| Mean (SD) | 29.8 (30.2) | 35.2 (30.5) | |
| Median | 31.3 | 37.5 | |
| Range | (−31.3 to 93.8) | (−43.8 to 87.5) | |
| HOOS—QOL | 0.043a | ||
| Mean (SD) | 32.6 (26.0) | 45.0 (23.0) | |
| Median | 31.3 | 43.8 | |
| Range | (−12.5 to 93.8) | (6.3 to 93.8) | |
| WOMAC—Pain | 0.056a | ||
| Mean (SD) | 22.4 (20.4) | 32.6 (21.1) | |
| Median | 25.0 | 30.0 | |
| Range | (−20.0 to 65.0) | (0.0 to 75.0) | |
| WOMAC—Stiffness | 0.081a | ||
| Mean (SD) | 21.2 (26.4) | 32.3 (24.7) | |
| Median | 25.0 | 25.0 | |
| Range | (−50.0 to 75.0) | (−25.0 to 75.0) | |
| WOMAC—Physical | 0.111a | ||
| Mean (SD) | 17.6 (20.6) | 26.3 (21.3) | |
| Median | 15.4 | 22.8 | |
| Range | (−42.6 to 50.0) | (0.0 to 72.1) | |
| WOMAC—Total | 0.091a | ||
| Mean (SD) | 18.6 (19.9) | 27.2 (19.2) | |
| Median | 18.8 | 24.0 | |
| Range | (−37.5 to 52.1) | (−1.0 to 71.9) | |
| SF-12 physical | 0.825a | ||
| Mean (SD) | 10.7 (11.6) | 11.3 (11.6) | |
| Median | 10.7 | 9.8 | |
| Range | (−15.3 to 39.0) | (−18.2 to 39.7) | |
| SF-12 mental | 0.927a | ||
| Mean (SD) | −0.1 (11.1) | −0.3 (13.2) | |
| Median | 0.6 | −3.2 | |
| Range | (−29.4 to 21.7) | (−36.3 to 28.1) |
aUnequal Variance t test.
PAO, periacetabular osteotomy; HA, hip arthroscopy; HOOS, Hip Disability and Osteoarthritis Outcome Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; ADL, Activity of Daily Living; QOL, quality of life.
Table VI.
PROs based on gender
| Pre-op to post-op change | Female (N = 62) | Male (N = 9) | P-Value |
|---|---|---|---|
| UCLA Score | 0.101a | ||
| Mean (SD) | 1.2 (2.6) | −0.4 (2.2) | |
| Median | 1.0 | 0.0 | |
| Range | (−4.0 to 6.0) | (−4.0 to 2.0) | |
| Harris hip score | 0.575b | ||
| Mean (SD) | 24.3 (17.2) | 20.9 (12.1) | |
| Median | 23.1 | 15.4 | |
| Range | (−6.6 to 64.9) | (4.4 to 44.0) | |
| HOOS—Pain | 0.050b | ||
| Mean (SD) | 30.5 (20.9) | 15.8 (16.1) | |
| Median | 31.3 | 10.0 | |
| Range | (−20.0 to 72.5) | (−2.5 to 42.5) | |
| HOOS—Symptom | 0.017b | ||
| Mean (SD) | 26.4 (20.4) | 6.3 (21.7) | |
| Median | 25.0 | 7.5 | |
| Range | (−25.0 to 70.0) | (−20.0 to 35.0) | |
| HOOS—ADL | 0.110a | ||
| Mean (SD) | 22.9 (19.5) | 8.3 (22.7) | |
| Median | 20.6 | 13.2 | |
| Range | (−23.5 to 72.1) | (−42.6 to 44.1) | |
| HOOS—Sports/Rec | 0.037b | ||
| Mean (SD) | 35.8 (28.5) | 13.2 (34.3) | |
| Median | 37.5 | 18.8 | |
| Range | (−31.3 to 93.8) | (−43.8 to 75.0) | |
| HOOS—QOL | 0.106b | ||
| Mean (SD) | 40.3 (25.1) | 25.7 (23.3) | |
| Median | 43.8 | 25.0 | |
| Range | (−12.5 to 93.8) | (−12.5 to 56.3) | |
| WOMAC—Pain | 0.044b | ||
| Mean (SD) | 29.2 (21.4) | 13.9 (14.3) | |
| Median | 30.0 | 10.0 | |
| Range | (−20.0 to 75.0) | (−15.0 to 30.0) | |
| WOMAC—Stiffness | 0.029a | ||
| Mean (SD) | 29.1 (25.0) | 8.3 (26.5) | |
| Median | 25.0 | 12.5 | |
| Range | (−25.0 to 75.0) | (−50.0 to 37.5) | |
| WOMAC—Physical | 0.105a | ||
| Mean (SD) | 24.1 (20.3) | 8.3 (22.7) | |
| Median | 23.5 | 13.2 | |
| Range | (−23.5 to 72.1) | (−42.6 to 44.1) | |
| WOMAC—Total | 0.044a | ||
| Mean (SD) | 25.0 (19.1) | 9.4 (20.3) | |
| Median | 25.0 | 12.5 | |
| Range | (−22.9 to 71.9) | (−37.5 to 39.6) | |
| SF-12 Physical | 0.002b | ||
| Mean (SD) | 12.5 (11.1) | 0.2 (8.3) | |
| Median | 11.3 | 4.9 | |
| Range | (−18.2 to 39.7) | (−15.3 to 7.8) | |
| SF-12 Mental | 0.344b | ||
| Mean (SD) | −0.7 (12.1) | 3.4 (11.2) | |
| Median | −2.6 | 6.4 | |
| Range | (−36.3 to 28.1) | (−18.8 to 14.3) |
HOOS, Hip Disability and Osteoarthritis Outcome Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; ADL, Activity of Daily Living ; QOL, quality of life.
aWilcoxon.
bEqual variance t test.
Table VII.
PROs based on performance of intra-articular intervention
| Majora and/or Minorb |
MajoraOnly |
|||||
|---|---|---|---|---|---|---|
| Pre-op to post-op change | Intervention (N = 53) | No intervention (N = 18) | P-Value | Intervention (N = 31) | No intervention (N = 40) | P-Value |
| UCLA score | 0.912c | 0.444c | ||||
| Mean (SD) | 0.9 (2.6) | 1.0 (2.5) | 0.7 (2.8) | 1.2 (2.3) | ||
| Median | 1.0 | 0.0 | 1.0 | 1.0 | ||
| Range | (−4.0 to 6.0) | (−4.0 to 6.0) | (−4.0 to 6.0) | (−4.0 to 6.0) | ||
| Harris hip score | 0.844c | 0.488c | ||||
| Mean (SD) | 24.1 (15.7) | 23.0 (19.4) | 25.4 (15.7) | 22.6 (17.3) | ||
| Median | 22.0 | 22.0 | 23.1 | 22.0 | ||
| Range | (−6.6 to 64.9) | (0.0 to 64.9) | (−6.6 to 64.9) | (−1.1 to 64.9) | ||
| HOOS—Pain | 0.995c | 0.408c | ||||
| Mean (SD) | 28.4 (20.7) | 28.4 (22.0) | 25.8 (21.0) | 30.3 (20.8) | ||
| Median | 30.0 | 30.0 | 25.0 | 32.5 | ||
| Range | (−20.0 to 72.5) | (−10.0 to 67.5) | (−17.5 to 65.0) | (−20.0 to 72.5) | ||
| HOOS—Symptom | 0.440c | 0.599c | ||||
| Mean (SD) | 21.2 (21.3) | 28.3 (24.5) | 20.8 (23.1) | 24.3 (21.1) | ||
| Median | 20.0 | 30.0 | 20.0 | 25.0 | ||
| Range | (−25.0 to 50.0) | (−10.0 to 70.0) | (−20.0 to 50.0) | (−25.0 to 70.0) | ||
| HOOS—ADL | 0.841c | 0.619c | ||||
| Mean (SD) | 20.4 (20.5) | 21.6 (20.9) | 19.1 (22.2) | 21.9 (19.4) | ||
| Median | 20.6 | 11.8 | 16.2 | 20.6 | ||
| Range | (−42.6 to 52.9) | (0.0 to 72.1) | (−42.6 to 152.9) | (−17.6 to 72.1) | ||
| HOOS—Sport/Rec | 0.614c | 0.296c | ||||
| Mean (SD) | 31.3 (31.3) | 35.4 (28.2) | 37.0 (29.7) | 28.9 (30.6) | ||
| Median | 31.3 | 37.5 | 37.5 | 31.3 | ||
| Range | (−31.3 to 93.8) | (−43.8 to 75.0) | (−25.0 to 93.8) | (−43.8 to 75.0) | ||
| HOOS—QOL | 0.336c | 0.425c | ||||
| Mean (SD) | 36.7 (26.8) | 42.7 (20.4) | 35.3 (29.3) | 40.5 (21.9) | ||
| Median | 37.5 | 43.8 | 40.6 | 37.5 | ||
| Range | (−12.5 to 93.8) | (6.3 to 75.0) | (−12.5 to 93.8) | (6.3 to 93.8) | ||
| WOMAC—Pain | 0.972c | 0.227c | ||||
| Mean (SD) | 27.0 (21.9) | 27.2 (19.6) | 23.1 (23.3) | 29.9 (19.4) | ||
| Median | 30.0 | 30.0 | 15.0 | 30.0 | ||
| Range | (−20.0 to 75.0) | (0.0 to 70.0) | (−20.0 to 65.0) | (−15.0 to 75.0) | ||
| WOMAC—Stiffness | 0.216c | 0.309c | ||||
| Mean (SD) | 24.0 (26.5) | 32.6 (24.3) | 22.4 (30.3) | 29.3 (22.2) | ||
| Median | 25.0 | 25.0 | 25.0 | 25.0 | ||
| Range | (−50.0 to 75.0) | (−25.0 to 75.0) | (−50.0 to 75.0) | (−25.0 to 75.0) | ||
| WOMAC—Physical | 0.965c | 0.508c | ||||
| Mean (SD) | 21.9 (21.6) | 21.6 (20.9) | 19.6 (22.4) | 23.3 (20.6) | ||
| Median | 20.6 | 11.8 | 16.2 | 23.5 | ||
| Range | (−42.6 to 63.2) | (0.0 to 72.1) | (−42.6 to 52.9) | (−17.6 to 72.1) | ||
| WOMAC—Total | 0.686c | 0.392c | ||||
| Mean (SD) | 22.0 (19.8) | 24.5 (20.8) | 20.1 (21.4) | 24.6 (18.8) | ||
| Median | 20.8 | 20.8 | 18.8 | 24.0 | ||
| Range | (−37.5 to 56.3) | (−1.0 to 71.9) | (−37.5 to 56.3) | (−17.7 to 71.9) | ||
| SF-12 Physical | 0.924c | 0.208c | ||||
| Mean (SD) | 11.0 (11.2) | 10.7 (12.6) | 12.9 (11.8) | 9.4 (11.2) | ||
| Median | 10.7 | 9.5 | 11.8 | 9.5 | ||
| Range | (−15.3 to 39.0) | (−18.2 to 39.7) | (−15.3 to 39.0) | (−18.2 to 39.7) | ||
| SF-12 Mental | 0.529c | 0.580c | ||||
| Mean (SD) | 0.4 (11.3) | −1.9 (14.1) | −1.1 (12.8) | 0.5 (11.5) | ||
| Median | 0.6 | −4.3 | −2.2 | −0.8 | ||
| Range | (−29.4 to 21.7) | (−36.3 to 28.1) | (−29.4 to 21.7) | (−36.3 to 28.1) | ||
HOOS, Hip Disability and Osteoarthritis Outcome Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; ADL, Activity of Daily Living; QOL, quality of life.
aLabral repair, Osteochondroplasty.
bLabral debridement, Chondroplasty.
cχ2.
DISCUSSION
PAO remains the standard of care for managing symptomatic DDH in skeletally mature patients with little or no osteoarthritis. Concomitant intra-articular pathology is common in these patients; however, there is a paucity of data demonstrating whether addressing these abnormalities at the time of PAO is beneficial. Intra-articular pathology can be addressed with HA or arthrotomy at the time of PAO. This study exhibits few differences between patients managed with HA versus arthrotomy, nor was a difference shown between patients who received intra-articular intervention versus those whose joint inspection required no intervention.
This study has a number of limitations. First, all patients had the joint interrogated by either HA or arthrotomy with subsequent treatment of identified pathology. Therefore, we cannot comment on whether addressing intra-articular abnormalities would lead to better outcomes as we do not have a control group where the intra-articular abnormality was left untreated. Furthermore, patients undergoing arthrotomy in the study received fewer interventions. This is certainly related to the inability to examine the entire joint, but not necessarily associated with less pathology in the cohort. These deficiencies will hopefully be addressed by a recently initiated randomized clinical trial at our institution where 50% of patients will receive no further treatment or inspection of the joint at the time of PAO. Second, each treatment algorithm was performed solely by one surgeon. As such differences in patient selection and technique may play a role as confounding variables. For example, patients treated with HA tended to have less severe dysplasia and more severe degenerative changes at baseline. However, these parameters were accounted for in the multivariable regression which showed no statistically significant differences in the PRO changes between surgical technique groups and as such, we believe this limitation is at least partially mitigated. Third, the short-term follow-up precludes analysis of how treating intra-articular disease may or may not alter the natural history of the dysplastic hip following PAO. The primary intent of this investigation was to determine patient function at a 1-year time point when post-operative healing is expected to be near completion. Nevertheless, longitudinal follow-up of the cohort is mandatory and further research regarding mid- to long-term outcomes is necessary.
Our study did not find a difference in 1 year PRO improvement following PAO between patients who had intra-articular assessment via HA or arthrotomy. Likewise, no difference was identified between patients who received intervention versus inspection alone. Siebenrock et al. showed in a previous report that patients with labral tears had worse performance after PAO [11]. In another study from Pitto et al., 37 patients that had labral tears at the time of PAO were treated as follows: 12 cases had labral repair, 21 had damaged labrum excised and 4 had labral debridement. There was no difference in observed outcomes between these groups and the surgeons concluded that treatment of the labrum may not be necessary as PAO unloads the chondrolabral junction, providing an improved environment for the labrum to heal [12]. The present study did not show a difference between those that had labral tears that were treated and those that did not have identified tears at the time of arthrotomy or arthroscopy.
A significant future area for PAO research is the establishment of procedure-specific minimum clinically important differences (MCIDs) for this procedure. While these have been relatively well-established for commonly used PRO measures in HA, especially in the case of HOOS Sports/Rec and mHHS, with conservative estimates of 25.0 and 9.0 points, respectively [13], such cutoffs are not readily available in the PAO literature. On the basis of the established values in the arthroscopy literature, both the PAO with HA and PAO with arthrotomy groups well-surpassed the MCIDs for mHHS and HOOS Sports/Rec between pre- and post-operative assessments. It is noteworthy that the differences in mHHS and HOOS Sports/Rec observed between the two intervention cohorts were neither statistically significant, nor did the point estimates for the differences between the groups meet MCID. Further comparisons between the two groups employing a prospective, randomized controlled study design are needed to investigate potential differences while minimizing the confounders present in retrospective analyses.
The results presented in this study are very similar to a recent report from Goronzy et al. who followed three groups of patients for a mean of 63 months: PAO alone for isolated DDH; PAO and osteochondroplasty via arthrotomy for DDH and cam lesions; PAO and osteochondroplasty and labral repair via HA for DDH with cam lesions and labral tears. They demonstrated no differences in post-operative PROs between all three groups [14]. This study shares an important limitation with the current work; in both, it remains unclear if the patients with intra-articular pathology would have done worse had their labral tears or cam lesions been ignored. Indeed, delineating sources of pain generation in DDH is a clinical challenge as concomitant intra-articular pathology is extremely common in these patients. Hartig-Andreasen et al. in a recent prospective study of 95 hips showed that labral disease was identified in 94% of patients on pre-operative MRA before PAO [7]. However, MRA should be interpreted with caution. In a recent conference abstract, our group showed poor concordance between pre-operative MRA and intraoperative HA with 55% agreement for labral pathology and 30% agreement for acetabular cartilage pathology [15]. MRA is an important tool, but is not reliable in determining what type of labral pathology would require fixation or repair, unless the MRI clearly shows a chondrolabral disruption. Intra-substance degeneration of the labrum, e.g. may be interpreted on MRI as a tear, but not require treatment at the time of HA. In addition, normal variants, such as a sulcus between the chondral and labral junction may be interpreted as a tear. Identifying what chondrolabral pathology requires treatment would help identify patients that should undergo HA or arthrotomy at the time of PAO. A prospective, randomized study that takes into account pre-operative MRI findings is necessary.
Hartig-Andreasen et al. perform a minimally invasive transsartorial approach for PAO and do not inspect the joint at the time of surgery [16]. Although 94% of patients had pre-operative MRA-diagnosed labral disease, only 27% returned within 2 years for subsequent HA to address persistent symptoms that were attributed in part to labral disease. At 2-year follow-up, patients that underwent subsequent HA had inferior outcomes to patients undergoing PAO alone, which would support identifying patients with labral disease or characteristics that lead to failure of the PAO alone [7]. The authors reported that those with pre-operative borderline dysplasia, acetabular retroversion and complete labral detachment had a higher likelihood of requiring subsequent surgery. Our historical experience would indicate that <10% of patients return for intra-articular intervention, however, we routinely perform either HA or arthrotomy in almost every patient. It remains unclear whether existent intra-articular damage that is not treated may progress after appropriate reorientation of the acetabulum or if an incompetent labrum poses an elevated risk for subsequent cartilage degeneration. Mechlenburg et al. demonstrated unchanged cartilage status more than 2 years after PAO regardless of whether there was concomitant labral damage [17]. Matheney et al. also showed that a labral tear at the time of PAO did not increase the risk for THA at long-term follow-up [18]. Further follow-up is needed to determine the differences in radiographic progression and natural history between groups and how this compares to the untreated dysplastic hip [19].
We showed that age and BMI did not have an impact on early PROs. This is not surprising as 66% were <30 years, 96% were <40 years and 86% were <30 BMI. Furthermore, relative advanced age and elevated BMI have been associated with inferior outcomes after PAO at later follow-up time points [2, 20]. Although numbers were limited (n = 4), we did not observe an association between concomitant acetabular retroversion and PRO outcomes. Presence of dysplasia with retroversion needs to be taken into account at the time of correction in order to prevent iatrogenic impingement [5]. Albers et al. have reported residual impingement in any plane after PAO adversely affects outcomes at 10 years [21]. In the present study, 14 hips underwent osteochondroplasty; however, their post-operative PROs were no different than those that did not. We did find that women had superior PRO outcomes to men with almost all metrics; 7 of the 13 were significantly improved. The vast majority of patients (87%) were women, which is representative of most DDH practices. Previous studies have shown that men have more severe forms of dysplasia and abnormal head neck junctions, potentially creating an environment for a more difficult correction [18]. This finding could also be related to the discrepant sample size; however, there was no difference in intra-articular intervention between men and women.
In conclusion, this study further confirms the ability of PAO to drastically improve symptoms and hip function in patients with DDH. Treating patients with HA as opposed to arthrotomy for intra-articular pathology did not demonstrate added benefit in this cohort of patients. Women showed greater clinical improvement than men regardless of which treatment algorithm was applied. This work highlights the need for high quality randomized clinical trials and larger cohort studies to provide definitive guidance on whether hip preservation surgeons should address intra-articular pathology at the time of PAO for DDH and which technique is best suited for this purpose.
ACKNOWLEDGEMENTS
We thank John C. Clohisy, MD and James Egan for management of the prospective ANCHOR registry and Prof. Reinhold Ganz, MD for thoughtful conversations regarding the presented work.
CONFLICT OF INTEREST STATEMENT
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements etc.) that might pose a conflict of interest in connection with the submitted article. Each author certifies that his or her institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
REFERENCES
- 1. Ganz R, Klaue K, Vinh TS. et al. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 1988; 232: 26–36. [PubMed] [Google Scholar]
- 2. Lerch TD, Steppacher SD, Liechti EF. et al. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2017; 475: 1154–68. PMCID: PMC5339143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Domb BG, Lareau JM, Baydoun H. et al. Is intraarticular pathology common in patients with hip dysplasia undergoing periacetabular osteotomy? Clin Orthop Relat Res 2014; 472: 674–80. PMCID: PMC3890175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ross JR, Zaltz I, Nepple JJ. et al. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med 2011; 39(Suppl): 72S–8S. [DOI] [PubMed] [Google Scholar]
- 5. Myers SR, Eijer H, Ganz R.. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 93–9. [PubMed] [Google Scholar]
- 6. Kim KI, Cho YJ, Ramteke AA. et al. Peri-acetabular rotational osteotomy with concomitant hip arthroscopy for treatment of hip dysplasia. J Bone Joint Surg Br 2011; 93: 732–7. [DOI] [PubMed] [Google Scholar]
- 7. Hartig-Andreasen C, Troelsen A, Thillemann TM. et al. Risk factors for the need of hip arthroscopy following periacetabular osteotomy. J Hip Preserv Surg 2015; 2: 374–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand 1939; 83: 5–135. [Google Scholar]
- 9. Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. New York: Springer, 1987. [Google Scholar]
- 10. Clohisy JC, Carlisle JC, Beaule PE. et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 2008; 90: 47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Siebenrock KA, Scholl E, Lottenbach M. et al. Bernese periacetabular osteotomy. Clin Orthop Relat Res 1999; 363: 9–20.. [PubMed] [Google Scholar]
- 12. Pitto RP, Klaue K, Ganz R.. [Labrum lesions and acetabular dysplasia in adults]. Z Orthop Ihre Grenzgeb 1996; 134: 452–6. [DOI] [PubMed] [Google Scholar]
- 13. Chahal J, Van Thiel GS, Mather RC III. et al. The patient acceptable symptomatic state for the modified Harris hip score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Am J Sports Med 2015; 43: 1844–9. [DOI] [PubMed] [Google Scholar]
- 14. Goronzy J, Franken L, Hartmann A. et al. What are the results of surgical treatment of hip dysplasia with concomitant cam deformity? Clin Orthop Relat Res 2017; 475: 1128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sutak AKMB, Howe BM, Sierra RJ.. MRI Arthrogram (MRA) was Unreliable in Predicting Intraoperative Findings at the Time of PAO in the Dysplatic Hip. 19–22 April 2017. Amelia Island, FL: Mid-America Orthopaedic Association, 2017. [Google Scholar]
- 16. Hartig-Andreasen C, Troelsen A, Thillemann TM. et al. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res 2012; 470: 2978–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mechlenburg I, Nyengaard JR, Gelineck J. et al. Cartilage thickness in the hip measured by MRI and stereology before and after periacetabular osteotomy. Clin Orthop Relat Res 2010; 468: 1884–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Matheney T, Kim YJ, Zurakowski D. et al. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am 2009; 91: 2113–23. [DOI] [PubMed] [Google Scholar]
- 19. Wyles CC, Heidenreich MJ, Jeng J. et al. The John Charnley award: redefining the natural history of osteoarthritis in patients with hip dysplasia and impingement. Clin Orthop Relat Res 2017; 475: 336–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Novais EN, Potter GD, Sierra RJ. et al. Surgical treatment of adolescent acetabular dysplasia with a periacetabular osteotomy: does obesity increase the risk of complications? J Pediatr Orthop 2015; 35: 561–4. [DOI] [PubMed] [Google Scholar]
- 21. Albers CE, Steppacher SD, Ganz R. et al. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res 2013; 471: 1602–14. [DOI] [PMC free article] [PubMed] [Google Scholar]