ABSTRACT
Robinson, in 1947 introduced for the first time the term ‘piriformis syndrome’. More recently, many etiologies of sciatic nerve entrapment around the gluteal region or the non-discogenic area have been identified, resulting in the use of a new term ‘The Deep Gluteal Syndrome’. The purpose of this study was to assess the outcomes following the endoscopic release of sciatic nerve entrapment. Type of study is a consecutive case series. Fifteen patients were diagnosed with sciatic nerve entrapment from January 2012 to December 2015, all of them were treated with endoscopic release of the piriformis tendon and sciatic nerve exploration on lateral decubitus position. Every patient had a minimum follow-up to 2 years. The patient-reported outcome scores used included the modified Harris Hip Score (mHHS), pain was estimated on a visual analog scale (VAS) and the Benson outcomes questionnaire. The patient’s mean age was 40.2 years (range, 28–50 years). The score improvement from pre-operative to 24-month follow-up was 46.8–84.9 for mHHS (P <0.05). The VAS decreased from pre-operative to 24-month follow-up was 7.4–1.86 (P < 0.05). The Benson outcome ratings were excellent for 11 patients, good for 3 and fair for 1. The Endoscopic Release of the Piriformis Tendon and Sciatic Nerve Exploration showed an improvement of functions, diminishing pain and allowing patients to return to daily activities without symptoms (Level of Evidence: IV).
INTRODUCTION
In 1947, Robinson [1] introduced the term ‘piriformis syndrome’ (PS) and proposed six main characteristics: (i) history of trauma in the sacroiliac and gluteal region; (ii) pain in the sacroiliac joint, greater sciatic notch and piriformis muscle, which extends down the leg and causes difficulty walking; (iii) exacerbations improve with rest or by raising the limb and to make traction in the affected leg; (iv) palpation of a soft mass like a sausage on the piriformis; (v) Lassegué sign and (vi) gluteal atrophy. The first mention of the piriformis muscle as a cause of sciatica is attributed to Yeoman in 1928 [2]. PS has been an elusive diagnosis often an exclusion one that can be done only when the symptoms suggests no spinal cause of significant sciatic pain [3]. On physical examination, pain and weakness with resisted abduction and external rotation of the hip often referred to ‘The Pace sign’ [4]. The ‘Freiberg’ sign is pain with internal rotation of the extended hip [5, 6]. Another active test, proposed by Beatty [7] involves having the patient lie on the affected side with the knee and hip flexed. Abducting the thigh to raise the knee off the table elicited deep buttock pain in those with PS, but back and leg pain in those with lumbar disk disease. The ‘FAIR’ maneuver is positive when the hip is passively flexed, adducted and internally rotated by the examiner, reproducing buttock pain radiating down the leg. The FAIR maneuver had a sensitivity of 85% in identifying PS and 82% in identifying normal legs when using a cutoff of 2 SDs above the normal H-reflex (1.36 ms) [8]. The ‘seated piriformis stretch’ test is a flexion and adduction with internal rotation test performed with the patient in the seated position [9]. The examiner extends the knee (engaging the sciatic nerve) and passively moves the flexed hip into adduction with internal rotation while palpating 1 cm lateral to the ischium (with the middle finger) and proximally at the sciatic notch (with the index finger). In the previous article published by Martin et al. the authors found that the active piriformis test and seated piriformis stretch tests can be used to help identify patients with and without sciatic nerve entrapment in the deep gluteal region [10].
A positive test is the recreation of the posterior pain at the level of the piriformis or external rotators. An active piriformis test is performed by having the patient push the heel down into the table and abduct and externally rotate the leg against resistance while the examiner monitors the piriformis.
Although numerous previous studies have considered the treatment of the sciatic nerve entrapment, the performance of the endoscopic release of the piriformis tendon and sciatic nerve exploration is currently evolving. The purpose of this study was to assess the outcomes following the endoscopic release of sciatic nerve entrapment in our population after 2-year follow-up.
MATERIALS AND METHODS
From January 2012 to December 2015, data were prospectively collected on all endoscopic release of the piriformis tendon and exploration of the sciatic nerve. Demographic factors, including gender, age, height, weight and body mass index (BMI) were recorded. All patients received 2 months of physical therapy and if they did not improve surgical treatment was indicated. Surgical cases were included if they were diagnosed with an entrapment of the sciatic nerve. Physical examination included the straight leg raise test and the seated piriformis stretch test. The straight leg raise test as described previously, was performed with the patient supine. With the knee remaining in full extension, the hip joint was taken to an endpoint of hip flexion or until the patient starts to complaint (i.e. pain and/or paraesthesias). The seated piriformis stretch test is performed with the patient seated over the edge of the examination table with the hip flexed to approximately 90° and the knee extended. While palpating the sciatic notch, the examiner adducts and internally rotates the limb, this will length the deep rotators and create dural tension of the sciatic nerve.
Magnetic resonance imaging of the sciatic nerve was performed in all cases to identify the relationship of the sciatic nerve and the piriformis tendon. Only cases where the sciatic emerged under the piriformis as a single trunk were included in this study. An ultrasound-guided diagnostic injection at the area where the sciatic nerve emerged under the piriformis was performed in all cases (relief of the buttock pain after injection was considered a positive test). All patients included had a minimum of 2-year follow-up. Exclusion criteria were patients with isolated femoroacetabular impingement or intra-articular pathology, lumbar spine or sacroiliac joint as the source of the posterior hip pain, patients who do not agree to sign the informed consent form or be a part of the research. The Institutional Review Board approved this study.
Lateral release of the piriformis tendon (at its insertion on the greater trochanter) was indicated in the case of a single sciatic nerve trunk emerging deep to the muscle belly of the piriformis.
When the sciatic nerve pierces through the muscle belly of the piriformis it must be released at the site of compression; the same is true for a bifurcated nerve that passes around or pierces the muscle belly of the piriformis.
Surgical technique
All hip endoscopic releases were performed by the senior author with patients in the lateral decubitus without traction, similar to the positioning for total hip replacement in lateral decubitus as described previously [11]. In this technique, a 30° scope and slotted or plastic disposable cannulas are used through two portals: a proximal trochanteric and distal trochanteric [11].
With the patient in lateral decubitus the leg that lies on top is prepared and drape in a similar fashion to total hip replacement. First, we start positioning a spinal needle on the lateral aspect of the greater trochanter, an image intensifier is used to assist in placing this needle. The distal trochanteric portal is established approximately 4–5 cm distal to the position of the spinal needle. Using a standard arthroscopic cannula that is introduced under the skin at the subcutaneous space lateral to the iliotibial band and directed proximally to the site of the proximal trochanteric portal, which is 4–5 cm proximal to the spinal needle. Using the blunt obturator to create a space above the iliotibial band. The site of the proximal trochanteric portal is identified arthroscopically using a needle inserted at the portal landmark; the skin incision is made, and a shaver is introduced to dissect the subcutaneous tissue lateral from the iliotibial band in the area situated between the portals. We start with a pump pressure of 30 mmHg (Fig. 1). Then, a radiofrequency hook probe is introduced from the proximal trochanteric portal, and a 4- to 6-cm vertical retrograde cut is performed on the iliotibial band, the spinal needle marks the center of this cut. Once the vertical cut on the iliotibial band is complete, a transverse posterior cut of approximately 2 cm in length is performed at the central portion of the longitudinal cut. The resulting superior and inferior anterior flaps are resected using a shaver developing an oval defect on the anterior iliotibial band that will provide access to the posterior iliotibial band. At this point, we can increase the pump pressure up to 60 mmHg if necessary to keep a clear field of view. The greater trochanter will rotate freely internally to enter the peritrochanteric space and advance towards the deep gluteal space. Positioning the leg in internal rotation and slight flexion of the hip and knee we position the scope posterior to the Great Trochanter (GT). Under fluoroscopy and direct arthroscopic vision, the piriformis tendon at its insertion on the GT is exposed and identified. The piriformis tendon was then released from its insertion on the GT in a retrograde fashion using a radiofrequency hook probe (Fig. 2). The relation of the sciatic nerve and the piriformis tendon was assessed endoscopically (in our series all the sciatic nerves were found in a deep position in relation to the piriformis). Using the blunt probe, a shaver and radiofrequency probes, the sciatic nerve was carefully dissected from fibro-vascular bands which were resected using radiofrequency probes with a retrograde technique cutting away from the nerve and the hip range of motion was repeated to ensure adequate mobility [12–13] (Fig. 3). The bands we identified and removed were type 1B according to Carro et al. [14]. The kinematic excursion of the sciatic nerve described by Coppieters et al. [12] and is assessed with the leg in flexion and internal/external rotation and full extension with internal/external rotation.
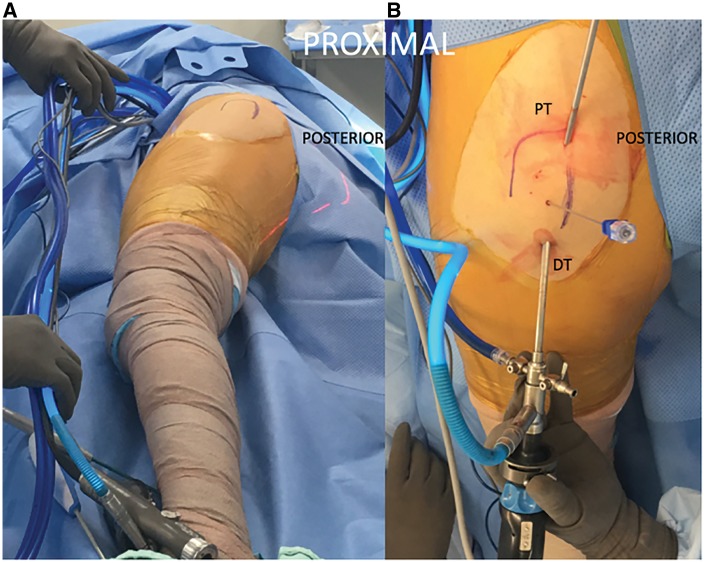
Fig. 1.
Clinical photograph showing a patient positioned in left lateral decubitus (right side operated on) (A) The greater trochanter has been outlined. The limb is freely draped without traction similar to positioning for total hip replacement. (B) A spinal needle has been introduced at the most lateral aspect of the greater trochanter (under fluoroscopic guidance). The proximal trochanteric (PT) and distal trochanteric (DT) portals have been established.
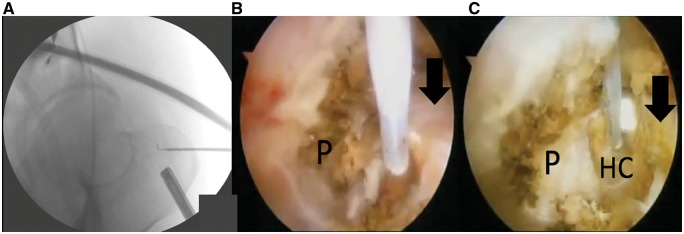
Fig. 2.
Endoscopic release of the piriformis tendon in a right hip. (A) Fluoroscope images demonstrate the position of the radiofrequency hook probe at the insertion of the piriformis tendon on the grater trochanter. Note the arthroscope at the inferior left. (B) The hook probe is the used to release the piriformis tendon in a retrograde fashion (P). (C) This figure demonstrates a complete release of the piriformis tendon.
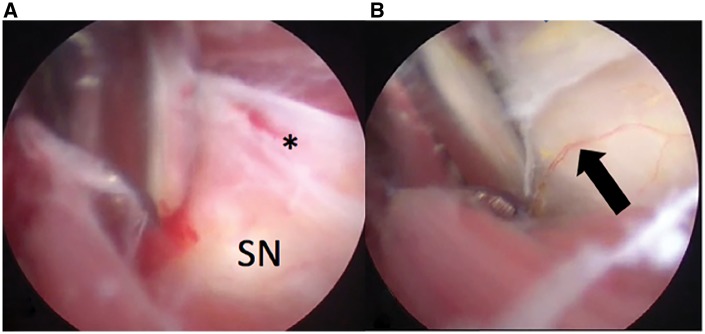
Fig. 3.
Endoscopic release of the sciatic nerve (SN) in a right hip. (A) A shaver is used to resect a fibrovascular band (*) going across the sciatic nerve (SN). (B) After release of the fibrous band the vasa nervorum reappear on the sciatic nerve (Black arrow). The nerve is more mobile after release of the fibrotic bands.
Surgical outcome measurement
All patients undergoing hip endoscopy were assessed using 2 patient-reported outcome measures: the modified Harris Hip Score (mHHS) [15, 16] and The Benson outcomes questionnaire [17]. Pain was estimated on the visual analog scale (VAS).
Statistical analyses
An a priori analysis was performed, and it was estimated a clinically significant for the evaluation between pre-operatory and follow-up for de-mHHS and VAS. We used Student t-test for related samples with normal distribution; Pearson correlation, for the association between continuous quantitative variables with normal distribution. A P values of < 0.05 was considered significant. Statistical analysis was done with Microsoft Excel 2007 (Microsoft Corp, Redmond, WA, USA) and IBM SPSS 12.0 for Windows (SPSS Inc, Chicago, IL, USA).
Rehabilitation protocol
Overall, we started the postoperative rehabilitation protocol the day after surgery protecting the walking with crutches for 2 weeks until the gait is normal and protect the wound during early healing [11]. The range of motion of the hip is limited to 90° of flexion during the first week to prevent pain and progressively increased. Similar caution was applied for internal rotation, external rotation of 30° and 30° of abduction for 3–6 weeks. Once the patient tolerates the walk with full support, therapy progresses to achieve strength and full activity for 3–4 months.
RESULTS
From January 2012 to December 2015, there were 15 patients that met the inclusion criteria. The mean length of post-surgical follow-up was 30 months (range, 24–48 months). Patients included 5 women (mean age, 41 ± 5.2 years; range, 35–48 years) and 10 men (mean age, 40 ± 6.8 years; range, 28–50 years) The mean height was 1.66.± 0.10 m (range, 1.52–1.89 m); mean weight, 78.8 ± 11.4 kg (range, 62–110 kg); and mean BMI, 28.5 ± 2.7 kg/m2 (range, 23–32.4 kg/m2). The right side was involved in eight cases and left seven cases. Demographic data are displayed in Table I. No patients were lost during the follow-up. The average time of surgery was 66 minutes. All cases had a complete history, physical and radiographic examination, magnetic resonance imaging and diagnostic injection tests.
Table I.
Patient demographics and results
| Results | Data (n = 15) |
|---|---|
| Gender | 10 male/5 female |
| Age (years) | 40.2 ± 6.2 (range, 28–50) |
| Operative side | 8 right/7 left |
| BMI | 28.5 ± 2.7 (range, 23–32.4) |
| FU (months) | 31.3 ± 8.5 (range, 18–50) |
| Surgery time (minutes) | 66 ± 3.8 (range, 60–70) |
| HHS | |
| Preoperative | 46.8 ± 13.2 (range, 21–78) |
| Postoperative (2-y FU) | 84.9 ± 4.7 (range, 78–96)* |
| Pain (VAS) | |
| Pre-operative | 7.4 ± 0.7 (range, 6–9) |
| Post-operative (2-y FU) | 1.86 ± 0.83 (range, 1–4) |
| Benson Surgical Outcomes (2-y FU) | Excellent: 11 |
| Good: 3 | |
| Fair: 1 | |
| Poor: 0 | |
| Physical examination | Positive patient tests |
| Palpation | 15 |
| Freiberg’s maneuver | 8 |
| Pace test | 7 |
| Beatty maneuver | 7 |
| FAIR | 10 |
| Seated piriformis test | 11 |
| Active piriformis test | 10 |
FU, follow-up
P < 0.05.
The mean duration of symptoms was 31 months (range, 18–50). Four patients reported the mechanism of injury to be traumatic, which involved falling. One patient had previous hip surgeries (open surgery for bursectomy 4 years previous) and the same patient had previous spine surgeries (lumbar spine instrumentation with discectomy L5–S1). The number of patients with related symptoms was 13 with sitting pain 14 with buttock pain and 5 with paresthesias or radicular pain. The mean preoperative pain level was 7.4 ± 0.7 out of a maximum pain of 10 points. The mean preoperative mHHS was 46.8 ± 13.2 (range, 28–71). No patient played sports high performance.
The postsurgical findings were 14 patients the greater trochanteric bursa was found to be excessively thickened with fibrous scar bands to extend to near the sciatic nerve. Fibrous bands were present in 15 patients. The sciatic nerve was entrapped by the piriformis tendon on the nerve in 13 patients. There were no complications during or after surgical procedure.
The score improvement from pre-operative to 24-months follow-up, was 46.8–84.9 for mHHS (P < 0.05). The VAS decreased from pre-operative to 24-month follow-up was 7.4–1.86 (P < 0.05). All the cases demonstrated statistically significant postoperative improvement in all scores (P < 0.05). The physical examination tests were negative in all patients after endoscopic sciatic nerve decompression. All patients were able to return to work and perform daily living activities without limitations. The Benson outcome ratings were excellent for 11 patients, good for 3 for and fair for 1.
DISCUSSION
The results of this study suggest that the Endoscopic Release of the Piriformis Tendon and Sciatic Nerve Exploration improves the symptoms in those patients with a long story of buttock pain with failed non-operative measurements.
The reports in the literature are varied, most are case reports and small series and generally are good but variable. The largest cohorts were published by Fishman et al. [18], Indrekvam and Sudmann [19] and Benson and Schutzer [17]. The results from these three studies, respectively, ranged from 68.8% achieving >50% relief, two thirds improved and 100% excellent or good results. The open surgical release published by Byrd [20] was performed in seven patients, five patients were deemed to have an excellent result based on their extreme satisfaction because of complete alleviation of their preoperative symptoms. Two of these had occasional posterior soft-tissue tenderness or slight radicular symptom. In the study of Martin et al. [13] reported a cohort of 35 patients with diagnosis of The Deep Gluteal Syndrome, the mean patient age was 47 years (range, 20–66 years). The mean duration of symptoms was 3.7 years (range, 1–23 years). The mean preoperative VAS score was 6.9 ± 2.0, and the mean preoperative mHHS was 54.4 ± 13.1 (range, 25.3–79.2). The Benson outcome ratings were 11 excellent, 5 good, 2 fair and 5 poor; these results are consistent with presented in this article. In our study, one patient (men) had a fair outcome in the Benson outcome rating; in this case, the patient had a concomitant pathology [obesity (BMI 31.1), open surgery bursectomy, L5–S1 disc disease, diabetes mellitus, smoking], history of traumatic injury, occasionally used narcotics to control the pain, but not radicular symptoms, this was felt to be inconsequential compared with their preoperative pain, and he returned to work and daily living activities in 6 months. The performance of this technique using the lateral decubitus position has been described previously by Knudsen et al. [21] This pathology and its diagnosis can be difficult because of the inner complexity of the surrounding soft tissues. Differential diagnosis includes other sources of entrapment such as pudendal nerve entrapment, hamstring pathology, ischiofemoral impingement or ischial tunnel syndrome or deep gluteal syndrome.
CONCLUSION
Establishing a good and organized protocol of diagnosis and treatment for the piriformis tendon is mandatory. The Endoscopic Release of the Piriformis Tendon and Sciatic Nerve Exploration showed improvement of functions, diminishing pain and allowing patients to return to daily activities. We suggest comparing this safe and reproducible technique with others described including open surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Robinson DR. Piriformis syndrome in relation to sciatic pain. Am J Surg 1947; 73: 355–8. [DOI] [PubMed] [Google Scholar]
- 2. Yeoman W. The relation of arthritis of the sacroiliac joint to sciatica, with an analysis of 100 cases. Lancet 1928; 2: 1119–22. [Google Scholar]
- 3. Guvencer M, Akyer P, Iyem C. et al. Anatomic considerations and the relationship between the piriformis muscle and the sciatic nerve. Surg Radiol Anat 2008; 30: 467–74. [DOI] [PubMed] [Google Scholar]
- 4. Pace JB, Nagle D.. Piriform syndrome. West J Med 1976; 124: 435–9. [PMC free article] [PubMed] [Google Scholar]
- 5. Freiberg AH. Sciatic pain and its relief by operations on muscle and fascia. Arch Surg 1937; 34: 337–50. [Google Scholar]
- 6. Freiberg AH, Vinke TH.. Sciatica and the sacroiliac joint. J Bone Joint Surg Am 1934; 16: 126–36. [Google Scholar]
- 7. Beatty RA. The piriformis muscle syndrome: a simple diagnostic maneuver. Neurosurgery 1994; 34: 512–4. [DOI] [PubMed] [Google Scholar]
- 8. Fishman LM, Anderson C, Rosner B.. BoTox and physical therapy in the treatment of piriformis syndrome. Am J Phys Med Rehabil 2002; 81: 936–42. [DOI] [PubMed] [Google Scholar]
- 9. Martin H. Clinical examination and imaging of the hip In Byrd J, Guanche C (eds). AANA Advanced Arthroscopy: The Hip. Philadelphia: Elsevier, 2010. [Google Scholar]
- 10. Martin HD, Kivlan BR, Palmer IJ. et al. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc 2014; 22: 882–8. [DOI] [PubMed] [Google Scholar]
- 11. Ilizaliturri VM Jr, Martínez-Escalante FA, Chaidez PA. et al. Endoscopic iliotibial band release for external snapping hip syndrome. Arthroscopy 2006; 22: 505–10. [DOI] [PubMed] [Google Scholar]
- 12. Coppieters MW, Alshami AM, Babri AS. et al. Strain and excursion of the sciatic, tibial, and plantar nerves during a modified straight leg raising test. J Orthop Res 2006; 24: 1883–9. [DOI] [PubMed] [Google Scholar]
- 13. Martin HD, Shears SA, Johnson JC. et al. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy 2011; 27: 172–81. [DOI] [PubMed] [Google Scholar]
- 14. Carro LP, Hernando MF, Cerezal L. et al. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles Ligaments Tendons J 2016; 6: 384–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Aprato A, Jayasekera N, Villar RN.. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy. Am J Sports Med 2012; 40: 2557–60. [DOI] [PubMed] [Google Scholar]
- 16. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969; 51: 737–55. [PubMed] [Google Scholar]
- 17. Benson ER, Schutzer SF.. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am 1999; 81: 941–9. [PubMed] [Google Scholar]
- 18. Fishman LM, Dombi GW, Michaelsen C. et al. Piriformis syndrome: diagnosis, treatment and outcome—a 10-year study. Arch Phys Med Rehabil 2002; 83: 295–301. [DOI] [PubMed] [Google Scholar]
- 19. Indrekvam K, Sudmann E.. Piriformis muscle syndrome in 19 patients treated by tenotomy—A 1- to 16-year follow-up study. Int Orthop 2002; 26: 101–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Byrd JWT. Piriformis syndrome. Oper Tech Sports Med 2005; 13: 71–9. [Google Scholar]
- 21. Knudsen JS, McConkey MO, Brick MJ.. Endoscopic sciatic neurolysis. Arthroscopy Techniques 2015; 4: e353–8. [DOI] [PMC free article] [PubMed] [Google Scholar]