Abstract
Kyasanur forest disease (KFD) is a known viral haemorrhagic fever in India, for the last 60 years. However, in recent years, the change in epidemiological profile of the disease has suggested that it is now time to consider KFD as an emerging tropical disease in India. The preference should be to educate not only the villagers where it is being reported or detected but also to public health experts, veterinarians, forest officials and medical professionals to pay attention while seeing a patient overlapping with endemic diseases such as Japanese encephalitis, West Nile, dengue, chikungunya, malaria and tuberculosis. Although the existence of KFD is known for a long time, updated understanding of its clinical profile in humans is still limited. This article describes in detail the clinical presentation of KFD reported till date. It also highlights geographical distribution of the disease, risk factors for virus transmission, biochemical/haematological findings and control measures. There is an urgent need for research on KFD, particularly for understanding biphasic nature of illness, development of cost-effective diagnostic tools, utility of non-invasive samples for diagnosis and development of new vaccines.
Keywords: Arbovirus, biphasic, haemorrhagic fever, Kyasanur forest disease, vaccine
Introduction
Kyasanur forest disease (KFD) or monkey fever is a unique public health problem along the belts of Western Ghats of India. The disease is caused by KFD virus (KFDV) which is an arbovirus, family Flaviviridae1. Humans are infected by the bite of tick and present with fever, sometimes haemorrhagic and/or neurological features2. Majority of patients (80%) will recover without any consequences1,3. However, about 20 per cent of patients manifest with biphasic presentation of symptoms, and of them, a few will develop severe haemorrhagic or neurological symptoms3,4,5. The disease was limited to the Western Ghats of Karnataka State of India for about seven decades, however, since the last five years cases have been reported from adjacent States of Karnataka along the course of Western Ghats. The burden of the disease is increasing with the years6,7. Detailed clinical and epidemiological aspects of KFD need to be explored for better understanding of the disease. This review provides information in detail on the clinical, epidemiological, advanced laboratory diagnosis and prevention aspects of KFD.
Clinical profile of Kyasanur forest disease (KFD)
International Classification of Diseases-10 (ICD-10), 2017 classifies KFD in category A98.2, which falls under other viral haemorrhagic fevers, not classified elsewhere8. The incubation period of KFDV in humans is 3-8 days9. The clinical presentation of KFD is usually described as biphasic10, but occasionally in four stages11. In the first phase, patients usually present with sudden onset of fever, headache and generalized body pain, especially of the neck, upper and lower back and extremities. Conjunctival inflammation of both the sclera and palpebra is often noted. In this early phase of illness, gastrointestinal symptoms including vomiting, abdominal pain and diarrhoea occur in majority of patients. Fever may subside, but patients can remain asthenic and listless for a long period. Dehydration may be aggravated due to poor intake of fluids. Other non-specific features such as lymphadenopathy and hepato-splenomegaly are also reported1,2,4,12,13,14,15. Convalescence period is prolonged.
Haemorrhagic manifestations are part of initial phase and may begin 3-4 days after onset of symptoms1,3. These may begin with oral mucosal inflammation and non-tender maculo-papular eruptions over both soft and hard palate. No specific skin lesion or rashes are observed. Ocular manifestation includes conjunctival congestion in almost all cases and serous discharge in 63 per cent of cases and retina and vitreous humour are involved in 13 per cent of cases16. Other features include haematemesis reported in eight per cent of cases, epistaxis in two per cent and bleeding per rectum reported in two per cent of cases17. Persistence of haemorrhagic manifestations can lead to poor outcome. In general, most patients recover in 10-14 days. During the recovery phase, patients may present with muscle twitching, coarse tremors, paraesthesia and generalized shaking due to weakness1,2,3,4,12,13,14,15.
Up to 20 per cent of patients may present with biphasic illness9. In this phase, fever with predominant neurological symptoms is a major presentation and can last for 12-14 days3,4,5. A few patients may have only febrile exacerbation without any neurological symptoms4. Neurological features include drowsiness, transient disorientation, confusion, rarely convulsion and loss of consciousness. Clinical signs include positive Kernig sign and abnormal ankle reflex. However, no studies have provided clear evidence of meningitis or encephalitis4,18,19. Many patients recover to normal mental alertness and orientation, with subsidence of fever, unless persistent haemorrhagic complications occur, which can lead to a poor outcome. The case fatality rate of KFDV infection is about 2-10 per cent13. Higher fatality is noted in naive non-endemic areas, mainly due to lack of awareness and also lower herd immunity to the virus13,20. Long-term complications are rare.
Post-mortem findings of Kyasanur forest disease (KFD) patients
Gross and microscopic autopsy findings of KFD cases have shown non-specific disease process. Post-mortem findings revealed predominance and flooding of macrophages and lymphocytes in the liver, spleen and kidney with features of parenchymal disease3,10. Focal necrosis of liver and tubular damage in kidney were the persistent findings3,21. Some cases have shown haemorrhagic pneumonia. Among fatal cases with neurological features, aseptic meningitis-like picture was noted with no specific lesions of meningitis, encephalitis or meningoencephalitis. Abnormalities related to cerebrospinal fluid (CSF) were also not observed4. Very few cases presented with cerebral oedema and inflammatory cells in the brain tissue11.
Biochemical and haematological findings
A study for biochemical and haematological findings on 26 KFD patients revealed that blood counts were on the lower side (leucopenia, eosinopenia with lymphopenia) during the first week of illness5. Features of marked leucopenia were common amongst all the cases. Lymphocytosis was observed in the fourth week of illness typical of viral infection. Eosinophilia (3/26 cases), atypical lymphocytes with irregular nuclei (9/26 cases) and atypical monocytes including vacuolated cytoplasm (3/26 cases) were found in the peripheral blood with features of thrombocytopenia5. Urine may show presence of granular casts, red blood cells and proteinuria. Deranged liver functions with reduced serum albumin and increased levels of alkaline phosphatase, bilirubin and gamma globulin were noted. The renal function tests including serum urea and creatinine were found to be normal5,21.
Laboratory diagnosis
Earlier laboratory tests for diagnosis of KFD included conventional tests such as virus isolation by in vivo inoculation of serum from patients into suckling mice, serological tests such as haemagglutination inhibition, complement fixation and neutralization test. All these tests were labour intensive and time-consuming. KFDV is ranked as one of the high-risk categories of pathogens belonging to Biosafety Level-4. However, numerous infections in field and laboratory personnel, in the early years following identification of this virus, resulted in suspension of work22, until an appropriate Biosafety Level-3 laboratory was fully functional in 200623. This was followed by the development of sensitive diagnostic approaches for identification of KFDV, including nested polymerase chain reaction (PCR) and real-time PCR23. IgM and IgG ELISA were also developed and validated23. These tests have contributed immensely to the early identification of KFD12,23,24,25. In spite of being reliable assays for disease identification, the limitation of these assays are the requirement of the expensive reagents and elaborate setup and trained workforce, which is challenging for a country like India. Under the Department of Health Research, network of Viral Research Diagnostic Laboratory (VRDL) has been set up for viral disease diagnosis, which is equipped with skilled workforce and infrastructure26. However, the prevalence of this disease in remote forested areas poses a great challenge in establishing molecular and serological diagnosis laboratory. Considering the emergence of KFD in locations across the Western Ghats, which are usually remote and inaccessible, a simple, user-friendly, rapid, point-of-care test which can be readily deployed in field conditions is the need of the hour. However, cross-reactivity among flaviviruses should be kept in mind while developing or using such assays. The preferred samples for KFD diagnosis are blood/serum and occasionally CSF. Although previous studies have reported absence of viruria22, it could be due to lack of sensitive molecular diagnostic tools. Recently, urine samples of KFD cases collected during acute phase of 1-4 days revealed the presence of low KFDV RNA positivity (unpublished data, NIV, Pune).
Treatment
There is no specific anti-viral drug therapy for KFD. Supportive treatment with maintenance of proper hydration and circulation by transfusion of intravenous fluids, colloids or blood products depending upon patient's clinical signs and symptoms is the mainstay of treatment27.
Epidemiology
During 1957-2012, KFDV activity was limited to Shimoga, Chikmagalur, Uttara Kannada, Dakshina Kannada and Udupi districts of Karnataka State. In 2012, KFD cases were reported in Nilgiris of Tamil Nadu. During 2013-2015, confirmed cases were reported from Wayanad, Malappuram, Palakkad and Nilambur districts of Kerala State. Some cases were reported from Sattari taluk of Goa during 20155,13,15,22,25. During 2016, KFD cases were reported from Dodamarg and Sindhudurg districts of Maharashtra and Dharbandora taluk of Goa6,7. The number of cases increased in 2017 from Dodamarg, Sawantwadi, Sindhudurg districts of Maharashtra and Valpoi, Pernem, Dharbandora taluk of Goa state6,7,28. Cases from Karnataka were reported regularly during these years. Since the last seven decades, the virus activity was known only in Karnataka and for the past five years the cases have been reported from adjacent States of Karnataka such as Tamil Nadu, Kerala, Goa and Maharashtra. This is a cause of concern considering the similar ecology of the affected areas, which are all situated in the Western Ghats6,10,12,13,15,21,28,29,30,31,32. It is not clear whether these areas are endemic24 or disease has spread due to movement of monkeys and small rodents (those harbour ticks), which act as reservoir for the virus25. Rodents develop very low-level of asymptomatic viral load in their system, which is sufficient to transmit infection to vector tick during blood meals22,33. Earlier sero-surveillance studies have reported positivity in Gujarat, West Bengal and Andaman Nicobar Islands34,35 Table and Figure.
Table.
Details of Kyasanur forest disease (KFD) virus infection in India
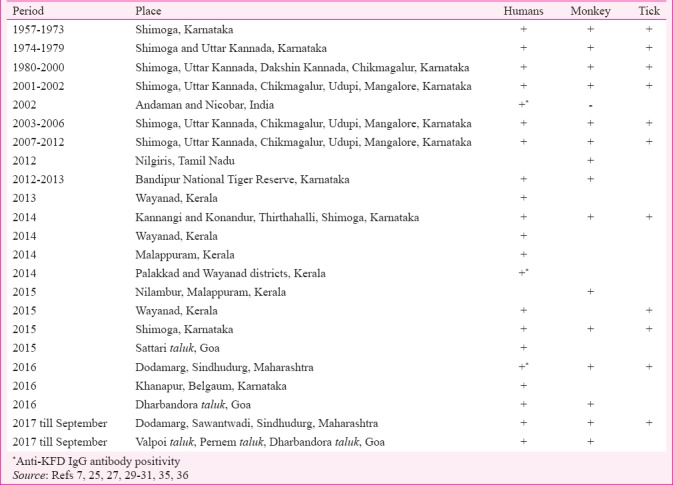
Figure.
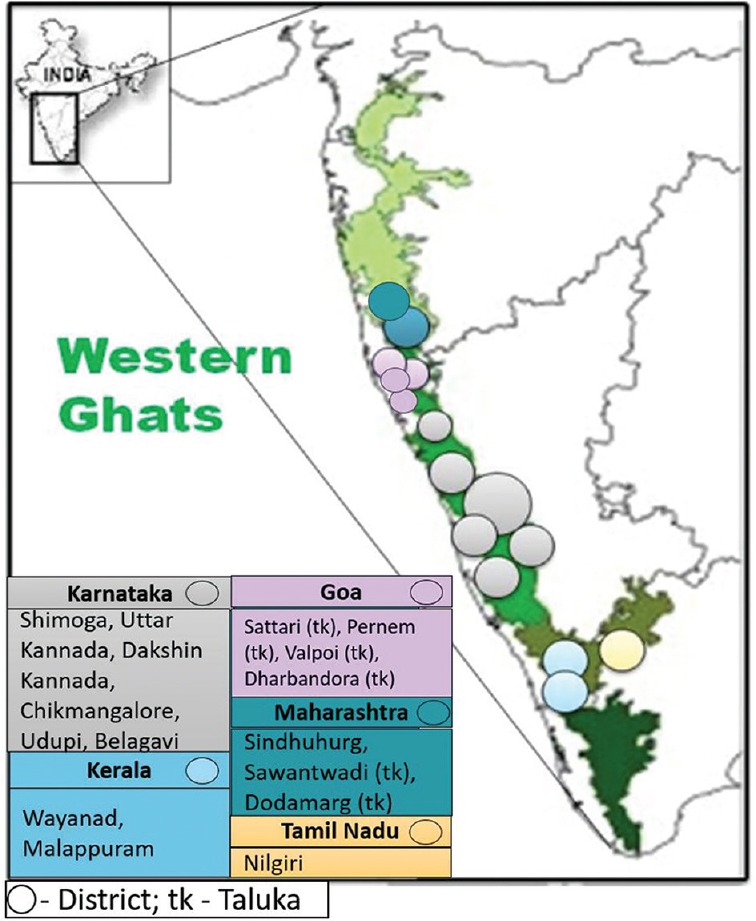
Map showing distribution of Kyasanur forest disease affected districts along the course of Western Ghats of India. Different colour represents different KFD affected States in India. Circles represent KFD affected districts in that State. Each circle denotes one affected district.
Ecological factors
The Western Ghats provide ideal topographical and climatological conditions for the vector ticks, thus making these Ghats as epitome for this tick-borne disease. The Western Ghats cover 1600 km area starting from south of Tapti river (near the border of Gujarat and Maharashtra) and pass through States of Maharashtra, Goa, Kerala, Karnataka and Tamil Nadu. These Western Ghats are full of wildlife sanctuaries, dense evergreen forest reserves. There is a high risk of spread of KFD amongst the people working/living in and around forest areas of these regions. Movement of monkeys and rodents also contribute, since they harbour vector ticks, which maintain the KFD virus in nature by trans-ovarial and trans-stadial transmission10,13. Human gets exposed to ticks while visiting the forest for farming or grazing livestock animals, collecting dried leaves or dry woods, hunting or trekking, cashew cut forming and disposal of KFD-infected dead monkeys. Earlier data accumulated from the five districts of Karnataka showed the KFD transmission from December to May, when nymphal activities are at peak, thus maintaining wildlife-livestock-human interfaces13,37. However, epidemiological data generated later from the other States suggest that the KFD cases can be detected as early as from October and cease of transmission is noticed by June13,38. Deforestation and encroachment of human dwellings towards forest areas are also responsible for increase in transmission and spread of KFDV in newer regions10,13. An ecological niche model of risk of transmission of KFDV reported that whole Western Ghats belt had high-to-moderate risk for KFD spread with time36. Probably, lack of awareness or knowledge on disease may be the possible reason for not reporting KFD in other regions of the Western Ghats.
Control and prevention
Treating forest floor with gamma-hexachlorocyclohexane can control tick population. Tick repellents such as N, N-diethyl-meta-toluamide (DEET) and dimethyl phthalate (DMP) oil can be used to avoid tick bites37. Injection of ivermectin to the cattle post-monsoon in September/October may reduce the tick burden on cattle stocks39.
Since 1990, in all KFD endemic areas of Karnataka, the State government has initiated vaccination campaign using formalin-inactivated tissue-culture vaccine. Vaccination is usually carried out within a range of 5 km of the affected area. The schedule for vaccine is two doses at baseline and one month to all persons aged 7-65 yr and with a booster dose at 6-9 months40. Vaccine efficacy was low with 62.4 per cent for first two doses and 82.9 per cent with booster dose after receiving the first two doses41. Hence, there is a need for booster doses annually for five years40. There is an urgent need to understand the validity of current vaccination schedule and look for reasons for poor vaccine effectiveness.
Scope for further research
There are several unanswered questions; such as, is there a role for host factors affecting the evolution of disease? Why do only specific patients develop haemorrhagic symptoms and biphasic illness? What is the clinical and sub-clinical ratio? This information can provide support to health system in taking precautionary measures as well as decision of introducing vaccination and time for first dose of vaccine in a high-risk area. It is also time to understand the influence if any of comorbid conditions such as diabetes, hypertension, alcoholism on the pathogenesis and evolution of disease. Detailed surveillance is needed in the Western Ghats, especially in the areas where KFD is not yet reported. A holistic approach involving medical, veterinary and entomology/vector biology experts is required to understand the current scenario. Focus on Information Education and Communication (IEC) activities in communities will help in timely reporting of monkey deaths for pro-active control measures.
Another priority is to develop a sensitive, safe, user-friendly point-of-care test, which will reduce turnaround time for detection of positive cases, considering remote locations of KFD-affected areas. Role of non-invasive specimens such as urine can be explored, which will lead to better patient compliance for sampling and follow up cases should be monitored for viral load in urine and blood. Review of vaccination strategies and detailed research for development of potential vaccine candidates are the need of the hour. A strong one-health approach with active inter-sectoral coordination with health, forest and livestock departments is essential for effective management and control of KFD. A systematic approach should be in place to do a serosurvey in northern India in fever cases to see if KFD exists in northern States of India.
Footnotes
Financial support & sponsorship: None.
Conflicts of Interest: None.
References
- 1.Work TH, Trapido H. Kyasanur forest disease, a new virus disease in India. Indian J Med Sci. 1957;11:341–5. [PubMed] [Google Scholar]
- 2.Work TH. Russian spring-summer virus in India: Kyasanur forest disease. Prog Med Virol. 1958;1:248–79. [PubMed] [Google Scholar]
- 3.Iyer CGS, Laxmana Rao R, Work TH, Narasimha Murthy DP. Kyasanur forest disease VI. Pathological findings in three fatal human cases of Kyasanur forest disease. Indian J Med Res. 1959;13:1011–22. [PubMed] [Google Scholar]
- 4.Work TH, Trapido H, Murthy DP, Rao RL, Bhatt PN, Kulkarni KG, et al. Kyasanur forest disease. III. A preliminary report on the nature of the infection and clinical manifestations in human beings. Indian J Med Sci. 1957;11:619–45. [PubMed] [Google Scholar]
- 5.Pavri K. Clinical, clinicopathologic, and hematologic features of Kyasanur forest disease. Rev Infect Dis. 1989;11(Suppl 4):S854–9. doi: 10.1093/clinids/11.supplement_4.s854. [DOI] [PubMed] [Google Scholar]
- 6.The Times News Network. Goa news 73 Kyasanur forest disease cases detected in Goa since January. The Times of India. 2017. Apr 18, [accessed on April 19, 2017]. Available from: http://www.timesofindia.indiatimes.com/city/goa/73-kfd-cases-detected-in-goa-since-jan/articleshow/58231025.cms .
- 7.Chari B. Goa News. 82 cases of Kyasanur forest disease reported since January. The Times of India. [Updated June 9, 2017]. accessed on October 4, 2017. Available from: https://www.timesofindia.indiatimes.com/city/goa/82-cases-of-kfd-reported-since-jan/articleshow/59060022.cms .
- 8.2017 ICD-10-CM Diagnosis Codes. [accessed on March 17, 2017]. Available from: http://www.icd10data.com/ICD10CM/Codes/A00-B99/A90-A99/A98-/A98.2 .
- 9.Centres for Disease Control and Prevention. Kyasanur forest disease (KFD): Signs and symptoms. [accessed on March 17, 2017]. Available from: http://www.cdc.gov/vhf/kyasanur/symptoms/index.html .
- 10.Holbrook MR. Kyasanur forest disease. Antiviral Res. 2012;96:353–62. doi: 10.1016/j.antiviral.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adhikari Prabhe MR, Prabhu MG, Raghaveer CV, Bai M, Male MA. Clinical study of 100 cases of KFD clinic pathological correlation. Indian J Med Sci. 1993;47:124–305. [PubMed] [Google Scholar]
- 12.John JK, Kattoor JJ, Nair AR, Bharathan AP, Valsala R, Sadanandan GV. Kyasanur forest disease: A status update. Adv Anim Vet Sci. 2014;4:329–36. [Google Scholar]
- 13.Pattnaik P. Kyasanur forest disease: An epidemiological view in India. Rev Med Virol. 2006;16:151–65. doi: 10.1002/rmv.495. [DOI] [PubMed] [Google Scholar]
- 14.Iyer CG, Laxmana Rao R, Work TH, Narasimha Murthy DP. Kyasanur forest disease VI. Pathological findings in three fatal human cases of Kyasanur forest disease. Indian J Med Sci. 1959;13:1011–22. [PubMed] [Google Scholar]
- 15.Mourya DT, Yadav PD. Recent scenario of emergence of Kyasanur forest disease in India and public health importance. Curr Trop Med Rep. 2016;3:7–13. [Google Scholar]
- 16.Ocular manifestations of Kyasanur forest disease (a clinical study) Indian J Ophthalmol. 1983;31:700–2. [PubMed] [Google Scholar]
- 17.Kasabi GS, Murhekar MV, Yadav PD, Raghunandan R, Kiran SK, Sandhya VK, et al. Kyasanur forest disease, India, 2011-2012. Emerg Infect Dis. 2013;19:278–81. doi: 10.3201/eid1902.120544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webb HE, Rao RL. Kyasanur forest disease: A general clinical study in which some cases with neurological complications were observed. Trans R Soc Trop Med Hyg. 1961;55:284–98. doi: 10.1016/0035-9203(61)90067-0. [DOI] [PubMed] [Google Scholar]
- 19.Wadia RS. Neurological involvement in Kyasanur forest disease. Neurol India. 1975;23:115–20. [PubMed] [Google Scholar]
- 20.Gurav YK, Yadav PD, Gokhale MD, Chiplunkar TR, Vishwanathan R, Patil DY, et al. Kyasanur forest disease prevalence in Western Ghats proven and confirmed by recent outbreak in Maharashtra, India, 2016. Vector Borne Zoonotic Dis. 2018;18:164–72. doi: 10.1089/vbz.2017.2129. [DOI] [PubMed] [Google Scholar]
- 21.Work TH, Roderiguez FR, Bhatt PN. Virological epidemiology of the 1958 epidemic of Kyasanur forest disease. Am J Public Health Nations Health. 1959;49:869–74. doi: 10.2105/ajph.49.7.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Banerjee K. Kyasanur forest disease. In: Monath TP, editor. Arboviruses: Epidemiology and ecology. Boca Raton, Florida: CRC Press; 1990. pp. 93–116. [Google Scholar]
- 23.Mourya DT, Yadav PD, Mehla R, Barde PV, Yergolkar PN, Kumar SR, et al. Diagnosis of Kyasanur forest disease by nested RT-PCR, real-time RT-PCR and IgM capture ELISA. J Virol Methods. 2012;186:49–54. doi: 10.1016/j.jviromet.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 24.Mourya DT, Yadav PD, Patil DY. Expediency of dengue illness classification: The Sri Lankan perspective highly infectious tick-borne viral diseases: Kyasanur forest disease and Crimean-Congo haemorrhagic fever in India. WHO South East. Asia J Public Health. 2014;3:8–21. doi: 10.4103/2224-3151.206890. [DOI] [PubMed] [Google Scholar]
- 25.Murhekar MV, Kasabi GS, Mehendale SM, Mourya DT, Yadav PD, Tandale BV, et al. On the transmission pattern of Kyasanur forest disease (KFD) in India. Infect Dis Poverty. 2015;4:37. doi: 10.1186/s40249-015-0066-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Department of Health Research. Establishment of a network of laboratories for managing epidemics and natural calamities (VRDL) [accessed on February 25, 2018]. Available from: https://dhr.gov.in/schemes/establishment-network-laboratories-managing-epidemics-and-natural-calamities .
- 27.Centers for Disease Control and Prevention. Fact Sheet: Kyasanur forest disease (KFD) [accessed on March 30, 2017]. Available from: https://www.cdc.gov/vhf/kyasanur/pdf/factsheet.pdf .
- 28.Porecha M. Monkey fever claims two lives in Maharashtra. Daily News and Analysis. 2017. Feb 19, [accessed on April 19, 2017]. Available from: http://www.dnaindia.com/india/report-monkey-fever-claims-two-lives-in-maharashtra-2327630 .
- 29.Tandale BV, Balakrishnan A, Yadav PD, Marja N, Mourya DT. New focus of Kyasanur forest disease virus activity in a tribal area in Kerala, India, 2014. Infect Dis Poverty. 2015;4:12. doi: 10.1186/s40249-015-0044-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mourya DT, Yadav PD, Sandhya VK, Reddy S. Spread of Kyasanur forest disease, Bandipur Tiger Reserve, India, 2012-2013. Emerg Infect Dis. 2013;19:1540–1. doi: 10.3201/eid1909.121884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yadav PD, Shete AM, Patil DY, Sandhya VK, Prakash KS, Surgihalli R, et al. Outbreak of Kyasanur forest disease in Thirthahalli, Karnataka, India, 2014. Int J Infect Dis. 2014;26:132–4. doi: 10.1016/j.ijid.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 32.KFD monkey fever reported in forest areas of Khanapur. 2016. Mar 19, [accessed on April 19, 2017]. Available from: https://www.allaboutbelgaum.com/news/kfd-monkey-fewer-reported-forest-areas-khanapur/
- 33.Boshell J, Rajagopalan PK. Observations on the experimental exposure of monkeys, rodents and shrews to infestation of ticks in forest in Kyasanur forest diseases area. Indian J Med Res. 1968;56:573–88. [PubMed] [Google Scholar]
- 34.National Health Portal of India. Kyasanur forest disease. [accessed on April 19, 2017]. Available from: https://www.nhp.gov.in/disease/communicable-disease/kyasanur-forest-disease .
- 35.Padbidri VS, Wairagkar NS, Joshi GD, Umarani UB, Risbud AR, Gaikwad DL, et al. A serological survey of arboviral diseases among the human population of the Andaman and Nicobar Islands, India. Southeast Asian J Trop Med Public Health. 2002;33:794–800. [PubMed] [Google Scholar]
- 36.Peterson AT, Talukdar G. Preliminary risk maps for transmission of Kyasanur forest disease in Southern India. Indian J Public Health. 2017;61:47–50. doi: 10.4103/0019-557X.200262. [DOI] [PubMed] [Google Scholar]
- 37.Work TH, Trapido H. Kyasanur Forest Disease: A new infection of man & monkeys in tropical India by a virus of the Russian Spring-Summer complex.Proc. Ninth Pacific Science Congress. 1957;17:80–4. [Google Scholar]
- 38.National Centre for Disease Control. CD Alert. Kyasanur forest disease: A public health concern. [accessed on March 17, 2018]. Available from: http://www.idsp.nic.in/WriteReadData/l892s/60398414361527247979.pdf .
- 39.Ghosh S, Azhahianambi P, Yadav MP. Upcoming and future strategies of tick control: A review. J Vector Borne Dis. 2007;44:79–89. [PubMed] [Google Scholar]
- 40.Kiran SK, Pasi A, Kumar S, Kasabi GS, Gujjarappa P, Shrivastava A, et al. Kyasanur forest disease outbreak and vaccination strategy, Shimoga district, India, 2013-2014. Emerg Infect Dis. 2015;21:146–9. doi: 10.3201/eid2101.141227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kasabi GS, Murhekar MV, Sandhya VK, Raghunandan R, Kiran SK, Channabasappa GH, et al. Coverage and effectiveness of Kyasanur forest disease (KFD) vaccine in Karnataka, South India, 2005-10. PLoS Negl Trop Dis. 2013;7:e2025. doi: 10.1371/journal.pntd.0002025. [DOI] [PMC free article] [PubMed] [Google Scholar]


