Abstract
Background:
During decortication surgery, fibrous peel over the lung was removed to allow expansion of the lung and therefore, wide raw area was created with surface oozing. The phenomenon of fibrinolysis usually activated after such procedure, resulting in increasing the postoperative bleeding. Tranexamic acid is one of antifibrinolytic therapies that could be used topically and to targets directly the source of bleeding and reducing the local activation of the fibrinolytic process and consequently reducing the postoperative bleeding.
Patients and Methods:
A total of 70 patients underwent lung decortication surgery in Cardiothoracic Surgery Department at Tanta University Hospital from January 2015 to May 2017. Patients were randomly allocated into two groups, Group I (35 patients) receiving 3 g of tranexamic acid in 100 ml of saline solution and Group II (35 patients) receiving 100 ml of saline solution as placebo. At the end of the operation and before closing the chest, in both groups, drug or placebo solution was distributed locally all over the pleural cavity. Comparison between the groups was done regarding the amount of postoperative bleeding, postoperative hemoglobin in the first 24 and 48 h postoperatively, blood transfusion, Intensive Care Unit (ICU) stay, and hospital stay.
Results:
Both groups were comparable regarding demographic and surgical data. Group I patients had the significantly lesser amount of postoperative blood loss than Group II during the first postoperative 48 h, and hence, the need of postoperative blood transfusion was significantly lower in Group I with better postoperative hemoglobin level than Group II. However, there was no difference in overall ICU and hospital stay.
Conclusion:
The local intrapleural use of tranexamic acid after decortication surgery of the lung is safe and significantly reduces the amount of postoperative blood loss and in consequence reduces the amount of postoperative blood transfusion.
Keywords: Lung decortication, postoperative bleeding, randomized trial, tranexamic acid
Introduction
Increased morbidity, mortality, and health-care cost are common complications from excessive postoperative bleeding.[1]
The incidence of patients’ reexploration in thoracic surgery for bleeding ranges from 1% to 3.7%, whereas the incidence for blood transfusion ranges from 20% to 52%.[2,3]
The serous membranes (pleura, pericardium, peritoneum, and meninges) when exposed to surgical insult, releases a high amount of plasminogen activators which result in increased local fibrinolytic activity and thus excessive bleeding occur.[4,5]
Tranexamic acid has been found to act either systemically or topically by binding to lysine binding sites of plasmin and plasminogen. Saturation of these sites blocks the attachment of plasminogen to fibrin thus inhibiting fibrinolysis.[6,7]
Systematic review and meta-analysis of randomized control trials showed that local application of tranexamic acid significantly decrease intraoperative blood loss in primary total hip replacement and reduce transfusion rates.[8] Furthermore, other studies used tranexamic acid topically after coronary artery bypass graft and concluded that such topical application results in a decrease in postoperative blood loss without imposing extra risks on the patients.[9]
The aim of this study is to evaluate the efficacy of local application of tranexamic acid in the pleural cavity after surgeries for decortication of the lung through open thoracotomy on postoperative blood loss.
Patients and Methods
From January 2015 to May 2017, 70 patients underwent lung decortication surgery in Cardiothoracic Surgery Department, Tanta University Hospital.
After having the approval from the ethical committee at the university hospital, these group of patients were studied in a prospective, randomized, double-blind placebo controlled study.
All selected patients underwent decortication surgery for chronic thoracic empyema, encysted effusion, or clotted hemothorax on the elective way. We excluded all patients required lung resection, reopening due to surgical bleeding, patients requiring anticoagulant postoperatively for fear of deep vein thrombosis, patients with renal failure, patients with liver cirrhosis, primary blood disease such as hemophilia or else, know allergy to tranexamic acid, and pregnant female patients.
Patients were allocated into two groups, Group I (35 patients) received 3 g of tranexamic-acid in 100 ml of saline solution for proper distribution all over the thoracic cavity and Group II (35 patients) received 100 ml of saline solution as placebo in a double-blind way, in both groups, solution was distributed locally all over the pleural cavity at the end of operation and before closing the chest. The choice of the doses was decided on the arbitrary way, 3 g is an average dose between (1 and 5 g) that has been used in other studies.
Blocked randomization was used to divide the patients into two groups, each block consists of 35 patients, and all surgical team, circulating nurse, ward staff, and intensive care staff were blinded regarding the study population. The bottles either containing the tranexamic acid or placebo were prepared the day of surgery in a sterile way by the resident staff that has no role in the surgical procedure but start scrubbing after positioning of the patient and only helping the research work by delivering the bottles in a randomized way to the operating room.
Hemostasis was done, and the solution was poured into the pleural cavity immediately before closing the ribs and chest tubes were clamped the time needed for closure of the chest (30–45 min).
The total drainage was measured every 4 h in the first 24 h postoperatively in both groups then after that, chest tubes drainage is evaluated to differentiate by physical examination between blood and serosanguinous pleural fluid drainage.
Postoperative blood transfusion was given according to the following protocol, blood transfusion is not indicated when hemoglobin concentration is more than 10 g/dl. Blood transfusion is indicated when hemoglobin concentration is <8 g/dl. Two units of the red cell should be transfused, and then, the clinical situation and hemoglobin concentration should be reassessed.
Blood transfusion is indicated in patients with hemoglobin between 8 and 10 g/dl if they are symptomatic or in patients who tolerate anemia poorly, for example, patients over 65 years or those with cardiovascular diseases or respiratory diseases.
We have followed the following protocol for chest tubes removal: removed sequentially, if no bleeding, no pus drainage, no air leakage, and pleural effusion drainage <200 cc/day.
Intensive Care Unit (ICU) and hospital stay time were recorded.
Technique of study
Under general anesthesia, standard posterolateral thoracotomy in all patients and lung decortication was carried out for removal of all fibrous peel over the lung with or without pleurectomy.
Regular hemostasis performed and all bleeding points were secured.
Only before closure of the chest, 3 g of tranexamic acid diluted in 100 ml of normal saline and was distributed all over the pleural cavity for the Group I and in Group II, 100 ml of normal saline was used instead.
The chest was closed in layers with two chest tubes inserted for drainage and connected to underwater seal system.
Statistical analysis
The collected data were organized, tabulated and statistically analyzed using the Statistical Package for the Social Sciences software (SPSS, IBM, Chicago, USA) version 22. For quantitative data, the range, mean and standard deviation were calculated. For qualitative data, the comparison between two groups and more was done using Chi-square test. For comparison between means of two groups of parametric data, Student's t-test was used.
Results
There were seventy patients included in the study, 35 patients in Group I and 35 patients in Group II.
Both groups were comparable and showed no significant differences regarding their age, sex, and surgical indication for decortication [Table 1].
Table 1.
Demographic data and indication for surgery
| Group I | Group II | Test | P | |
|---|---|---|---|---|
| Age | ||||
| Range | 18-68 | 19-69 | T: 0.911 | 0.343 |
| Mean±SD | 41.97±14.65 | 45.20±13.64 | ||
| Sex (%) | ||||
| Male | 21 (60) | 20 (57.1) | χ2: 0.059 | 0.808 |
| Female | 14 (40) | 15 (42.9) | ||
| Indication for decortication (%) | ||||
| Chronic empyema | 21 (60) | 26 (74.3) | χ2: 1.624 | 0.444 |
| Clotted hemothorax | 8 (22.9) | 5 (14.3) | ||
| Encysted effusion | 6 (17.1) | 4 (11.4) |
SD: Standard deviation
No significant difference between both groups regarding ICU stay and hospital stay were noted [Table 2]. However, patients in Group I had significant better hemoglobin level during the first and second day postoperatively (P = 0.019 and 0.001), and received lesser units of blood transfusion (P = 0.001).
Table 2.
Blood transfusion, Intensive Care Unit and hospital stay, pre- and post-operative hemoglobin
| Group I | Group II | Test | P | |
|---|---|---|---|---|
| Blood transfusion | ||||
| Range | 0-2 | 0-3 | T: 12.814 | 0.001* |
| Mean±SD | 0.69±0.90 | 1.54±1.09 | ||
| ICU stay | ||||
| Range | 1-3 | 1-3 | T: 0.633 | 0.429 |
| Mean±SD | 1.34±0.59 | 1.46±0.61 | ||
| Hospital stay | ||||
| Range | 4-9 | 4-9 | T: 0.593 | 0.444 |
| Mean±SD | 6.11±1.51 | 6.40±1.59 | ||
| Preoperative Hgb | ||||
| Range | 10-11.5 | 10-11 | T: 1.573 | 0.214 |
| Mean±SD | 10.59±0.43 | 10.47±0.35 | ||
| Hgb in the first 24 h | ||||
| Range | 7.5-10 | 7.5-10 | T: 5.804 | 0.019* |
| Mean±SD | 8.81±0.81 | 8.36±0.74 | ||
| Hgb in the second 24 h | ||||
| Range | 8.4-9.7 | 8-9.5 | T: 11.649 | 0.001* |
| Mean±SD | 8.93±0.44 | 8.56±0.46 |
Hgb: Hemoglobin, SD: Standard deviation, ICU: Intensive Care Unit, *: Statistically significant at P ≤ 0.05
In spite of both groups had no statistically significant differences in the amount of blood loss during the surgical procedures [Table 3]. Group I had statistically significant lesser amount of postoperative blood loss starting from immediate postoperative time (4 h) and continued lesser in all the measurements up to 48 h postoperatively [Table 2 and Figure 1].
Table 3.
Intraoperative and postoperative blood loss
| Blood loss | Group I | Group II | t-test | P |
|---|---|---|---|---|
| Intraoperative | ||||
| Range | 200-550 | 200-500 | 0.052 | 0.821 |
| Mean±SD | 340.0±114.28 | 334.29±95.31 | ||
| Post 4 h | ||||
| Range | 50-200 | 100-250 | 20.799 | 0.001* |
| Mean±SD | 115.50±41.99 | 180.50±47.96 | ||
| Post 8 h | ||||
| Range | 70-300 | 130-300 | 15.078 | 0.001* |
| Mean±SD | 150.00±56.85 | 218.50±54.70 | ||
| Post 12 h | ||||
| Range | 80-350 | 170-360 | 15.465 | 0.001* |
| Mean±SD | 179.50±65.01 | 258.50±62.01 | ||
| Post 16 h | ||||
| Range | 100-450 | 200-430 | 13.499 | 0.001* |
| Mean±SD | 209.00±78.93 | 297.00±72.41 | ||
| Post 20 h | ||||
| Range | 120-500 | 240-500 | 14.326 | 0.001* |
| Mean±SD | 239.00±86.63 | 340.50±82.94 | ||
| Post 24 h | ||||
| Range | 130-500 | 280-550 | 18.212 | 0.001* |
| Mean±SD | 267.50±86.93 | 385.00±87.21 | ||
| Post 48 h | ||||
| Range | 200-700 | 400-850 | 30.342 | 0.001* |
| Mean±SD | 382.50±119.51 | 632.50±164.06 |
SD: Standard deviation, *: Statistically significant at P ≤ 0.05
Figure 1.
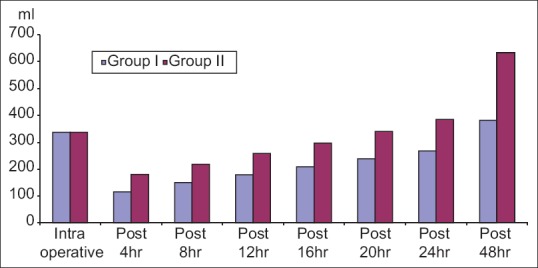
Intraoperative and postoperative blood loss
Discussion
A phenomenon of activation of fibrinolysis during and after surgical intervention is a well-known phenomenon. The surgical trauma to the serous membrane, operative blood loss with consumption of clotting factors and platelet, and administration of crystalloids and or colloids during or after the surgery, all are precipitating factors for activation of fibrinolysis cascade.[10,11,12]
Decortication surgery of the lung is one of the best examples of cases where patients may suffer this phenomenon.
Hence, using antifibrinolytic therapy postoperatively to minimize such bleeding is indicated and has proved its efficacy in the field of cardiothoracic surgery. To minimize the side effects of the thrombotic tendency by systemic infusion, local administration of tranexamic acid has been studied in cardiac and noncardiac surgery with encouraging results.[9,13]
A dose of 1 g of tranexamic acid in 100 ml saline was used both by De Bonis et al.[14] and Fawzy et al.[9] in their study in patients undergoing coronary artery bypass graft surgery before closing the chest with very favorable results with significant reduction of postoperative bleeding.
In our study, we used 3 g of tranexamic acid in 100 ml saline before closing the chest after decortication surgery. We used larger amount than open heart surgery because the raw surface area after decortication surgery is larger and we did not report any side effect of such doses but rather a significant clinical and statistical reduction in postoperative bleeding in the first 48 h postoperatively in patients in Group I than patients in Group II.
Dell’Amore et al. in 2012 used the tranexamic acid after thoracic surgery (resection surgeries) in topical form by pouring 5 g of tranexamic acid in 100 saline before closing the chest and proved its statistical and clinical effect in reducing the postoperative bleeding in this group of patients in comparison to other group of patients who received a placebo in the form of 100 ml saline.[15] They reported that no side effects due to such doses.
So which dose is the best, more effective and safe is not clear until now, but in the literature, it has been hypothesized that topical antifibrinolytic agents directly target the source of bleeding and reducing the local activation of the fibrinolytic process.[5]
We proved the effective role of the topical use of tranexamic acid in reducing the postoperative bleeding after decortication surgery of the lung (P = 0.001) associated with significant reduction in blood transfusion, even if there was no significant impact on ICU or hospital stay.
Conclusion
The local intrapleural use of tranexamic acid after decortication surgery of the lung is safe and significantly reduces the amount of postoperative blood loss and in consequence, reduces the amount of postoperative blood transfusion.
Study limitations
The study population needs to be on a larger scale to have more powered results, and the dose of tranexamic acid is somewhat arbitrary and needs to be more sharply defined.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank the involved residents (Dr. Mostafa Elhamshary and Dr. Ahmed Magdy) who was responsible for delivering the topical tranexamic acid versus the placebo in the operative room while the rest of the team in the OR and ICU were blinded to what is poured in the chest.
References
- 1.Tang GH, Maganti M, Weisel RD, Borger MA. Prevention and management of deep sternal wound infection. Semin Thorac Cardiovasc Surg. 2004;16:62–9. doi: 10.1053/j.semtcvs.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 2.Bedirhan MA, Turna A, Yagan N, Taşçi O. Aprotinin reduces postoperative bleeding and the need for blood products in thoracic surgery: Results of a randomized double-blind study. Eur J Cardiothorac Surg. 2001;20:1122–7. doi: 10.1016/s1010-7940(01)01016-8. [DOI] [PubMed] [Google Scholar]
- 3.Sirbu H, Busch T, Aleksic I, Lotfi S, Ruschewski W, Dalichau H, et al. Chest re-exploration for complications after lung surgery. Thorac Cardiovasc Surg. 1999;47:73–6. doi: 10.1055/s-2007-1013114. [DOI] [PubMed] [Google Scholar]
- 4.Wang NS. Anatomy and physiology of the pleural space. Clin Chest Med. 1985;6:3–16. [PubMed] [Google Scholar]
- 5.Khalil PN, Ismail M, Kalmar P, von Knobelsdorff G, Marx G. Activation of fibrinolysis in the pericardial cavity after cardiopulmonary bypass. Thromb Haemost. 2004;92:568–74. doi: 10.1160/TH03-07-0455. [DOI] [PubMed] [Google Scholar]
- 6.Longstaff C. Studies on the mechanisms of action of aprotinin and tranexamic acid as plasmin inhibitors and antifibrinolytic agents. Blood Coagul Fibrinolysis. 1994;5:537–42. [PubMed] [Google Scholar]
- 7.Adler Ma SC, Brindle W, Burton G, Gallacher S, Hong FC, Manelius I, et al. Tranexamic acid is associated with less blood transfusion in off-pump coronary artery bypass graft surgery: A systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2011;25:26–35. doi: 10.1053/j.jvca.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg Br. 2011;93:39–46. doi: 10.1302/0301-620X.93B1.24984. [DOI] [PubMed] [Google Scholar]
- 9.Fawzy H, Elmistekawy E, Bonneau D, Latter D, Errett L. Can local application of tranexamic acid reduce post-coronary bypass surgery blood loss? A randomized controlled trial. J Cardiothorac Surg. 2009;4:25. doi: 10.1186/1749-8090-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litle VR, Swanson SJ. Postoperative bleeding: Coagulopathy, bleeding, hemothorax. Thorac Surg Clin. 2006;16:203–7. doi: 10.1016/j.thorsurg.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 11.Pavie A, Szefner J, Leger P, Gandjbakhch I. Preventing, minimizing, and managing postoperative bleeding. Ann Thorac Surg. 1999;68:705–10. doi: 10.1016/s0003-4975(99)00628-1. [DOI] [PubMed] [Google Scholar]
- 12.Tanaka KA, Key NS, Levy JH. Blood coagulation: Hemostasis and thrombin regulation. Anesth Analg. 2009;108:1433–46. doi: 10.1213/ane.0b013e31819bcc9c. [DOI] [PubMed] [Google Scholar]
- 13.Dunn CJ, Goa KL. Tranexamic acid: A review of its use in surgery and other indications. Drugs. 1999;57:1005–32. doi: 10.2165/00003495-199957060-00017. [DOI] [PubMed] [Google Scholar]
- 14.De Bonis M, Cavaliere F, Alessandrini F, Lapenna E, Santarelli F, Moscato U, et al. Topical use of tranexamic acid in coronary artery bypass operations: A double-blind, prospective, randomized, placebo-controlled study. J Thorac Cardiovasc Surg. 2000;119:575–80. doi: 10.1016/s0022-5223(00)70139-5. [DOI] [PubMed] [Google Scholar]
- 15.Dell’Amore A, Caroli G, Nizar A, Cassanelli N, Luciano G, Greco D, et al. Can topical application of tranexamic acid reduce blood loss in thoracic surgery? A prospective randomised double blind investigation. Heart Lung Circ. 2012;21:706–10. doi: 10.1016/j.hlc.2012.06.016. [DOI] [PubMed] [Google Scholar]


