Abstract
Background
The elderly population presents higher morbidity of H. pylori associated diseases in proximal stomach. The specific pathogenesis and mechanism have not been clearly addressed. The gastric environment for H. pylori colonization is dynamic with increasing age. The aim of present study is to investigate the correlation among the distribution of H. pylori, mucosal inflammation, gastric microenvironment and age.
Methods
A total of 180 patients with dyspepsia symptoms were divided into young, middle-aged and elderly groups. Biopsies were obtained from each patient in five locations: great curvature (mid-corpus, mid-antrum), lesser curvature (mid-corpus, mid-antrum) and incisura angularis (IA), analyzed for H. pylori density, mucosal inflammation and histopathology.
Results
The infection rate of H. pylori increased linearly with age (p < 0.001) in corpus, but not in antrum and IA. The H. pylori density was significantly aggravated in IA (p = 0.002) and corpus (p < 0.001) in elderly patient, but not in antrum. The mucosa inflammation scores were consistent with the severity of H. pylori colonization among three age groups. In elderly patients, the pyloric glands present more frequently in corpus, comparing with young and middle-aged group. A significant positive correlation among aggravating severity of H. pylori infection, mucosal inflammation and pyloric metaplasia in corpus with increasing age (p < 0.001) was occurred.
Conclusions
With increasing age, both topographic distribution of H. pylori and the expansion of pyloric glands increased in a distal-to-proximal gastric direction. Pyloric metaplasia in corpus was correlated with the risk of aggravated H. pylori colonization and associated inflammation in elderly population.
Keywords: Helicobacter pylori, Pyloric glands, Metaplasia, Aged
Background
Helicobacter pylori were catapulted to the hot field of gastroenterological research in less than three decades after its discovery in 1983 by Warren and Marshall [1]. Since then, evidence has accumulated to link H. pylori to chronic gastritis, gastric ulcer, gastric carcinoma and lymphoma [2–10], which are referred to as H. pylori associated diseases. Eradication of H. pylori significantly decreases the risk of these diseases.
There is convincing evidence that the elderly population has a significantly higher mean morbidity of H. pylori associated diseases than young people [11–13]. Graham et al. have reported that H. pylori infection prevalence increased gradually with age, leveling out at 60–70% in elderly people from less than 20% in 25–30-year-olds [14]. Note, H. pylori associated diseases, such as ulcers and gastric cancer, are more evenly distributed throughout the stomach in the elderly, particularly in proximal stomach [11, 12, 15]. However, the specific pathogenesis and mechanism of the high prevalence of H. pylori associated diseases in proximal stomach of elderly population have not been clearly addressed.
H. pylori organisms within the mucous layer are exposed to different local microenviorment in the antrum and body. H. pylori have been shown to present a strong affinity to gastric-type epithelium, prefer to colonize first and initiate in the lower part of stomach (antrum) [15, 16]. Within different gastric niches, the pH levels [17], distribution and viscosities of mucin glycoforms [18] and binding of H. pylori to gastric mucins in a pH-dependent manner [19] might impact on the H. pylori adaption. Recent studies have reported that gastric mucin plays dual roles in preventing gastric cancer by inhibiting H. pylori infection and suppressing tumor-promoting inflammation [20–22].
At the meanwhile, the tendency of pyloric gland moving to proximal stomach changed with increasing age has been demonstrated [15, 17]. In gastric body or at the body-antrum junction, the gland was specially replaced by mucous-secreting glands with increasing age, which is identified as pyloric metaplasia or named as antralization. Therefore, our hypothesis was that age-related pyloric metaplasia can effect H. pylori distribution in stomach, which might contribute to the high morbidity of H. pylori associated disease in the elderly population, especially in proximal stomach. The dynamic characteristics of H.pylori colonization in different gland types with increasing age has not been reported yet.
Our study aims to investigate the correlation among age, H. pylori distribution, gastric gland type and mucosa inflammation in different areas of stomach.
Methods
Patients
A total of 180 patients (105 men, median age: 45.5 years, range: 20–80 years) who were admitted to outpatient clinic center with complains of dyspepsia and present the normal findings of upper gastrointestinal endoscopy were enrolled into this study. This study was conducted at Wuhan Union Hospital. Exclusion criteria were: (1) patients with visible abnormalities detected through endoscopy; (2) previous H. pylori eradication treatment; (3) use of PPI (proton pump inhibitors), H2-receptor antagonists, bismuth preparations and antibiotics in the preceding two weeks; (4) severe or unstable cardiovascular, pulmonary, renal or hepatic disease or endocrine disease in whom endoscopy would not be safe; (5) hematological disorder or concomitant anticoagulant; (6) pregnant or nursing women.
Patients were divided into three groups: young group (20–25 years old), middle-aged group (40–50 years old) and elderly group (> 60 years old). There were 60 patients in each group. Informed consent was obtained from all patients.
Endoscopy procedure
We employed both white light endoscopy using an OLympus GIF-Q260Z instrument, and endoscope-based confocal laser endomicroscopy (CLE) using a Cellvizio GastroFlex UHD instrument. A full assessment of the upper gastrointestinal tract for each patient was carried out first using white light endoscopy according to a standard protocol. One endoscopist (R.L.) experienced with endomicroscopy carried out the CLE. At least 10 images were obtained from the great curvature, lesser curvature and incisura angularis (IA). H. pylori infection was diagnosed on the basis of CLE criteria while the image was generated as described in previous study [23].
In each patient, biopsies from 5 predetermined sites: great and lesser curvature of the mid-antrum (2-3 cm from pylori, A1, A2), lesser curvature of the mid-body (4 cm proximal from IA, B1), great curvature of the mid-body (8 cm from cardia, B2) and IA, as described in updated Sydney system were taken [2, 24] (Fig. 1).
Fig. 1.
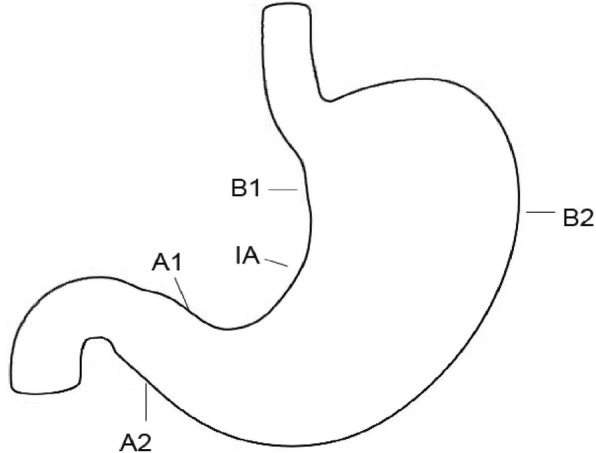
A schematic illustration of Gastric biopsies carried out in present study. Gastric biopsies were obtained from the stomach in five locations: lesser curvature (mid-antrum, A1; mid-corpus, B1), greater curvature (mid-antrum, A2; mid-corpus, B2) and incisura angularis(IA) according to the updated Sydney system
Histology and H. pylori status
Each biopsy was immediately subjected to a 1-min ultra-rapid urease test (URUT test kit, Sanqiang Bio. co., Jiangsu, China), and the color change was noted after 1 min. Then formalin fixation and paraffin blocks were prepared. The sections stained with haematoxylin and eosin for histopathological details were used to demonstrate gland type and mucosa inflammation. The Giemsa staining and CLE images was performed to measure H. pylori density.
H. pylori infection was confirmed when URUT and histopathological result were both positive. The H. pylori density in single field was grades as: 0, normal (did not detect H. pylori colonization, Grade 0); 1, sporadic (single cluster was detected in one villus, Grade 1); 2, small amount (H. pylori diffused distributed in more than one villus, Grade 2); 3, moderate (the medium amount of H. pylori in the field, Grade 3); 4, marked (the field was filled with H. pylori, Grade 4). And the mucosal inflammation was scored as: 0, normal; 1, very mild; 2, mild; 3, moderate; 3, marked [24]. The H. pylori infection in antrum was defined as positive with either A1 or A2 present positive. The average score in A1 and A2 was used to evaluate H. pylori infection and mucosal inflammation in antrum for each patient. So did B1 and B2 in corpus.
Statistical analysis
The H.pylori infection rates and detection rates of pyloric gland in antrum, IA and corpus with increasing age were analyzed by a Chi-square test, respectively. The density of H.pylori colonization and H. pylori associated mucosal inflammation in antrum, IA and corpus with increasing age were tested by Kruskal-Wallis H test, respectively. The density of H.pylori colonization between young group and elderly group was tested by One-way ANOVA. A chi-square test was performed to analyze the correction between the mucosal inflammation and H. pylori colonization. The Pearson correlation was used to observe the relation between H. pylori infection rate and proximal expansion of pyloric gland. The correlation between the colonization of H. pylori-associated mucosal inflammation and the gland type expansion was determined with a chi-square test. The correlation among H. pylori colonization, severity of mucosal inflammation, pyloric metaplasia and age was further measured with zero-order (Pearson) multiple correlations. Statistical significance of differences and relationships were determined by p values of less than 0.05.
Results
H. pylori infection rates increase with age in the gastric corpus
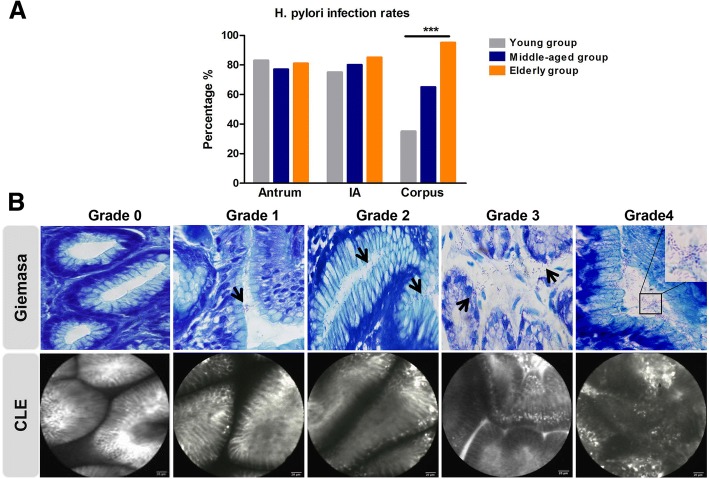
H. pylori infection rates were 83%, 77% and 81% respectively in three age-based groups, (young, middle-aged, elderly group) in antrum. The rates presented 75%, 80% and 85% in IA (Fig. 2a), and there was no significance among three groups. The infection rates in corpus increased linearly with age, being 35%, 65%, and 95% in young, middle-aged and elderly populations separately (Fig. 2a, p < 0.001). The data indicated that H. pylori infection rate presented as an age-dependent tendency in corpus, but not in antrum and IA.
Fig. 2.
The distribution and severity of H. pylori in stomach in different age groups. a H. pylori infection rates in antrum, incisura angularis (IA) and corpus with increasing age. b The H. pylori colonization density was graded by Giemsa staining (upper panel) and confocal laser endomicroscopy (lower panel). A total of 20 high power (× 40 objective) microscopic fields were randomly choosed in each Giemsa staining sample, and the average scores of those 20 fields for each slide were defined as H. pylori density scores. *** p < 0.001
H. pylori colonization extend proximally with increasing age
The severity of H. pylori colonization were further detected by Giemsa staining and CLE examination as described in methods (shown in Fig. 2b). The mean H. pylori density scores in antrum were around 1.5 without significant difference among three age groups (Table 1). The H. pylori density scores were dramatically elevated in IA (p=0.031) and corpus (p < 0.001) comparing among young, middle-aged and elderly group. With increasing age, there was no statistically difference of H. pylori grading/density score in antrum, the scores in IA were increasing slightly (the difference present between young group and elderly group, but not middle-aged group), while the elevation of infection scores in corpus was significant. It suggests that H. pylori distribution in proximal atomach augmented with increasing age.
Table 1.
The severity and distribution of H.pylori colonization with increasing age
| Age group | Antrum | IA | Corpus | P Value |
|---|---|---|---|---|
| Young group (20y-25y) | 1.30 ± 0.11 | 1.12 ± 0.11* | 0.50 ± 0.10 | < 0.001 |
| Mid-aged group (40y-50y) | 1.52 ± 0.14 | 1.25 ± 0.12 | 1.05 ± 0.12 | 0.031 |
| Elderly group (>60y) | 1.58 ± 0.13 | 1.55 ± 0.12* | 1.58 ± 0.10 | 0.974 |
| Kruskal-Wallis H (p) | 0.257 | 0.031 | < 0.001 | – |
*means a statistically significant difference between young group and elderly group in IA, p = 0.002. IA incisura angularis
H. pylori associated mucosal inflammation aggravate in elderly patient, especially in proximal stomach
Among three age groups, the mean grading/density scores for mucosal inflammation were 1.20, 1.57, and 1.72 respectively in antrum, 0.85, 1.45, 1.77 in IA and 0.37, 1.03, 1.83 in corpus (Table 2). The mucosal inflammation was statistically correlated to H. pylori colonization (Table 3, X2 = 102.68, p < 0.001). In young group, the antrum presented more severe inflammation with H. pylori infection (p < 0.001), comparing with IA and corpus. However, the mucosal inflammation density in corpus dramatically increased in elderly group (p < 0.001) and did not show the significant difference with antrum in the same age group. These data demonstrate that the H. pylori associated mucosal inflammation aggravated in elderly patient, especially in proximal stomach.
Table 2.
The characters of H. pylori associated gastric mucosal inflammation in different age population: H. pylori associated mucosal inflammation aggravate in elderly patient, especially in proximate stomach
| Age group | Antrum | IA | Corpus | p Value |
|---|---|---|---|---|
| Young group(20y~25y) | 1.20 ± 0.17 | 0.85 ± 0.13 | 0.37 ± 0.10 | < 0.001 |
| Mid-aged group(40y~50y) | 1.57 ± 0.19 | 1.45 ± 0.19 | 1.03 ± 0.13 | 0.077 |
| Elderly group(>60y) | 1.72 ± 0.19 | 1.77 ± 0.17 | 1.83 ± 0.18 | 0.902 |
| Kruskal-Wallis H (p) | 0.132 | < 0.001 | < 0.001 | – |
IA Incisura angularis, Data present as standard error of the mean
Table 3.
The characters of H. pylori associated gastric mucosal inflammation in different age population: The mucosa inflammation is consistent with the severity of H. pylori colonization
| Mucosal inflammation | H.pylori(+) | H.pylori (−) | Total |
|---|---|---|---|
| + | 292 | 30 | 322 |
| – | 114 | 104 | 218 |
| Total | 406 | 134 | 540 |
X2 = 102.68, p < 0.001
Pyloric metaplasia frequently present in elderly population
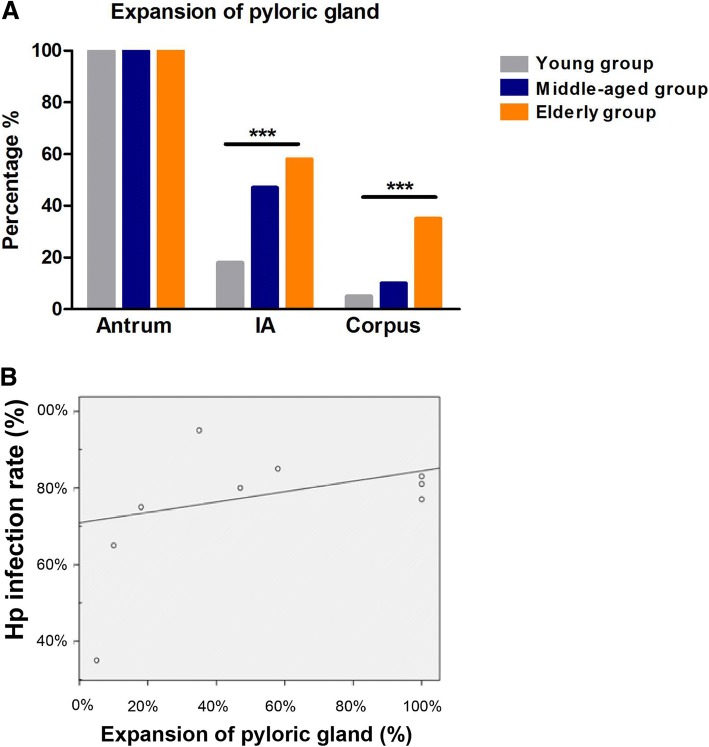
Among three different age groups, the detection rate of pyloric gland present equally 100% in antrum, 18%, 47%, 58% respectively in IA and 5%, 10%, 35% in corpus, shown as Fig. 3a. The frequencies of pyloric gland in IA and corpus were significantly increased with increasing age (Fig. 3a, X2 = 20.97, p < 0.001; X2 = 22.32, p < 0.001).
Fig. 3.
The association of H. pylori distribution and pyloric metaplasia with increasing age. a Distribution of pylori gland in different sites of stomach in different age groups. *** p < 0.001. b The correlation between the infection rate of H. pylori and the gland type expansion in five sites among three age groups
The colonization of H. pylori and H. pylori associated mucosal inflammation are correlated to the gland type expansion with age separately
The Pearson correlation was used to observe the relation between H. pylori infection rate and proximal expansion of pyloric gland. The coefficient was 0.804 (Fig. 3b, p < 0.01). The data showed that H. pylori infection dynamically correlated with pyloric gland with increasing age.
The correlation of H. pylori associated mucosal inflammation and pyloric metaplasia was determined with Chi-Square Goodness-of-Fit Test. The mucosal inflammation presents a correlation with pyloric metaplasia similar as H. pylori infection with age-dependent tendency (Table 4, X2 = 106.14, p < 0.001).
Table 4.
The correlation between the colonization of H. pylori-associated mucosal inflammation and the gland type expansion
| Mucosal inflammation | Pyloric gland (+) | Fundic gland (−) | Total |
|---|---|---|---|
| + | 228 | 94 | 322 |
| – | 56 | 162 | 218 |
| Total | 284 | 256 | 540 |
X2 = 106.14, p < 0.001
Pyloric metaplasia in corpus is correlated with the aggravated H. pylori colonization and associated inflammation in elderly population
As shown above, the H. pylori infection rates, severity of H. pylori colonization and mucosal inflammation predominantly aggravated in corpus with increasing age, comparing with antrum and IA. The increase of pyloric metaplasia in corpus with age was also confirmed as Fig. 3a depicted. To evaluate the mechanism of pyloric metaplasia with age on H. pylori associated inflammation in corpus, the correlation among H. pylori colonization, severity of mucosal inflammation, pyloric metaplasia and age was further measured with zero-order (Pearson) multiple correlations. Mucosa inflammation and H. pylori density were evaluated as variables in the calculation with pyloric gland and age as controlling variables. The Table 5 revealed the significant correlation among these four dimensions (p < 0.001), which indicated that pyloric metaplasia in corpus was correlated with the aggravated H. pylori colonization and inflammation in elderly population.
Table 5.
Multiple correlation analysis among mucosal inflammation, Hp density, the pyloric gland and age in corpus
| Correlationsa,b,c | Mucosal inflammation | Hp density | Pyloric gland | Age | |
|---|---|---|---|---|---|
| Mucosal inflammation | Correlation | 1.00 | 0.90 | 0.57 | 0.48 |
| Significance(2-detailed) | – | 0.00 | 0.00 | 0.00 | |
| Hp density | Correlation | 0.90 | 1.00 | 0.43 | 0.50 |
| Significance(2-detailed) | 0.00 | – | 0.00 | 0.00 | |
| Pyloric gland | Correlation | 0.57 | 0.43 | 1.00 | 0.33 |
| Significance(2-detailed) | 0.00 | 0.00 | – | 0.00 | |
| Age | Correlation | 0.48 | 0.50 | 0.33 | 1.00 |
| Significance(2-detailed) | 0.00 | 0.00 | 0.00 | – | |
acells contain zero-order (Pearson) correlations, bmucosal inflammation and Hp density were choosen as variables, cpyloric gland and age were set as controlling variables
Discussion
Epidemiologic studies on H. pylori infection in elderly people reported a prevalence of 60% in asymptomatic subjects and more than 70% in elderly patients with gastrointestinal diseases [25]. In particularly, the elderly population presents a significantly higher mean morbidity of H. pylori associated diseases [2–6], such as chronic gastritis, gastric ulcer and gastric carcinoma, especially in proximal stomach [11, 12, 15]. However, the mechanisms underlying the markedly elevated morbidity of H. pylori associated diseases in proximal stomach of elderly population are still not clear.
In the present study, biopsies from five predetermined sites in stomach were taken from each patient to approach the correlation among H. pylori distribution, mucosa inflammation, gland type and age in different areas of stomach. Misra et al. have shown the utility of using the same biopsy specimen for two tests [26].
The average infection rate of H. pylori in antrum and gastric corpus were about 80% and 65% respectively in our study, which were higher than developed countries [25, 27, 28]. The subjects observed in present study are patients with dyspepsia symptoms,which might be the reason for the higher H. pylori infection rate. It was also probably due to public health condition and eating habit in China. Note, data from our research further demonstrated that the aggravations of both H. pylori infection rate and H. pylori colonization severity in corpus was more conspicuous than the antrum and IA with increasing age, which clearly revealed that the distribution of H. pylori extends to proximal stomach with increasing age.
The mucosal inflammation was also observed in functional gastrointestinal disorder patients with dyspepsia symptom. The severity of mucosa inflammation was consistent with H. pylori colonization among three age groups, and presents a distal-to-proximal gastric direction similar as H. pylori infection with increasing age.
The pyloric metaplasia in corpus was significantly upgraded in elderly population compared with young group and middle-aged group, which revealed that pyloric metaplasia tends to proximal stomach with increasing age. This age-related tendency of pyloric gland running to proximal stomach has also been reported by Van Zanten et al. [15, 17].
We further compared the correlation of the colonization of H. pylori, mucosal inflammation and distribution of pyloric gland in different stomach sites among three age groups. A statistically significant positive correlation was obtained. The data revealed that pyloric metaplasia in corpus was correlated with the aggravated H. pylori colonization and associated inflammation in elderly population.
As described in the introduction, pyloric gland and fundus gland in stomach present different cell types, the different pathophysiologic characters on pH levels [17], mucin glycoforms [18], binding manner of H. pylori [19]. H. pylori have been shown prefer to colonize first and initiate in the lower part of stomach (pyloric gland). Therefore, the running tendency of antral-corpus transitional zones with age might contribute to the high morbidity of H. pylori in proximal stomach of elderly population.
Moreover, H. pylori infection could aggravate mucosa atrophy. The parietal cells and chief cells of fundic glands can be partially insteaded by mucus cells of pylori glands after the H. pylori infection [2, 15, 29, 30], which might accelerate transitional zones moving to proximal of stomach. Besides, antrum-corpus transitional zones were known as a sanctuary site in eradication failure [31].
Conclusions
Based on the findings in the present study, it is concluded that both H. pylori distribution and mucosal inflammation present a tendency running to the proximal of stomach with increasing age, which correlated with pyloric metaplasia. We speculated this might make a reasonable explanation for the higher morbidity of H. pylori associated diseases in proximal stomach of elderly population.
The limitation of this study is that there is the potential bias due to time-cohort effect with different environmental factors exposed among different age groups, but the positive association among H. pylori colonization and pyloric metaplasia is demonstrated within each age group. Further clinical trials evaluating the effect of eradication of H. pylori infection on the pyloric metaplasia process are now needed to further understand.
Acknowledgements
The authors wish to acknowledge all participants in this study and everybody involved in the set-up and implementation of the study.
Funding
This study was supported by the National Natural Science Foundation of China (Nos. 81770539, 81572428 and 81272656). The funding body had no part in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The raw data generated and analyzed in the current study are not publicly available due to appropriate protection of patient personal information but are available from the corresponding author on reasonable request.
Abbreviations
- CLE
Confocal laser endomicroscopy
- IA
Incisura angularis
- URUT
Ultra-rapid urease test
Authors’ contributions
RL and HYS designed/performed most of the investigation, data analysis and wrote the manuscript; HHX provided endoscopy procedure assistance; WQ contributed to interpretation of the data and analyses. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the ethics committee of Tongji Medical College, Huazhong University of Science and Technology, and performed in accordance with the Declaration of Helsinki. All patients provided written informed consent before enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Huiying Shi, Email: shihuiying23@hotmail.com.
Hanhua Xiong, Email: hanhuaxiong@163.com.
Wei Qian, Email: qianwei63@126.com.
Rong Lin, Phone: 86-27-85726057, Email: selinalin35@hotmail.com.
References
- 1.Warren JR, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet. 1983;1(8336):1273–1275. [PubMed] [Google Scholar]
- 2.Kodama M, Murakami K, Okimoto T, Sato R, Uchida M, Abe T, Shiota S, Nakagawa Y, Mizukami K, Fujioka T. Ten-year prospective follow-up of histological changes at five points on the gastric mucosa as recommended by the updated Sydney system after helicobacter pylori eradication. J Gastroenterol. 2012;47(4):394–403. doi: 10.1007/s00535-011-0504-9. [DOI] [PubMed] [Google Scholar]
- 3.Tomtitchong P, Siribumrungwong B, Vilaichone RK, Kasetsuwan P, Matsukura N, Chaiyakunapruk N. Systematic review and meta-analysis: helicobacter pylori eradication therapy after simple closure of perforated duodenal ulcer. Helicobacter. 2012;17(2):148–152. doi: 10.1111/j.1523-5378.2011.00928.x. [DOI] [PubMed] [Google Scholar]
- 4.Fock KM. Functional dyspepsia, H. pylori and post infectious FD. J Gastroenterol Hepatol. 2011;26(Suppl 3):39–41. doi: 10.1111/j.1440-1746.2011.06649.x. [DOI] [PubMed] [Google Scholar]
- 5.Schottker B, Adamu MA, Weck MN, Brenner H. Helicobacter pylori infection is strongly associated with gastric and duodenal ulcers in a large prospective study. Clin Gastroenterol Hepatol. 2012;10(5):487–493. doi: 10.1016/j.cgh.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 6.Sugano K. Should we still subcategorize helicobacter pylori-associated dyspepsia as functional disease? J Neurogastroenterol Motil. 2011;17(4):366–371. doi: 10.5056/jnm.2011.17.4.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwak HW, Choi IJ, Cho SJ, Lee JY, Kim CG, Kook MC, Ryu KW, Kim YW. Characteristics of gastric cancer according to helicobacter pylori infection status. J Gastroenterol Hepatol. 2014;29(9):1671–1677. doi: 10.1111/jgh.12605. [DOI] [PubMed] [Google Scholar]
- 8.Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology. 2015;148(4):719–731. doi: 10.1053/j.gastro.2015.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huerta-Franco MR, Banderas JW, Allsworth JE. Ethnic/racial differences in gastrointestinal symptoms and diagnosis associated with the risk of helicobacter pylori infection in the US. Clin Exp Gastroenterol. 2018;11:39–49. doi: 10.2147/CEG.S144967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Murakami TT, Scranton RA, Brown HE, Harris RB, Chen Z, Musuku S, Oren E. Management of Helicobacter Pylori in the United States: results from a national survey of gastroenterology physicians. Prev Med. 2017;100:216–222. doi: 10.1016/j.ypmed.2017.04.021. [DOI] [PubMed] [Google Scholar]
- 11.Coban S, Soykan I, Toruner M, Akbulut H, Atli T, Ensari A. The effect of age and helicobacter pylori infection on gastric epithelial cell kinetics. Clin Res Hepatol Gastroenterol. 2011;35(10):661–665. doi: 10.1016/j.clinre.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 12.Seoane A, Bessa X, Balleste B, O'Callaghan E, Panades A, Alameda F, Navarro S, Gallen M, Andreu M, Bory F. Helicobacter pylori and gastric cancer: relationship with histological subtype and tumor location. Gastroenterol Hepatol. 2005;28(2):60–64. doi: 10.1157/13070701. [DOI] [PubMed] [Google Scholar]
- 13.Sonnenberg A, Genta RM. Changes in the gastric mucosa with aging. Clin Gastroenterol Hepatol. 2015;13(13):2276–2281. doi: 10.1016/j.cgh.2015.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Graham DY, Malaty HM, Evans DG, Evans DJ, Jr, Klein PD, Adam E. Epidemiology of helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology. 1991;100(6):1495–1501. doi: 10.1016/0016-5085(91)90644-Z. [DOI] [PubMed] [Google Scholar]
- 15.Greenwald DA. Aging, the gastrointestinal tract, and risk of acid-related disease. Am J Med. 2004;117(Suppl 5A):8S–13S. doi: 10.1016/j.amjmed.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 16.Carroll IM, Ahmed N, Beesley SM, Khan AA, Ghousunnissa S, Morain CA, Habibullah CM, Smyth CJ. Microevolution between paired antral and paired antrum and corpus helicobacter pylori isolates recovered from individual patients. J Med Microbiol. 2004;53(Pt 7):669–677. doi: 10.1099/jmm.0.05440-0. [DOI] [PubMed] [Google Scholar]
- 17.Van Zanten SJ, Dixon MF, Lee A. The gastric transitional zones: neglected links between gastroduodenal pathology and helicobacter ecology. Gastroenterology. 1999;116(5):1217–1229. doi: 10.1016/S0016-5085(99)70025-9. [DOI] [PubMed] [Google Scholar]
- 18.Radziejewska I, Borzym-Kluczyk M, Namiot Z, Stefanska E. Glycosylation of mucins present in gastric juice: the effect of helicobacter pylori eradication treatment. Clin Exp Med. 2011;11(2):81–88. doi: 10.1007/s10238-010-0113-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reeves EP, Ali T, Leonard P, Hearty S, O'Kennedy R, May FE, Westley BR, Josenhans C, Rust M, Suerbaum S, et al. Helicobacter pylori lipopolysaccharide interacts with TFF1 in a pH-dependent manner. Gastroenterology. 2008;135(6):2043–2054. doi: 10.1053/j.gastro.2008.08.049. [DOI] [PubMed] [Google Scholar]
- 20.Karasawa F, Shiota A, Goso Y, Kobayashi M, Sato Y, Masumoto J, Fujiwara M, Yokosawa S, Muraki T, Miyagawa S, et al. Essential role of gastric gland mucin in preventing gastric cancer in mice. J Clin Invest. 2012;122(3):923–934. doi: 10.1172/JCI59087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kubota S, Yamauchi K, Sugano M, Kawasaki K, Sugiyama A, Matsuzawa K, Akamatsu T, Ohmoto Y, Ota H. Pathophysiological investigation of the gastric surface mucous gel layer of patients with helicobacter pylori infection by using immunoassays for trefoil factor family 2 and gastric gland mucous cell-type mucin in gastric juice. Dig Dis Sci. 2011;56(12):3498–3506. doi: 10.1007/s10620-011-1724-9. [DOI] [PubMed] [Google Scholar]
- 22.Wen R, Gao F, Zhou CJ, Jia YB. Polymorphisms in mucin genes in the development of gastric cancer. World J Gastrointest Oncol. 2015;7(11):328–337. doi: 10.4251/wjgo.v7.i11.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ji R, Li YQ, Gu XM, Yu T, Zuo XL, Zhou CJ. Confocal laser endomicroscopy for diagnosis of Helicobacter pylori infection: a prospective study. J Gastroenterol Hepatol. 2010;25(4):700–705. doi: 10.1111/j.1440-1746.2009.06197.x. [DOI] [PubMed] [Google Scholar]
- 24.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney system. International workshop on the histopathology of gastritis, Houston 1994. Am J Surg Pathol. 1996;20(10):1161–1181. doi: 10.1097/00000478-199610000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Pilotto A, Franceschi M, Leandro G, Paris F, Niro V, Longo MG, D'Ambrosio LP, Andriulli A, Di Mario F. The risk of upper gastrointestinal bleeding in elderly users of aspirin and other non-steroidal anti-inflammatory drugs: the role of gastroprotective drugs. Aging Clin Exp Res. 2003;15(6):494–499. doi: 10.1007/BF03327372. [DOI] [PubMed] [Google Scholar]
- 26.Misra SP, Misra V, Dwivedi M, Singh PA, Bhargava V, Jaiswal PK. Evaluation of the one-minute ultra-rapid urease test for diagnosing helicobacter pylori. Postgrad Med J. 1999;75(881):154–156. doi: 10.1136/pgmj.75.881.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dursun M, Yilmaz S, Yukselen V, Kilinc N, Canoruc F, Tuzcu A. Evaluation of optimal gastric mucosal biopsy site and number for identification of helicobacter pylori, gastric atrophy and intestinal metaplasia. Hepato-Gastroenterology. 2004;51(60):1732–1735. [PubMed] [Google Scholar]
- 28.Jones N, Chiba N, Fallone C, Thompson A, Hunt R, Jacobson K, Goodman K, et al. Helicobacter pylori in first nations and recent immigrant populations in Canada. Can J Gastroenterol. 2012;26(2):97–103. doi: 10.1155/2012/174529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Syder AJ, Oh JD, Guruge JL, O'Donnell D, Karlsson M, Mills JC, Bjorkholm BM, Gordon JI. The impact of parietal cells on Helicobacter pylori tropism and host pathology: an analysis using gnotobiotic normal and transgenic mice. Proc Natl Acad Sci U S A. 2003;100(6):3467–3472. doi: 10.1073/pnas.0230380100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mueller A, Merrell DS, Grimm J, Falkow S. Profiling of microdissected gastric epithelial cells reveals a cell type-specific response to Helicobacter pylori infection. Gastroenterology. 2004;127(5):1446–1462. doi: 10.1053/j.gastro.2004.08.054. [DOI] [PubMed] [Google Scholar]
- 31.van Zanten SJ, Kolesnikow T, Leung V, O'Rourke JL, Lee A. Gastric transitional zones, areas where Helicobacter treatment fails: results of a treatment trial using the Sydney strain mouse model. Antimicrob Agents Chemother. 2003;47(7):2249–2255. doi: 10.1128/AAC.47.7.2249-2255.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data generated and analyzed in the current study are not publicly available due to appropriate protection of patient personal information but are available from the corresponding author on reasonable request.