Abstract
BACKGROUND AND OBJECTIVES:
Early term infants (37–<39 weeks’ gestation) are at higher risk of adverse outcomes than term infants (39–<41 weeks’ gestation). We hypothesized that a policy to eliminate elective, early term deliveries would result in fewer NICU admissions and shorter lengths of stay among infants born ≥37 weeks.
METHODS:
This was a retrospective cohort study of singleton infants born ≥37 weeks at a tertiary medical center from 2004 to 2015 (preperiod: 2004–2008; postperiod: 2010–2015; washout period: 2009). We compared the incidence of early term delivery, NICU admissions (short: ≥4–<24 hours, long: ≥24 hours), NICU diagnoses, and stillbirths in both periods. We used modified Poisson regression to calculate adjusted risk ratios.
RESULTS:
There were 20 708 and 24 897 singleton infants born ≥37 weeks in the pre- and postperiod, respectively. The proportion of early term infants decreased from 32.5% to 25.7% (P < .0001). NICU admissions decreased nonsignificantly (9.2% to 8.8%; P = .22), with a significant reduction in short NICU stays (5.4% to 4.6%; adjusted risk ratio: 0.85 [95% confidence interval: 0.79–0.93]). Long NICU stays increased slightly (3.8% to 4.2%), a result that was nullified by adjusting for neonatal hypoglycemia. A nonsignificant increase in the incidence of stillbirths ≥37 to <40 weeks was present in the postperiod (7.5 to 10 per 10 000 births; P = .46).
CONCLUSIONS:
Reducing early term deliveries was associated with fewer short NICU stays, suggesting that efforts to discourage early term deliveries in uncomplicated pregnancies may minimize mother-infant separation in the newborn period.
Infants born after 37 completed weeks’ gestation have traditionally been classified as “full term.” However, because health outcomes vary widely according to week of gestation within this heterogeneous group, the American College of Obstetricians and Gynecologists subdivided these infants into early term (37–<39 weeks), term (39–<41 weeks), late term (41–<42 weeks), and postterm (≥42 weeks).1 Morbidities, such as respiratory distress syndrome (RDS), transient tachypnea of the newborn (TTN), and hypoglycemia, are more common among early term infants and decrease in incidence with increasing gestational age.1–5 Furthermore, early term infants are more likely to require admission to NICUs.5
An elective early term delivery is a nonspontaneous delivery before 39 weeks’ gestation without a medical indication.5 The increased risk of adverse outcomes in early term infants motivated public health efforts to reduce early elective deliveries.5–7 In 2009, our tertiary medical center adopted American College of Obstetricians and Gynecologists guidelines to discourage early elective deliveries of singleton pregnancies. A cesarean delivery or an induction of labor before 39 weeks’ gestation requires a medical indication as specified by the Joint Commission. These indications include, but are not limited to, conditions such as placental previa, previous classic cesarean delivery, fetal growth restriction, oligohydramnios, or other comorbidities, such as hypertension and diabetes.8 If the provider’s indication is not on the list, it must be approved by the medical director of labor and delivery or the designee.8 Although other researchers have reported associations between early term delivery and an increased risk of NICU admission9 as well as quality improvement efforts to reduce early elective deliveries,10 these reports lacked detail on NICU lengths of stay and associated diagnoses.
We hypothesized that a reduction in the proportion of singleton infants born early term would result in a lower incidence of NICU admissions among infants born at ≥37 weeks’ gestation and shorter NICU lengths of stay among admitted infants born at ≥37 weeks. Our objectives for this study were to confirm a lower incidence of early term deliveries and compare the incidence of NICU admissions and lengths of stay before and after the policy change in 2009. We also compared the incidence of common NICU diagnoses and the incidence of stillbirths in the 2 time periods.
Methods
Participants and Study Design
On approval from the institutional review board, we performed a retrospective cohort study of singleton infants born at ≥37 completed weeks’ gestation at our institution from January 1, 2004, to December 31, 2015. We excluded infants who were transferred to other hospitals because we did not have length of stay data available. We also excluded infants who were transferred into our NICU from other hospitals because they would not have been the targets of our institution’s obstetric policy. During the study period, 253 infants born at ≥37 weeks’ gestation were transferred to the local quaternary children’s hospital; the majority were transferred for surgical management of prenatal congenital heart disease or other anomalies. These infants were not the targets of the policy to reduce elective early term deliveries. We split our study period into 2 time periods using the year of the formally implemented policy change (2009) as a washout period to allow for the implementation of a new obstetric practice to eliminate early elective deliveries. Our institution adopted a hard-stop policy that required health professionals to refuse early elective inductions and primary and repeat cesarean deliveries before 39 weeks without an approved medical indication. We compared the 2010–2015 postimplementation period (“postperiod”) with the 2004–2008 preimplementation period (“preperiod”), which was chosen because of electronic data availability, thereby designating the time period as the exposure. Early term delivery was the primary outcome, and NICU admission was the secondary outcome. NICU admissions were defined as stays of ≥4 hours. Our institute admits infants who are asymptomatic to the NICU for <4 hours to evaluate for sepsis because of maternal fever during labor. We examined length of stay as a continuous variable and as a dichotomized variable, defining each NICU stay as short (≥4–<24 hours) or long (≥24 hours).
Data Collection and Analysis
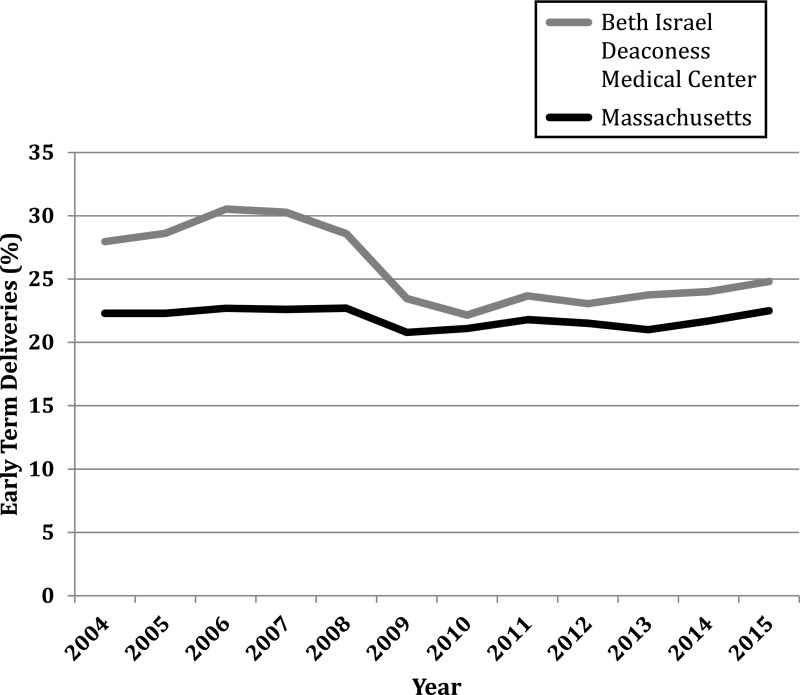
From the electronic medical record, we obtained birth year, gestational age at delivery, data on NICU use, and maternal characteristics, including age, race and/or ethnicity, insurance, gravidity, parity, mode of delivery, hypertension, and diabetes in pregnancy. Gestational age was based on the best obstetric estimate by using last menstrual period and ultrasound data and was recorded in completed weeks throughout our study. We obtained data from the Department of Public Health to compare gestational age distributions between our institution and the state of Massachusetts (Fig 1).11 To obtain NICU diagnoses, we used International Classification of Diseases, Ninth Revision codes for hypoglycemia, RDS, and TTN, but infants were only assigned diagnoses of RDS or TTN if they also required respiratory support as noted on electronic nursing flow sheets. We used flow sheet documentation of feeding tube use for feeding immaturity, of phototherapy use for hyperbilirubinemia, and of incubator use for thermoregulatory immaturity. We collected stillbirth data by reviewing all medical records with an International Classification of Diseases, Ninth Revision code for intrauterine fetal demise and confirmed the gestational age at the time of fetal death. We performed a post hoc power analysis to determine if we had sufficient power to detect differences in stillbirths because they have a low incidence.
FIGURE 1.
Early term (37–<39 weeks’ gestation) deliveries from 2004 to 2015 at Beth Israel Deaconess Medical Center and in Massachusetts overall.11
Data are presented as mean ± SD, median (interquartile range), or proportion. We compared data in the pre- and postperiod using a χ2 test for categorical variables and a t test or Wilcoxon rank sum test on the basis of data distribution for continuous variables. We used modified Poisson regression to calculate risk ratios (RRs) and 95% confidence intervals (CIs), adjusting for potential confounding variables, including maternal age, race and/or ethnicity, insurance, parity, mode of delivery, hypertension, and diabetes in pregnancy.12 We did not have access to maternal BMI or income data and relied on administrative data for maternal characteristics. We also evaluated whether differences in the incidence of common NICU diagnoses affected the RRs. When modeling the risk of a short NICU stay, we excluded infants who had a long NICU stay. When modeling the risk of a long NICU stay, we excluded infants who had a short NICU stay. NICU admissions of ≥4 hours (both short and long stay) were compared with no NICU admission. All analyses were completed by using SAS version 9.4 (SAS Institute, Inc, Cary, NC). All tests were 2 sided, and P values of <.05 were considered statistically significant.
Results
There were 49 625 singleton infants born at ≥37 weeks’ gestation in the study period (20 708 infants in the preperiod, 4020 infants in the 2009 washout period, and 24 897 infants in the postperiod). We observed changes in maternal demographics over time (Table 1). In the postperiod, there was a higher proportion of women 25 to <35 years of age, a lower proportion of white women (with a higher proportion of Asian American and women of other races and/or ethnicities), and a higher proportion of women insured by Medicaid. Women were more likely to be multiparous and have diabetes and hypertension in the postperiod.
TABLE 1.
Characteristics of Singleton Births at ≥37 Weeks’ Gestation
| 2004–2008 (n = 20 708), %a | 2010–2015 (n = 24 897), %a | P | |
|---|---|---|---|
| Maternal age, y | <.0001 | ||
| <25 | 8.5 | 6.8 | — |
| 25–<35 | 55.5 | 58.4 | — |
| ≥35 | 36.0 | 34.7 | — |
| Race and/or ethnicity | <.0001 | ||
| White | 59.9 | 46.8 | — |
| African American | 10.5 | 10.4 | — |
| Hispanic | 5.4 | 5.3 | — |
| Asian American | 13.3 | 15.6 | — |
| Other or unknown | 10.9 | 22.0 | — |
| Insuranceb | <.0001 | ||
| Private | 81.8 | 80.8 | — |
| Medicaid | 13.5 | 16.1 | — |
| Other | 4.7 | 3.1 | — |
| Parity >0 | 52.9 | 51.1 | .0002 |
| Vaginal delivery | 65.1 | 70.8 | <.0001 |
| Diabetesc | 3.9 | 5.3 | <.0001 |
| Hypertensionc | 9.5 | 10.4 | .002 |
| Male infant | 50.4 | 51.0 | .18 |
—, not applicable.
Percentages do not always add to 100 because of rounding.
Missing: n = 9.
Combination of gestational and prepregnancy or chronic.
Gestational Age
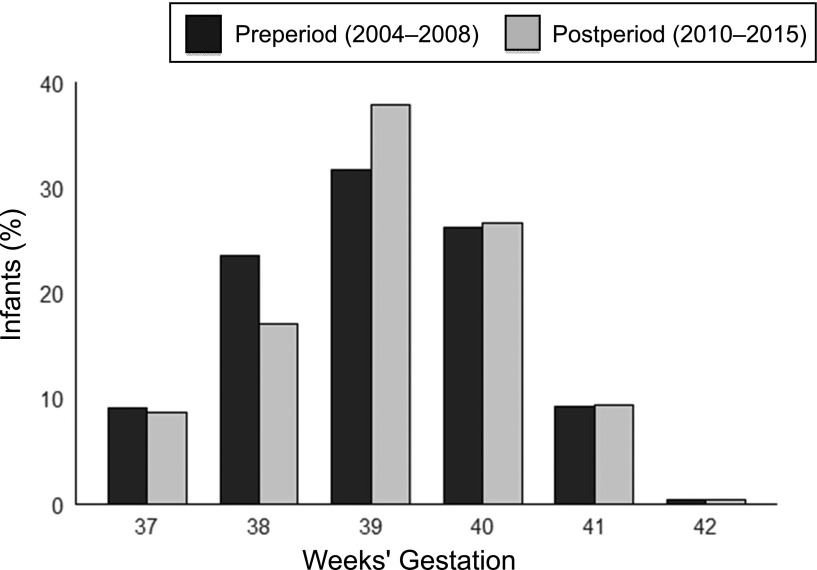
Among singleton infants born at ≥37 weeks’ gestation, the proportion of early term infants decreased from 32.5% in the preperiod to 25.7% in the postperiod (Table 2), yielding an adjusted RR of early term delivery in the post- versus preperiod of 0.79 (95% CI: 0.76–0.82; Table 3). The reduction in early term deliveries and the consequent increase in term deliveries was largely attributable to the reduction in the proportion of infants born at 38 completed weeks (from 23.5% to 17.1%) and the corresponding increased proportion of infants born at 39 completed weeks’ gestation (from 31.8% to 38.0%; Fig 2).
TABLE 2.
Outcomes of Singleton Infants Born at ≥37 Weeks’ Gestation
| 2004–2008 (n = 20 708), % | 2010–2015 (n = 24 897), % | P | |
|---|---|---|---|
| Gestational category, completed wk | <.0001 | ||
| 37–<39 | 32.5 | 25.7 | |
| 39–<41 | 57.9 | 64.6 | |
| ≥41 | 9.6 | 9.7 | |
| NICU admissiona | — | ||
| No admission or <4 h | 90.8 | 91.2 | — |
| ≥4 h | 9.2 | 8.8 | .22a |
| Short stays (4–<24 h) | 5.4 | 4.6 | .0001a |
| Long stays (≥24 h) | 3.8 | 4.2 | .01a |
| NICU diagnoses | — | ||
| Hypoglycemia | 1.4 | 3.0 | <.0001 |
| Hyperbilirubinemia requiring phototherapy | 0.7 | 1.1 | <.0001 |
| Feeding immaturity requiring nasogastric feeds | 0.4 | 0.4 | .57 |
| RDS | 0.3 | 0.3 | .88 |
| TTN | 1.6 | 1.8 | .25 |
| Thermoregulatory immaturity requiring incubator | 0.7 | 0.7 | .45 |
—, not applicable.
NICU admission, short NICU stays, and long NICU stays are each compared with no NICU admission or NICU stays of <4 h.
TABLE 3.
Risk of Early Term Delivery and NICU Admission in the Postperiod (2010–2015) Versus the Preperiod (2004–2008) After a Hospital Policy to Eliminate Early Elective Deliveries Before 39 Weeks’ Gestation
| Outcome | Model 0, RR (95% CI) | Model 1, RR (95% CI) | Model 2, RR (95% CI) | Model 3, RR (95% CI) |
|---|---|---|---|---|
| Early term delivery | 0.79 (0.77–0.81) | 0.79 (0.76–0.82) | — | — |
| NICU admissiona | ||||
| ≥4 h | 0.96 (0.91–1.02) | 0.97 (0.92–1.03) | 0.91 (0.86–0.97) | 0.89 (0.84–0.95) |
| Short stays (≥4–<24 h) | 0.85 (0.79–0.92) | 0.85 (0.79–0.93) | 0.83 (0.77–0.91) | 0.81 (0.75–0.88) |
| Long stays (≥24 h) | 1.12 (1.02–1.23) | 1.15 (1.05–1.26) | 1.00 (0.92–1.10) | 0.98 (0.89–1.08) |
Model 0 was unadjusted; model 1 was adjusted for maternal age, race and/or ethnicity, insurance status, parity, mode of delivery, diabetes, and hypertension; model 2 was model 1 with an additional adjustment for neonatal hypoglycemia; and model 3 was model 2 with an additional adjustment for neonatal hyperbilirubinemia. —, not applicable.
NICU admission, short NICU stays, and long NICU stays are each compared with no NICU admission or NICU stays of <4 h.
FIGURE 2.
Gestational age distribution among singleton infants born at ≥37 weeks’ gestation.
NICU Admissions and Diagnoses
During the study period, 9.1% of infants born at ≥37 weeks’ gestation were admitted to the NICU. NICU admissions were more common among early term (11.5%) and late- and postterm (9.6%) infants compared with term infants (7.9%; P < .0001). Rates of NICU admissions did not differ significantly among early term infants in the pre- and postperiod (11.7% and 11.0%, respectively; P = .24). Overall, the proportion of infants born at ≥37 weeks admitted to the NICU decreased from 9.2% to 8.8% in the postperiod, although this difference was not statistically significant (P = .22). The median NICU length of stay increased from 20 to 39 hours in the postperiod (P < .0001). The incidence of short NICU stays decreased from 5.4% to 4.6% in the postperiod (adjusted RR: 0.81; 95% CI: 0.75–0.88; Table 3). Conversely, the incidence of long NICU admissions increased from 3.8% to 4.2% in the postperiod (adjusted RR: 1.15; 95% CI: 1.05–1.26). Among infants admitted to the NICU, the most common diagnoses associated with short NICU stays were TTN (34.7%) and hypoglycemia (27.4%). Similarly, for conditions requiring respiratory support (TTN or RDS), the most common diagnoses we ascertained among infants with long NICU stays (33.0%). Hypoglycemia was present among 21.0% of these infants. Among all infants, the NICU diagnoses we analyzed were stable between the 2 time periods (Table 2). However, in the postperiod, there was a significant increase in the proportion of infants born at ≥37 weeks’ gestation in the NICU who were diagnosed with hypoglycemia and hyperbilirubinemia. A post hoc adjustment for neonatal hypoglycemia nullified the association between the time period and long NICU admissions (adjusted RR: 1.00; 95% CI: 0.92–1.10; Table 3).
Stillbirths
During the study period, 35 of the 49 660 singleton pregnancies (7.0 per 10 000 deliveries) that reached 37 weeks’ gestation ended in stillbirth. In the preperiod, the incidence of stillbirth was slightly lower, at 11 of 20 719 pregnancies (5.3 per 10 000 deliveries), than the incidence of stillbirth in the postperiod, at 22 of 24 919 pregnancies (8.8 per 10 000 deliveries), but this difference did not reach statistical significance (P = .16). Post hoc power analyses revealed that we had 23% power to detect differences in stillbirths at ≥37 weeks’ gestation. To achieve 80% power to detect differences in stillbirth incidences observed, we would have required a sample size of 189 160.
Discussion
In this study of 49 625 singleton live-born infants at ≥37 weeks’ gestation, we observed a significant reduction in early term deliveries and short NICU stays (<24 hours) after an intervention to eliminate early elective deliveries. We observed the largest decrease in the proportion of early term infants from 2008 (28.6%) to 2009 (23.5%), the year the policy was implemented. This reduction was more pronounced than in the state of Massachusetts overall (from 22.7% in 2008 to 20.8% in 2009; Fig 1). There was an increase in longer NICU stays (≥24 hours) in the postperiod, which was nullified once analyses were adjusted for hypoglycemia. These findings suggest that obstetric guidelines or policies can successfully reduce the proportion of early term deliveries and may decrease NICU use, particularly in short NICU stays. Because we did not observe a reduction in long NICU stays, our data do not suggest that reducing early elective deliveries will prevent major morbidities. However, substantial and significant reductions in short NICU stays can minimize mother-infant separation in the first 24 hours, thereby improving other important outcomes, such as breastfeeding success and bonding.13 Early breastfeeding (in the first 2 hours after birth) can improve rates of breastfeeding success. Additionally, reducing short NICU stays may reduce health care costs.6
Our findings are consistent with others from analyses of population-based samples.9,10 Over a 2-month study period across 27 hospitals, Clark et al9 found that 31% of 17 794 deliveries were elective at a gestation of ≥37 completed weeks and that early term infants were more likely to require NICU admission than infants born at ≥39 weeks’ gestation. In Utah, across an integrated system of 9 delivery centers, Oshiro et al10 prospectively collected data and demonstrated the success of a quality improvement program in reducing elective early term, singleton deliveries from 27.8% to 4.8% (P < .001) over 1 year. In contrast, we did not specifically measure elective deliveries, and therefore, secular trends of valid medical indications for delivery may have influenced our findings. Ehrenthal et al3 compared gestational age distributions and NICU admissions of >24 000 births before and after a policy to eliminate early elective deliveries among singleton infants. They found a significant reduction in early term deliveries and NICU admissions but a significant increase in stillbirths at 37 and 38 weeks from 2.5 to 9.1 per 10 000 term pregnancies (RR: 3.67; 95% CI: 1.02–13.15).3 Our study differed from theirs in a few important ways. We analyzed common NICU diagnoses and found increases in hypoglycemia and hyperbilirubinemia. It is possible that Ehrenthal et al3 would have found an even more significant reduction in NICU stays had secular trends of other common diagnoses been considered. Furthermore, they did not differentiate short from long NICU stays.
We observed a smaller increase in stillbirth incidence than Ehrenthal et al,3 and thus we were underpowered to detect a significant difference, although our study was almost twice the sample size. Although our finding of an increase in stillbirth incidence may not be statistically significant, we are conscious of its clinical significance. After interventions to reduce early elective deliveries, increases in stillbirths have also been noted in other studies.10,14 Decisions to prolong pregnancy requires careful balancing of the benefits of further fetal maturation associated with lower risks of neonatal morbidity with the ongoing risk of intrauterine fetal demise during pregnancy.15 Careful monitoring of stillbirth rates with shifting distributions in gestational age remains warranted.
Our study has several strengths. Our large sample size allowed for us to examine both short and long NICU stays. We were also able to adjust for multiple potential confounders. We used a combination of clinical variables from the electronic medical record to verify administrative data. However, our study should be considered within the context of its limitations and secular trends. There were several important changes in the incidence of NICU diagnoses between the 2 time periods. The increase in the proportion of hypoglycemia diagnoses may have occurred because of a true increase in incidence or a change in individual clinicians’ thresholds for normal glucose levels, as noted in relevant literature.16,17 Our institution followed the same internal definition of hypoglycemia (glucose levels of <40 mg/dL) throughout the study period. Nonetheless, awareness of the importance of euglycemia in the newborn period increased over the length of our study period and could have influenced providers’ thresholds for admission and intravenous (IV) dextrose administration in the postperiod.18 Infants with hypoglycemia who are treated with IV dextrose also require a period off of IV fluids with stable glucose concentrations, and they also generally require NICU stays longer than 24 hours. In addition, the increase in the prevalence of diabetes observed in our data is consistent with international trends19–23 and likely is due to a change in the threshold for diagnosis and increases in maternal age24 and obesity.23,25,26 Infants born to mothers with diabetes are routinely screened for asymptomatic hypoglycemia18; therefore, some infants with hypoglycemia in the preperiod might have gone without a diagnosis if their mothers were not categorized as having diabetes when they would have been in the postperiod. When we adjusted the models for hypoglycemia, the increase in long NICU stays in the postperiod disappeared.
Another secular trend that may have contributed to the increase in long NICU stays in the postperiod was the increase in diagnoses of hyperbilirubinemia requiring phototherapy. An infant with a bilirubin concentration of >20 mg/dL is often admitted to the NICU to optimize phototherapy and hydration to avoid exchange transfusion. There was an increase in the proportion of infants born to women with diabetes and to Asian American women, who are at risk for hyperbilirubinemia.27,28 When we added hyperbilirubinemia to models with hypoglycemia included, no additional change to the effect estimate was observed, suggesting that the true driver of the increase in long NICU stays was hypoglycemia as opposed to hyperbilirubinemia (Table 3).
We observed significant differences in maternal characteristics between the two time periods. Women were more likely to deliver vaginally in the postperiod, which may be correlated to simultaneous efforts to lower the cesarean delivery rate during this same time period. Historically, many early elective deliveries occurred in the setting of planned repeat cesarean deliveries after a woman had had a cesarean delivery in a previous pregnancy. Repeat cesarean deliveries have become more common as vaginal births after cesarean deliveries have declined in the last 20 years.1 A cesarean delivery, especially preceding labor, results in an increased risk of infant morbidities, such as respiratory distress, that in turn increase the likelihood of NICU admission.1,2,4,6
With respect to race and/or ethnicity, there was an increase in the proportion of women in the “other race and/or ethnicity” category in the postperiod. Other than this category of infants, which was slightly less likely to be admitted to the NICU, race and/or ethnicity was not a significant predictor of NICU admission. Including these characteristics in our regression model did not appreciably alter the results (Table 3). However, we cannot rule out residual confounding. There were no formal changes to NICU policies that would affect infants born at ≥37 weeks’ gestation, with the exception of the initiation of therapeutic hypothermia for hypoxic-ischemic encephalopathy. A sensitivity analysis excluding these 20 infants did not affect our results.
We did not have access to maternal BMI; however, we were able to adjust for factors related to BMI, such as maternal diabetes and hypertension. We did not have income information, but other demographic factors allowed for us to adjust for socioeconomic factors. We used billing codes to obtain maternal diagnoses and some NICU diagnoses as well as data from electronic nursing flow sheets, such as the use of nasogastric tubes, IV fluids, and phototherapy, to confirm our diagnoses. Nonetheless, we likely underestimated the incidence of these diagnoses given that billing data can induce misclassification and rely on providers’ documentations. We would not expect that billing errors would have differed between the 2 periods; thus, we would not expect them to affect our findings.
Conclusions
We found that an obstetric policy to reduce early elective deliveries was associated with fewer early term deliveries and fewer short NICU stays. These findings suggest that ongoing institutional and public health efforts to discourage early term deliveries in uncomplicated pregnancies may minimize mother-infant separation in the newborn period. However, population-level monitoring of stillbirth rates is warranted.
Footnotes
Ms Kennedy conceptualized the study under the mentorship of Dr Burris and drafted the initial manuscript; Dr Hacker supervised the analysis and critically edited the final manuscript; Mr Miedema designed the data collection instruments and critically reviewed the manuscript; Dr Pursley oversaw data collection and critically edited the manuscript; Dr Modest assisted with data analysis, collected stillbirth data, and critically edited the manuscript; Dr Golen assisted in study design and critically edited the manuscript; Dr Burris conceived the study, supervised the data collection, performed the analysis, supervised the writing, and critically edited the final manuscript. The work was conducted primarily when Dr Burris was at Beth Israel Deaconess Medical Center and completed when she was at Children’s Hospital of Philadelphia. All authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Burris is funded by National Institutes of Health National Institute of Environmental Health Sciences (grant K23ES02224204). This work was conducted with support from Harvard Catalyst (the Harvard Clinical and Translational Science Center), the National Center for Research Resources, National Center for Advancing Translational Sciences National Institutes of Health (award UL1 TR001102), and financial contributions from Harvard University and its affiliated academic health care centers. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Tita ATN, Landon MB, Spong CY, et al. ; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. Timing of elective repeat cesarean delivery at term and neonatal outcomes. N Engl J Med. 2009;360(2):111–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilmink FA, Hukkelhoven CW, Lunshof S, Mol BW, van der Post JA, Papatsonis DN. Neonatal outcome following elective cesarean section beyond 37 weeks of gestation: a 7-year retrospective analysis of a national registry. Am J Obstet Gynecol. 2010;202(3):250.e1–250.e8 [DOI] [PubMed] [Google Scholar]
- 3.Ehrenthal DB, Hoffman MK, Jiang X, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011;118(5):1047–1055 [DOI] [PubMed] [Google Scholar]
- 4.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW; Women and Newborn Clinical Integration Program. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113(4):804–811 [DOI] [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists Committee on Obstetric Practices Society for Maternal-Fetal Medicine. Nonmedically indicated early-term deliveries. Available at: www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Nonmedically-Indicated-Early-Term-Deliveries. Accessed March 13, 2016
- 6.National Institute for Health Care Management Foundation. Born too early: improving maternal and child health by reducing early elective deliveries. Available at: https://www.nihcm.org/topics/population-health/maternal-child-health/born-too-early-issue-brief. Accessed September 14, 2018
- 7.March of Dimes. Why at least 39 weeks is best for your baby. Available at: www.marchofdimes.org/pregnancy/why-at-least-39-weeks-is-best-for-your-baby.aspx#. Accessed March 13, 2016
- 8.The Joint Commission. Specifications manual for Joint Commission national quality measures (v2013A1): appendix A: ICD-9-CM code tables. Available at: https://manual.jointcommission.org/releases/TJC2013A/AppendixATJC.html#Table_Number_11_07_Conditions_Po. Accessed March 18, 2016
- 9.Clark SL, Miller DD, Belfort MA, Dildy GA, Frye DK, Meyers JA. Neonatal and maternal outcomes associated with elective term delivery. Am J Obstet Gynecol. 2009;200(2):156.e1–156.e4 [DOI] [PubMed] [Google Scholar]
- 10.Oshiro BT, Kowalewski L, Sappenfield W, et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation [published correction appears in Obstet Gynecol. 2013;122(1):160]. Obstet Gynecol. 2013;121(5):1025–1031 [DOI] [PubMed] [Google Scholar]
- 11. Massachusetts Department of Public Health; Registry of Vital Records and Statistics. Massachusetts births 2015. December 2016. Available at: www.mass.gov/eohhs/gov/departments/dph/programs/admin/dmoa/repi/birth-data.html. Accessed November 3, 2017.
- 12.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706 [DOI] [PubMed] [Google Scholar]
- 13.Aghdas K, Talat K, Sepideh B. Effect of immediate and continuous mother-infant skin-to-skin contact on breastfeeding self-efficacy of primiparous women: a randomised control trial. Women Birth. 2014;27(1):37–40 [DOI] [PubMed] [Google Scholar]
- 14.Clark SL, Frye DR, Meyers JA, et al. Reduction in elective delivery at <39 weeks of gestation: comparative effectiveness of 3 approaches to change and the impact on neonatal intensive care admission and stillbirth. Am J Obstet Gynecol. 2010;203(5):449.e1–449.e6 [DOI] [PubMed] [Google Scholar]
- 15.Flenady V, Wojcieszek AM, Middleton P, et al. ; Lancet Ending Preventable Stillbirths Study Group Lancet Stillbirths in High-Income Countries Investigator Group. Stillbirths: recall to action in high-income countries. Lancet. 2016;387(10019):691–702 [DOI] [PubMed] [Google Scholar]
- 16.Stanley CA, Rozance PJ, Thornton PS, et al. Re-evaluating “transitional neonatal hypoglycemia”: mechanism and implications for management. J Pediatr. 2015;166(6):1520–1525.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thornton PS, Stanley CA, De Leon DD, et al. ; Pediatric Endocrine Society. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr. 2015;167(2):238–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adamkin DH; Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127(3):575–579 [DOI] [PubMed] [Google Scholar]
- 19.Au CPY, Raynes-Greenow CH, Turner RM, Carberry AE, Jeffery HE. Antenatal management of gestational diabetes mellitus can improve neonatal outcomes. Midwifery. 2016;34:66–71 [DOI] [PubMed] [Google Scholar]
- 20.Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization guideline. Diabetes Res Clin Pract. 2014;103(3):341–363 [DOI] [PubMed] [Google Scholar]
- 21.Farrar D. Hyperglycemia in pregnancy: prevalence, impact, and management challenges. Int J Womens Health. 2016;8:519–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guariguata L, Linnenkamp U, Beagley J, Whiting DR, Cho NH. Global estimates of the prevalence of hyperglycaemia in pregnancy. Diabetes Res Clin Pract. 2014;103(2):176–185 [DOI] [PubMed] [Google Scholar]
- 23.Stuebe AM, Landon MB, Lai Y, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network, Bethesda, MD. Maternal BMI, glucose tolerance, and adverse pregnancy outcomes. Am J Obstet Gynecol. 2012;207(1):62.e1–62.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Solomon CG, Willett WC, Carey VJ, et al. A prospective study of pregravid determinants of gestational diabetes mellitus. JAMA. 1997;278(13):1078–1083 [PubMed] [Google Scholar]
- 25.Bhattacharya S, Campbell DM, Liston WA, Bhattacharya S. Effect of body mass index on pregnancy outcomes in nulliparous women delivering singleton babies. BMC Public Health. 2007;7:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiss JL, Malone FD, Emig D, et al. ; FASTER Research Consortium. Obesity, obstetric complications and cesarean delivery rate–a population-based screening study. Am J Obstet Gynecol. 2004;190(4):1091–1097 [DOI] [PubMed] [Google Scholar]
- 27.Porter ML, Dennis BL. Hyperbilirubinemia in the term newborn. Am Fam Physician. 2002;65(4):599–606 [PubMed] [Google Scholar]
- 28.Silva JK, Kaholokula JK, Ratner R, Mau M. Ethnic differences in perinatal outcome of gestational diabetes mellitus. Diabetes Care. 2006;29(9):2058–2063 [DOI] [PubMed] [Google Scholar]