Abstract
Importance:
Sports- and recreation-related traumatic brain injuries (SRR-TBIs) are a growing public health problem affecting persons of all ages in the United States.
Objective:
To describe the trends of SRR-TBIs treated in US emergency departments (EDs) from 2001 to 2012 and to identify which sports and recreational activities and demographic groups are at higher risk for these injuries.
Design:
Data on initial ED visits for an SRR-TBI from the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP) for 2001-2012 were analyzed.
Setting:
NEISS-AIP data are drawn from a nationally representative sample of hospital-based EDs.
Participants:
Cases of TBI were identified from approximately 500 000 annual initial visits for all causes and types of injuries treated in EDs captured by NEISS-AIP.
Main Outcome Measure(s):
Numbers and rates by age group, sex, and year were estimated. Aggregated numbers and percentages by discharge disposition were produced.
Results:
Approximately 3.42 million ED visits for an SRR-TBI occurred during 2001-2012. During this period, the rates of SRR-TBIs treated in US EDs significantly increased in both males and females regardless of age (all Ps < .001). For males, significant increases ranged from a low of 45.8% (ages 5-9) to a high of 139.8 % (ages 10-14), and for females, from 25.1% (ages 0-4) to 211.5% (ages 15-19) (all Ps < .001). Every year males had about twice the rates of SRR-TBIs than females. Approximately 70% of all SRR-TBIs were reported among persons aged 0 to 19 years. The largest number of SRR-TBIs among males occurred during bicycling, football, and basketball. Among females, the largest number of SRR-TBIs occurred during bicycling, playground activities, and horseback riding. Approximately 89% of males and 91% of females with an SRR-TBI were treated and released from EDs.
Conclusion and Relevance:
The rates of ED-treated SRR-TBIs increased during 2001-2012, affecting mainly persons aged 0 to 19 years and males in all age groups. Increases began to appear in 2004 for females and 2006 for males. Activities associated with the largest number of TBIs varied by sex and age. Reasons for the reported increases in ED visits are unknown but may be associated with increased awareness of TBI through increased media exposure and from campaigns, such as the Centers for Disease Control and Prevention’s Heads Up. Prevention efforts should be targeted by sports and recreational activity, age, and sex.
Keywords: emergency department, epidemiology, recreation, sports, traumatic brain injury
DURING 2001-2010, the number of sports- and recreation-related (SRR) injuries treated in emergency departments (EDs) increased approximately 5% from 3.9 million to 4.1 million.1,2 Among these SRR injuries, traumatic brain injuries (TBIs) are a major outcome. TBIs resulting from sports and recreational activities (SRAs) have become a major public health problem in the United States.3,4
Approximately 65% of all SRR-TBIs treated in EDs from 2001 to 2009 occurred among persons 19 years or younger.3,4 Most of these injuries were associated with bicycling, football, and playground activities and disproportionately affected 10- to 19-year-old males.3,4 Unlike the small increases in all SSR injuries, the number of SRR-TBIs has increased substantially (62%; from 153 375 in 2001 to 248 418 in 2009).3,4
TBI has significant medical and socioeconomic consequences. Approximately 90% of SRR-TBIs were treated and released from EDs, suggesting that these injuries were mild.4 And yet, research indicates that 15% to 25% of all persons with mild TBI may have long-term physical, cognitive, and emotional consequences.5–8 The economic impact of TBI is staggering. Estimated in 2009 US dollars, the total lifetime healthcare cost of fatal, hospitalized, and nonhospitalized TBIs was approximately $221 billion. Of this, $57.8 billion were related to hospitalization-related costs.9 TBIs can be experienced by persons of any age who participate in SRAs. Therefore, information on SRR-TBIs across the entire life span is critical for prevention planning and health promotion. To our knowledge, this is the first national study that describes the magnitude of and trends in SRR-TBIs treated in US hospital EDs among all ages. In addition, this study seeks to identify population subgroups at higher risk, SRAs that are associated with the higher number of TBIs, and the number of SRR-TBIs stratified by discharge disposition (as a proxy for TBI severity).
METHODS
The National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP), an expansion of NEISS, has been cosponsored by the Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control, and the Consumer Product Safety Commission since 2000.10 It collects data, on initial visits, for all types and external causes of nonfatal injuries and poisonings treated in US hospital EDs—even those not associated with consumer products. Detailed information on NEISS-AIP methods have been published elsewhere.1,2,4 Given that NEISS-AIP collects data on initial visits, not on unique patient data, a patient can have valid repetitive initial visits for a second or third time. To address this issue, every year, the CDC uses a computerized program to identify and delete possible (invalid) duplicates. Every year, on average, 10 records are removed. In summary, data were drawn from a nationally representative subsample of 66 of 100 NEISS hospitals selected as a stratified probability sample of hospitals in the United States and territories that have 6 or more beds and a 24-hour ED.10 Trained abstractors extract relevant information from NEISS-eligible ED records,11 including, for example, the body part injured, diagnosis, external cause, and injury intent.11 Abstractors may also record a brief narrative with additional details about the injury. NEISS-AIP has been used previously to estimate the incidence of SRR-TBIs treated in EDs.3,4
For this study, NEISS-AIP records were examined for injuries from SRAs that were treated in the ED between January 1, 2001, and December 31, 2012. An algorithm using the consumer products involved (eg, swing sets) and the narrative description of the incident obtained from the NEISS-AIP medical record were used to identify SRAs. For this study, an SRR injury was classified as a TBI if an NEISS-AIP record documented that the primary body part injured was the head and the principal head injury diagnosis was concussion or internal organ injury. All SRR-TBIs could have occurred during organized or unorganized sports, as well as all types of recreational activities.
Initially, cases were classified into 39 mutually exclusive SRAs using an algorithm developed by the CDC and the Consumer Product Safety Commission for the consumer products involved (eg, baseball equipment), a description of events leading to the injury, injury locale, and injury diagnosis obtained from the ED medical record. Fifteen of the 39 activities with the highest occurrence of TBI were retained as separate categories: all-terrain vehicle (ATV) use, baseball, basketball, bicycling, football, golf, gymnastics, ice hockey, horseback riding, playground activities, soccer, scooter use, softball, trampoline, and volleyball. Because of small sample sizes, selected activities that share certain characteristics were combined, including combative sports/wrestling; exercise/weight lifting; inline/roller skating; miscellaneous ball sports; moped/minicar/off-road vehicles/go-cart; snow sports (ie, snow skiing, ice skating, toboggan/sled/discovery, and snowmobile); swimming/water sports (ie, water skiing/surfing, personal watercraft, and fishing); and racket sports/tennis. Disparate activities with lower occurrence of TBI were categorized as “other sports.” Because this category is nonspecific and not conducive to identifying clear prevention implications, the results are presented but not discussed. In this report, we present the results of the most common single or combined SRAs with the highest occurrence of TBI by year, sex, age group, and discharge disposition. Patient discharge disposition was used as a proxy for TBI severity and was categorized as (1) treated and released (ie, mild TBI or concussion) and (2) hospitalized/transferred (ie, more severe TBI). The latter category includes hospitalizations following the ED visit and those transferred to other facilities for more specialized care. The “other” category includes observed, left against medical advice, left without being seen, and unknown discharge disposition. The severity of these “other” cases cannot be ascertained.
Cases of an SRR-TBI were excluded if the injury was violence-related (ie, self-harm, assault, or legal intervention). Also excluded were assault-related injuries that occurred during SRAs. Persons with an SRR-TBI who were dead on arrival or died in the ED were also excluded because of small sample size (N = 84).
Because the exact number of people who participate in specific SRAs in the United States is not known,3,4 US Census Bureau population estimates were used as the denominator to compute the overall population rates of SRR-TBIs per 100 000 population per year by sex and age group.3,4 Although NEISS-AIP collects data on race/ethnicity, these demographic variables were not included in this study. NEISS-AIP does not offer the option to request leading causes of injury by race/ethnicity because of the relatively high percentage of records (~17 %) with unknown race/ethnicity. Therefore, annualized national estimates presented for each race/ethnicity category will be low because they do not count cases recorded as “unknown” race/ethnicity (available at: http://aspe.hhs.gov/datacncl/datadir/cdc5.htm). Estimates with coefficients of variation more than 30%, a weighted estimate of less than 1200, or an unweighted count of less than 20 were considered unstable.5 Rates resulting from these unstable estimates were not reported; resulting numbers and percentages were reported and flagged. Analyses were conducted using SAS 9.3; 95% confidence intervals (CIs) and statistical tests took into consideration sample weights and the complex survey design.10) Significance of trends over time was assessed using weighted rate regression analyses. Joinpoint regression version 4.1.0 was fitted to estimate annual percent change (APC) in rates and to identify possible joinpoints (ie, years at which trends may change significantly).12 A maximum of 3 joinpoints were allowed for each estimate, and the APC for each segment was computed using log-linear models. In addition, 95% CIs were calculated for each APC estimate and were used to determine if the APC for each segment differed significantly from zero (see Tables 1 and 2). When multiple significant joinpoints occurred, the overall (full range) percent changes were reported as an average annual percent change (AAPC).
TABLE 1.
Estimated numbers and rates of emergency department visits per 100 000 population of sports- and recreation-related traumatic brain injury by sex and age group, NEISS-AIP, 2001-2012, United States
| 2001 |
2012 |
2001 vs 2012 rate change (%) |
Trend test p value |
|||
|---|---|---|---|---|---|---|
| n | Rate (95% CI)a | n | Rate (95% CI)a | |||
| Sex | ||||||
| Male | 144 546 | 99.9 (86.1-113.7) | 308 566 | 205.1 (181.7-228.5) | 105.3 | <.01 |
| Female | 63 257 | 45.2 (39.2-51.1) | 142 157 | 97.1 (85.6-108.7) | 114.8 | <.01 |
| Total | 207 829 | 73.1 (63.7-82.5) | 450 724 | 152.0 (135.1-169.0) | 107.9 | <.01 |
| All age groups | ||||||
| 0-4 | 14 176 | 73.5 (50.9-96.1) | 23 957 | 119.8 (84.7-154.9) | 63.0 | <.01 |
| 5-9 | 39 170 | 194.2 (141.2-247.2) | 61 011 | 298.0 (227.6-368.4) | 53.5 | <.01 |
| 10-14 | 54 143 | 258.1 (191.4-324.7) | 128 672 | 622.5 (462.5-782.5) | 141.2 | <.01 |
| 15-19 | 45 886 | 224.3 (169.1-279.5) | 115 650 | 541.4 (410.5-672.3) | 141.4 | <.01 |
| 20-24 | 12 992 | 65.8 (29.4-102.2) | 33 072 | 146.4 (99.4-193.5) | 122.5 | <.01 |
| 25-34 | 15 014 | 38.0 (24.0-52.0) | 30 729 | 72.6 (52.0-93.3) | 91.1 | <.01 |
| 35-44 | 11 734 | 26.0 (12.2-39.9) | 17 856 | 44.1 (30.8-57.4) | 69.6 | <.01 |
| ≥45 | 14 704 | 14.7 (7.4-22.0) | 39 777 | 31.6 (21.4-41.7) | 115.0 | <.01 |
| Sex and age group | ||||||
| Male | ||||||
| 0-4 | 8 467 | 85.8 (66.0-105.6) | 16 553 | 162.0 (111.9-212.2) | 88.8 | <.01 |
| 5-9 | 28 363 | 274.6 (196.9-352.3) | 41 877 | 400.4 (302.5-498.3) | 45.8 | <.05 |
| 10-14 | 38 827 | 361.3 (263.2-459.3) | 91 586 | 866.7 (637.0-1 096.0) | 139.9 | <.01 |
| 15-19 | 34 731 | 329.3 (260.6-397.9) | 79 171 | 722.2 (563.3-881.0) | 119.3 | <.01 |
| 20-24 | 9 032 | 89.6 (41.3-137.9) | 22 028 | 190.7 (129.1-252.3) | 112.8 | <.01 |
| 25-34 | 9 517 | 47.8 (28.8-66.8) | 20 558 | 96.3 (69.6-123.1) | 101.5 | <.01 |
| 35-44 | 6 980b | 11 520 | 57.1 (38.6-75.6) | c | … | |
| ≥45 | 8 621 | 18.7 (10.9-26.6) | 25 274 | 42.7 (29.2-56.2) | 128.3 | <.01 |
| Female | ||||||
| 0-4 | 5 709 | 60.5 (35.1-86.0) | 7 404 | 75.7 (54.7-96.7) | 25.1 | <.01 |
| 5-9 | 10 807 | 109.8 (94.5-125.0) | 19 134 | 191.0 (150.7-231.4) | 74.0 | <.01 |
| 10 -14 | 15 316 | 149.7 (128.1-171.3) | 37 086 | 367.1 (280.6-453.6) | 145.2 | <.01 |
| 15-19 | 11 155 | 112.6 (88.1-137.1) | 36 479 | 350.8 (252.5-449.2) | 211.5 | <.01 |
| 20-24 | 3 960 | 40.9 (18.1-63.7) | 11 044 | 100.1 (66.2-134.0) | 144.7 | <.01 |
| 25-34 | 5 498 | 28.1 (19.2-37.0) | 10 171 | 48.5 (32.2-64.9) | 72.6 | <.05 |
| 35-44 | 4 755 | 21.0 (13.8-28.2) | 63 36 | 31.1 (22.1-40.2) | 48.1 | <.01 |
| ≥45 | 6 057b | … | 14 503 | 21.7(14.1-29.3) | … | |
Abbreviations: CI, confidence interval; NEISS-AIP, National Electronic Injury Surveillance System-All Injury Program.
Total rates and rates by sex are age-adjusted rates. Rates by age group are crude rates. Rates derived from unstable estimates are not presented. Estimates are considered unstable when the number of unweighted NEISS cases is less than 20 or the national (weighted) estimate is less than 1200 or the coefficient of variation is more than 30%. 95% CI (not presented for unstable estimates).
The number was derived from an unstable estimate.
TABLE 2.
Estimated AAPC and period APC in sports- and recreation-related traumatic brain injury in emergency department visits by segment period and sex, NEISS-AIP, 2001-2012
| Full range 2001-2012 AAPC (95% CI) |
Segment 1 |
Segment 2 |
|||
|---|---|---|---|---|---|
| Period | APC (95% CI) | Period | APC (95% CI) | ||
| All | 7.8 (5.4-10.3)a | 2001-2006 | 2.8 (−1.9 to 7.6) | 2006-2012 | 12.3 (8.7-15.9)a |
| Sex | |||||
| Male | 7.5 (5.4-9.8)a | 2001-2006 | 2.8 (−1.5 to 7.2) | 2006-2012 | 11.7 (8.6-14.9)a |
| Female | 7.7 (4.2-11.3)a | 2001-2004 | −2.6 (−14.1 to 10.5) | 2004-2012 | 11.8 (8.9-14.8)a |
Abbreviations: AAPC, average annual percent change; APC, annual percent change; CI, confidence interval; NEISS-AIP, National Electronic Injury Surveillance System-All Injury Program.
Statistically significant change (P < .05).
RESULTS
Overall SRR-TBI ED visits by sex
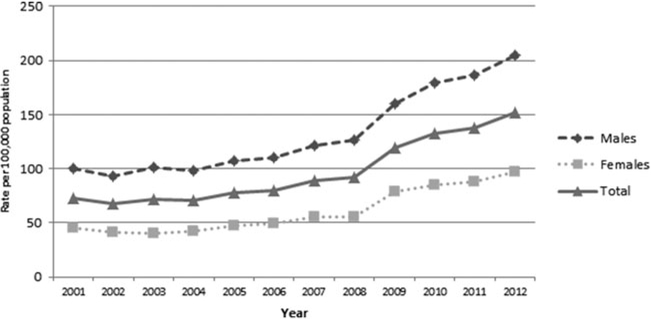
During 2001-2012, the unweighted counts for all SRR injury ED visits were 869 472, of which 71 982 (8.3%) were TBIs; weighted counts totaled 49 560 999 ED visits for all SRR injuries, of which 3 417 370 (7.0%) were TBIs (not displayed). The overall age-adjusted rate of SRR-TBI ED visits per 100 000 population significantly increased from 73.1 in 2001 to 152.0 in 2012 (P < .0001) (see Figure 1 and Table 1). The overall 2001-2012 AAPC in the age-adjusted rate of SRR-TBI ED visits was 7.8% (95% CI, 5.4-10.3; P < .0001; see Table 2). For all cases, the APC in the age-adjusted rate of SRR-TBI ED visits from 2001 to 2006 was 2.8% (95% CI, −1.9 to 7.6; P = .2) and then from 2006 to 2012, the APC significantly increased to 12.3% (95% CI, 8.7-15.9, P < .0001; see Table 2). The joinpoint for the line segments among males occurred at 2006, whereas among females it occurred at 2004 (see Table 2).
Figure 1.
Age-adjusted rates of emergency department visits per 100 000 population of sports- and recreation-related traumatic brain injury, by year and sex, National Electronic Injury Surveillance System-All Injury Program, 2001-2012, United States.
SRR-TBI ED visits by age group
On average each year during the reporting period, approximately 70% of all SRR-TBI ED visits occurred among persons 19 years or younger (see Table 1). Rates of SRR-TBI ED visits increased significantly between 2001 and 2012 for all age groups (all Ps < 0.001), with persons in age groups ranging from 10 to 24 years and 45 years or older showing increases exceeding 110% (see Table 1).
Estimated rates for SRR-TBI ED visits by sex, year, and age group
Among males, the rates of SRR-TBI ED visits per 100 000 population increased significantly from 2001 to 2012 in all age groups, except for those aged 35 to 44 years whose rates were not calculated because the estimates were unstable (see Table 1). SRR-TBI ED visit rates for males were significantly higher in those aged 5 to 9, 10 to 14, and 15 to 19 years than in those in other age groups (all Ps < .05; see Table 1).
Among females, the rates of SRR-TBI ED visits per 100 000 population increased significantly from 2001 to 2012 in all age groups, except for those 45 years or older whose rates were not calculated because the estimates were unstable (see Table 1). SRR-TBI ED visit rates were significantly higher among females aged 5 to 9, 10 to 14, and 15 to 19 years than in those in other age groups (P < .05; see Table 1).
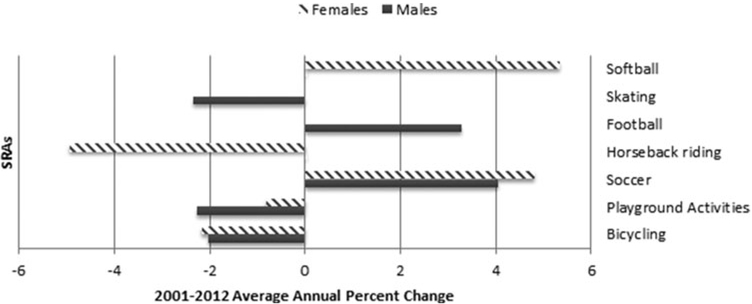
Ten leading SRAs with the highest proportion of TBI ED visits by sex
Among the 10 leading SRAs comprising the highest proportion of TBI-related ED visits, the activities that accounted for the largest SRR-TBI AAPCs varied by sex and year (see Table 3). Among males, the highest number of SRR-TBI ED visits in 2001 and 2012 occurred while engaged in bicycling and football. From 2001 to 2012, the AAPC in SRR-TBI ED visits significantly increased the most in soccer (4.04%; 95% CI, 1.35-6.79; P = .0071) and football (3.29%; 95% CI, 1.70-4.90; P = .0009) (see Figure 2). In contrast, the AAPC decreased the most in skating (−2.34%; 95% CI, −4.47 to −0.17; P = .0374) and playground activities (−2.26%; 95% CI, −4.43 to −0.04; P = .0467) (see Figure 2).
TABLE 3.
Number, percent, and AAPC of the 10 most common SRAs resulting in traumatic brain injury–related emergency department visits, by sex, NEISS-AIP, 2001-2012, United States
| Ten leading SRAs by sex |
2001 |
2012 |
2001-2012 AAPC (95% CI)a |
Trend test p value |
||
|---|---|---|---|---|---|---|
| n | % (95% CI)a | n | % (95% CI)a | |||
| Male | ||||||
| Bicycling | 29 532 | 20.4 (10.4-30.4) | 52 077 | 16.9 (11.1-22.7) | − 2.04 (− 3.05 to − 1.02) | .01 |
| Football | 21 907 | 15.2 (13.2-17.1) | 64 322 | 20.8 (15.5-26.2) | 3.29 (1.70-4.90) | .01 |
| Basketball | 10 475 | 7.2 (4.9-9.6) | 26 530 | 8.6 (6.7-10.5) | 1.15 (− 1.07 to 3.42) | |
| Playground activities |
11 042 | 7.6 (5.4-9.8) | 17 379 | 5.6 (4.3-7.0) | − 2.26 (− 4.43 to − 0.04) | .05 |
| Baseball | 8236 | 5.7 (4.1-7.3) | 15 554 | 0.04 (−1.70 to 1.81) | 5.0 (3.5-6.6) | |
| ATV | 6 930b | 4.8 (. . .) | 10 957 | 3.6 (2.0-5.1) | . . . | . . . |
| Snow sportsc | 10 647b | 7.4 (. . .) | 10 184 | 3.3 (1.4-5.2) | . . . | . . . |
| Skatingd | 6 720 | 4.6 (3.2-6.1) | 11 546 | 3.7 (2.3-5.2) | − 2.34 (− 4.47 to − 0.17) | .05 |
| Soccer | 4 787 | 3.3 (1.8-4.8) | 17 259 | 5.6 (3.7-7.5) | 4.04 (1.35- 6.79) | .01 |
| Mopede | 3 794 | 2.6 (1.7-3.5) | 7 965 | 2.6 (1.9-3.2) | − 0.18 (− 3.82 to 3.60) | |
| All other SRAs | 30 477 | 21.1 (15.5-26.6) | 74 793 | 24.2 (17.9-30.6) | 1.26 (.023-2.28) | .05 |
| Total | 144 546 | 100.0 (73.3-126.7) | 308 566 | 100.0 (76.5-123.5) | . . . | . . . |
| Female | ||||||
| Bicycling | 9 139 | 14.4 (6.8-22.1) | 16 395 | 11.5 (7.6-15.5) | − 2.18 (− 7.79 to 3.78) | |
| Playground activities |
6 663 | 10.5 (6.2-14.8) | 15 041 | 10.6 (8.1-13.0) | − 0.83 (− 2.82 to 1.21) | |
| Horseback riding |
7 016 | 11.1 (4.8-17.4) | 6 340 | 4.5 (2.5-6.4) | − 4.95 (− 8.69 to − 1.05) | .05 |
| Soccer | 3 419 | 5.4 (3.9-6.9) | 14 881 | 10.5 (6.0-14.9) | 4.80 (3.23-6.40) | .01 |
| Basketball | 4 580 | 7.2 (5.4-9.0) | 12 506 | 8.8 (5.9-11.7) | 2.93 (0.78-5.13) | .05 |
| Snow sportsc | 6 862b | 10.8 ( . . . ) | 7 009 | 4.9 (3.2-6.7) | . . . | . . . |
| ATV | 1 589b | 2.5 ( . . . ) | 5 718 | 4.0 (1.8-6.2) | . . . | . . . |
| Softball | 1 618 | 2.6 (1.3-3.8 | 7 705 | 5.4 (3.7-7.1) | 5.35 (0.41-10.54) | .05 |
| Gymnastics | 2 700 | 4.3 (2.8-5.8) | 10 636 | 7.5 (4.8-10.2) | 4.37 (0.88-7.99) | .05 |
| Water sportsf | 2 580 | 4.1 (2.0-6.2) | 6 355 | 4.5 (3.2-5.8) | 0.17 (− 4.27 to 4.81) | |
| All other SRAs | 17 090b | 27.0 ( . . . ) | 39 572 | 27.8 (21.6-34.1) | . . . | . . . |
| Total | 63 257 | 100.0 (80.5-119.5) | 142 157 | 100.0 (77.2-122.8) | . . . | . . . |
Abbreviations: AAPC, average annual percent change; ATV, all-terrain vehicle; CI, confidence interval; NEISS-AIP, National Electronic Injury Surveillance System-All Injury Program; SRA, sports and recreational activity.
95% CI (not presented for unstable estimates).
The number was derived from an unstable estimate. Estimates are considered unstable when the number of unweighted NEISS cases is less than 20 or the national (weighted) estimate is less than 1200 or the coefficient of variation is more than 30%. No 95% CIs and no full range 2001-2012 AAPC were calculated for unstable estimates.
Includes snow skiing, ice skating, toboggan/sled/discovery, and snowmobile.
Includes in-line, roller, and board skating.
Includes minicars/off-road vehicles/go-carts.
Includes swimming, water skiing/surfing/personal watercraft, and fishing.
Figure 2.
SRAs with the largest average annual percentage change in TBI-related emergency department visits, by sex, National Electronic Injury Surveillance System-All Injury Program, 2001-2012, United States. SRA indicates sports and recreational activity.
Among females, the SRAs associated with the largest number of SRR-TBI ED visits varied in 2001 and 2012 (see Table 3). In 2001, the highest number of TBI-related ED visits occurred while engaged in bicycling and horse-back riding, respectively. In 2012, the second highest number of TBI-related ED visits occurred as a result of playground activities. From 2001 to 2012, the largest significant increase in the AAPC in SRR-TBI ED visits was observed in softball (5.35%; 95% CI, 0.41-10.54; P = .0363) and soccer (4.80%; 95% CI, 3.23-6.40; P = .00004) (see Figure 2). In contrast, the AAPC significantly decreased the most in horseback riding (−4.95%; 95% CI, −8.69 to −1.05; P = .0183) (see Figure 2).
SRAs with the highest number and proportion of TBI ED visits by sex and age group
The 5 leading SRAs associated with TBI ED visits varied by age group and sex (see Table 4). Among males aged 0 to 4 and 5 to 9 years, SRR-TBI ED visits occurred frequently during bicycling and playground activities. Among 10- to 14- and 15- to 19-year-old males, football and bicycling were activities in which TBI frequently occurred. Among 20- to 24-year-old men, bicycling, basketball, and ATVs were frequent activities resulting in TBI; and among men 25 years or older, bicycling and ATVs were the activities in which TBI frequently occurred.
TABLE 4.
SRAs with the highest proportion of traumatic brain injury–related emergency department visits, by sex and age group, NEISS-AIP, 2001-2012, United States
| Rank order by sex |
0-4 y |
5-9 y |
10-14 y |
15-19 y |
20-24 y |
25-34 y |
35-44 y |
45+ y |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SRA | % | SRA | % | SRA | % | SRA | % | SRA | % | SRA | % | SRA | % | SRA | % | |
| Male | N = 128 377 | N = 343 890 | N = 638 525 | N = 632 909 | N = 171 213 | N = 162 185 | N = 111 724 | N = 179 208 | ||||||||
| 1 | Playground activities | 35.6 | Bicycling | 21.0 | Football | 24.9 | Football | 30.6 | Bicycling | 18.8a | Bicycling | 22.0a | Bicycling | 35.7 | Bicycling | 49.5 |
| 2 | Bicycling | 17.5 | Playground activities | 19.0 | Bicycling | 16.1 | Bicycling | 9.6 | Basketball | 10.7 | ATV | 13.9 | ATV | 12.0 | ATV | 7.0a |
| 3 | Baseball | 6.5 | Baseball | 8.6 | Basketball | 10.0 | Basketball | 9.6 | ATV | 10.7 | Snow sportsb | 6.7a | Mopedc | 6.0 | Horse riding | 5.5a |
| 4 | Scooter | 5.3 | Football | 8.2 | Baseball | 7.0 | Soccer | 6.6 | Football | 8.8 | Soccer | 5.9 | Horse riding | 5.9a | Snow sportsb | 5.4a |
| 5 | Water sportsd | 4.3 | Basketball | 5.0 | Skatinge | 5.8 | Snow sportsb | 4.8a | Mopedc | 6.6 | Football | 5.8 | Snow sportsb | 5.8a | Exercisef | 5.0 |
| All other | 30.8 | All other | 38.2 | All other | 36.2 | All other | 38.8 | All other | 11.2 | All other | 45.7 | All other | 34.6 | All other | 27.6 | |
| Female | N = 72 882 | N = 156 235 | N = 247 443 | N = 252 600 | N = 69 632 | N = 73 848 | N = 65 759 | N = 110 304 | ||||||||
| 1 | Playground activities | 46.0 | Playground activities | 31.0 | Soccer | 12.8 | Soccer | 16.1 | Bicycling | 17.5a | Bicycling | 20.4a | Horse Riding | 22.2 | Bicycling | 22.6 |
| 2 | Bicycling | 13.5 | Bicycling | 19.1 | Basketball | 12.2 | Basketball | 14.8 | Horse riding | 11.1 | Horse riding | 11.3 | Bicycling | 19.1 | Horse riding | 19.5 |
| 3 | Trampoline | 5.9 | Water sportsd | 5.2 | Bicycling | 10.0 | Gymnastics | 9.5 | ATV | 10.0a | Snow sportsb | 9.4 | Snow sportsb | 10.3 | Exercisef | 11.8 |
| 4 | Baseball | 5.6 | Snow sportsb | 5.0 | Gymnastics | 7.2 | Snow sportsb | 7.2 | Snow sportsb | 8.8 | ATV | 9.2 | Water sportsd | 6.2 | Snow sportsb | 6.7 |
| 5 | Water sportsd | 4.8 | Scooter | 4.6 | Softball | 6.9 | Softball | 7.2 | Water sportsd | 5.6 | Softball | 7.7 | ATV | 5.8a | ATV | 5.3a |
| All other SRAs | 24.2 | All other SRAs | 35.1 | All other SRAs | 35.1 | All other SRAs | 45.2 | All other SRAs | 47.0 | All other SRAs | 42.0 | All other SRAs | 36.4 | All other SRAs | 34.1 | |
Abbreviations: ATV, all-terrain vehicle; CI, confidence interval; NEISS-AIP, National Electronic Injury Surveillance System-All Injury Program; SRA, sports and recreational activity.
The percentage was derived from an unstable estimate. Estimates are considered unstable when the number of unweighted NEISS cases is less than 20 or the national (weighted) estimate is less than 1200 or the coefficient of variation is more than 30%.
Includes snow skiing, ice skating, toboggan/sled/discovery, and snowmobile.
Includes minicars/off road vehicles/go-carts.
Includes swimming, water skiing/surfing/personal watercraft, and fishing.
Includes in line, roller, and board skating.
Includes weight lifting
Playground activities and bicycling were frequent SRAs resulting in TBI-related ED visits among 0- to 4- and 5- to 9-year-old females. Among 10- to 14- and 15- to 19-year-old females, soccer and basketball were activities in which TBI frequently occurred, whereas among women 20 years or older, bicycling and horseback riding were activities frequently resulting in TBI.
Five leading activities with the highest percent estimates of TBI ED visits by discharge disposition
The discharge disposition of persons with SRR-TBI ED visits varied by activity and sex (see Table 5). Of the 2 368 405 males with an SRR-TBI treated in EDs during 2001-2012, 89.0% were treated and released, with the remainder being hospitalized or transferred to other facilities. Hospitalization or transfers to other facilities in males were frequently associated with bicycling and ATV use, although the estimate of the latter activity was unstable.
TABLE 5.
Aggregated yearly numbers and percentages of 5 leading SRAs associated with the highest number and percentage of traumatic brain injury–related emergency department visits by discharge disposition and sex, NEISS-AIP, 2001-2012, United States
| Rank order by sex | Treated and released |
Hospitalized/transferred |
Totala |
|||
|---|---|---|---|---|---|---|
| SRAs | % | SRAs | % | SRAs | % | |
| Male | N = 2 107 008 | N = 216 368 | N = 2 368 405 | |||
| 1 | Football | 18.5 | Bicycling | 33.3 | Bicycling | 19.2 |
| 2 | Bicycling | 17.7 | ATV | 16.2b | Football | 17.3 |
| 3 | Basketball | 8.1 | Mopedc | 7.7 | Basketball | 7.6 |
| 4 | Playground activities | 6.2 | Football | 6.1 | Playground activities | 5.8 |
| 5 | Baseball | 5.9 | Snow sportsb | 6.0b | Baseball | 5.5 |
| All other SRAs | 43.6 | All other SRAs | 30.7 | All other SRAs | 44.6 | |
| Female | N = 953 206 | N = 77 385 | N = 1 048 864 | |||
| 1 | Bicycling | 12.7 | Horseback riding | 23.2b | Bicycling | 13.3 |
| 2 | Playground activities | 10.5 | Bicycling | 19.8b | Playground activities | 10.1 |
| 3 | Soccer | 8.6 | ATV | 16.5b | Horseback riding | 8.3 |
| 4 | Basketball | 8.3 | Snow sportsd | 5.4b | Soccer | 8.1 |
| 5 | Horseback riding | 7.1 | Exercisee | 4.4b | Basketball | 7.8 |
| All other SRAs | 52.8 | All other SRAs | 30.7 | All other SRAs | 52.4 | |
Abbreviations: ATV, ATV, all-terrain vehicle; NEISS-AIP, National Electronic Injury Surveillance System-All Injury Program; SRA, sports and recreational activity.
Includes unknown and other discharge dispositions.
Unstable estimate. Estimates are considered unstable when the number of unweighted NEISS cases is less than 20 or the national (weighted) estimate is less than 1200 or the coefficient of variation is more than 30%.
Includes minicars/off-road vehicles/go-carts.
Includes snow skiing, ice skating, toboggan/sled/discovery, and snowmobile.
Includes weight lifting.
Of the 1 048 864 females with an SRR-TBI treated in EDs during the study period, the majority (90.9%) were treated and released; all estimates of SRR-TBIs resulting in hospitalization or transfers to another facility were unstable.
DISCUSSION
This study indicates that SRR-TBIs accounted for 7.0% of all SRR injuries during 2001-2012. This latter statistic, however, represents approximately 3.4 million SRR-TBIs. Results also reveal that SRR-TBIs treated in US EDs have increased from 2001 to 2012 among males and females of all ages, particularly those aged 10 to 19 years. Overall, annual rates of SRR-TBI visits to EDs per 100 000 population significantly increased from 73.1 in 2001 to 152.0 in 2012; increases in rates were significant for all age groups and for both sexes. The leading activities related to TBI treated in EDs varied by sex and age group and were likely related to activity popularity, ability, and choice. In general, among males, bicycling, football, and basketball were the leading activities associated with SRR-TBI ED visits; and among females, these activities were bicycling, playground activities, and horseback riding.
The significant increases observed during 2001-2012 are difficult to interpret because of limited information regarding changes over time in the numbers and demographics of persons participating in each SRA. Multiple factors might have contributed to these changes, including increased incidence, participation, or awareness of potential TBI that may have prompted injured persons to seek medical care. Previous research found ED visits for all SRR injuries among persons 19 years or younger did not increase during 2001-2009 whereas ED visits for SRR-TBIs increased.4 In addition, the percentage of persons with SRR-TBIs seen in EDs requiring hospitalization/transfer for further care decreased.4 These data suggest that the observed increase in ED-treated SRR-TBIs may not be a consequence of an actual increase in incidence in TBIs in sports and recreation. Only a portion of injuries from sports and recreation are treated in the ED.13 If activities actually were more dangerous, one would expect to see increases in all types of sports injuries, not just TBIs, and the hospitalization of a similar proportion of ED-treated TBI.4 While hospitalization rates in general have decreased, this does not explain the lack of increase in other SRR injuries treated in the ED. Finally, there also does not appear to have been a large shift in SRR participation in general as the proportion of persons 15 years or younger in the United States who were engaged in sports, exercise, and recreation activities increased from 18.5% in 2003 to 19.5% in 2010.14–16
These findings suggest that the significant increases in ED visits for SRR-TBIs across most age groups and in both sexes might reflect the increased knowledge of the importance of early diagnosis and management of mild TBI among healthcare providers, sports coaches, parents, and the public. This might have prompted people, who in the past may have deemed these injuries as minimal, to seek medical care by visiting an ED.17,18 Several efforts might account for the potential increase in TBI awareness and knowledge. For example, in 2004, the CDC, in conjunction with many partners, launched the “Heads Up” program to improve prevention, recognition, and response to concussion in sports among clinicians.19 In 2005, the Heads Up program began engaging coaches, parents, and athletes in a similar vein (http://www.cdc.gov/headsup/youthsports/index.html). There also has been increased media attention related to cases of TBI observed in US troops and professional athletes in the last decade.17 Finally, the passage of youth sports concussion laws in all 50 states since 2009 may also partially explain the increase in ED visits in the present study (http://www.ncsl.org/research/health/traumatic-brain-injury-legislation.aspx). Joinpoint regression analyses conducted in the current study found significant increases in SRR-TBIs that began in 2004 for females and in 2006 for males. The reasons for these sex and time differences are unclear and merit further investigation.
Although the US population-based rates we report suggest that males have higher rates of SRR-TBIs than females, studies using participation- or exposure-based rates often find the reverse, with higher rates of SRR-TBIs among females within comparable activities.20–23 This discrepancy may have occurred because our study did not take into account participation by or exposure to SRAs; therefore, comparisons across activities between this and the other studies cannot be made. Furthermore, the SRAs in this study may not have been the same as those reported in studies that used participation or exposure information.
The large number of SRR-TBI ED visits among persons aged 0 to 19 years align with previous research3,4and may be the result of many factors. In children, participation in higher-risk activities, such as organized team sports, and increases in participants’ weight and speed are positively associated with age, and this may lead to greater force of impact.24 In addition, one study found that participation in team sports has a higher risk of injury than that in individual sports.25 Our study found that during 2001-2012, TBIs that occurred while engaged in football was a frequent activity resulting in ED visits among males aged 10 to 19 years. Opportunities for organized team sports participation expand with age. Findings from a national survey of high school students aged 15 to 19 years found that 58.4% of students have played on at least 1 sports team, with a higher prevalence for males (64.0%).26 Although scant literature exists about the practices of coaches and athletic trainers, 2 studies of coaches who were exposed to the CDC “Heads Up: Concussion in High School Sports” toolkit27,28 found that respondents self-reported favorable changes in knowledge, attitudes, and practices toward the prevention and management of concussions.27 This, in turn, led to better prevention practices, better recognition of the injury, and better response to the injury by coaches.28 Other factors that are not measured in NEISS, for example, alcohol use, may also contribute to SRR injuries among certain age groups. A study found that almost 24% of the pedal cyclists killed in 2010 traffic crashes in the United States had a high blood alcohol concentration.29 Characterizing these factors merits further research so that they can be potentially be targeted for prevention.
Despite reports finding decreases in the average number of hours spent participating in sports, exercise, and recreation per day among persons 45 years or older,14,16 our study found that the rates and numbers of SRR-TBI ED visits in this age group almost doubled during 2001-2012. Some of these increases also may be related to the increased knowledge and awareness of TBI described earlier. Healthcare providers who serve these populations, especially older adults (ie, 65 years or older), should be vigilant about the increasing number of comorbidities (eg, diabetes); the number and type of medications taken; and the age-related decreases in vision, hearing, coordination, strength, and cognitive function.30–37 All these factors may contribute to an increased risk for injuries, including TBIs, and they may even affect recovery. It is also important for healthcare providers, regardless of patient age, to inquire about a history of TBI, as those who sustain a TBI may be at risk of sustaining subsequent TBIs.38–40
Our study suggests that bicycling is significantly associated with SRR-TBI ED visits in males and females and is a leading cause of hospitalization/transfer to other hospitals. NEISS, however, contains limited information regarding whether a bicycle-related injury occurred during sports or leisure riding, as opposed to bicycling for mobility purposes. Therefore, the estimates we reported likely include bicycle injuries that did not occur during a purely recreational endeavor. Regardless, our study found that bicycling was a leading activity resulting in a TBI-related ED visit. Hence, bicycle safety should be a main target for prevention, as many of bicycling injuries result from collisions or near-collisions with motor vehicles, especially those that result in death.29
Various prevention efforts, such as helmet use, may help reduce the number and severity of TBI in bicyclists. Use of helmets should be encouraged, as our results indicate that riding on bicycles, horses, and ATVs resulted in a high number of SRR-TBI–related hospitalizations or transfers to other hospitals in both males and females. The higher proportion of hospitalizations we found in bicycling- and ATV-related TBIs (although this latter estimate was unstable in this study) suggest that certain biomechanical forces may be involved41,42; for example, the higher velocity of impact, impact force, force impulse to injury, and the angle of impact observed in bicycle-related injury events may result in more severe injuries requiring higher levels of care, including hospitalization.43 Previous research also found that at least 90% of bicycle riders44 and 70% of ATV riders45 who crashed and died were not wearing helmet. This suggests that despite some progress, prevention efforts can benefit by increasing helmet use for all riders. Nonetheless, TBIs can still occur, even when helmets are worn as has been reported in football.46,47 To be effective, appropriate helmet use requires a helmet that is appropriate for the position and activity, properly fitted, well-maintained, and used consistently and correctly.48 Regarding ATVs, research indicates that the number of ATV-related deaths have declined since 2005.45 Although this decline coincided with the increase in the number of states with legislation regulating ATV rider behavior (eg, helmet laws, age, and use restrictions),49 studies of the efficacy of such legislation have produced inconclusive results.50–54
Providing safer environments as recommended by the Consumer Product Safety Commission’s Public Playground Safety Handbook (eg, using age-appropriate equipment, using shock-absorbing surfaces, adult supervision)55 can also reduce the risk and severity of TBI such as in playground activities,56 which are associated with high occurrence of TBI in young children of both sexes. Despite that these recommendations have been periodically updated and disseminated since 1981,55 NEISS-AIP data indicate that the rate of playground-related TBI per 100 000 population significantly increased from 22.7 in 2005 to 45.8 in 2011 (CDC unpublished data).
Other SRR-preventive measures include implementing and enforcing the return-to-play decision strategies and other rules/policy change19; teaching sports-specific skills and proper techniques (eg, blocking/tackling in football); encouraging good sportsmanship; and actively educating referees, coaches, trainers, parents, athletes, and the public about the consequences of TBI.18,19 Overall, a combination of protective measures, such as safe environments, appropriate use of helmets, and non–equipment-based protective methods (eg, good conditioning), may have the potential to reduce injury incidence and severity in SRR-TBIs.57
Our study found that almost 90% of persons with SRR-TBI ED visits were treated and released, suggesting that these cases may have been of mild TBI. However, despite some controversy,58–61 the term “mild TBI” is in some cases a misnomer because up to 15% to 25% of people with this condition5–7 may have persistent signs and symptoms 1 year after the injury.54–66 Of the remainder, approximately 6% were transferred or hospitalized; an undetermined number of these may have had more severe TBI. Persons with more severe TBI may even have lifelong impairment or disability.67
Limitations
Limitations of the NEISS-AIP have been detailed elsewhere.3 In summary, the lack of denominator data to calculate activity-specific rates in NEISS (eg, the number of people riding bicycles in the United States) limited our ability to identify activities and groups at higher risk within specific activities. Second, NEISS-AIP underestimates the number of ED-treated TBIs in SRAs. Because only the principal diagnosis and data about the primary body part injured are collected in NEISS-AIP, many TBIs that were secondary diagnoses, such as those reported in conjunction with other more severe nonbrain injuries or were listed in the narrative section of the questionnaire, may have been missed.3,10 In addition, certain TBI-related diagnoses, for example, skull fractures, which commonly involve TBI, are listed as fractures of the head, and not as TBIs, resulting in an underestimation of the number of ED visits due to an SRR-TBI. Also missed were cases treated in non-ED healthcare settings or those who did not seek medical care. Third, for certain surveillance years and population subgroups, small sample sizes precluded the production of stable estimates for those groups. Caution should be used when interpreting unstable estimates. Fourth, NEISS-AIP does not include information on risk or protective factors (eg, use of helmets while riding on ATVs) limiting our understanding of the changes observed during 2001-2012. Additional information that may be missing includes the consumer products involved (eg, baseball equipment), a description of events leading to the injury, injury locale, and even details of the injury diagnosis. Much of this information can only be obtained from the NEISS records’ narratives; however, it is not systematically available since patients may not share these details with providers, providers may not choose to document it in the medical record, or coders may not choose to enter the information. Finally, increases in the overall SRR-TBI rate over the study period may have resulted from increases in the knowledge of the risk of sports-and recreation-related concussion and TBI, from shifts in location of medical care, or other issues.
CONCLUSIONS
On the basis of this first nationally representative study of trends in SRR-TBIs among persons of all ages in the United States, we found that the number of SRR-TBI ED visits has increased from 2001 to 2012. Overall, 3.42 million ED visits for SRR-TBI diagnoses were identified during the study period; this figure, however, is likely an underestimate of the true burden of SRR-TBIs because it captures only ED visits. SRR-TBIs affected mostly males, especially those aged 0 to 19 years. Our study also found that the leading activities associated with TBI-related ED visits varied by age and sex.
This information can be used to tailor prevention strategies intended to reduce the burden of SRR-TBIs in the United States by age group, sex, and SRA. Additional research that includes population-based information on participation (eg, number of participants and duration of participation) by the specific SRA is needed to better characterize risk and protective factors to prevent these injuries and determine the most effective prevention and management strategies. Special attention for prevention should be given, for example, to activities with a large number of affected participants (eg, bicycling, playground activities, and some team sports) and those with more severe injuries (eg, bicycling and riding on ATVs). Because our findings indicate that the leading types of SRAs associated with TBI-related ED visits varied by age and sex, prevention strategies should be focused on those most at risk among the activities that are more likely to result in TBI.
Footnotes
The Centers for Disease Control and Prevention (CDC) Experience is a 1-year fellowship in applied epidemiology at the CDC) made possible by a public/private partnership supported by a grant to the CDC Foundation from External Medical Affairs, Pfizer Inc.
The authors thank Tom Schroeder, Director, Division of Hazard and Injury Data Systems, and other staff of the US Consumer Product Safety Commission for providing high-quality National Electronic Injury Surveillance System-All Injury Program data for this study.
The findings and conclusion of this research are those of the authors and do not necessarily represent the official views of the US Department of Health and Human Services (DHHS) and the Centers for Disease Control and Prevention (CDC). The inclusion of individuals, programs, or organizations in this article does not constitute endorsement by the US federal government, DHHS, or CDC.
The authors declare no conflicts of interest.
Contributor Information
Victor G. Coronado, Division of Unintentional Injury Prevention.
Tadesse Haileyesus, Division of Analysis, Research Practice Integration.
Tabitha A. Cheng, Division of Unintentional Injury Prevention; National Center for Injury Prevention and Control, and The CDC Experience Applied Epidemiology Fellowship, Division of Scientific Education and Professional Development.
Jeneita M. Bell, Division of Unintentional Injury Prevention.
Juliet Haarbauer-Krupa, Division of Unintentional Injury Prevention.
Michael R. Lionbarger, Division of Unintentional Injury Prevention.
Javier Flores-Herrera, Centers for Disease Control and Prevention, Atlanta, Georgia; and Medical Emergency Service ofMadrid, SUMMA 112, Spanish Field Epidemiology Training Program, Epidemiology National Center, Madrid, Spain.
Lisa C. McGuire, Division of Nutrition Physical Activity, National Center for Chronic Disease Prevention and Health Promotion.
Julie Gilchrist, Division of Unintentional Injury Prevention.
REFERENCES
- 1.US Consumer Product Safety Commission. NEISS data highlights 2001. [Google Scholar]
- 2.US Consumer Product Safety Commission. NEISS data highlights 2010. http://www.cpsc.gov//PageFiles/106634/2010highlights.pdf Accessed Feburary 13, 2015.
- 3.Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries from sports and recreation activities—United States, 2001–2005. MMWR Morb Mortal Wkly Rep. 2007;56(29):733–737. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Nonfatal traumatic brain injuries related to sports and recreation activities among persons aged ≤19 years—United States, 2001–2009. MMWR Morb Mortal Week Rep. 2011;60(39):1337–1342. [PubMed] [Google Scholar]
- 5.Cassidy JD, Cancelliere C, Carroll LJ, et al. Systematic review of self-reported prognosis in adults after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3)(suppl):S132–S151. [DOI] [PubMed] [Google Scholar]
- 6.Carroll LJ, Cassidy JD, Cancelliere C, et al. Systematic review of the prognosis after mild traumatic brain injury in adults: cognitive, psychiatric, and mortality outcomes: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3)(suppl):S152–S173. [DOI] [PubMed] [Google Scholar]
- 7.Cancelliere C, Kristman VL, Cassidy JD, et al. Systematic review of return to work after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil. 2014;95(3)(suppl): S201–S209. [DOI] [PubMed] [Google Scholar]
- 8.Bazarian JJ, Blyth B, Mookerjee S, He H, McDermott MP. Sex differences in outcome after mild traumatic brain injury. J Neurotrauma. 2010;27:527–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Runge JW. The cost of injury. Emerg Med Clin N Am. 1993;11(1):241–253. [PubMed] [Google Scholar]
- 10.Schroeder T, Ault K. The NEISS sample (design and implementation): 1997 to present 2001. http://www.cpsc.gov/neiss/2001d011-6b6.pdf Published April 14, 2012. Accessed February 12, 2015.
- 11.US Consumer Product Safety Commission. NEISS Coding Manual January 2013. http://www.cpsc.gov/PageFiles/106513/completemanual.pdf Published April 11, 2013. Accessed February 11, 2015.
- 12.Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. [DOI] [PubMed] [Google Scholar]
- 13.Warner M, Barnes PM, Fingerhut LA. Injury and poisoning episodes and conditions: National Health Interview Survey, 1997. Vital Health Stat 2000;10(202):1–38. [PubMed] [Google Scholar]
- 14.US Department of Labor Bureau of Labor Statistics. American Time Use Survey (ATUS). ATUS Tables. Table 9. Average hours per day spent in leisure and sports activities for the total population by selected characteristics, 2003 annual averages. http://www.bls.gov/news.release/archives/atus09142004.pdf Published 2003. Accessed February 13, 2015.
- 15.US Department of Labor, Bureau of Labor Statistics. American Time Use Survey (ATUS). ATUS Tables. Table A-1. Time spent in detailed primary activities, and percent of the civilian population engaging in each detailed activity category, averages per day by sex (PDFS). http://www.bls.gov/tus/#tables. Published 2003–2010. Accessed February 27, 2015.
- 16.US Department of Labor, Bureau of Labor Statistics. American Time Use Survey. ATUS Tables. Table 11. Time spent in leisure and sports activities for the civilian population by selected characteristics, 2010 annual averages. http://www.bls.gov/news.release/archives/atus06222011.pdf Published 2010. Accessed February 11, 2015.
- 17.Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Saf Res. 2012;43(4):299–307. [DOI] [PubMed] [Google Scholar]
- 18.Coronado VG, Thurman DJ, Greenspan AJ, Weissman B. Epidemiology of traumatic brain injury In:Jallo J, Loftus CM, eds. Neurotrauma and Critical Care of the Brain. New York, NY: Thieme Medical Publishers; Inc; 2009:3–19. [Google Scholar]
- 19.Centers for Disease Control and Prevention. Heads Up: brain injury in your practice. http://www.cdc.gov/headsup/providers/index.html. Published December 4, 2014. Accessed February 11, 2015.
- 20.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 21.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. [PMC free article] [PubMed] [Google Scholar]
- 22.Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40(4):747–755. [DOI] [PubMed] [Google Scholar]
- 23.Dick RW. Is there a gender difference in concussion incidence and outcomes? Br J Sports Med. 2009;43(suppl 1):i46–i50. [DOI] [PubMed] [Google Scholar]
- 24.Proctor MR, Cantu RC. Head and neck injuries in young athletes. Clin Sports Med. 2000;19(4):693–715. [DOI] [PubMed] [Google Scholar]
- 25.Theisen D, Frisch A, Malisoux L, Urhausen A, Croisier JL, Seil R. Injury risk is different in team and individual youth sport. J Sci Med Sport/Sports Med Aust. 2013;16(3):200–204. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Youth Risk Behavioral Surveillance— United States. Atlanta, GA: Division of Adolescent and School Health, National Center for HIV/AIDS, Viral Hepatitis, STD & TB Prevention; 2011. [Google Scholar]
- 27.Sarmiento K, Mitchko J, Klein C, Wong S. Evaluation of the Centers for Disease Control and Prevention’s concussion initiative for high school coaches: “Heads Up: Concussion in High School Sports.” J School Health. 2010;80(3):112–118. [DOI] [PubMed] [Google Scholar]
- 28.Covassin T, Elbin RJ, Sarmiento K. Educating coaches about concussion in sports: evaluation of the CDC’s “Heads Up: concussion in youth sports” initiative. J School Health. 2012;82(5):233–238. [DOI] [PubMed] [Google Scholar]
- 29.US Department of Transportation, National Highway Traffic Safety Administration. Bicyclists and Other Cyclists. Traffic Safety Facts, 2008 Data. Washington, DC: US Department of Transportation, National Highway Traffic Safety Administration; 2008. DOT HS 810 886W. [Google Scholar]
- 30.Coronado VG, Thomas KE, Sattin RW, Johnson RL. The CDC traumatic brain injury surveillance system: characteristics of persons aged 65 years and older hospitalized with a TBI. J Head Trauma Rehabil. 2005;20(3):215–228. [DOI] [PubMed] [Google Scholar]
- 31.Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28(6):513–518. [DOI] [PubMed] [Google Scholar]
- 32.Judge JO, Lindsey C, Underwood M, Winsemius D. Balance improvements in older women: effects of exercise training. Phys Ther. 1993;73(4):254–262; discussion 63–65. [DOI] [PubMed] [Google Scholar]
- 33.Kraus JF, McArthur DL. Epidemiologic aspects of brain injury. Neurol Clin. 1996;14(2):435–450. [DOI] [PubMed] [Google Scholar]
- 34.Lord SR, Caplan GA, Ward JA. Balance, reaction time, and muscle strength in exercising and nonexercising older women: a pilot study. Arch Phys Med Rehabil. 1993;74(8):837–839. [DOI] [PubMed] [Google Scholar]
- 35.Ray WA, Griffin MR. Prescribed medications and the risk of falling. Top Geriatr Rehabil. 1990;5:12–20. [Google Scholar]
- 36.Sasser HC, Hammond FM, Lincourt AE. To fall or not to fall. Brain injury in the elderly. N C Med J. 2001;62(6):364–367. [PubMed] [Google Scholar]
- 37.Tinetti ME. Clinical practice. Preventing falls in elderly persons. New Engl J Med. 2003;348(1):42–49. [DOI] [PubMed] [Google Scholar]
- 38.Annegers JF, Grabow JD, Kurland LT, Laws ER Jr. The incidence, causes, and secular trends of head trauma in Olmsted County, Minnesota, 1935–1974. Neurology. 1980;30(9): 912–919. [DOI] [PubMed] [Google Scholar]
- 39.Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996–1999. Am J Epidemiol. 2004;160(10):937–944. [DOI] [PubMed] [Google Scholar]
- 40.Salcido R, Costich JF. Recurrent traumatic brain injury. Brain Inj. 1992;6(3):293–298. [DOI] [PubMed] [Google Scholar]
- 41.Bigler ED. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc. 2008;14:1–22. [DOI] [PubMed] [Google Scholar]
- 42.Son BC, Park CK, Choi BG. Metabolic changes in pericontusional oedematous areas in mild head injury evaluated by 1H MRS. Acta Neurochirurgica. 2000;76(suppl):13–16. [DOI] [PubMed] [Google Scholar]
- 43.Syed SH, Willing R, Jenkyn TR, Yazdani A. Video analysis of the biomechanics of a bicycle accident resulting in significant facial fractures. J Craniofac Surg. 2013;24(6):2023–2029. [DOI] [PubMed] [Google Scholar]
- 44.Insurance Institute for Highway, Safety Highway Loss Data Insti-tute Highway Safety Topics. Fatality Facts. Bicyclists. Bicyclist Deaths by Helmet Use, 1994–2009. Ruckersville, VA: Insurance Institute for Highway Safety; 2009. [Google Scholar]
- 45.US Consumer Product Safety Commission. ATV-Related Deaths and Injuries for All Ages 1985–2010. Bethesda, MD: US Consumer Product Safety Commission; http://www.atvsafety.gov/stats.html. Published December 31, 2011. Accessed October 12, 2013. [Google Scholar]
- 46.Viano DC, Pellman EJ, Withnall C, Shewchenko N. Concussion in professional football: performance of newer helmets in reconstructed game impacts, part 13. Neurosurgery. 2006;59(3):591–606; discussion 591–606. [DOI] [PubMed] [Google Scholar]
- 47.Cantu RC. Active voice: is helmet design the answer to concussion in collision sports? Sports Med Bull (IN). 2010. http://www.multibriefs.com/briefs/acsm/100510.html. Accessed January 12, 2015. [Google Scholar]
- 48.Marshall SWG J, Saluja G Sports and recreational injuries In: Liller KD, ed. Injury Prevention for Children and Adolescents: Integration of Research, Practice, and Advocacy. 2nd ed. Washington, DC: American Public Health Association; 2011:261–290. [Google Scholar]
- 49.US Consumer Product Safety Commission. ATV State Legislative Resource Bank. Bethesda, MD: US Consumer Product Safety Commission; http://www.atvsafety.gov/legislation/legislation.html. Accessed January 30, 2015. [Google Scholar]
- 50.Upperman JS, Shultz B, Gaines BA, et al. All-terrain vehicle rules and regulations: impact on pediatric mortality. J Pediatr Surg. 2003;38(9):1284–1286. [DOI] [PubMed] [Google Scholar]
- 51.Helmkamp JC, Aitken ME, Graham J, Campbell CR. State-specific ATV-related fatality rates: an update in the new millennium. Public Health Rep. 2012;127(4):364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keenan HT, Bratton SL. All-terrain vehicle legislation for children: a comparison of a state with and a state without a helmet law. Pediatrics. 2004;113(4):e330–e334. [DOI] [PubMed] [Google Scholar]
- 53.McBride AS, Cline DM, Neiberg RH, Westmoreland KD. Pediatric all-terrain vehicle injuries: does legislation make a dent? Pediatr Emerg Care. 2011;27(2):97–101. [DOI] [PubMed] [Google Scholar]
- 54.Winfield RD, Mozingo DW, Armstrong JH, et al. All-terrain vehicle safety in Florida: is legislation really the answer? Am Surg. 2010;76(2):149–153. [PubMed] [Google Scholar]
- 55.US Consumer Product Safety Commission. Public Playground Safety Handbook (Publication No. 325). http://www.cpsc.gov/pagefiles/122149/325.pdf Published November 2010. Accessed December 2, 2014.
- 56.Coronado VG, McGuire LC, Lionbarger MR, Wald MM, Sarmiento K, Gilchrist J. Sports and recreation-related traumatic brain injury In:Rippe JM, ed. Lifestyle Medicine. 2nd ed. London, England: CRC Press; 2013:1519–1530. [Google Scholar]
- 57.Navarro RR. Protective equipment and the prevention of concussion—what is the evidence? Curr Sports Med Rep. 2011;10(1):27–31. [DOI] [PubMed] [Google Scholar]
- 58.Smith-Seemiller L, Fow NR, Kant R, Franzen MD. Presence of post-concussion syndrome symptoms in patients with chronic pain vs. mild traumatic brain injury. Brain Inj. 2003;17(3):199–206. [DOI] [PubMed] [Google Scholar]
- 59.Gasquoine PG. Postconcussional symptoms in chronic back pain. Appl Neuropsychol. 2000;7:83–89. [DOI] [PubMed] [Google Scholar]
- 60.Iverson GL. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Arch Clin Neuropsychol. 2006;21:303–310. [DOI] [PubMed] [Google Scholar]
- 61.Iverson GL, Lange RT. Examination of “Postconcussion-Like” symptoms in a healthy sample. Appl Neuropsychol. 2003;10:137–144. [DOI] [PubMed] [Google Scholar]
- 62.Tellier A, Della Malva LC, Cwinn A, Grahovac S, Morrish W, Brennan-Barnes M. Mild head injury: a misnomer. Brain Inj. 1999;13(7):463–475. [DOI] [PubMed] [Google Scholar]
- 63.National Center for Injury Prevention and Control. Report to Congress on Mild Traumatic Brain Injury in the United States: Steps to Prevent a Serious Public Health Problem. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 64.McCrea MA. Mild traumatic brain injury and postconcussion syndrome: the new evidence base for diagnosis and treatment (Oxford Workshop Series: American Academy of Clinical Neuropsychology) New York, NY: Oxford University Press; 2008. [Google Scholar]
- 65.Carroll LJ, Cassidy JD, Peloso PM, Borg J, von Holst H, Holm L, Paniak C, Pepin M. Prognosis for mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain injury. J Rehabil Med 2004;43(Suppl): 84–105. [DOI] [PubMed] [Google Scholar]
- 66.Ruff R Two decades of advances in understanding of mild traumatic brain injury. J Head Trauma Rehabil. 2005;20:5–18. [DOI] [PubMed] [Google Scholar]
- 67.Bazarian JJ, Cernak I, Noble-Haeusslein L, Potolicchio S, Temkin N. Long-term neurologic outcomes after traumatic brain injury. J Head Trauma Rehabil. 2009;24(6):439–451. [DOI] [PubMed] [Google Scholar]