Abstract
Guidelines recommend measuring out-of-clinic blood pressure (BP) to identify masked hypertension (MHT) defined by out-of-clinic BP in the hypertensive range among individuals with clinic-measured BP not in the hypertensive range. The aim of this study was to determine the overlap between ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM) for the detection of MHT. We analyzed data from 333 community-dwelling adults not taking antihypertensive medication with clinic BP<140/90 mmHg in the Improving the Detection of Hypertension Study. Any MHT was defined by the presence of daytime MHT (mean daytime BP≥135/85 mmHg), 24-hour MHT (mean 24-hour BP≥130/80 mmHg), and/or nighttime MHT (mean nighttime BP≥120/70 mmHg). Home MHT was defined as mean BP≥135/85 mmHg on HBPM. The prevalence of MHT was 25.8% for any MHT and 11.1% for home MHT. Among participants with MHT on either ABPM and/or HBPM, 29.5% had MHT on both ABPM and HBPM; 61.1% had MHT only on ABPM; and 9.4% of participants had MHT only on HBPM. After multivariable adjustment and compared to participants without MHT on ABPM and HBPM, those with MHT on both ABPM and HBPM and only on ABPM had a higher left ventricular mass index (mean difference [standard error, SE] 12.7 [2.9] g/m2, p<0.001; and 4.9 [2.1] g/m2, p=0.022, respectively), whereas participants with MHT only on HBPM did not have an increased left ventricular mass index (mean difference [SE] −1.9 [4.8] g/m2, p=0.693). These data suggest that conducting ABPM will detect many individuals with MHT who have an increased cardiovascular disease risk.
Keywords: Masked hypertension, cardiovascular risk, left ventricular mass, ambulatory blood pressure, ambulatory blood pressure monitoring, home blood pressure monitoring
Some adults with blood pressure (BP) not in the hypertensive range when measured in the clinic have levels in the hypertension range when measurements are obtained outside of the clinic setting, a phenotype known as masked hypertension (MHT).1 Compared to individuals with sustained normotension, defined by the absence of hypertension both in and outside of the clinic setting, individuals with MHT have an increased risk for cardiovascular disease (CVD) and target organ damage.2,3
There are two primary methods of measuring out-of-clinic BP to diagnose MHT: ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM). Currently, there is little evidence to determine whether ABPM, HBPM, or both modalities should be used to detect MHT among individuals not taking antihypertensive medication. A prior study by Stergiou et. al. assessed the prevalence of MHT according to both ABPM and HBPM.4 In this analysis, only 44% of individuals with MHT had elevated BP outside of the clinic according to both ABPM and HBPM, with the remainder having MHT detected by ABPM only (34%) or HBPM only (22%). However, this study included patients from a hypertension clinic, one-third of whom were taking antihypertensive medication. Further, MHT on ABPM was defined using only daytime BP. More recent guidelines from the European Society of Hypertension / European Society of Cardiology (ESH/ESC) have recommended that MHT be defined by the presence of daytime, 24-hour and/or nighttime hypertension.5 Despite this recommendation, few published data are available on the overlap between ABPM and HBPM for detecting MHT when daytime, 24-hour, and nighttime BP on ABPM are used to identify MHT.
The primary aim of this study was to compare the prevalence of MHT when out-of-clinic BP is measured by ABPM versus HBPM in individuals not taking antihypertensive medications. A secondary aim of this study was to compare levels of left ventricular mass index (LVMI), a measure of cardiovascular target-organ damage, between participants without MHT on ABPM and HBPM, MHT only on ABPM, MHT only on HBPM, and MHT on both ABPM and HBPM.
Methods
Sample Population
The data that support the findings of this study are available from the corresponding author upon reasonable request. The Improving the Detection of Hypertension (IDH) Study is a community-based study of adults in the metropolitan New York City area designed to compare strategies for diagnosing ambulatory hypertension. Between March 2011 and October 2013, the IDH Study enrolled 408 adults age 18 years or older, without a history of treated hypertension.6,7 Study exclusion criteria were: clinic systolic BP ≥160 mmHg or diastolic BP ≥105 mmHg during a screening visit; evidence of secondary hypertension; taking antihypertensive medication; taking other medications that affect BP (e.g., steroids, tricyclic antidepressants, etc.); a self-reported history of CVD, kidney, liver, adrenal, thyroid, rheumatologic, or hematologic diseases; organ transplantation; cancer or dementia; or current pregnancy. The study protocol was approved by the Institutional Review Board at Columbia University and all participants provided written informed consent.
For the current analysis, participants were excluded if they did not have complete clinic BP data (n = 3), did not have complete ABPM data (n = 15) or complete HBPM data (n = 3), or did not have echocardiography data (n = 5). Criteria for defining complete clinic BP, ABPM, and HBPM are provided below. As this study focused on participants with MHT, we further restricted the analysis to those with mean clinic systolic BP <140 mmHg and mean clinic diastolic BP <90 mmHg at Visit 1, leaving a final analytic sample of 333 participants for the primary analysis.
Study Procedures
Demographic information (i.e., age, sex, race/ethnicity) was ascertained at the time of study enrollment using a self-administered questionnaire and information regarding cardiovascular risk factors including smoking status, current use of antihypertensive medication, and self-reported diabetes status was ascertained during a structured interview. Eligible participants attended five visits (Visits 1 to 5) over approximately a four-week period. Clinic BP was measured at Visits 1, 3, and 4, ABPM was performed for 24-hours following Visit 1, and HBPM was conducted by the participants for three weeks, beginning after Visit 2. Echocardiography and laboratory measures were performed at Visit 5.
Laboratory Measures.
Urine and fasting blood samples were obtained from participants. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation based on serum creatinine.8 Albuminuria was defined as urine albumin-to-creatinine ratio ≥30 mg/g. Chronic kidney disease was defined as having reduced eGFR (defined as <60 mL/min/1.73m2) or albuminuria.
Clinic BP.
Clinic BP was measured following a standardized protocol. After resting in a seated position for five minutes, BP was measured in triplicate with at least one minute between readings by a trained research nurse/technician using a mercury sphygmomanometer (Baum, Copiague, NY) and an appropriate-sized arm cuff.9 Complete clinic BP data was defined as having three readings at Visit 1, which were averaged.
ABPM.
After clinic BP was measured at Visit 1, participants were trained in the use of a validated ABPM device (Spacelabs Model 9020710; Snoqualmie, WA) and fitted with an appropriate-sized arm cuff and a wrist actigraphy device (ActiWatch; Phillips Respironics, Murrayville, PA). Ambulatory BP measurements were taken at 30-minute intervals throughout the subsequent 24-hour period and the device was returned the next day. The nighttime and daytime periods were defined by the onset of asleep and awake periods, assessed using the wrist actigraphy device supplemented by participant diary reports. Using the International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO) criteria,11 participants with ≥10 daytime and ≥5 nighttime readings were considered to have a complete ABPM recording. The BP readings during the daytime, 24-hour, and nighttime period were averaged to obtain mean daytime BP, mean 24-hour BP, and mean nighttime BP, respectively.
HBPM.
After returning the ABPM device (Visit 2), participants were given a HBPM device, Omron HEM-790IT (HEM-7080-ITZ2)12 or HEM-791IT (HEM-7222-ITZ),13 with an appropriate-sized cuff and trained on its use. Participants were instructed to obtain home BP measurements in the seated position after five minutes of rest with one minute between readings, and to measure their BP twice in the morning immediately after awakening and twice before going to bed for three consecutive weeks. BP readings were automatically stored in the memory of the HBPM device with time and date stamps, and directly extracted by study staff. For the current analysis, participants with 16 or more HBPM readings were considered to have complete HBPM data. All of the BP readings were averaged to obtain mean home BP.
2D Echocardiography.
After returning the HBPM device, participants returned for a two-dimensional echocardiogram. Standard images were acquired, and primary measures of left ventricular (LV) dimensions, volumes, and wall thickness were obtained according to recommendations from the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACI).14 LV mass (LVM, g) was calculated using the ASE formula. LVMI (g/m2) was calculated as LVM divided by body surface area derived by the DuBois method.15
Definitions of Hypertension Categories
Clinic hypertension was defined as mean clinic systolic BP ≥140 mmHg or mean clinic diastolic BP ≥90 mmHg. Systolic and diastolic BP thresholds for daytime, 24-hour, and nighttime hypertension, which are based on US and international guidelines,5,16 are shown in Table S1 As the current analysis only included participants with mean clinic systolic BP <140 mmHg and mean clinic diastolic BP <90 mmHg, those with daytime, 24-hour, nighttime, and home hypertension met criteria for daytime MHT, 24-hour MHT, nighttime MHT, and home MHT, respectively. Any MHT was defined as having MHT for any ABPM period (i.e. daytime MHT, 24-hour MHT, and/or nighttime MHT).
Participants were categorized as having MHT on both ABPM and HBPM, MHT on ABPM but not HBPM (MHT only on ABPM), MHT on HBPM but not ABPM (MHT only on HBPM), and without MHT on ABPM and HBPM. Classifications were done for each type of MHT (any MHT, daytime MHT, 24-hour MHT, and nighttime MHT) on ABPM and Home MHT.
Statistical Analyses
Participant characteristics were calculated for the overall analytic sample and by categories defined by the cross-classification of any MHT and home MHT status. The prevalence of each type of MHT on ABPM (any, daytime, 24-hour, and nighttime MHT) and MHT on HBPM was calculated. Also, we determined the proportion of participants within categories defined by the cross-classification of the status of each type of MHT on ABPM and home MHT.
Next, the difference in mean LVMI between participants with versus without each type of MHT on ABPM was calculated in an unadjusted model using one-way Analysis of Variance (ANOVA), and in a model adjusting for age, sex, race (Black or not), ethnicity (Hispanic or not), and current smoking using Analysis of Covariance (ANCOVA). The adjusted model did not include body mass index, since LVM was indexed to body surface area, and both body mass index and body surface area are derived from height and weight. The analysis was repeated with MHT on HBPM.
Differences in mean LVMI between categories defined by the cross-classification of MHT on ABPM and MHT on HBPM with the reference group being those without MHT on ABPM and HBPM, were determined in an unadjusted one-way ANOVA model, and in an ANCOVA model adjusting for age, sex, race, and ethnicity. Secondary analyses were performed by replacing any MHT with daytime MHT, 24-hour MHT, and nighttime MHT, one at a time.
Four sensitivity analyses were performed. First, the primary analyses were repeated after restricting the sample to participants with mean clinic systolic BP <130 mmHg and mean clinic diastolic BP <80 mmHg (N=234) at Visit 1, which is the threshold for clinic hypertension in the 2017 American College of Cardiology (ACC) / American Heart Association (AHA) BP guideline.17 Hypertension status on ABPM and HBPM was also defined using BP thresholds from the 2017 ACC/AHA BP guideline (Table S1). Second, the analyses were repeated after the sample was restricted to participants with mean clinic systolic BP <140 mmHg and a mean clinic diastolic BP <90 mmHg (N=309) at each of the 3 study visits at which clinic BP measurement was assessed (Visits 1, 3, and 4). Third, the analyses were repeated after the sample was restricted to participants with a complete ABPM defined according to European Society of Hypertension (ESH) guideline criteria18 (N=309) instead of IDACO criteria: 20 daytime measurement, 7 nighttime measurements, and 24-hour recording with at least 70% of expected measurements. Finally, the analyses were repeated after using the HBPM data collected during the first 7 days of HBPM recording (N=333).
Results
Baseline Characteristics
In the cohort included in these analyses, the mean (standard deviation [SD]) age was 40.1 (12.9) years, 61.3% of participants were female, and 24.3% and 61.9% were Black and Hispanic, respectively (Table 1). Also, 1.5% of participants had diabetes and 4.8% had chronic kidney disease. The mean (SD) clinic systolic and diastolic BP were 112.2 (11.6) mmHg and 73.7 (8.0) mmHg, respectively. The mean (SD) number of daytime BP and nighttime BP readings on ABPM were 30 (5) and 13 (3), respectively. The mean (SD) number of HBPM readings was 82 (20).
Table 1:
Characteristics of participants in the overall analytical sample and by masked hypertension (MHT) status, defined using ambulatory blood pressure monitoring (ABPM) cross-classified by home blood pressure monitoring (HBPM).
| Characteristics | Overall Analytic Sample (N=333) | Neither Any MHT nor Home MHT (N = 238) | Any MHT without Home MHT (N = 58) | Home MHT without Any MHT (N = 9) | Both Any MHT and Home MHT (N = 28) |
|---|---|---|---|---|---|
| Age, years | 40.1 (12.9) | 37.6 (11.8) | 45.4 (14.1) | 47.6 (11.7) | 47.9 (12.9) |
| Female | 204 (61.3) | 156 (65.5) | 34 (58.6) | 4 (44.4) | 10 (35.7) |
| Black race | 81 (24.3) | 50 (21.0) | 21 (36.2) | 3 (33.3) | 7 (25.0) |
| Hispanic ethnicity | 206 (61.9) | 151 (63.4) | 33 (56.9) | 5 (55.6) | 17 (60.7) |
| Clinical Characteristics | |||||
| Diabetes | 5 (1.5) | 2 (0.8) | 1 (1.7) | 1 (11.1) | 1 (3.6) |
| Chronic kidney disease | 16 (4.8) | 11 (4.6) | 2 (3.4) | 0 (0.0) | 3 (10.7) |
| Current smoker | 29 (8.7) | 19 (8.0) | 5 (8.6) | 0 (0.0) | 5 (17.9) |
| Body mass index kg/m2 | 27.0 (4.7) | 26.3 (4.5) | 28.7 (4.7) | 30.7 (5.7) | 28.0 (5.3) |
| Blood Pressure Measures | |||||
| Clinic SBP, mmHg | 112.2 (11.6) | 109.1 (10.7) | 118.8 (10.0) | 118.6 (12.7) | 123.1 (8.5) |
| Clinic DBP, mmHg | 73.7 (8.0) | 71.6 (7.5) | 77.9 (7.2) | 77.3 (7.1) | 81.9 (4.3) |
| Daytime SBP, mmHg | 122.0 (10.4) | 117.6 (7.7) | 131.5 (7.4) | 127.7 (4.1) | 137.5 (8.4) |
| Daytime DBP, mmHg | 76.4 (6.8) | 73.8 (5.3) | 82.0 (5.8) | 79.1 (3.1) | 86.5 (4.3) |
| 24-hour SBP, mmHg | 117.7 (10.0) | 113.3 (7.2) | 127.9 (6.6) | 121.6 (5.1) | 132.1 (8.4) |
| 24-hour DBP, mmHg | 72.3 (6.5) | 69.6 (4.8) | 78.6 (5.3) | 73.6 (3.7) | 81.9 (4.2) |
| Nighttime SBP, mmHg | 107.1 (10.8) | 102.6 (7.5) | 119.2 (9.2) | 109.0 (8.0) | 118.9 (10.0) |
| Nighttime DBP, mmHg | 62.2 (7.4) | 59.3 (5.2) | 70.2 (6.7) | 62.3 (4.6) | 70.9 (6.3) |
| Home SBP, mmHg | 113.2 (11.7) | 109.0 (9.3) | 118.7 (7.7) | 126.6 (7.7) | 133.7 (8.1) |
| Home DBP, mmHg | 75.2 (7.7) | 72.4 (6.4) | 79.0 (4.3) | 84.8 (1.9) | 87.8 (5.4) |
The numbers in the table are mean (standard deviation) or n (percentage)
Any MHT was defined as having daytime MHT, 24-hour MHT, and/or nighttime MHT on ABPM
Daytime MHT was defined as mean SBP ≥ 135 mmHg and/or mean DBP ≥ 85 mmHg using BP readings during the daytime period on ABPM
24-hour MHT was defined as mean SBP ≥ 130 mmHg and/or mean DBP ≥ 80 mmHg using all available readings on ABPM
Nighttime MHT was defined as mean SBP ≥ 120 mmHg and/or mean DBP ≥ 70 mmHg during the nighttime period on ABPM
Home MHT was defined as mean home SBP ≥ 135 mmHg and/or mean DBP ≥ 85 mmHg on HBPM
ABPM: Ambulatory blood pressure monitoring
DBP: Diastolic blood pressure
HBPM: Home blood pressure monitoring
MHT: Masked hypertension
SBP: Systolic blood pressure
Prevalence of MHT on ABPM and MHT on HBPM
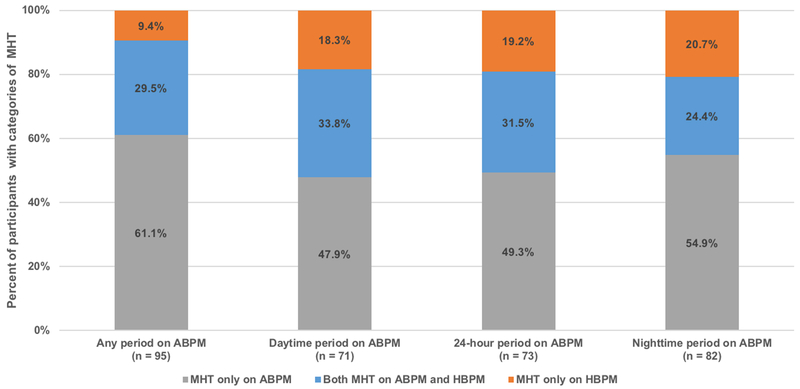
Among participants without clinic hypertension, the prevalence of any MHT on ABPM was 25.8% and 11.1% for Home MHT. The prevalence of daytime, 24-hour, and nighttime MHT were 17.4%, 17.7% and 19.5%, respectively. When any ABPM period was used to define MHT, 71.5% did not have MHT on ABPM and HBPM, 8.4% of participants had MHT on both ABPM and HBPM, 17.4% had MHT only on ABPM, and 2.7% of participants had MHT only on HBPM (Table 2). Among the participants with MHT on ABPM and/or HBPM, 29.5% had MHT on both ABPM and HBPM, 61.1% had MHT only on ABPM, and only 9.4% had MHT only on HBPM (Figure 1). Among participants with MHT on ABPM and/or HBPM, 18.3%, 19.2%, and 20.7% of participants, respectively, had MHT only on HBPM when the daytime, 24-hour, and nighttime period were examined.
Table 2:
Cross-classification of masked hypertension (MHT) status defined using ambulatory blood pressure monitoring (ABPM) by MHT status defined using home blood pressure monitoring (HBPM)
| Classification | Any MHT Status | |
|---|---|---|
| Home MHT Status | Without Any MHT | Any MHT |
| Without Home MHT | 238 (71.5%, 66.6% – 76.3%) | 58 (17.4%, 13.3% – 21.5%) |
| Home MHT | 9 (2.7%, 1.0% – 4.4%) | 28 (8.4%, 5.4% – 11.4%) |
| Daytime MHT Status | ||
| Home MHT Status | Without Daytime MHT | Daytime MHT |
| Without Home MHT | 262 (78.7%, 74.3% – 83.1%) | 34 (10.2%, 7.0% – 13.5%) |
| Home MHT | 13 (3.9%, 1.8% – 6.0%) | 24 (7.2%, 4.4% – 10.0%) |
| 24-hour MHT Status | ||
| Home MHT Status | Without 24-hour MHT | 24-hour MHT |
| Without Home MHT | 260 (78.1%, 73.6% – 82.5%) | 36 (10.8%, 7.5% – 14.1%) |
| Home MHT | 14 (4.2%, 2.0% – 6.4%) | 23 (6.9%, 4.2% – 9.6%) |
| Nighttime MHT Status | ||
| Home MHT Status | Without Nighttime MHT | Nighttime MHT |
| Without Home MHT | 251 (75.4%, 70.7% – 80.0%) | 45 (13.5%, 9.8% – 17.2%) |
| Home MHT | 17 (5.1%, 2.7% – 7.5%) | 20 (6.0%, 3.5% – 8.6%) |
Data are expressed as number (percentage, 95% CI)
Any MHT was defined as having daytime MHT, 24-hour MHT, and/or nighttime MHT on ABPM
Daytime MHT was defined as mean SBP ≥ 135 mmHg and/or mean DBP ≥ 85 mmHg using BP readings during the daytime period on ABPM
24-hour MHT was defined as mean SBP ≥ 130 mmHg and/or mean DBP ≥ 80 mmHg using all available readings on ABPM
Nighttime MHT was defined as mean SBP ≥ 120 mmHg and/or mean DBP ≥ 70 mmHg during the nighttime period on ABPM
Home MHT was defined as mean home SBP ≥ 135 mmHg and/or mean DBP ≥ 85 mmHg on HBPM
ABPM: Ambulatory blood pressure monitoring
CI: confident interval
DBP: Diastolic blood pressure
HBPM: Home blood pressure monitoring
MHT: Masked hypertension
SBP: Systolic blood pressure
Figure 1:
Distribution of participants into categories based on the absence or presence of masked hypertension on ambulatory blood pressure monitoring and home blood pressure monitoring.
Associations of MHT Defined by ABPM and HBPM with LVMI
Compared to participants without MHT, those with any MHT, daytime MHT, 24-hour MHT, nighttime MHT, and home MHT each had a higher LVMI in unadjusted and adjusted models (Table S2).
Associations of Categories Defined by the Cross-Classification of Each Type of MHT on ABPM and Home MHT Status with LVMI
Compared to those without any MHT on ABPM and HBPM (reference group), LVMI was higher among participants with MHT only on ABPM (adjusted mean difference [standard error (SE)] 4.9 [2.1] g/m2, p=0.022) and participants with MHT on both ABPM and HBPM (adjusted mean difference [SE] 12.7 [2.9] g/m2, p<0.001) (Table 3). In contrast, compared to those without MHT on ABPM and HBPM, participants with MHT only on HBPM did not have a higher LVMI (adjusted mean difference [SE] –1.9 [4.8] g/m2, p=0.693).
Table 3:
Mean and mean differences in left ventricular mass index comparing participants with neither masked hypertension (MHT) on ambulatory blood pressure monitoring (ABPM) nor home blood pressure monitoring (HBPM) versus participants with MHT only on ABPM, MHT only on HBPM, and MHT on both ABPM and HBPM.
| Measure | Categories Defined by Any MHT Status and Home MHT Status | ||||
|---|---|---|---|---|---|
| Neither Any MHT nor Home MHT (N = 238) | Any MHT without Home MHT (N = 58) | Home MHT without Any MHT (N = 9) | Both Any MHT and Home MHT (N = 28) | p-value | |
| LVMI* | 76.0 (15.1) | 82.1 (14.4) | 77.1 (9.2) | 92.6 (18.0) | - |
| Unadjusted difference† | 0 (ref) | 6.1 (2.2) | 1.1 (5.1) | 16.6 (3.0) | P1=0.006 P2=0.837 P3<0.001 |
| Adjusted difference† | 0 (ref) | 4.9 (2.1) | −1.9 (4.8) | 12.7 (2.9) | P1=0.022 P2=0.693 P3<0.001 |
| Categories Defined by Daytime MHT Status and Home MHT Status | |||||
| Neither Daytime MHT nor Home MHT (N = 262) | Daytime MHT without Home MHT (N = 34) | Home MHT without Daytime MHT (N = 13) | Both Daytime MHT and Home MHT (N = 24) | p-value | |
| LVMI* | 76.5 (15.1) | 82.6 (14.4) | 84.0 (17.8) | 91.5 (17.2) | - |
| Unadjusted difference† | 0 (ref) | 6.2 (2.8) | 7.5 (4.4) | 15.0 (3.3) | P1=0.028 P2=0.085 P3<0.001 |
| Adjusted difference† | 0 (ref) | 4.0 (2.6) | 3.7 (4.1) | 11.0 (3.1) | P1=0.126 P2=0.367 P3<0.001 |
| Categories Defined by 24-hour MHT Status and Home MHT Status | |||||
| Neither 24-hour MHT nor Home MHT (N = 260) | 24-hour MHT without Home MHT (N = 36) | Home MHT without 24-hour MHT (N = 14) | Both 24-hour MHT and Home MHT (N = 23) | p-value | |
| LVMI* | 76.4 (15.1) | 82.7 (14.6) | 81.5 (13.4) | 93.3 (18.5) | - |
| Unadjusted difference† | 0 (ref) | 6.3 (2.7) | 5.1 (4.2) | 16.9 (3.3) | P1=0.021 P2=0.223 P3<0.001 |
| Adjusted difference† | 0 (ref) | 4.3 (2.6) | 1.1 (3.9) | 13.2 (3.2) | P1=0.093 P2=0.788 P3<0.001 |
| Categories Defined by Nighttime MHT Status and Home MHT Status | |||||
| Neither Nighttime MHT nor Home MHT (N = 251) | Nighttime MHT without Home MHT (N = 45) | Home MHT without Nighttime MHT (N = 17) | Both Nighttime MHT and Home MHT (N = 20) | p-value | |
| LVMI* | 76.0 (15.1) | 84.1 (13.9) | 84.1 (13.2) | 92.9 (20.0) | - |
| Unadjusted difference† | 0 (ref) | 8.1 (2.5) | 8.1 (3.8) | 16.9 (3.5) | P1=0.001 P2=0.033 P3<0.001 |
| Adjusted difference† | 0 (ref) | 7.5 (2.3) | 3.4 (3.6) | 14.7 (3.3) | P1=0.001 P2=0.343 P3<0.001 |
Adjusted model adjusts for age, sex, race, ethnicity, and current smoking
P1= comparison of Neither MHT on ABPM nor HBPM with MHT on ABPM without MHT on HBPM
P2= comparison of Neither MHT on ABPM nor HBPM with MHT on HBPM without MHT on ABPM
P3= comparison of Neither MHT on ABPM nor HBPM with Both MHT on ABPM and HBPM
Left ventricular mass index (LVMI) defined as left ventricular mass indexed to body surface area in g/m2
Any MHT was defined as having daytime MHT, 24-hour MHT, and/or nighttime MHT on ABPM
Daytime MHT was defined as mean SBP ≥ 135 mmHg and/or mean DBP ≥ 85 mmHg using BP readings during the daytime period on ABPM
24-hour MHT was defined as mean SBP ≥ 130 mmHg and/or DBP ≥ 80 mmHg using all available readings on ABPM
Nighttime MHT was defined as SBP ≥ 120 mmHg and/or DBP ≥ 70 mmHg during the nighttime period on ABPM
Home MHT was defined as home SBP ≥ 135 mmHg and/or DBP ≥ 85 mmHg on HBPM
Mean (standard deviation)
Mean difference (standard error)
ABPM: Ambulatory blood pressure monitoring
DBP: Diastolic blood pressure
HBPM: Home blood pressure monitoring
MHT: Masked hypertension
SBP: Systolic blood pressure
Compared to the reference group, LVMI was higher among participants with MHT on both ABPM and HBPM when MHT on ABPM was defined using the daytime period (adjusted mean difference [SE] 11.0 [3.1] g/m2, p<0.001), and separately, the 24-hour period (adjusted mean difference [SE] 13.2 [3.2], p<0.001). Compared to the reference group, adjusted differences [SE] in LVMI were 4.0 [2.6] g/m2 for participants with MHT only on ABPM (p=0.126), and 3.7 [4.1] g/m2 for participants with MHT only on HBPM (p=0.367) when using the daytime period on ABPM. Also, compared to the reference group, adjusted differences [SE] in LVMI were 4.3 [2.6] g/m2 for participants with MHT only on ABPM (p=0.093), and 1.1 [3.9] g/m2 for participants with MHT only on HBPM (p=0.788) when using the 24-hour period on ABPM. Further, when MHT on ABPM was examined using the nighttime period, LVMI was higher among participants with MHT only on ABPM (adjusted mean difference [SE] 7.5 [2.3] g/m2, p=0.001) and MHT on both ABPM and HBPM (adjusted mean difference [SE] 14.7 [3.3] g/m2, p<0.001). Finally, compared to the reference group, adjusted mean difference [SE] in LVMI was 3.4 [3.6] g/m2 for participants with MHT only on HBPM (p=0.343).
Sensitivity Analyses Applying the BP Thresholds From the 2017 ACC/AHA BP Guideline
When using the BP thresholds recommended in the 2017 ACC/AHA BP guideline, the prevalence of any MHT, daytime MHT, 24-hour MHT, nighttime MHT, and home MHT were 40.6%, 21.8%, 25.6%, 32.1%, and 16.2% respectively. A higher percentage of participants had MHT only on ABPM, and MHT on both ABPM and HBPM compared to the BP thresholds used in the primary analysis (Table S3). Among participants with MHT on ABPM and/or HBPM, the greatest proportion of participants had MHT only on ABPM (Figure S1). When all ABPM periods were used to define MHT, compared with the participants without MHT on ABPM and HBPM (reference group), adjusted mean difference [SE] in LVMI was 4.0 [2.1] g/m2 (p=0.053) for participants with MHT only on ABPM, 11.2 [5.0] g/m2 (p=0.027) for participants with MHT only on HBPM, and 12.5 [2.7] g/m2 (p<0.001) for those with MHT on both ABPM and HBPM (Table S4).
Sensitivity Analyses Among Participants without Clinic Hypertension at Visits 1, 3, and 4
When the sample size was restricted to participants with a mean clinic systolic BP <140 mmHg and a mean clinic diastolic BP <90 mmHg at Visits 1, 3, and 4, the prevalence of any MHT, daytime MHT, 24-hour MHT, nighttime MHT, and home MHT was 23.0%, 14.2%, 14.6%, 17.2%, and 8.1% respectively. The distribution of participants with MHT on ABPM, HBPM, or both was similar to the primary analysis (Table S5). When all ABPM periods were used to define MHT, compared to participants without MHT on ABPM and HBPM (reference group), the adjusted mean difference [SE] in LVMI was 4.6 [2.2] g/m2 (p=0.033) for participants with MHT only on ABPM, −0.1 [5.3] g/m2 (p=0.985) for participants with MHT only on HBPM, and 11.4 [3.5] g/m2 (p=0.001) for those with MHT on both ABPM and HBPM (Table S6).
Additional Sensitivity Analyses
The prevalence of BP phenotypes and their associations with LVMI did not change when using the ESH18 versus IDACO11 criteria for a complete ABPM (data not shown). When repeating the analyses using the HBPM data collected during the first 7 days of HBPM, the findings were also similar to the corresponding analyses using all HBPM recordings (data not shown).
Discussion
In the current study, we examined the overlap between ABPM and HBPM for detecting MHT and the associations of MHT categories, defined by the cross-classification of MHT on ABPM and MHT on HBPM, with LVMI in individuals not taking antihypertensive medications. The majority of participants with MHT had it on ABPM with or without it on HBPM, whereas a small percentage of participants with MHT had it on HBPM but not ABPM.
Consistent with the current results, prior population-based studies of individuals without clinic hypertension have shown that the prevalence of MHT differs when defined using ABPM or HBPM; ranging from 14% to 30% when assessed using daytime and/or 24-hour periods on ABPM and 12% to 18% when assessed using HBPM.19–22 There is also evidence to suggest that MHT prevalence differs by the period examined on ABPM.19,23 In an analysis of individuals in IDACO without clinic hypertension and not taking antihypertensive medication, the prevalence of MHT was 14% when using the 24-hour period, 19% when using the daytime period, and 28% when using any period (daytime, 24-hour, and/or the nighttime period) on ABPM.21 In the current study, the prevalence of nighttime MHT (19.5%) was slightly higher than the prevalence of daytime MHT (17.4%) or 24-hour MHT (17.7%). These findings are consistent with prior data from the Jackson Heart Study, a cohort of African Americans, where the prevalence of nighttime MHT was also higher than the prevalence of daytime MHT and 24-hour MHT (48.2%, 28.2% and 31.7%, respectively).23
In the current study, participants with MHT on ABPM and, separately, participants with MHT on HBPM each had increased LVMI compared to participants without MHT. Although these results suggest that MHT is associated with increased CVD risk regardless of which out-of-clinic BP monitoring approach is performed, there is controversy regarding whether ABPM or HBPM is the best approach in clinical practice to diagnose MHT.16,24 Compared to HBPM, there are more studies demonstrating an association of ABPM with CVD risk.16,25 Further, ABPM has been the reference standard for measuring BP during the nighttime period and assessing diurnal patterns. However, in the US, ABPM is not widely available in primary care settings,16 and reimbursement for ABPM is low.26 HBPM may also be more practical for routine clinical practice as it more widely available and is associated with greater patient acceptability and tolerability.16,20 Whether using ABPM or HBPM is the superior approach is further complicated by many individuals having MHT on one modality but not the other. Prior studies found that among those with MHT on ABPM and/or HBPM, only 36% to 45% of participants had MHT detected on both ABPM and HBPM.4,27,28 These studies only examined the daytime4,27 or 24-hour28 periods on ABPM and analyzed participants taking and not taking antihypertensive medication pooled together. In 2013, the ESH/ESC hypertension guidelines recommended using all periods (i.e. daytime, 24-hour, and nighttime) on ABPM to detect MHT, and that the term MHT be used only for those not taking antihypertensive medication.5 In the current study, which only includes individuals not taking antihypertensive medication, 90.6% of participants with MHT had MHT on ABPM with or without it on HBPM when using all periods to define MHT on ABPM, whereas only 9.4% with MHT had it detected only on HBPM. When the daytime, 24-hour, and nighttime period were examined separately, 18.3% to 20.7% of participants had MHT only on HBPM. These findings suggest that only a small proportion of individuals with MHT would not be detected if ABPM was conducted without HBPM, and all periods were used to define MHT on ABPM.
MHT is associated with poor prognosis, including increased CVD risk and all-cause mortality.29,30 However, few data exist on the CVD risk associated with MHT when present on ABPM and not HBPM or when present on HBPM but not ABPM.24 In the primary analysis, participants with MHT detected on ABPM with or without MHT on HBPM, had a higher LVMI compared to participants without MHT on ABPM and HBPM, whereas LVMI was not higher among participants with MHT only on HBPM. In contrast, in a sensitivity analysis using BP thresholds from the 2017 ACC/AHA BP guideline, LVMI was higher among participants with MHT only on HBPM. Therefore, it is unclear whether individuals with MHT only on HBPM are at increased CVD risk. In a prior study by Satoh et al.,28 among participants without hypertension based on BP measured in the clinic setting in the Ohasama Study, stroke risk was higher among participants with 24-hour MHT on ABPM but without MHT on HBPM (HR 1.93, 95% CI 1.15 – 3.24) and MHT on HBPM without 24-hour MHT on ABPM (HR 2.26, 95% CI 1.32 – 3.89) compared to individuals with sustained normotension, defined as not having hypertension on 24-hour BP on ABPM and HBPM. One potential explanation for the discrepant results is the outcome was LVMI in the current study and stroke in the Ohasama Study.28 Additionally, in the Ohasama Study, the sample size of participants with MHT only on HBPM was substantially greater (N=75) than in the current study (N=9). Therefore, our study may be underpowered to examine the relation between LVMI and MHT only on HBPM in both the primary and sensitivity analyses.
If individuals with MHT only on HBPM are at increased CVD risk, HBPM may be warranted if ABPM is initially performed and MHT is not present. However, this approach is unlikely to be cost-effective as individuals would have to undergo both ABPM and HBPM, and the prevalence of having MHT on HBPM among individuals without any MHT on ABPM is very low (9/247 = 3.6%). An alternative approach would be to conduct ABPM if MHT is absent on HBPM. However, many individuals would need to undergo both ABPM and HBPM since a substantial proportion (58/296 = 19.6%) of individuals without MHT on HBPM have any MHT on ABPM. Therefore, despite practical concerns regarding the widespread implementation of ABPM,7,16,24,31 it may be preferable to HBPM since it will detect the vast majority of participants with MHT.
This study has several strengths. The IDH Study enrolled a community-based sample with a high representation of Hispanics and Blacks. In addition, both ABPM and HBPM were performed under standardized conditions among the same participants. Further, all BP readings on HBPM were automatically recorded in the devices’ memory, overcoming potential issues regarding inaccurate reporting of readings by participants.32,33 Finally, we examined all time periods on ABPM, allowing us to examine how different time periods on ABPM affect the overlap between MHT on ABPM and MHT on HBPM.
There are also possible limitations. As previously mentioned, the sample size was small for some of the groups defined by the cross-classification of MHT on ABPM and HBPM, and we were unable to conduct subgroup analyses by age, sex or race/ethnicity. The analysis was restricted to individuals not taking antihypertensive medication and, therefore, the findings may not be generalizable to those taking antihypertensive medication. Further, although a large proportion of the sample was Black or Hispanic, it is unknown if the findings from the current study are generalizable to other race/ethnic populations. Finally, the IDH Study was cross-sectional and CVD outcomes were not assessed.
Perspectives
Many individuals without clinic hypertension have MHT, which cannot be detected using clinic BP measurements alone. While ABPM and HBPM both measure out-of-clinic BP, some individuals may be diagnosed as having MHT on one modality but not the other. The results of the current study indicate that among those with MHT detected using ABPM and/or HBPM, the majority had MHT on ABPM with or without it on HBPM, where a minority had MHT only on HBPM. Compared to participants without MHT on ABPM and HBPM, participants with MHT on both modalities and participants with MHT only on ABPM had higher LVMI, whereas those with MHT only on HBPM did not have increased LVMI. MHT only on HBPM was associated with increased LVMI when 2017 ACC/AHA BP guideline-recommended thresholds were used. These findings suggest that using ABPM is essential for detecting most individuals with MHT who are at high CVD risk.
Supplementary Material
Novelty and Significance.
What is New
Few studies have previously examined the overlap between masked hypertension (MHT) on ambulatory blood pressure monitoring (ABPM) using different periods on ABPM and MHT on home blood pressure monitoring (HBPM) among individuals not taking antihypertensive medication.
A large majority of participants with MHT had MHT on ABPM with or without MHT on HBPM, whereas a small minority of participants with MHT had it detected only by HBPM.
Individuals with MHT detected by ABPM only, or both ABPM and HBPM, had an increased left ventricular mass index (LVMI) compared to those without MHT on ABPM and HBPM. Those with MHT only on HBPM did not have increased LVMI.
What is Relevant
MHT is associated with an increased risk of target-organ damage and cardiovascular disease (CVD) events.
This study has direct relevance to whether ABPM or HBPM should be routinely used to detect MHT among individuals not taking antihypertensive medication.
Summary
ABPM detects many individuals with MHT who have increased CVD risk.
Acknowledgements
We are indebted to the study participants and research staff of the Improving the Detection of Hypertension Study, without whose cooperation and dedication this study would not have been possible.
Sources of Funding
This work was supported by P01-HL047540 (D Shimbo, JE Schwartz) and K24-HL125704 (D Shimbo) from the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH). DE Anstey and DN Pugliese received support through T32-HL007854 from NHLBI. NA Bello was supported by the NIH National Center for Advancing Translational Sciences 5KL2-TR001874 and the American College of Cardiology, she is supported by K23-HL136853 from NHLBI. IM Kronish received support from AHRQ, R01-HS024262
Footnotes
Conflict(s) of Interest/Disclosure(s)
PM received an institutional grant from Amgen Inc. unrelated to the topic of the current manuscript. There are no other potential conflicts of interest.
References
- 1.Pickering TG, Davidson K, Gerin W, Schwartz JE. Masked hypertension. Hypertension. 2002;40(6):795–796. [DOI] [PubMed] [Google Scholar]
- 2.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens 2011;24(1):52–58. [DOI] [PubMed] [Google Scholar]
- 3.Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Untreated Masked Hypertension and Subclinical Cardiac Damage: A Systematic Review and Meta-analysis. Am J Hypertens. 2015;28(6):806–813. [DOI] [PubMed] [Google Scholar]
- 4.Stergiou GS, Salgami EV, Tzamouranis DG, Roussias LG. Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: is it the same phenomenon? Am J Hypertens 2005;18(6):772–778. [DOI] [PubMed] [Google Scholar]
- 5.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013;34(28):2159–2219. [DOI] [PubMed] [Google Scholar]
- 6.Abdalla M, Goldsmith J, Muntner P, et al. Is Isolated Nocturnal Hypertension A Reproducible Phenotype? Am J Hypertens 2016;29(1):33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Booth JN 3rd, Muntner P, Diaz KM, et al. Evaluation of Criteria to Detect Masked Hypertension. J Clin Hypertens. (Greenwich). 2016;18(11):1086–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pickering TG. Principles and techniques of blood pressure measurement. Cardiol Clin 2002;20(2):207–223. [DOI] [PubMed] [Google Scholar]
- 10.Peixoto AJ, Gray TA, Crowley ST. Validation of the SpaceLabs 90207 ambulatory blood pressure device for hemodialysis patients. Blood Press Monit 1999;4(5):217–221. [PubMed] [Google Scholar]
- 11.Thijs L, Hansen TW, Kikuya M, et al. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit 2007;12(4):255–262. [DOI] [PubMed] [Google Scholar]
- 12.Coleman A, Steel S, Freeman P, de Greeff A, Shennan A. Validation of the Omron M7 (HEM-780-E) oscillometric blood pressure monitoring device according to the British Hypertension Society protocol. Blood Press Monit 2008;13(1):49–54. [DOI] [PubMed] [Google Scholar]
- 13.Topouchian J, Agnoletti D, Blacher J, et al. Validation of four devices: Omron M6 Comfort, Omron HEM-7420, Withings BP-800, and Polygreen KP-7670 for home blood pressure measurement according to the European Society of Hypertension International Protocol. Vasc Health Risk Manag 2014;10:33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28(1):1–39 e14. [DOI] [PubMed] [Google Scholar]
- 15.Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition. 1989;5(5):303–311; discussion 312-303. [PubMed] [Google Scholar]
- 16.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Ann Intern Med. 2015;163(9):691–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. [DOI] [PubMed] [Google Scholar]
- 18.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013;31(9):1731–1768. [DOI] [PubMed] [Google Scholar]
- 19.Anstey DE, Pugliese D, Abdalla M, Bello NA, Givens R, Shimbo D. An Update on Masked Hypertension. Curr Hypertens Rep 2017;19(12):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens 2014;28(9):521–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asayama K, Thijs L, Li Y, et al. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension. 2014;64(5):935–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white-coat and masked hypertension: International database of home blood pressure in relation to cardiovascular outcome. Hypertension. 2014;63(4):675–682. [DOI] [PubMed] [Google Scholar]
- 23.Booth JN 3rd, Diaz KM, Seals SR, et al. Masked Hypertension and Cardiovascular Disease Events in a Prospective Cohort of Blacks: The Jackson Heart Study. Hypertension. 2016;68(2):501–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anstey DE, Shimbo D. Masked hypertension-what lies ahead? J Hum Hypertens 2017;31(9):545–546. [DOI] [PubMed] [Google Scholar]
- 25.Siu AL, USPSTF. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2015;163(10):778–786. [DOI] [PubMed] [Google Scholar]
- 26.Kent ST, Shimbo D, Huang L, et al. Rates, amounts, and determinants of ambulatory blood pressure monitoring claim reimbursements among Medicare beneficiaries. J Am Soc Hypertens 2014;8(12):898–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hanninen MR, Niiranen TJ, Puukka PJ, Jula AM. Comparison of home and ambulatory blood pressure measurement in the diagnosis of masked hypertension. J Hypertens 2010;28(4):709–714. [DOI] [PubMed] [Google Scholar]
- 28.Satoh M, Asayama K, Kikuya M, et al. Long-Term Stroke Risk Due to Partial White-Coat or Masked Hypertension Based on Home and Ambulatory Blood Pressure Measurements: The Ohasama Study. Hypertension. 2016;67(1):48–55. [DOI] [PubMed] [Google Scholar]
- 29.Ben-Dov IZ, Kark JD, Mekler J, Shaked E, Bursztyn M. The white coat phenomenon is benign in referred treated patients: a 14-year ambulatory blood pressure mortality study. J Hypertens 2008;26(4):699–705. [DOI] [PubMed] [Google Scholar]
- 30.Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between Clinic and Ambulatory Blood-Pressure Measurements and Mortality. N Engl J Med. 2018;378(16):1509–1520. [DOI] [PubMed] [Google Scholar]
- 31.Kronish IM, Kent S, Moise N, et al. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens. 2017;11(9):573–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens. 1998;11(12):1413–1417. [DOI] [PubMed] [Google Scholar]
- 33.van der Hoeven NV, van den Born BJ, Cammenga M, van Montfrans GA. Poor adherence to home blood pressure measurement schedule. J Hypertens 2009;27(2):275–279. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.