Abstract
Ventricular arrhythmias are life-threatening and can serve as a precursor to sudden death. They are a common presentation in patients with severely reduced left ventricular (LV) function. The use of an implantable cardioverter defibrillator (ICD) is seen as an acceptable therapy against malignant ventricular arrhythmias. In patients with LV heart failure, a left ventricular assist device (LVAD) can provide pulsatile flow to mimic the cardiac systolic and diastolic function. We report a case of a 38-year-old male with a LVAD who presented to the emergency department due to syncope and frequent ICD discharges. There were documented episodes of ventricular fibrillation and a failed defibrillator threshold test.
Keywords: Implantable Cardioverter Defibrillator, Left Ventricular Assist Device, Ventricular Fibrillation
Case Presentation
A 38-year-old male was admitted to the emergency department due to syncope and frequent device discharges. The past medical history was significant for dilated cardiomyopathy (DCMP) (LVEF of 25 %) and no reversible cause for the DCMP was found. A previous 12-lead electrocardiogram (ECG) revealed complete left bundle branch block (QRS 145 ms), and a biventricular implantable cardioverter defibrillator (ICD) was implanted at the time. Two years following implantation, his left ventricular (LV) function and functional capacity deteriorated. A left ventricular assist device (LVAD) (Heart Mate III, Abbott, USA) was then implanted and the patient was stable. He was also elected for cardiac transplant and put on the transplant list.
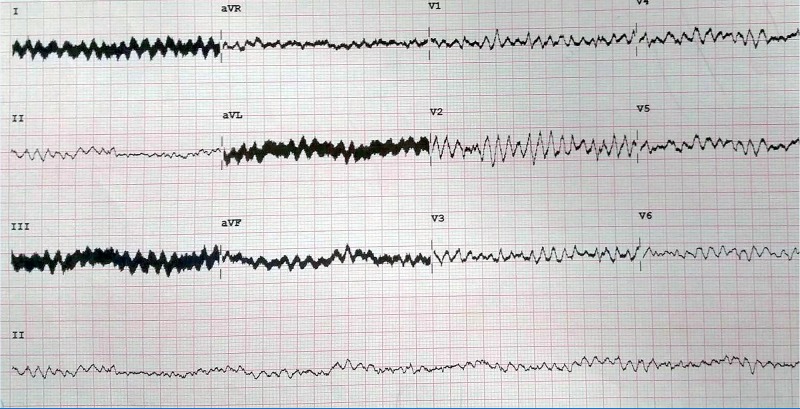
During this indexed episode, the patient witnessed recurrent ICD shocks. Upon arrival of emergency medical services, the patient was found on the floor without consciousness. While in the emergency department (ED), his ECG showed ventricular fibrillation (VF). The patient’s blood pressure was 95/60 mmHg. An external shock of 200 J (bipolar) converted the patient to sinus rhythm (SR). A follow-up ECG revealed atrial sensed biventricular paced rhythm at 67 beats per minute. The patient was admitted for further investigation. During his stay, he did not experience any further ventricular arrhythmias. A chest X-ray showed the atrial lead in a stable position, however the right ventricular (RV) lead was in the base of the RV. Device interrogation was performed and showed detected episodes of VF and shocks; however, the delivered shocks from the device failed to convert the VF into SR. RV sensing was 11.9 mV and both paced and shock impedances were within normal ranges. A defibrillator threshold test (DFT) was scheduled.
Figure 1. 12-lead electrocardiogram showing ventricular fibrillation.
After obtaining consent, the patient was brought into the electrophysiology lab for the DFT. External blood pressure and defibrillator monitoring were present. Under anesthesia, a supported DFT was performed and the ICD delivered [3]shocks. The shocks were ineffective in terminating the VF. External defibrillation was needed to convert the patient to SR. The arterial blood pressure did not change during the recorded VF episode. The patient was informed about his failed DFT and new RV lead implantation was discussed. The patient refused all treatments and requested discharge, which was granted upon his request.
Figure 2A. 2A)Live cardiac monitoring during the DFT depicting paced rhythm with simultaneous recording of arterial blood pressure.

Figure 2B. 2B)) Inductıon of VF with shock on T algorithm and arterial blood pressure remained unaffected.

Discussion
Ventricular arrhythmias are a common presentation in patients with severely reduced LV function. ICDs are a widely accepted treatment option to prevent sudden death from malignant ventricular arrhythmias.[1],[2] However, failed, ineffective, or inappropriate ICD discharges are a possibility. Failure to terminate malignant ventricular arrhythmias in patients with ICDs is not a common scenario. Possible reasons for ineffective ICD therapy can be: excessive changes in the sympathetic tone due to epinephrine release which can cause catecholaminergic polymorphic ventricular tachycardia, lead issues (dislocation, inappropriate lead placement or fracture), ICD dysfunction, metabolic decompensation, or structural heart diseases such as hypertrophic cardiomyopathy[3-08]. The Heart Mate III is a wearable LVAD that is designed to supplement the pumping of the heart through the LV[9]. It serves as the bridge during cardiac transplantation, but it can also assist patients with LV heart failure[10]. The device is attached to the LV and aorta to provide continuous flow. Its unique Full MagLevTM flow technology, based on the CentriMag Pumps, uses magnetic fields to float the device’s rotor, creating a contact and friction-free environment[9],[11],[12]. In our patient, the possible explanations for ineffective ICD discharge can be the following:
1. Inappropriate RV lead position:
the RV lead was implanted in the base of the RV and did not cover the entire ventricle. This can be a possible explanation for ineffective ICD shocks. Repositioning of the RV lead was suggested with a follow-up DFT test, however, the patient declined.
2. Magnetic interference between the LVAD and ICD:
ICDs are commonly used in combination with ventricular assist devices, however, their role together has not been fully established[13]. LVADs may have a direct effect on ICDs, causing alteration of lead parameters, ventricular tachycardias, and electromagnetic interference[13].
3. Possible scarring in the LV apex following LVAD implantation causing refractory
VF: This speculation can be proven by a cardiac MRI or 3D mapping. However, the patient refused any further investigations.
Thus far, there have been two reported cases of sustained VF in alert patients with an LVAD and ICD[10],[14]. We add to the growing literature and discuss the possible reasons and explanations for ineffective device treatments in a patient with an LVAD.
Conflicts of Interest
None.
References
- 1.A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N. Engl. J. Med. 1997 Nov 27;337 (22):1576–83. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 2.Moss A J, Hall W J, Cannom D S, Daubert J P, Higgins S L, Klein H, Levine J H, Saksena S, Waldo A L, Wilber D, Brown M W, Heo M. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N. Engl. J. Med. 1996 Dec 26;335 (26):1933–40. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 3.Yasuda Masayuki, Nakazato Yuji, Sasaki Akitoshi, Kawano Yasunobu, Nakazato Kaoru, Tokano Takashi, Daida Hiroyuki. Ventricular fibrillation refractory to ICD therapy. Intern. Med. 2005 Aug;44 (8):829–31. doi: 10.2169/internalmedicine.44.829. [DOI] [PubMed] [Google Scholar]
- 4.Papaioannou Georgios I, Kluger Jeffrey. Ineffective ICD therapy due to excessive alcohol and exercise. Pacing Clin Electrophysiol. 2002 Jul;25 (7):1144–5. doi: 10.1046/j.1460-9592.2002.01144.x. [DOI] [PubMed] [Google Scholar]
- 5.Veltmann Christian, Borggrefe Martin, Schimpf Rainer, Wolpert Christina. Fatal inappropriate ICD shock. J. Cardiovasc. Electrophysiol. 2007 Mar;18 (3):326–8. doi: 10.1111/j.1540-8167.2006.00692.x. [DOI] [PubMed] [Google Scholar]
- 6.Gul Enes E, Boles Usama, Haseeb Sohaib, Glover Benedict, Simpson Chris, Baranchuk Adrian, Michael Kevin. "Spontaneous Twiddler's" Syndrome: The Importance of the Device Shape. Pacing Clin Electrophysiol. 2017 Mar;40 (3):326–329. doi: 10.1111/pace.12974. [DOI] [PubMed] [Google Scholar]
- 7.Maron B J, Shen W K, Link M S, Epstein A E, Almquist A K, Daubert J P, Bardy G H, Favale S, Rea R F, Boriani G, Estes N A, Spirito P. Efficacy of implantable cardioverter-defibrillators for the prevention of sudden death in patients with hypertrophic cardiomyopathy. N. Engl. J. Med. 2000 Feb 10;342 (6):365–73. doi: 10.1056/NEJM200002103420601. [DOI] [PubMed] [Google Scholar]
- 8.Gul EE, Boles U, Ali F Sadiq, Haseeb S, Simpson C. Double-sensing and Inappropriate Shock: Case Presentation with Differential Diagnosis. Innov Card Rhythm Manag. 2016;7:2489–2491. [Google Scholar]
- 9.Abbott. HeartMate 3TM Left Ventricular Assist System. https://www.sjmglobal.com/en-int/patients/heart-failure/our-solutions/left-ventricle-assist-device/heartmate-3. 2016;0:0–0. [Google Scholar]
- 10.Busch Mathias C, Haap Michael, Kristen Arnt, Haas Christian S. Asymptomatic sustained ventricular fibrillation in a patient with left ventricular assist device. Ann Emerg Med. 2011 Jan;57 (1):25–8. doi: 10.1016/j.annemergmed.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Thoratec Corporation. Full MagLev TM flow technology. http://www.thoratec.com/medical-professionals/vad-product-information/maglev/GL-HM3-03150198%20Full%20MagLev%20info%20sheet.pdf. 2015;0:0–0. [Google Scholar]
- 12.Levitronix. CentriMag Ventricular Assist System (VAS): Patient & Device Management Guidelines. http://www.mc.vanderbilt.edu/documents/heart/files/CentriMag%20VAS%20Patient%20and%20Device%20Management%20Guidelines.pdf. 2009;0:0–0. [Google Scholar]
- 13.Foo David, Walker Bruce D, Kuchar Dennis L, Thorburn Charles W, Tay Andre, Hayward Christopher S, Macdonald Peter, Keogh Anne, Kotlyar Eugene, Spratt Philip, Jansz Paul. Left ventricular mechanical assist devices and cardiac device interactions: an observational case series. Pacing Clin Electrophysiol. 2009 Jul;32 (7):879–87. doi: 10.1111/j.1540-8159.2009.02403.x. [DOI] [PubMed] [Google Scholar]
- 14.Patel Poonam, Williams Jefferson G, Brice Jane H. Sustained ventricular fibrillation in an alert patient: preserved hemodynamics with a left ventricular assist device. Prehosp Emerg Care. 2011 Aug 3;15 (4):533–6. doi: 10.3109/10903127.2011.598616. [DOI] [PubMed] [Google Scholar]