Abstract
Objective:
Posttraumatic stress disorder (PTSD) results from exposure to traumatic events. Social support is negatively related to PTSD symptoms in cross-sectional and longitudinal studies. It is unclear, however, if social support is associated with treatment response for PTSD. The current study evaluated the extent to which social support was associated with PTSD treatment response among treatment-seeking veterans receiving prolonged exposure (PE). It was hypothesized that social support would improve PTSD treatment response and that PTSD symptom reduction would improve social support.
Method:
123 veterans were recruited from Veterans Affairs Medical Center and affiliate referrals and evaluated for PTSD, diagnostic related symptoms, and social support. All participants received prolonged exposure. Data were analyzed using mixed effects models.
Results:
Findings suggested that elevated social support during treatment was associated with greater reductions in PTSD symptoms during treatment. Social support also increased during treatment. Increases in social support were not moderated by PTSD symptoms during treatment.
Conclusions:
These findings suggest that social support and PTSD symptoms are related throughout treatment. Social support moderated the change in PTSD symptoms whereas PTSD symptoms did not moderate changes in social support.
Keywords: Veterans, PTSD, Social Support, Prolonged Exposure
1.1. Introduction
Posttraumatic stress disorder (PTSD) is a chronic condition associated with marked functional impairment after exposure to highly distressing, traumatic events (APA, 2013; Bryant et al., 2015). Exposure-based interventions are efficacious at reducing symptom severity for PTSD (Acierno et al., 2011, 2016; Bradley, Greene, Russ, Dutra, & Westen, 2005; Maples-Keller, Price, Rauch, Gerardi, & Rothbaum, in press). However, a sizable portion of those who receive treatment show limited or minimal symptom change (Schottenbauer, Glass, Arnkoff, Tendick, & Gray, 2008; Steenkamp, Litz, Hoge, & Marmar, 2015). As such, it is necessary to identify factors that determine for whom treatment is more or less effective. Furthermore, if such factors are malleable, they may allow for novel ways to enhance treatment response.
Perceived social support is defined as the perception that others would provide assistance and care in a time of need (Sherbourne & Stewart, 1991; Thoits, 1995). The majority of PTSD-related research on social support has used this definition as will the current study (Brancu et al., 2014; Ozer, Best, Lipsey, & Weiss, 2003). It should be noted, however, that social support is a multidimensional construct that includes both the structure of a support network, the function of the support, and the user and giver’s perceptions (Sherbourne & Stewart, 1991). Numerous cross-sectional studies using different trauma-exposed populations have shown a negative relation between social support and PTSD symptoms severity including disaster victims (Paul et al., 2015), survivors of sexual assault (Borja, Callahan, & Long, 2006; Ullman, Townsend, Filipas, & Starzynski, 2007), and combat veterans (Pietrzak, Johnson, Goldstein, Malley, & Southwick, 2009). Taken together, there is a consensus that elevated social support is associated with reduced PTSD symptom severity. There have been relatively few studies, however, that have investigated the association between social support and PTSD symptom severity during treatment.
It is hypothesized that elevated social support is associated with improved PTSD treatment response. Social support may protect against the stress associated with undergoing treatment for PTSD. Exposure can be an emotionally challenging treatment; patients confront their trauma repeatedly by retelling the trauma narrative in vivid detail during sessions, listening to recordings outside of sessions, and encountering previously avoided trauma reminders. Such activities can temporarily exacerbate PTSD as shown by a study in which 10.5% of patients experienced a temporary increase in PTSD symptoms, and 21.1% experienced a temporary increase of anxiety, during initial sessions of exposure before responding positively to treatment (Foa, Zoellner, Feeny, Hembree, & Alvarez-Conrad, 2002). Social support may buffer the potentially stressful experience of confronting trauma memories and cues. In the context of exposure-based therapy, this could enable individuals with better social support to more readily confront trauma-related stimuli, thereby leading to more improvement during treatment.
Three studies to date have examined the association between social support and treatment response for PTSD. The first examined the association between baseline social support and posttreatment PTSD symptom severity (Thrasher, Power, Morant, Marks, & Dalgleish, 2010). Elevated baseline social support was associated with reduced PTSD symptoms for those who underwent a protocol based on prolonged exposure (PE) as well as those who received cognitive restructuring. Change in social support during the course of treatment was not evaluated. The second examined the role of different types of social support on treatment response in a sample of OEF/OIF veterans (Price, Gros, Strachan, Ruggiero, & Acierno, 2013). Elevated emotional support at baseline was associated with improved treatment response whereas other types of social support were unrelated to treatment outcome. Social support did not change during treatment. The most recent study evaluated the effect of conjoint cognitive behavioral therapy for PTSD in a sample of couples in which one member met criteria for the disorder (Shnaider, Sijercic, Wanklyn, Suvak, & Monson, 2017). Increased support from the significant other at the start of treatment was associated with greater reduction in PTSD symptoms. Change in social support was not evaluated in this study, however. Taken together, these results suggest that baseline support is associated with improved treatment response. Given that social support is proposed to enhance engagement with exposure, it is warranted to evaluate the relation between social support and treatment response for PE specifically.
Furthermore, it is unclear if social support improves during treatment as a result of reductions in PTSD symptoms. This bidirectional relation – that increased social support is associated with reduced PTSD symptoms and decreased PTSD symptoms are associated with improved social support – stems from work on two prominent models: social causation and social selection (Kaniasty & Norris, 2008). Social causation suggests that elevated social support is protective against PTSD and is consistent with the stress buffering models of social support (Cohen & Wills, 1985), whereas social selection suggests that elevated PTSD reduces the amount of social support. Studies with military populations have supported the social selection model. In a longitudinal study of combat veterans, elevated PTSD symptoms at the first assessment were associated with reduced social support at the second assessment (King, Taft, King, Hammond, & Stone, 2006). Social support at the first assessment, however, was unrelated to PTSD symptoms at the second assessment. These findings were replicated in a study of combat veterans examining support from veteran and non-veteran peers (Laffaye, Cavella, Drescher, & Rosen, 2008). Support for social causation comes from a study of natural disaster victims. Social support reported 6-months after a natural disaster was associated with fewer PTSD symptoms at 12-month follow-up (Kaniasty & Norris, 2008). A more recent study with sexual assault victims demonstrated some support for the bidirectional nature of this relation (Ullman & Relyea, 2016). Negative social reactions from members of a support network exacerbated PTSD symptoms. The increased PTSD symptoms, in turn, resulted in poorer social support at a later assessment point. Studies with other populations have not shown this bidirectional relation, however, and thus may be limited to victims of sexual assault. No studies to date have examined these relations within the context of treatment.
There are several gaps in the literature with regard to the role of social support during PTSD treatment. The reviewed literature suggests that social support is associated with PTSD treatment response but has yet to evaluate this relation during PE, a well validated treatment for the disorder (Powers et al., 2010). Furthermore, it is unclear if social support improves during treatment and if these improvements are moderated by decreases in PTSD symptoms that occur from treatment. Understanding how social support changes as a result of treatment and how these changes affect PTSD symptoms may account for significant variance in outcomes. To address these questions, the current study evaluated the relation between social support and PTSD treatment response. First, it was hypothesized that reductions in PTSD symptoms during treatment would be moderated by social support during treatment. Second, it was hypothesized that social support would improve during treatment response and that these improvements would be moderated by PTSD symptom reduction. It was also hypothesized that these moderating relations would be found during the follow-up period.
Methods
The present study is a secondary data analysis of a non-inferiority trial on the use of PE via telehealth (Acierno et al., 2017). The primary aim of the parent trial was to determine if PE administered via telehealth was comparable to PE delivered via in-person to treat PTSD resulting from combat exposure in veterans. The results of the parent study suggested that these two modalities were non-inferior – the differences in treatment response across telehealth and in-person treatment were not clinically meaningful. Ten participants were removed from the original sample due to attending fewer than 3 treatment sessions. As a result, a sample of N = 123 was used. All procedures were approved by the local VAMC Research and Development committee as well as the Institutional Review Board at the affiliated university.
Participants
Participants (N = 123) were recruited via referrals from medical staff at a large southeastern Veterans Affairs Medical Center (VAMC) and its affiliated community-based outpatient clinics, as well as self-referrals resulting from flyers, billboards, health fairs, online advertisements, and media announcements. Eligibility was determined by an in-person intake assessment delivered by masters-level clinicians. Combat veterans and military personnel meeting DSM-IV-TR criteria for PTSD per the Clinical-Administered PTSD Scale (CAPS; Blake et al., 1995) using the dichotomous scoring method (diagnosis presence/absent) were eligible. Exclusion criteria included alcohol or substance dependence within the past 6 months and/or an active psychotic disorder (from chart review), and severe suicidal ideation with plan and intent. To maximize the generalizability of results, the presence of other forms of psychopathology (major depressive disorder, panic disorder, and generalized anxiety disorder) and/or use of a psychiatric medication, after 21-day stabilization period, were not a basis for exclusion.
Participants were M = 41.69 (SD = 14.18) years old and predominantly male (95.8%). The majority of the sample was White (59.4%). A substantial portion identified as Black (35.0%). The remaining participants identified as Hispanic (4.9%) and ‘Other’ (0.7%). Written consent was obtained from all participants at their first assessment.
Measures
Clinician Administered PTSD Scale
The CAPS is a clinician-administered structured interview designed to diagnose current and lifetime PTSD (Blake, et al., 1995). The CAPS targets the 17 specific PTSD symptoms from the DSM-IV (APA, 2000) to assess the intensity and frequency of each symptom on a five-point Likert scale. Although a full assessment of past trauma was completed, current PTSD that stemmed from combat exposure was the focus of the symptom assessments and related diagnosis. The internal consistency of the CAPS in the present study was good to excellent (Cronbach’s α’s = .82-.94). Internal consistency across raters was excellent (96% agreement among interviewers).
Structured Clinical Interview for DSM-IV
The SCID-IV is a semi-structured clinician-administered, diagnostic interview designed to assess the DSM-IV diagnostic criteria for Axis I disorders (First, Spitzer, Gibbon, & Williams, 2002). The SCID-IV was used to determine the presence of comorbid mood (depression, mania) and anxiety (panic disorder, generalized anxiety disorder, social phobia, and specific phobia) conditions. Internal consistency across raters was excellent (96% agreement among interviewers).
Medical Outcomes Study Social Support Survey Form (MOSSS).
The MOSSS is a widely used 19-item self-report measure designed to assess social support (Sherbourne & Stewart, 1991). Responses are given on a six point Likert scale ranging from 1–6. Total scores range from 19 to 114 with greater scores indicating greater support. The total score represents an overall social support index and has been shown to be an accurate measure of social support in veteran samples with mental health issues (Brancu et al., 2014; Jakupcak et al., 2011; Kilbourne, McCarthy, Post, Welsh, & Blow, 2007). Internal consistency for the MOSSS subscales at pretreatment and posttreatment were consistently in the excellent range (αs > .95). The internal consistency of the MOSSS in the present study was excellent (Cronbach’s α’s = .91-.97).
PTSD Checklist-Military.
The PCL-M is a 17-item self-report measure designed to assess PTSD symptom severity related to military/combat-related trauma (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). The measure used in the current study mapped onto DSM-IV criteria. Respondents were presented with 17 specific symptoms of PTSD and asked to rate “how much you have been bothered by that problem in the last month” on a 5-point Likert scale, ranging from 1 (not at all) to 5 (extremely). The scale score is sum of all items with a range of 17 to 85. The internal consistency of the PCL-M in the present study was excellent (Cronbach’s α’s = .91-.97).
Procedures
Participants meeting eligibility requirements were block randomized to home-based telehealth and in-person conditions. An initial intake was completed with the pretreatment PCL, CAPS, and MOSSS. The CAPS was administered by a trained research assistant who was supervised by a licensed clinical psychologist. After intake, participants in both conditions received a binder of PE and assessment materials to complete throughout their treatment period (e.g., exposure recording forms, PCL). All participants received PE administered by one of three masters-level therapists, all with experience in conducting exposure-based therapy for PTSD in prior clinical trials. Therapists received weekly supervision from a licensed clinical psychologist who was a certified PE trainer. Each therapist was randomly assigned to provide treatment to participants in both the in-person and telehealth conditions. The main components of PE are available from Foa et al. (2007) and included psychoeducation, situational (in vivo) exposure, and imaginal exposures that involved recounting aloud the most upsetting traumatic memory followed by processing of the imaginal recounting experience. The specific number of sessions for each participant was determined on a case-by-case basis, taking the participant’s progress into account. Participants were initially told that the therapy consisted of 8 – 12 sessions and that most veterans choose to have about 10 sessions but can go up to 12 if needed. The mean number of sessions completed was 8.54 (SD = 3.09, Range = 2–12) with 23.6% of participants receiving the maximum of 12 sessions.
Irrespective of the number of attended sessions, participants completed a posttreatment assessment session that occurred within 1 week of their final treatment session. The PCL-M, CAPS, and MOSSS were administered at this assessment, which served as the “posttreatment” point for the current study. That is, the posttreatment assessment occurred at the same point in treatment for all participants (1-week after their final session). Posttreatment assessments evaluated symptoms for the past month. Follow-up assessments were conducted at 3-months and 6-months after the posttreatment assessment. Completion rates for posttreatment assessments and follow-ups were as follows: Posttreatment: n = 88, 72.1%; 3-month follow-up: n = 64, 52.5%; 6-month follow-up: n = 86, 70.5%.
Data Analytic Plan
The hypotheses were tested using mixed-effect models. A spline model was used, which allows the slope to differ across conceptually different periods of time. For the present study, the treatment and follow-up periods were established as distinct periods as has been established in prior work (Price et al., 2015; Price & Gros, 2014; Rothbaum et al., 2014). In these studies, the rate of change during treatment was greater than during follow-up. Time was structured such that the intercept (γ00; time = 0) correspond to posttreatment, and time was scaled in months such that pretreatment was coded −2, 3-month follow-up coded as 3, and 6-month follow-up coded as 6. The model of longitudinal change takes the form of:
| (1) |
where γ00 corresponds to the posttreatment assessment, γ10 corresponds to change during treatment, and γ20 corresponds to change during follow-up. The remaining terms correspond to random errors and residual variation: u0i corresponds to individual-level variation at posttreatment, u1i corresponds to individual-level variation in change during treatment, and εit corresponds to residual variation. The subscript i corresponds to individuals and the subscript t corresponds to time points.
Preliminary analyses were conducted to evaluate the effect of treatment condition and number of sessions attended on the CAPS, PCL, and MOSSS. These variables were included in Equation 1 by adding the following fixed effects for separate models as indicated by a / : [γ01(Conditioni/Sessionsi); γ11(Txit*Conditioni/ Sessionsi); γ11(Txit*Conditioni/ Sessionsi)]. None of these terms were significant for any outcome variable. Thus, these variables were excluded from subsequent analyses and the sample was collapsed across conditions to increase power.
To evaluate the hypothesis that social support moderated PTSD symptom reduction during treatment and follow-up, the following mixed-effect model was used:
| (2) |
where γ30 corresponds to the relation between the moderator (MOSSS) and outcomes, γ40 corresponds to effect of moderator (MOSSS) scores on change in outcomes during treatment, and γ50 corresponds to the moderator (MOSSS) on change in outcomes during follow-up. The other terms in this equation should be interpreted as they were in equation 1. The same model was used to evaluate the second hypothesis in which PTSD symptoms were the outcome and social support was the moderator. The interaction terms were the product of moderator and the respective slope variable. Moderator scores and the respective time scales were not centered as to preserve the time coding scheme. Missing data was handled with full information maximum likelihood. Analyses were conducted in R version 3.2.
Results
Initial models evaluated change in the PTSD during treatment and follow-up. CAPS and PCL scores decreased during treatment (CAPS: γ10 = −12.42, SE = 0.87, p < .001; PCL: γ10 = −7.67, SE = 0.73, p < .001), but not during follow-up (CAPS: γ20 = 0.26, SE = 0.26, p = .305; PCL: γ20 = 0.35, SE = 0.21, p = .105).
The moderating effect of social support on PTSD symptoms was evaluated first. There was a significant social support x treatment slope interaction (γ40 = −0.20, SE = 0.04, p < .001), but not a significant social support x follow-up slope (γ50 = 0.03, SE = 0.02, p = .073) (Table 2). Similar results were found for the PCL in that there was a significant social support x treatment slope interaction (γ40 = −0.15, SE = 0.03, p < .001). The social support x follow-up slope interaction was significant (γ50 = 0.03, SE = 0.01, p = .021).
Table 2.
Multilevel models evaluating the effect of social support on treatment response for PTSD symptoms during treatment..
| Outcome | Coefficient | SE | p | Pseudo-R2 | |
|---|---|---|---|---|---|
| CAPS (Clinician Rated PTSD) | Intercept γ00 | 72.67 | 5.51 | < .001 | 0.22 |
| Treatment slope γ10 | 1.82 | 3.15 | .564 | ||
| FU slope γ20 | −1.72 | 1.29 | .184 | ||
| Social Support γ30 | − 0.42 | 0.07 | < .001 | ||
| Treatment x Social Support γ40 | − 0.20 | 0.04 | < .001 | ||
| FU x Social Support γ50 | 0.03 | 0.02 | .073 | ||
| PCL (Self-Report PTSD) |
Intercept γ00 | 78.49 | 4.71 | < .001 | 0.27 |
| Treatment slope γ10 | 4.41 | 2.63 | .095 | ||
| FU slope γ20 | −1.61 | 0.98 | .105 | ||
| Social Support γ30 | −0.40 | 0.06 | < .001 | ||
| Treatment x Social Support γ40 | −0.15 | 0.03 | < .001 | ||
| FU x Social Support γ50 | 0.03 | 0.01 | 0.021 |
Note: SE = standard error. MOSSS = Medical Outcomes Social Support Scale. PCL = PTSD symptom Checklist. FU = Follow-Up. N = 122.
The interactions were probed at +/− 1SD of the average MOSSS score across the entire time series. Those with higher MOSSS scores during treatment had a greater change in CAPS (Figure 1) and PCL (Figure 2). The effects of the MOSSS and interaction effects were determined using the Psuedo-R2 (Singer & Willett, 2003), which is the proportional change in the residual variance attributed to the inclusion of the interaction terms. The interaction effects accounted for 21% and 28% of the variance in the CAPS and PCL, respectively. During follow-up, however, those with elevated social support experienced a gradual increase in symptoms. However, this rate of the increase was marginal relative the improvement they experienced during treatment.
Figure 1.
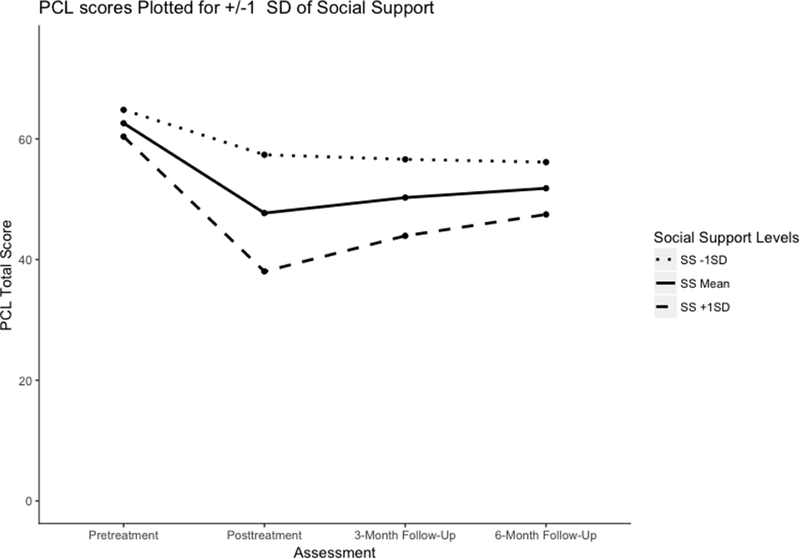
Estimated scores on the PCL for those with social support +/− 1 standard deviation across all assessment points. PCL = PTSD symptom Checklist.
Figure 2.
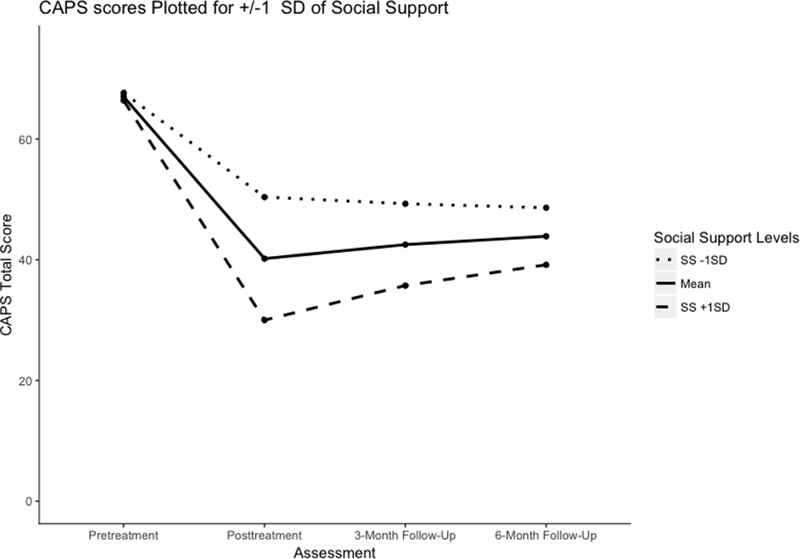
Estimated scores on the CAPS for those with social support +/− 1 standard deviation across all assessment points. CAPS = Clinician Administered PTSD Scale.
The second hypothesis was supported in that social support increased over the course of treatment (γ10 = 3.49, SE = 1.12, p < .001), but remained stable during follow-up (γ20 = −0.02, SE = 0.41, p = .953). However, PTSD symptoms did not moderate these changes as measured by the CAPS (γ40 = 0.10, SE = 0.07, p = 0.190) or PCL (γ50 = 0.04, SE = 0.08, p = 0.636) (Table 3).
Table 3.
Multilevel models evaluating the effect of PTSD symptoms on social support during treatment.
| Moderator | Coefficient | SE | p | Pseudo-R2 | |
|---|---|---|---|---|---|
| - | Intercept γ00 | 81.85 | 2.51 | <.001 | - |
| Treatment slope γ10 | 3.49 | 1.12 | < .001 | ||
| FU slope γ20 | −0.02 | 0.41 | .953 | ||
| CAPS (Clinician Rated PTSD) | Intercept γ00 | 94.85 | 4.19 | <.001 | 0.14 |
| Treatment slope γ10 | −7.65 | 4.71 | .106 | ||
| FU slope γ20 | −1.50 | 0.86 | .084 | ||
| CAPS γ30 | −0.33 | 0.09 | <.001 | ||
| Treatment x CAPS γ40 | 0.10 | 0.07 | .190 | ||
| FU x CAPS γ50 | 0.04 | 0.02 | .069 | ||
| PCL (Self-Report PTSD) |
Intercept γ00 | 105.34 | 5.23 | < .001 | 0.12 |
| Treatment slope γ10 | −2.68 | 4.56 | .557 | ||
| FU slope γ20 | −1.73 | 1.08 | .110 | ||
| PCL γ30 | −0.49 | 0.10 | < .001 | ||
| Treatment x PCL γ40 | 0.04 | 0.08 | .636 | ||
| FU x PCL γ50 | 0.04 | 0.02 | 0.081 |
Note: SE = standard error. MOSSS = Medical Outcomes Social Support Scale. PCL = PTSD symptom Checklist. CAPS = Clinician Administered PTSD Scale. FU = Follow-Up. N = 122.
Discussion
The results of the present study are consistent with prior work that suggested elevated social support during treatment is associated with a greater reduction in PTSD symptoms (Price et al., 2013; Shnaider et al., 2017; Thrasher et al., 2010). The present study builds upon this work in several ways. First, these findings suggest that social support accounts for a meaningful amount of PTSD symptom change during PE. Consistent with a social causation model, social support across treatment moderated the change in PTSD during treatment. Social support also increased during treatment, however this increase was not moderated by PTSD symptoms. These relations were found in a sample of combat veterans and may differ for other types of trauma-exposed populations.
There are several potential mechanisms whereby social support could facilitate response during PE for PTSD. As mentioned previously, support during the course of treatment may help individuals more readily engage with the aspects of the treatment and thus receive greater benefit. Alternatively, consistent with a prior study demonstrating on the role of positive social support with posttraumatic growth (Borja et al., 2006), supportive friends and family may assist patients in processing the meaning of the trauma as it becomes more salient during the course of treatment. Furthermore, in the context of PE, supportive individuals might be helpful in assisting with completion of homework. Since the full protocol consists of twelve sessions, the majority of practice confronting the memory (i.e., imaginal exposure) and reminders of the trauma (i.e., in vivo or situational exposure) occurs outside of sessions. It is possible that supportive friends and family help encourage and remind one to complete homework, and may even accompany or assist patients when completing situational exposures. Finally, it may be that the hope of further improving already-present relationships provides patients with additional motivation to more fully engage with treatment, possibly leading to more robust treatment effects.
Social support increased during the course of treatment, but these increases were unrelated to reductions in PTSD symptoms. Of note, PTSD includes several symptoms that directly relate to interpersonal functioning, such as a sense of emotional detachment from others, increased irritability, and erosions in trust (American Psychiatric Association, 2013; Cias, Young, & Barreira, 2000). By processing the trauma memory during evidence-based psychotherapy for PTSD, patients could potentially experience reductions in social withdrawal. Alternatively, those receiving treatment may draw upon social resources for the in vivo exposures that are part of PE. For example, individuals may ask others to accompany them on exposure exercises, which in turn may improve perceptions of social support. Future work should obtain additional information about the nature of social interactions throughout the treatment and posttreatment period to better understand what may drive this increase in perceived support.
These results have several clinical implications. There are now four published studies that suggest elevated perceived social support during PTSD treatment is associated with improved treatment response. Clinicians should assess an individual’s social support resources at the start of treatment. Doing so may help calibrate expectations for treatment response among the clinician and client. Furthermore, brief interventions to improve interpersonal functioning or social resources may prove beneficial in preparing the individual for treatment. Prior work with victims of childhood maltreatment (Cloitre, Koenen, Cohen, & Han, 2002) and combat veterans (Cloitre, Jackson, & Schmidt, 2016) suggseted that adding social skills training to exposure treatment improves interpersonal functioning as well as reduces PTSD symptoms.
The study had several additional limitations of note. A comparison group was not included, which limits the strength of our conclusions. If social support was associated with symptom improvement in PE, but not in a wait-list or placebo condition, then it would provide experimental evidence regarding the unique role of social support in change during treatment. However, two prior experimental studies have demonstrated that greater social support was related to greater treatment response in those who received active treatment (e.g., cognitive behavioral conjoint therapy, exposure therapy, and cognitive restructuring) as opposed to a no-treatment control (Shnaider et al., 2017; Thrasher et al., 2010). The current study focused on perceived support from the perspective of the individual in treatment. Obtaining information from an individual’s support network may further elucidate how support is associated with treatment and provide additional information as to the directionality of this relation. A comparison of perceived and received support may help determine how best to leverage social support in treatment. That is, it may be more helpful to increase awareness of support that is available (perceived) than attempting to marshal more social resources from the network (received). Support from the therapist in the form of the therapeutic alliance was also not examined. Prior work on non-specific factors have highlighted the importance of the therapeutic alliance with regards to improved treatment response (Cloitre, Chase Stovall-McClough, Miranda, & Chemtob, 2004). Future work should examine the interaction between therapist-based support and external support as it relates to improved outcomes. These analyses should be extended to other forms of treatment as well. Negative social interactions or negative social responses were not included in the current study. Prior work has shown that negative social reactions to a trauma influence PTSD symptoms (Ullman & Filipas, 2001; Ullman & Relyea, 2016) and may also play a role during treatment. The current study used DSM-IV criteria for the diagnosis of PTSD due to the initiation date of the parent trial prior to publication of the DSM 5. The disorder underwent a substantial diagnostic revision in DSM 5, which may have affected the hypothesized relations. Future work should replicate these findings using the new diagnostic criteria. Finally, the current sample was predominately male and had attrition during the follow-up periods. These factors may limit generalizability of the findings to women and the interpretability of the follow-up relations.
Despite these limitations, this study provides a unique contribution to the literature. It is the only study to demonstrate the association of social support with symptom reduction for PE, which is among the strongest PTSD treatment protocols to date (Powers et al., 2010). Overall, the findings highlight an important connection between social support and symptom improvement over the course of PTSD treatment. Future work should evaluate the mechanism by which social support enhances treatment response to determine how best to capitalize on its adaptive effects.
Table 1.
Descriptive statistics for all assessments
| Pretreatment | Posttreatment | 3-Month Follow-Up | 6-Month Follow-Up | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| MOSSS Total Scale | 72.43 | 23.88 | 81.29 | 24.55 | 76.92 | 26.08 | 81.55 | 23.08 |
| CAPS | 66.73 | 13.40 | 40.68 | 22.39 | 39.44 | 19.85 | 43.04 | 20.63 |
| PCL | 62.37 | 12.56 | 46.68 | 19.78 | 47.32 | 16.25 | 49.38 | 18.31 |
Note: MOSSS = Medical Outcomes Social Support Scale. PCL = PTSD symptom Checklist. CAPS = Clinician Administered PTSD Scale. N = 122.
Acknowledgements
This research was supported by the Department of Veterans Affairs Health Services Research and Development grant #HX00152 (PI: Acierno) and by the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina through NIH/NCATS Grant Number UL1 TR001450. Matthew Price, Katherine van Stolk-Cooke, and Alison Legrand are supported by National Institute of Mental Health grant #MH 1K08MH107661–01A (PI: Price). Daniel Gros is supported by the Department of Veterans Affairs Health Services Research and Development grant CX000845.
References
- Acierno R, Gros DF, Ruggiero KJ, Hernandez-Tejada MA, Knapp RG, Lejuez CW, … Tuerk PW (2016). Behavioral Activation and Therapeutic Exposure for Posttraumatic Stress Disorder: A Noninferiority Trial of Treatment Delivered in Person Versus Home-Based Telehealth Depression and Anxiety, 33(5), 415–423. 10.1002/da.22476 [DOI] [PubMed] [Google Scholar]
- Acierno R, Knapp R, Tuerk P, Gilmore AK, Lejuez C, Ruggiero K, Foa EB (2017).> A non-inferiority trial of Prolonged Exposure for posttraumatic stress disorder: In person versus home-based telehealth. Behaviour Research and Therapy, 89, 57–>65. 10.1016/j.brat.2016.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acierno R, Rheingold A, Amstadter A, Kurent J, Amella E, Resnick H, Lejuez C (2011). Behavioral activation and therapeutic exposure for bereavement in older adults. American Journal of Hospice and Palliative Medicine, 1049909111411471 10.1177/1049909111411471 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition: DSM 5. Washington DC: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association, & others. (2000). DSM-IV-TR: Diagnostic and statistical manual of mental disorders, text revision. Washington DC: American Psychiatric Association. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress, 8(1), 75–>90. 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA (1996). Psychometric properties of the PTSD checklist (PCL). Behaviour Research and Therapy, 34(8), 669–>673. 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Borja SE, Callahan JL, Long PJ (2006). Positive and negative adjustment and social support of sexual assault survivors. Journal of Traumatic Stress, 19(6), 905–>914. 10.1002/jts.20169 [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 162(2), 214–>227. 10.1176/appi.ajp.162.2.214 [DOI] [PubMed] [Google Scholar]
- Brancu M, Thompson NL, Beckham JC, Green KT, Calhoun PS, Elbogen EB, Wagner HR (2014). The impact of social support on psychological distress for U.S. Afghanistan/Iraq era veterans with PTSD and other psychiatric diagnoses. Psychiatry Research, 2171–2), 86–>92. 10.1016/j.psychres.2014.02.025 [DOI] [PubMed] [Google Scholar]
- Bryant RA, McFarlane AC, Silove D, O’Donnell ML, Forbes D, Creamer M (2015). The Lingering Impact of Resolved PTSD on Subsequent Functioning. Clinical Psychological Science, 2167702615598756 10.1177/2167702615598756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cias CM, Young R, Barreira P 2000).> Loss Of Trust: Correlates Of The Comorbidity Of Ptsd and Severe Mental Illness. Journal of Personal and Interpersonal Loss, 52–3), 103–>123. 10.1080/10811440008409747 [DOI] [Google Scholar]
- Cloitre M, Chase Stovall-McClough K, Miranda R, Chemtob CM (2004). Therapeutic Alliance, Negative Mood Regulation, and Treatment Outcome in Child Abuse-Related Posttraumatic Stress Disorder. Journal of Consulting and Clinical Psychology, 72 (3), 411–>416. 10.1037/0022-006X.72.3.411 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Jackson CL, Schmidt J (2016). Case Reports: STAIR for Strengthening Social Support and Relationships Among Veterans With Military Sexual Trauma and PTSD. Military Medicine. 10.7205/MILMED-D-15-00209 [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Cohen LR, Han H (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase-based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 705), 1067–>1074. 10.1037/0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 982), 310–>357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW (2002). Structured clinical interview for the DSM-IV-TR Axis 1 Disorders, Research Version, Ptient Edition. New York: Biometrics Research: New York State Psychiatric Institute. [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO (2007). Prolonged exposure therapy for PTSD: emotional processing of traumatic experiences: therapist guide. Oxford: ; New York: Oxford University Press. [Google Scholar]
- Foa EB, Zoellner LA, Feeny NC, Hembree EA, Alvarez-Conrad J (2002). Does imaginal exposure exacerbate PTSD symptoms? Journal of Consulting and Clinical Psychology, 704), 1022–>1028. 10.1037/0022-006X.70.4.1022 [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Hoerster KD, Varra A, Vannoy S, Felker B, Hunt S (2011). Hopelessness and suicidal ideation in Iraq and Afghanistan War Veterans reporting subthreshold and threshold posttraumatic stress disorder. The Journal of Nervous and Mental Disease, 1994), 272–>275. 10.1097/NMD.0b013e3182124604 [DOI] [PubMed] [Google Scholar]
- Kaniasty K, Norris FH (2008). Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress, 213), 274–>281. 10.1002/jts.20334 [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, McCarthy JF, Post EP, Welsh D, Blow FC (2007). Social support among veterans with serious mental illness. Social Psychiatry and Psychiatric Epidemiology, 428), 639–>646. 10.1007/s00127-007-0212-1 [DOI] [PubMed] [Google Scholar]
- King DW, Taft C, King LA, Hammond C, Stone ER (2006). Directionality of the Association Between Social Support and Posttraumatic Stress Disorder: A Longitudinal Investigation1. Journal of Applied Social Psychology, 3612), 2980–>2992. 10.1111/j.0021-9029.2006.00138.x [DOI] [Google Scholar]
- Laffaye C, Cavella S, Drescher K, Rosen C (2008). Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. Journal of Traumatic Stress, 214), 394–>401. 10.1002/jts.20348 [DOI] [PubMed] [Google Scholar]
- Maples-Keller JL, Price M, Rauch S, Gerardi M, Rothbaum BO (in press). Investigating Relationships Between PTSD Symptom Clusters Within Virtual Reality Exposure Therapy for OEF/OIF Veterans. Behavior Therapy. 10.1016/j.beth.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin, 1291), 52–>73. [DOI] [PubMed] [Google Scholar]
- Paul LA, Felton JW, Adams ZW, Welsh K, Miller S, Ruggiero KJ (2015). Mental Health Among Adolescents Exposed to a Tornado: The Influence of Social Support and Its Interactions With Sociodemographic Characteristics and Disaster Exposure. Journal of Traumatic Stress, 283), 232–>239. 10.1002/jts.22012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM (2009). Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety, 268), 745–>751. 10.1002/da.20558 [DOI] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, Foa EB (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 306), 635–>641. 10.1016/j.cpr.2010.04.007 [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF (2014). Examination of prior experience with telehealth and comfort with telehealth technology as a moderator of treatment response for PTSD and depression with veterans. International Journal of Psychiatry in Medicine, 481), 57–>67. [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF, Strachan M, Ruggiero KJ, Acierno R (2013). The role of social support in exposure therapy for Operation Iraqi Freedom/Operation Enduring Freedom veterans: A preliminary investigation. Psychological Trauma: Theory, Research, Practice, and Policy, 51), 93–>100. 10.1037/a0026244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price M, Maples JL, Jovanovic T, Norrholm SD, Heekin M, Rothbaum BO (2015). An Investigation of Outcome Expectancies as a Predictor of Treatment Response for Combat Veterans with Ptsd: Comparison of Clinician, Self-Report, and Biological Measures. Depression and Anxiety, 326), 392–>399. 10.1002/da.22354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum BO, Price M, Jovanovic T, Norrholm SD, Gerardi M, Dunlop B, Ressler KJ (2014). A Randomized, Double-Blind Evaluation of D -Cycloserine or Alprazolam Combined With Virtual Reality Exposure Therapy for Posttraumatic Stress Disorder in Iraq and Afghanistan War Veterans. American Journal of Psychiatry, 1716), 640 10.1176/appi.ajp.2014.13121625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH (2008). Nonresponse and Dropout Rates in Outcome Studies on PTSD: Review and Methodological Considerations. Psychiatry, 712), 134–>168. 10.1521/psyc.2008.71.2.134 [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL (1991). The MOS social support survey. Social Science & Medicine, 326), 705–>714. 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- Shnaider P, Sijercic I, Wanklyn SG, Suvak MK, Monson CM (2017). The Role of Social Support in Cognitive-Behavioral Conjoint Therapy for Posttraumatic Stress Disorder. Behavior Therapy, 483), 285–>294. 10.1016/j.beth.2016.05.003 [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR (2015). Psychotherapy for Military-Related PTSD: A Review of Randomized Clinical Trials. JAMA, 3145), 489 10.1001/jama.2015.8370 [DOI] [PubMed] [Google Scholar]
- Thoits PA (1995). Stress, Coping, and Social Support Processes: Where Are We? What Next? Journal of Health and Social Behavior, 53–>79. 10.2307/2626957 [DOI] [PubMed] [Google Scholar]
- Thrasher S, Power M, Morant N, Marks I, Dalgleish T (2010). Social Support Moderates Outcome in a Randomized Controlled Trial of Exposure Therapy and (or) Cognitive Restructuring for Chronic Posttraumatic Stress Disorder. The Canadian Journal of Psychiatry, 553), 187–>190. 10.1177/070674371005500311 [DOI] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH (2001). Predictors of PTSD Symptom Severity and Social Reactions in Sexual Assault Victims. Journal of Traumatic Stress, 142), 369–>389. 10.1023/A:1011125220522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Relyea M (2016). Social Support, Coping, and Posttraumatic Stress Symptoms in Female Sexual Assault Survivors: A Longitudinal Analysis. Journal of Traumatic Stress, 296), 500–>506. 10.1002/jts.22143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Townsend SM, Filipas HH, Starzynski LL 2007). Structural models of the relations of assault severity, social support, avoidance coping, self-blame, and PTSD among sexual assault survivors. Psychology of Women Quarterly, 311), 23–>37. 10.1111/j.1471-6402.2007.00328.x [DOI] [Google Scholar]


