Abstract
This study examines associations between women’s alcohol intoxication at the time of sexual assault and posttraumatic stress disorder (PTSD) symptoms. Drawing on the dual representation theory (Brewin, Gregory, Lipton, & Burgess, 2010), we hypothesized that intoxication at the time of assault would be positively associated with both overall symptoms of PTSD and PTSD re-experiencing symptoms in particular. A total of 143 community women (ages 18 to 26; 71.3% European American) reporting sexual victimization completed questionnaires assessing severity of coercion involved in the assault, perceived level of intoxication at the time of assault, and current PTSD symptoms. Overall, results suggested that greater alcohol intoxication (but not alcohol use alone) was associated with more severe PTSD symptoms when controlling for severity of coercion. Further, higher levels of victim intoxication at the time of the assault were most predictive of re-experiencing symptoms relative to the other symptom clusters.
Keywords: peritraumatic, substance use, risk factors, sexual victimization, posttraumatic stress
Approximately one in five female sexual assault victims have reported being under the influence of substances at the time of their assault; of these, 83.9% reported using alcohol only (Brecklin & Ullman, 2002). Women who are intoxicated at the time of their assault are more prone to negative sequelae such as self-blame and drinking to cope (Littleton, Grills-Taquechel, & Axsom, 2009). However, it remains unclear whether these women are also at greater risk for posttraumatic stress disorder (PTSD), the most pervasive mental health outcome of sexual assault (Campbell, Dworkin, & Cabral, 2009).
Although diverse theoretical approaches have been used to explain the development of PTSD (Ehlers & Clark, 2000; Foa & Kozak, 1986), the dual representation theory (Brewin, Dalgleish, & Joseph, 1996; Brewin, Gregory, Lipton, & Burgess, 2010) is particularly well suited to explain linkages between peritraumatic drinking and subsequent PTSD symptoms. According to this theory, memory for an event is supported by contextual and sensation-based memory systems. Contextual memory representations (C-reps) are the basis for narrative memory, can be voluntarily retrieved, and are contextually bound. C-reps include the timing, sequence, and location of events. Sensory memory representations (S-reps) include low-level, sensation-based information pertaining to sensory and affective experiences, such as smells, pain, or emotions experienced during the event.
Typical memory encoding involves interconnected and equally salient C-reps and S-reps. This allows for integration of a given memory into one’s broader autobiographical context, thus increasing top-down control over memory retrieval and preventing the event from being re-experienced in the present. However, pathological encoding may occur during traumatic events, resulting in salient and enduring S-reps that are disconnected from corresponding C-reps (Brewin et al., 2010). Without the ability to contextualize sensory memories, individuals are less able to control memory retrieval. As a result, the reactivation of an S-rep (e.g., through reminders) can trigger perceptual re-experiencing of the event without information regarding the encoding context (e.g., flashbacks). When trauma memories are experienced without being placed in the context of the past, trauma reminders can lead to a sense of current threat (Ehlers & Clark, 2000), evoking fear, physiological reactions, and distress.
Though this theory has been the subject of some debate (see Kvavilashvili, 2014), the processes hypothesized by the dual representation theory have been supported in a number of empirical studies (see Brewin, 2014). For example, in a series of experiments using a trauma film paradigm (Holmes, Brewin, & Hennessy, 2004), participants reported less frequent intrusive memories when they had engaged in visuospatial tasks (designed to interfere with sensory memory processes) while watching the film. On the other hand, when participants engaged in verbal tasks (designed to interfere with contextual memory processes), they reported more frequent intrusions. Likewise, participants who modeled clay during a trauma film (designed to interfere with sensory memory processes) reported fewer intrusive memories in the following week (Stuart, Holmes, & Brewin, 2006). Together, these findings support major tenets of the dual representation theory by suggesting that selective impairment of contextual memory encoding exacerbates subsequent re-experiencing symptoms.
The dual representation theory provides a useful framework for generating hypotheses to explain how peritraumatic alcohol intoxication might influence the development of PTSD. Much like a traumatic experience, acute intoxication appears to differentially impact memory processes. Specifically, whereas performance on tasks assessing episodic memory (i.e., intentional recall of the occurrence and context of an event) is negatively affected by intoxication, performance on tasks involving semantic memory (i.e., retrieval of general, concept-based knowledge) is less affected (Söderlund, Parker, Schwartz, & Tulving, 2005). Because alcohol intoxication may selectively impair contextual memories, we propose that peritraumatic alcohol intoxication may intensify re-experiencing symptoms by further increasing the disconnect between C-reps and S-reps. In the case of sexual assault, we expect that greater intoxication at the time of the assault may interfere with recall of the contextual aspects of the incident (e.g., sequence of events), but not memory for sensory and affective details (e.g., smell of cigarettes). As a result of this amplified disconnect between C-reps and S-reps, exposure to cues associated with the assault may reactivate S-reps, triggering intrusive memories devoid of context and resulting in re-experiencing symptoms (e.g., flashbacks following exposure to the smell of cigarettes). In this manner, peritraumatic intoxication may be associated with a greater occurrence of re-experiencing symptoms.
Although re-experiencing symptoms may be most affected by these hypothesized memory processes, peritraumatic intoxication may lead to heightened hyperarousal and avoidance symptoms as well. Consistent with well-known associations among PTSD symptom clusters (Ruggiero, Del Ben, Scotti, & Rabalais, 2003), individuals experiencing more severe re-experiencing symptoms may feel tense and on edge (i.e., hyperaroused) as they anticipate future intrusions. These individuals may also attempt to manage re-experiencing symptoms through avoidance of affective and environmental triggers (Ehlers & Clark, 2000). In turn, such avoidance may maintain re-experiencing symptoms by preventing consolidation of trauma memories.
Findings from studies examining alcohol as a peritraumatic risk factor for PTSD symptoms are mixed. When examining participants exposed to non-interpersonal forms of trauma, some studies find that peritraumatic intoxication is a risk factor for PTSD (Richmond & Kauder, 2000), others suggest it protects against PTSD (Maes, Delmeire, Mylle, & Altamura, 2001; Mellman, Ramos, David, Williams, & Augenstein, 1998), and others find no significant relation between intoxication and PTSD (McFarlane et al., 2009). Adding to these mixed findings, results from alcohol administration studies revealed an inverted “U-shaped” effect (Bisby, Brewin, Leitz, & Curran, 2009; Bisby, King, Brewin, Burgess, & Curran, 2010). Specifically, participants receiving a low dose of alcohol before viewing a trauma film reported more intrusive memories than those in the placebo condition, whereas those in the high dose condition reported similar or fewer intrusive memories. In the context of the dual representation theory, the authors suggest that low doses of alcohol impair contextual memory, whereas high doses impair encoding of both sensory and contextual memory.
Findings of studies examining PTSD symptoms among victims of alcohol-involved and non-alcohol-involved sexual assaults are also mixed, with some cross-sectional studies finding that forcible rape is more predictive of PTSD than substance-facilitated or incapacitated rape (Brown, Testa, & Messman-Moore, 2009, Study 1; Masters et al., 2015; Zinzow et al., 2010, 2012) and others finding no differences in PTSD between victims of alcohol-involved versus non-alcohol-involved assault (Brown et al., 2009, Study 2; Littleton et al., 2009). In longitudinal studies, the use of alcohol prior to a sexual assault has been directly associated with fewer initial PTSD symptoms in general (Peter-Hagene & Ullman, 2016) and re-experiencing symptoms in particular (Kaysen et al., 2010). However, whereas Peter-Hagene and Ullman (2016) found that this association did not change over time, Kaysen and colleagues (2010) found that victims of alcohol-involved assault reported more persistent re-experiencing symptoms over time than victims of non-alcohol-involved assault. Consistent with this notion of persistent symptoms, recent findings among college students suggest that a higher level of subjective intoxication at the time of a sexual assault is associated with more current (but not past) distress (Blayney & Read, 2015) and greater PTSD symptoms (Blayney, Read, & Colder, 2016).
The current study adds to the literature by examining associations between peritraumatic alcohol use and PTSD while addressing several methodological limitations of past studies. First, in contrast to the dichotomous assessment of intoxication in most prior studies, we assessed intoxication both dichotomously (i.e., intoxicated vs. not) and continuously (to examine effects of alcohol in general and dose-dependent effects). Second, whereas previous studies have typically assessed PTSD symptoms in general, women in the present study reported PTSD symptoms specifically related to their sexual assault. Finally, although the severity of coercion experienced during sexual assault may contribute to PTSD (Brown et al., 2009), few studies have examined the unique impact of intoxication on PTSD symptoms beyond the impact of coercion severity.
Based on theory suggesting that selective impairment of contextual memory increases intrusive memories (Brewin et al., 2010), we hypothesized that intoxication status (any vs. none) and degree at the time of the sexual assault would be associated with greater overall PTSD symptoms (Hypothesis 1). We also hypothesized that intoxication would evidence a particularly strong association with PTSD re-experiencing symptoms (relative to avoidance/numbing symptoms and hyperarousal symptoms; Hypothesis 2).
Method
Participants and Procedure
Participants were drawn from a larger study of sexual victimization and emotion dysregulation. This community sample included 491 women from four sites in Mississippi, Nebraska, and Ohio. Institutional Review Boards of participating institutions approved all methods. Women aged 18 to 25, regardless of victimization history, were recruited through flyers, newspaper advertisements, and online advertisements for a study on “women’s life experiences and adjustment.” Participants were informed fully, both verbally and in writing, about the purpose and procedures of the study, and were given an opportunity to ask questions prior to providing written informed consent.
Participants completed online assessments every 4 months for 1 year (at months 0, 4, 8, and 12). The first and third assessments were completed in the laboratory (along with other tasks); the second and fourth assessments (online only) could be completed at home or in the laboratory. Women who reported an experience of sexual assault since the age of 18 at any of the four assessments (n = 270)—and who completed an assessment of PTSD symptoms in reference to the sexual assault (n = 157)—were included. The first assessment at which a participant endorsed a sexual assault meeting these criteria was utilized in the current analysis. Cases with missing data on one or more variables (n = 8) or with inconsistent data on intoxication questions (i.e., any substance use and amount of intoxication; n = 4) were excluded. Given our focus on alcohol intoxication, reports involving victim use of other drugs (but not alcohol) at the time of assault were excluded from analyses (n = 2).
Of the 143 women included in the final sample, 63 (43.8%) reported alcohol use prior to the assault; of these, 19 also reported using drugs (with 18 reporting marijuana use and 4 reporting cocaine or methamphetamine use). Participant age at the time of the included assessment ranged from 18 to 26 (M = 22.00, SD = 2.18); more than half (59.4%) were students. Participants were ethnically diverse (71.3% European American; 28.0% African American; 4.9% Latina) and 21.1% identified as lesbian, bisexual, or questioning.
Measures
Adult sexual assault and alcohol intoxication.
The Modified Sexual Experiences Survey (MSES; Messman-Moore, Walsh, & DiLillo, 2010), an expanded version of the Sexual Experiences Survey (Koss, Gidycz, & Wisiniewski, 1987), was used to assess unwanted sexual activities (i.e., attempted or completed oral-genital contact, sexual intercourse, or other sexual acts involving penetration). At the first assessment, participants reported unwanted sexual experiences since the age of 18; at subsequent assessments, participants reported unwanted sexual experiences since the last assessment. If a participant endorsed more than one assault during an assessment, the experience they identified as the most distressing was used as the index event.
On the MSES, participants were asked whether they were “using alcohol or drugs just before or during the unwanted sexual activity,” and, if so, which substances they consumed. Level of intoxication was assessed with the question: “During and just prior to the unwanted activity, how intoxicated, high, or stoned were you?” Response options were: 0 (Not at all intoxicated), 1 (A little), 2 (Somewhat), 3 (Quite), and 4 (Very intoxicated). Because responses were zero-inflated (55.9% reported no intoxication), a piecewise model for intoxication was used in order to examine the separate effects of any intoxication (i.e., a response of 0 versus 1 or more) and amount of intoxication (if any, centered at 1). Thus, the any intoxication variable represented the use of any alcohol, specifically the difference between no intoxication (=0) and intoxication (=1), whereas linear and quadratic effects of amount of any intoxication were included to distinguish among levels of intoxication.
Additional questions from the MSES asked about the extent to which various coercive tactics were used by the perpetrator, on a scale from 0 (Not at all) to 4 (Very much). The mean score of items corresponding to verbal pressure and physical force was used to represent coercion severity. Time since the index assault was estimated by subtracting age at the time of the assault from participant age at the time of the assessment.
PTSD symptom severity.
The PTSD Checklist-Civilian Version (PCL-C; Weathers, Litz, Herman, Huska, & Keane, 1993) consists of 17 items corresponding to PTSD symptoms on the DSM-IV-TR (American Psychiatric Association, 2000). Participants were instructed to complete the PCL-C in reference to a specific index event (for the purposes of this study, a sexual assault). Three subscales corresponding to the PTSD symptom clusters were computed, including Re-experiencing (5 items), Avoidance/Numbing (7 items), and Hyperarousal (5 items) symptoms. Participants were asked to rate how much they had been bothered by each symptom in the past month on a scale from 1 (Not at all) to 5 (Extremely). For the current analyses, a sum total centered at 0 was used for modeling overall PTSD symptom severity; mean scores were used for cluster subscales. To facilitate comparisons with standard PCL-C total scores, original sum totals ranging from 17 to 85 (i.e., modeled score plus 17) are presented in the descriptive statistics and figure representing PTSD symptom severity. (Model results and coefficients are presented in reference to the sum total centered at 0.) In the present study, alpha coefficients for symptom clusters range from .89 (Avoidance/Numbing and Hyperarousal) to .91 (Re-experiencing).
Prior sexual victimization.
The sexual abuse scale of the Computer Assisted Maltreatment Inventory (CAMI; DiLillo et al., 2010) was used to measure sexual victimization before the age of 18, defined as any sexual experience that was against the participant’s will, involved a close family member, or involved someone 5 or more years older than the participant. Participants were also classified as having experienced prior sexual victimization if they endorsed an unwanted sexual experience since the age of 18 on the MSES that did not meet the criteria for inclusion as the index assault.
Analytic Rationale
To address Hypothesis 1, we examined overall PTSD symptom severity, which was positively skewed (skewness = 0.872, SE = 0.203, p < .001) and included many zero responses (n = 20, 14.0%). Regression approaches assuming a conditionally normal distribution of the dependent variable were therefore not appropriate. To model the observed distribution of PTSD symptom severity, we instead estimated both the presence and severity of PTSD symptoms. Specifically, the first (hurdle) sub-model predicted the presence of any PTSD symptoms dichotomously (any vs. none) using a Bernoulli distribution with a logit link (to keep predicted probabilities of any symptoms bounded between zero and one). The second (count) sub-model predicted severity of PTSD symptoms (for those who endorsed any symptoms) with a zero-truncated negative binomial model with a log link (to keep predicted counts of symptom severity above zero). We compared a series of alternative models for such count outcomes as estimated using maximum likelihood in SAS PROC NLMIXED following Stroup (2012). The best-fitting model was selected based upon Vuong (1989) Tests for non-nested models. Then, the most parsimonious conditional (predictive) model was determined through an iterative process of removing non-significant predictors and assessing for reductions in model fit through likelihood ratio tests. The final combined model can be understood as predicting PTSD symptoms (i.e., presence and severity) using two sub-models.
To address Hypothesis 2, the PTSD symptom clusters were also examined as separate multivariate outcomes. After comparing the fit of normal, lognormal, and gamma distributions for their univariate residuals (Clarke, 2003; Vuong, 1989), a gamma distribution with a log link was determined to be the best fit for each outcome. The multivariate models for the PTSD symptom clusters were estimated using maximum likelihood with a Laplace approximation; the amount of variance explained (R2) was computed by squaring correlations between the outcome values predicted by the model fixed effects and the observed outcome values.
In each model, any intoxication, amount of any intoxication, and amount of any intoxication squared (to consider potential non-linear, quadratic trends) were predictors. To isolate the effects of alcohol intoxication, additional predictors that might independently covary with both intoxication and PTSD symptoms were considered for inclusion as covariates, including coercion severity, prior sexual victimization, other drug use (in addition to alcohol) before the assault, years since the index assault, and data collection site.
Results
Descriptive statistics and intercorrelations are provided in Table 1. Of the 143 women in the current study, 63 (44.1%) reported some level of intoxication at the time of the index sexual assault. Specifically, 14 (9.8%) reported being “a little” intoxicated, 8 (5.6%) “somewhat” intoxicated, 16 (11.2%) “quite” intoxicated, and 25 (17.5%) “very” intoxicated at the time of the assault. Further, 41 (28.7%) participants endorsed clinically significant PTSD symptoms (based on a cut-score of 44; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). A total of 106 participants (74.1%) reported a history of prior sexual victimization.
Table 1.
Descriptive statistics and correlations for predictor and outcome variables (N = 143).
| Mean | SD | Range | Correlations | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||||
| 1. Total PTSD suma | 34.33 | 16.16 | 17-84 | |||||||||
| 2. Mean Re-experiencing | 1.98 | 1.02 | 1-5 | .908** | ||||||||
| 3. Mean Avoidance/Numbing | 2.01 | 0.97 | 1-5 | .954** | .797** | |||||||
| 4. Mean Hyperarousal | 2.07 | 1.09 | 1-4.8 | .929** | .762** | .838** | ||||||
| 5. Any Intoxication | 0.44 | 0.50 | 0-1 | .093 | .030 | .108 | .113 | |||||
| 6. Level of intoxication | 0.80 | 1.20 | 0-3 | .171* | .118 | .201* | .149 | .758** | ||||
| 7. Level of intoxication squared | 2.08 | 3.43 | 0-9 | .211* | .167* | .239** | .171* | .684** | .978** | |||
| 8. Coercion severity | 0.61 | 0.54 | 0-3.3 | .230** | .249** | .217** | .177* | −.365** | −.301** | −.279** | ||
| 9. Prior sexual victimization | 0.74 | 0.44 | 0-1 | .146 | .140 | .161 | .101 | .010 | −.017 | −.010 | .066 | |
| 10. Years since assault | 1.27 | 1.72 | 0-7 | −.043 | .020 | −.066 | −.064 | .083 | .090 | .100 | .069 | −.245** |
Note: p < .01.
p < .05.
SD=Standard Deviation. Although overall intoxication scores ranged from 0 to 4, a piecewise effect was used to represent Any Intoxication (i.e., a response of 0 versus 1 or more) and Level of Intoxication (if any, centered at 1, ranging from 0 to 3). Prior sexual victimization was coded such that 0=No, 1=Yes. The mean can therefore be interpreted as the percent of the sample (74.1%) that endorsed prior sexual victimization. The measure used to assess variables 1-4 was the PCL-C, 5-8 and 10 were assessed with the MSES, and 9 was aggregated from the CAMI and MSES.
Total PTSD sum statistics presented in the table are on the original scale of 17 to 85. For the modeled total PTSD sum score (centered at 0), the mean is 17.33 with a range of 0 to 67.
Overall PTSD Symptoms
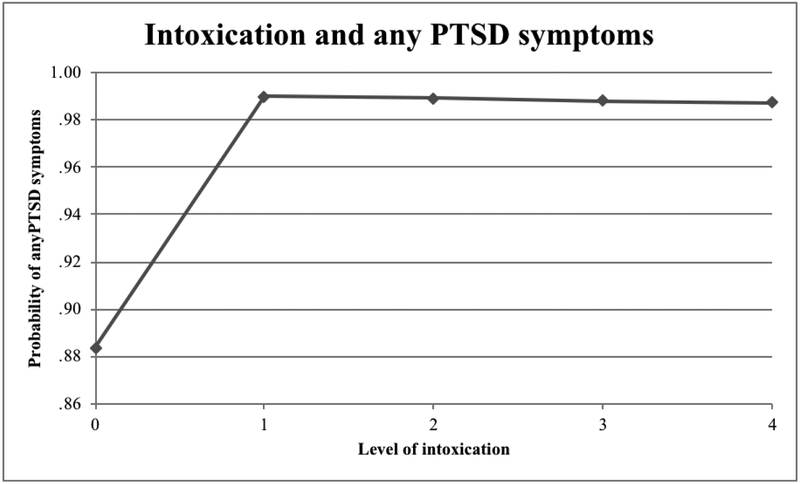
To address Hypothesis 1, total PTSD symptoms were examined using a negative binomial hurdle model; results are shown in Table 2. Prior sexual victimization, years since the assault, other drug use, and site were not significant predictors in either the hurdle or count sub-model and were therefore removed from analyses. The quadratic effect of amount of any intoxication was not a significant contributor to the hurdle sub-model, and so was removed from the hurdle sub-model but retained in the count sub-model. The hurdle sub-model accounted for 15.4% of the variance in differentiating participants who reported zero and any PTSD symptoms. Any intoxication (b = 2.572, p = .044) and coercion severity (b = 2.007, p = .012) significantly predicted the probability of endorsing any PTSD symptoms, whereas amount of intoxication did not (b = −0.082, p = .878). These findings suggest that any intoxication at the time of the assault was associated with a greater probability of reporting any PTSD symptoms even after controlling for the severity of coercion. Figure 1 displays the probability of endorsing any PTSD symptoms for each level of alcohol intoxication when holding coercion severity constant at 1. The only significant differences in predicted probability of PTSD symptoms were between no intoxication (0) and levels 1, 2, 3, and 4 (p < .05), while holding coercion severity constant at 1.
Table 2.
Negative binomial hurdle model estimates for all parameters predicting total PTSD sum score.
| b (SE) | R2 | |
|---|---|---|
| Hurdle sub-model | ||
| Intercept | 0.023 (0.517) | |
| Any intoxication | 2.572 (1.263)* | |
| Level of intoxication | −0.081 (0.528) | |
| Coercion severity | 2.007 (0.793)* | |
| .1536 | ||
|
Count sub-model | ||
| Intercept | 2.655 (0.171)** | |
| Any intoxication | −0.020 (0.252) | |
| Level of any intoxication | ||
| At 1 | −0.676 (0.366) | |
| At 2 | −0.109 (0.154) | |
| At 3 | 0.458 (0.143)** | |
| At 4 | 1.026 (0.353)** | |
| Level of any intoxication squared | 0.284 (0.116)* | |
| Coercion severity | 0.376 (0.157)* | |
| .1166 | ||
| Scale | 0.665 (0.106)** | |
Note: p < .01.
p < .05.
SE = Standard Error. Estimates (b) for the hurdle sub-model predict the logit of no symptoms while estimates for the count sub-model predict the log of the count.
Figure 1.
Mean probability that participants will endorse any PTSD symptoms by level of intoxication, holding coercion severity constant at 1, as predicted by the hurdle sub-model.
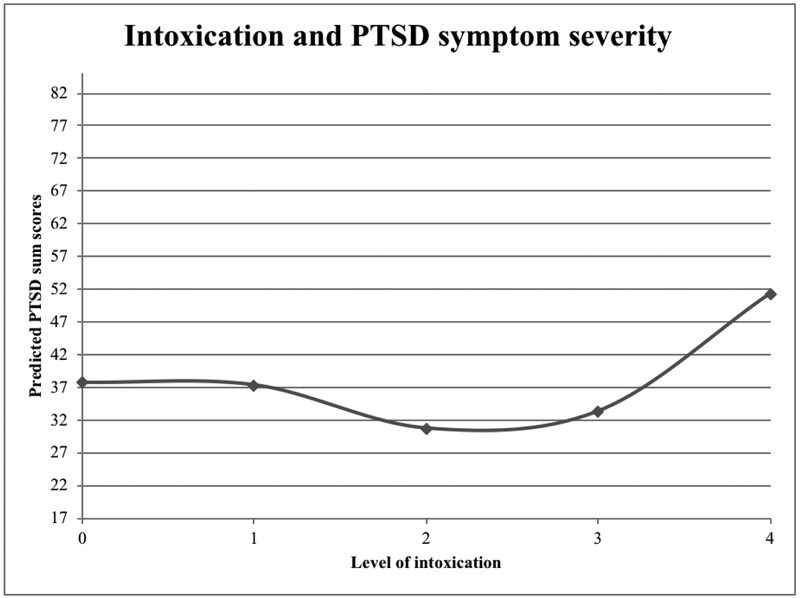
A different pattern was demonstrated in the count sub-model, which accounted for 11.7% of the variance in PTSD symptoms among participants who endorsed any PTSD symptoms. In this sub-model, any intoxication (b = −0.020, p = .938) was not a significant predictor of PTSD symptoms. However, results revealed a significant quadratic effect of intoxication level on PTSD symptoms (if any), such that the linear relation (i.e., slope) between level of any intoxication and PTSD symptoms moved from negative to positive by twice the quadratic coefficient of 0.284 per each additional unit of any intoxication. In other words, the linear effect of intoxication on PTSD symptoms was significantly more positive at higher levels of intoxication. Greater coercion severity was also significantly related to higher PTSD symptoms (b = 0.376, p = .018). Figure 2 displays the predicted sum score of PTSD symptoms (on the original scale of 17 to 85) for each level of intoxication, while holding coercion severity constant at 1. Results from the count sub-model indicate that participants who reported an intoxication score of 4 (n = 25) had significantly greater PTSD symptoms than those who reported an intoxication level of 0, 2, or 3 (ps < .05), while holding coercion severity constant at 1. No other significant differences in predicted PTSD sum scores were found.
Figure 2.
For those who endorsed any PTSD symptoms, the mean of predicted PTSD symptom severity by level of intoxication, holding coercion severity constant at 1, as predicted by the count sub-model. Predicted PTSD sum scores are presented on the original scale of 17 to 85.
Overall, results of the hurdle model for the total PTSD symptom severity score indicate that participants who reported any intoxication at the time of the assault were more likely to report any PTSD symptoms than participants who reported no intoxication. Further, among those participants who reported any intoxication and any PTSD symptoms, there was a significant positive quadratic relationship between level of intoxication and PTSD symptom severity, such that the relation between level of intoxication and PTSD symptom severity moved from negative to positive as the level of intoxication increased (with a significant linear relation between intoxication and PTSD symptoms at high levels of intoxication). Although Figure 2 suggests that predicted PTSD severity may be lower at low to moderate levels of intoxication (levels 1, 2, or 3) when compared to no intoxication (0), these differences were not significant (all p’s > .05). Together, these findings suggest that, when controlling for coercion severity, severe intoxication at the time of a sexual assault appeared to increase the risk for overall PTSD symptoms.
Differences in PTSD Clusters
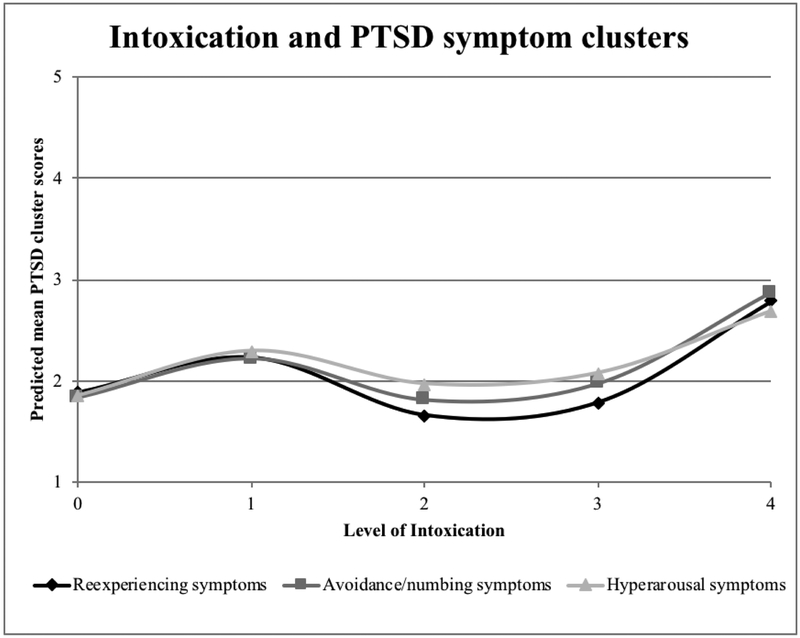
Results of the multivariate analyses to address Hypothesis 2 are presented in Table 3. Prior sexual victimization, years since assault, other drug use, and site were non-significant predictors and were removed from the model. Whether a participant reported any intoxication was not a significant predictor for any of the PTSD symptom clusters, but was retained as part of the piecewise model of intoxication. The multivariate model accounted for 14.6% of the variance in re-experiencing symptoms, 15.5% of the variance in avoidance/numbing symptoms, and 9.6% of the variance in hyperarousal symptoms. Figure 3 displays mean PTSD symptom cluster scores (on a scale from 1 to 5) predicted by this model for each self-reported level of intoxication, when holding coercion severity constant at 1. A nonlinear relationship between intoxication and PTSD symptoms was observed. As evaluated specifically for level of intoxication = 1, greater level of any intoxication linearly predicted fewer re-experiencing symptoms (b = −0.484, p = .010) and did not predict avoidance/numbing symptoms (b = −0.343, p = .068) or hyperarousal symptoms (b = −0.253, p = .177). However, findings revealed significant quadratic effects for both re-experiencing (b = 0.186, p = .002) and avoidance/numbing symptoms (b = 0.143, p = .015), such that the relation between level of any intoxication and both PTSD re-experiencing and avoidance/numbing symptoms moved from negative to positive by twice the quadratic coefficient per additional unit of intoxication. As such, the linear effect of any intoxication on re-experiencing and avoidance/numbing symptoms became more positive and significant at more severe levels of intoxication (Table 3). Although predicted mean PTSD symptom cluster scores appear to be lower at low to moderate levels of intoxication, the only significant negative difference in predicted scores was for re-experiencing symptoms from level of intoxication = 1 to 2 (p = .024).
Table 3.
Parameter estimates for PTSD symptom clusters model with gamma distribution and log link.
| Re-experiencing Symptoms | Avoidance/Numbing | Hyperarousal | |
|---|---|---|---|
| Effect | b (SE) | b (SE) | b (SE) |
| Intercept | 0.318 (0.077)** | 0.342 (0.077)** | 0.362 (0.077)** |
| Any intoxication | 0.169 (0.130) | 0.186 (0.131) | 0.211 (0.131) |
| Level of any intoxication | |||
| At 1 | −0.484 (0.187)* | −0.343 (0.187) | −0.253 (0.187) |
| At 2 | −0.112 (0.080) | −0.058 (0.080) | −0.049 (0.080) |
| At 3a | 0.261 (0.072)** | 0.228 (0.072)** | 0.155 (0.072)* |
| At 4a | 0.633 (0.177)** | 0.513 (0.177)** | 0.359 (0.177)* |
| Level of any intoxication squareda | 0.186 (0.059)** | 0.143 (0.059)* | 0.102 (0.059) |
| Coercion severity | 0.318 (0.075)** | 0.271 (0.075)** | 0.257 (0.074)** |
Note: p < .01.
p < .05.
SE = Standard Error. Estimates are represented in log values.
Difference between Re-experiencing and Hyperarousal is significant, p < .05
Figure 3.
Multivariate prediction of PTSD scores by cluster for each possible self-reported level of intoxication, holding coercion severity constant at 1.
With regard to differences between symptom clusters, the difference in prediction by level of intoxication between re-experiencing and hyperarousal symptoms was significant at level of intoxication = 3 (p = .028) and at level of intoxication = 4 (p = .021). Further, the quadratic effect of level of any intoxication was a significantly better predictor for re-experiencing symptoms than for hyperarousal symptoms (p = .031). Although the prediction by level of any intoxication was stronger for re-experiencing symptoms than avoidance/numbing symptoms, this difference was not statistically significant for the linear effects (p > .05 for all levels of intoxication) or the quadratic effect (p = .265). Overall, alcohol intoxication was somewhat more important in the prediction of re-experiencing than the other PTSD symptoms.
Discussion
Results suggest that victim alcohol intoxication at the time of a sexual assault may play a role in subsequent PTSD symptoms. Consistent with Hypothesis 1, participants who endorsed any peritraumatic intoxication (i.e., any alcohol use prior to the assault) were more likely to endorse any PTSD symptoms related to that assault. However, contrary to expectations, level of intoxication was not a significant predictor of any (vs. no) PTSD symptoms in the hurdle sub-model. Though the hurdle sub-model was statistically indicated, endorsement of any item on the PTSD Checklist (including common problems such as difficulty sleeping, irritability, and difficulty concentrating) may be more indicative of general distress than clinically significant PTSD symptoms subject to impairment in peritraumatic cognitive processes. When examining severity of sub-clinical and clinical PTSD symptoms in the count sub-model, any intoxication was not a significant predictor (contrary to expectations). However, greater levels of intoxication were associated with more severe PTSD symptoms (consistent with expectations). Supporting Hypothesis 2, the quadratic effect of peritraumatic intoxication on PTSD symptoms was particularly strong for re-experiencing symptoms. These effects remained when controlling for coercion severity.
Consistent with prior research (Blayney et al., 2016; Brown et al., 2009, Study 2; Littleton et al., 2009), the current pattern of results suggests that PTSD symptom severity is not substantially influenced by a victim’s use of any (vs. no) alcohol prior to an assault (though see Kaysen et al., 2010 for an exception). However, results suggest that greater levels of intoxication during a sexual assault are associated with more severe PTSD symptoms. Indeed, the only other study known to have examined the degree of intoxication during a sexual assault found that greater levels of intoxication were associated with both more PTSD symptoms (Blayney et al., 2016) and more distress (Blayney & Read, 2015). Together, these results point to the importance of considering intoxication severity as a potential contributor to PTSD symptoms, rather than classifying assault victims simply according to the presence versus absence of any intoxication (e.g., as victims of “alcohol-involved” assault).
Consistent with the dual representation theory, the present findings support the inference that high levels of intoxication may hinder the formation of contextual memories. Without contextual information, memories of the assault may be primarily sensory and, when triggered, experienced as intrusive. Indeed, re-experiencing symptoms evidenced the strongest relation to peritraumatic intoxication. These distressing memories may motivate victims to avoid reminders of the assault, which could hinder recovery (Brewin et al., 2010). More frequent intrusive memories may also foster a sense that the world is unsafe, potentially increasing hyperarousal or avoidance symptoms. Thus, the present findings highlight the possibility that inhibited formation of contextual representations at high levels of intoxication may lead to more severe symptoms of PTSD overall.
Despite these consistencies with the prior literature and theory, our findings differ from those of Bisby and colleagues (2009, 2010), whose lab-based studies found that greater intoxication resulted in fewer intrusive memories following exposure to a trauma film. Differences in study methodology (e.g., assessing symptoms in response to a film clip versus actual assault; controlled laboratory vs. real-world alcohol consumption) and sample (i.e., no traumatic exposure vs. personal sexual assault exposure) likely contributed to these differing results. For example, for at least some individuals, it is likely that the levels of intoxication achieved in the controlled laboratory environment are far lower than those that would be experienced in a real-world setting. Thus, the current study may reflect a broader range of intoxication and, therefore, capture processes not replicable in a lab setting. Further, even in situations involving alcohol-related memory impairment at high levels of intoxication, victims are likely to retain memories from before and after the trauma. Ehlers and colleagues (2002) assert that victims may experience intrusive memories of events retrospectively identified as warning signs (e.g., being handed a drink). Intrusive memories may also involve events associated with the realization or negative interpretation of the assault. Moreover, psychosocial factors related to experiencing a sexual assault while severely intoxicated (e.g., perceived lack of control, passive bystanders) may contribute to increased PTSD symptoms. These factors are difficult to replicate within a laboratory paradigm assessing responses to a trauma film.
Limitations and Future Directions
Methodological limitations of the present study highlight directions for future research. First, the correlational nature of our design precludes conclusions about causation and the exclusive use of self-report measures may introduce shared method bias. Second, although we recruited for a study on “women’s life experiences and adjustment,” it is possible some individuals (e.g., those with the most severe PTSD symptoms) were less likely to participate. Future work with larger samples is needed to determine the generalizability of the current findings to specific subgroups (e.g., sexual minorities, those with more severe PTSD symptoms). Third, although our assessment of any intoxication focused on participants’ recollections of any alcohol use prior to the assault, the assessment of amount of intoxication involved one item focused on participants’ subjective perceptions of intoxication at the time of the assault. Although perceived intoxication can be affected by a variety of factors (e.g., tolerance, expectancies, family history; Morzorati, Ramchandani, Flury, Li, & O’Connor, 2002), it also correlates positively with blood alcohol concentration (Thombs, Olds, & Snyder, 2003)—and our item generally followed expected correlations with other variables. Still, more work is needed to understand this item as a measure of perceived intoxication. Moreover, although post-assault perceptions are relevant to understanding the development of PTSD (Ullman, 1997), future studies should also include objective measures of drinking obtained soon after an assault (e.g., direct measures such as blood alcohol concentration or number of drinks consumed). Finally, future research should examine mechanisms that underlie linkages between alcohol-involved assault and PTSD. Pre-trauma psychological problems, including anxiety and mood disorders, have been associated with increased risk for PTSD (Ozer, Best, Lipsey, & Weiss, 2003) and may also be linked to increased drinking (e.g., Lai, Cleary, Sitharthan, & Hunt, 2015); prospective studies are needed to clarify the unique impact of both pre- and peri-traumatic factors on PTSD symptoms. Experimental studies (e.g., using a trauma film paradigm) could also clarify causal effects and more directly test the dual representation theory. Though we speculate that reactivation of S-reps triggers intrusive memories among victims intoxicated at the time of assault, future research should measure victims’ contextual versus sensory-based intrusions. This work could also examine other potential mediators of the relation of alcohol intoxication to later symptoms, such as self-blame or social support following the assault. Future studies should also examine changes in post-assault PTSD symptoms and their related mechanisms over time.
Conclusion
Current findings suggest that a high (perceived) level of intoxication at the time of a sexual assault is associated with more severe PTSD symptoms, particularly re-experiencing symptoms. These results are consistent with past work (e.g., Brewin et al., 2010; Söderlund et al., 2005) suggesting that a high degree of alcohol intoxication may foster re-experiencing symptoms by selectively impairing high-level contextual memory representations. Given the high co-occurrence of alcohol use and sexual victimization, additional research is needed to further clarify the role of peritraumatic alcohol use in the development of PTSD. Ultimately, this work may inform the development of targeted interventions tailored specifically to victims of alcohol-involved sexual assault.
Acknowledgments
This research was supported by National Institute of Child Health and Human Development Grant R01 HD062226, awarded to the third author (DD).
Contributor Information
Anna E. Jaffe, Department of Psychology, University of Nebraska-Lincoln
Anne L. Steel, Department of Psychology, University of Nebraska-Lincoln
David DiLillo, Department of Psychology, University of Nebraska-Lincoln.
Lesa Hoffman, Schiefelbusch Institute for Life Span Studies, University of Kansas.
Kim L. Gratz, Department of Psychology, University of Toledo
Terri L. Messman-Moore, Department of Psychology, Miami University, Oxford, Ohio
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- Bisby JA, Brewin CR, Leitz JR, & Curran H (2009). Acute effects of alcohol on the development of intrusive memories. Psychopharmacology, 204, 655–666. doi: 10.1007/s00213-009-1496-5 [DOI] [PubMed] [Google Scholar]
- Bisby JA, King JA, Brewin CR, Burgess N, & Curran H (2010). Acute effects of alcohol on intrusive memory development and viewpoint dependence in spatial memory support a dual representation model. Biological Psychiatry, 68, 280–286. doi: 10.1016/j.biopsych.2010.01.010 [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–673. doi: 10.1016/0005-7967(96)00033-2 [DOI] [PubMed] [Google Scholar]
- Blayney JA, & Read JP (2015). Sexual assault characteristics and perceptions of event-related distress. Journal of Interpersonal Violence. Advance online publication. doi: 10.1177/0886260515614560 [DOI] [PubMed] [Google Scholar]
- Blayney JA, Read JP, & Colder C (2016). Role of alcohol in college sexual victimization and postassault adaptation. Psychological Trauma: Theory, Research, Practice, and Policy, 8, 421–430. doi: 10.1037/tra0000100 [DOI] [PubMed] [Google Scholar]
- Brecklin LR & Ullman SE (2002). The roles of victim and offender alcohol use in sexual assaults: Results from the National Violence against Women Survey. Journal of Studies on Alcohol, 63, 57–63. doi: 10.1177/0886260509354584 [DOI] [PubMed] [Google Scholar]
- Brewin CR (2014). Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin, 140, 69–97. doi: 10.1037/a0033722 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Dalgleish T, & Joseph S (1996). A dual representation theory of posttraumatic stress disorder. Psychological Review, 103, 670–686. doi: 10.1037/0033-295X.103.4.670 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Gregory JD, Lipton M, & Burgess N (2010). Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review, 117, 210–232. doi: 10.1037/a0018113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown AL, Testa M, & Messman-Moore TL (2009). Psychological consequences of sexual victimization resulting from force, incapacitation, or verbal coercion. Violence Against Women, 15, 898–919. doi: 10.1177/1077801209335491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell R, Dworkin E, & Cabral G (2009). An ecological model of the impact of sexual assault on women’s mental health. Trauma, Violence, & Abuse, 10, 225–246. doi: 10.1177/1524838009334456 [DOI] [PubMed] [Google Scholar]
- Clarke KA (2003). Nonparametric model discrimination in international relations. Journal of Conflict Resolution, 47, 72–93. doi: 10.1177/0022002702239512 [DOI] [Google Scholar]
- DiLillo D, Hayes-Skelton SA, Fortier MA, Perry AR, Evans SE, Messman-Moore TL, Fauchier A (2010). Development and initial psychometric properties of the Computer Assisted Maltreatment Inventory (CAMI): A comprehensive self-report measure of child maltreatment history. Child Abuse and Neglect, 34, 305–317. doi: 10.1016/j.chiabu.2009.09.015 [DOI] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. doi: 10.1016/S0005-7967(99)00123–0 [DOI] [PubMed] [Google Scholar]
- Ehlers A, Hackmann A, Steil R, Clohessy S, Wenninger K, & Winter H (2002). The nature of intrusive memories after trauma: The warning signal hypothesis. Behaviour Research and Therapy, 40, 995–1002. doi: 10.1016/S0005-7967(01)00077–8 [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. doi: 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Holmes EA, Brewin CR, & Hennessy RG (2004). Trauma films, information processing, and intrusive memory development. Journal of Experimental Psychology: General, 133, 3–22. doi: 10.1037/0096-3445.133.1.3 [DOI] [PubMed] [Google Scholar]
- Kaysen DL, Lindgren KP, Lee CM, Lewis MA, Fossos N, & Atkins DC (2010). Alcohol-involved assault and the course of PTSD in female crime victims. Journal of Traumatic Stress, 23, 523–527. doi: 10.1002/jts.20542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Gidycz CA, & Wisiniewski N (1987). The scope of rape: Incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. Journal of Consulting and Clinical Psychology, 55, 162–170. doi: 10.1037/0022-006X.55.2.162 [DOI] [PubMed] [Google Scholar]
- Kvavilashvili L (2014). Solving the mystery of intrusive flashbacks in posttraumatic stress disorder: Comment on Brewin (2014). Psychological Bulletin, 140, 98–104. doi: 10.1037/a0034677 [DOI] [PubMed] [Google Scholar]
- Lai HX, Cleary M, Sitharthan T, & Hunt GE (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. doi: 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Littleton H, Grills-Taquechel A, & Axsom D (2009). Impaired and incapacitated rape victims: Assault characteristics and post-assault experiences. Violence and Victims, 24, 439–457. doi: 10.1891/0886-6708.24.4.439 [DOI] [PubMed] [Google Scholar]
- Maes M, Delmeire L, Mylle J, & Altamura C (2001). Risk and preventive factors of post-traumatic stress disorder (PTSD): Alcohol consumption and intoxication prior to a traumatic event diminishes the relative risk to develop PTSD in response to that trauma. Journal of Affective Disorders, 63, 113–121. doi: 10.1016/S0165-0327(00)00173-7 [DOI] [PubMed] [Google Scholar]
- Masters NT, Stappenbeck CA, Kaysen D, Kajumulo KF, Davis KC, George WH, . . . Heiman JR (2015). A person-centered approach to examining heterogeneity and subgroups among survivors of sexual assault. Journal of Abnormal Psychology, 124, 685–696. doi: 10.1037/abn0000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, Browne DD, Bryant RA, O’Donnell MM, Silove DD, Creamer MM, & Horsley KK (2009). A longitudinal analysis of alcohol consumption and the risk of posttraumatic symptoms. Journal of Affective Disorders, 118, 166–172. doi: 10.1016/j.jad.2009.01.017 [DOI] [PubMed] [Google Scholar]
- Mellman TA, Ramos J, David D, Williams L, & Augenstein JS (1998). Possible inhibition of early PTSD symptoms by alcohol intoxication. Depression and Anxiety, 7, 145. doi: [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Walsh K, & DiLillo D (2010). Emotion dysregulation and risky sexual behavior in revictimization. Child Abuse and Neglect, 34, 967–976. doi: 10.1016/j.chiabu.2010.06.004 [DOI] [PubMed] [Google Scholar]
- Morzorati SL, Ramchandani VA, Flury L, Li T, & O’Connor S (2002). Self-reported subjective perception of intoxication reflects family history of alcoholism when breath alcohol levels are constant. Alcoholism: Clinical and Experimental Research, 26, 1299–1306. doi: 10.1097/00000374-200208000-00024 [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. doi: 10.1037/0033-2909.129.1.52 [DOI] [PubMed] [Google Scholar]
- Peter-Hagene LC & Ullman SE (2016). Longitudinal effects of sexual assault victims’ drinking and self-blame on posttraumatic stress disorder. Journal of Interpersonal Violence. Advance online publication. doi: 10.1177/0886260516636394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond TS & Kauder D (2000). Predictors of psychological distress following serious injury. Journal of Traumatic Stress, 13, 681–692. doi: 10.1023/A:1007866318207 [DOI] [PubMed] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, & Rabalais AE (2003). Psychometric properties of the PTSD Checklist—Civilian Version. Journal of Traumatic Stress, 16, 495–502. doi: 10.1023/A:1025714729117 [DOI] [PubMed] [Google Scholar]
- Söderlund H, Parker ES, Schwartz BL, & Tulving E (2005). Memory encoding and retrieval on the ascending and descending limbs of the blood alcohol concentration curve. Psychopharmacology, 182, 305–317. doi: 10.1007/s00213-005-0096-2 [DOI] [PubMed] [Google Scholar]
- Stroup WW (2012). Generalized linear mixed models: Modern concepts, methods and applications. Boca Raton, FL: CRC Press. [Google Scholar]
- Stuart AP, Holmes EA, & Brewin CR (2006). The influence of a visuospatial grounding task on intrusive images of a traumatic film. Behaviour Research and Therapy, 44, 611–619. doi: 10.1016/j.brat.2005.04.004 [DOI] [PubMed] [Google Scholar]
- Thombs DL, Olds R, & Snyder BM (2003). Field assessment of BAC data to study late-night college drinking. Journal of Studies on Alcohol, 64, 322–330. doi: 10.15288/jsa.2003.64.322 [DOI] [PubMed] [Google Scholar]
- Ullman SE (1997). Attributions, world assumptions, and recovery from sexual assault. Journal of Child Sexual Abuse, 6, 1–19. doi: 10.1300/J070v06n01_01 [DOI] [Google Scholar]
- Vuong QH (1989). Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica, 57, 307–333. doi: 10.2307/1912557 [DOI] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, & Keane TM (1993). The PTSD Checklist: Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies, San Antonio, TX. [Google Scholar]
- Zinzow HM, Resnick HS, Amstadter AB, McCauley JL, Ruggiero KJ, & Kilpatrick DG (2010). Drug- or alcohol-facilitated, incapacitated, and forcible rape in relationship to mental health among a national sample of women. Journal of Interpersonal Violence, 25, 2217–2236. doi: 10.1177/0886260509354887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley JL, Amstadter AB, Ruggiero KJ, & Kilpatrick DG (2012). Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a national survey of women. Social Psychiatry and Psychiatric Epidemiology, 47, 893–902. doi: 10.1007/s00127-011-0397-1 [DOI] [PMC free article] [PubMed] [Google Scholar]