Abstract
We aimed to investigate the molecular epidemic characteristics and viral transmission patterns of HIV-1 in a typical labor export area, Guangyuan city, China. Based on conducting phylogenetic trees and molecular transmission networks, a phylogenetic analysis was performed on HIV-1 pol sequences obtained from 211 migrant-history workers, 83 non-migrant-history individuals, and 21 migrant-history unknown individuals between January, 2012 and February, 2017 in Guangyuan city. Phylogenetic analysis revealed that CRF07_BC (48.3%, n = 152) and CRF01_AE (33.3%, n = 105) were the dominant strains in Guangyuan city, and circulated by multiple lineages with various epidemic characteristics. Geographic network analysis showed that Guangyuan city-related sequences with 20.3% CRF07_BC and 28.3% CRF01_AE were linked to that of other provinces, compared to that with 1.7% CRF07_BC and 5.0% CRF01_AE in cities of Sichuan. Molecular transmission network analysis further illustrated that migrant-history workers linked more sequences from other provinces than non-migrant-history individuals in both CRF07_BC (29.3% versus 0.0%, P = 0.013) and CRF01_AE (40.5% versus 10.0%, P = 0.001) networks. Our results highlighted that migrant-history workers in recent year played a vital role in fueling HIV-1 epidemic in Guangyuan city. Molecular transmission network analysis could be a useful approach for disclosing the transmission mechanism of HIV, which should be used in prevention and intervention efforts.
Introduction
By the end of December 2017, approximately 758,610 people were living with HIV-1 in China, with an estimated 321,233 cases of AIDS. Among the 134,512 newly diagnosed HIV-1 infections in 2017, 69.4% was attributed to heterosexual and 25.3% to homosexual transmission1. One of the current challenges was that China faced the rapid increase of HIV-1 prevalence among floating population and lacking effective intervention strategies for this group2,3. With the rapid urbanization of China, outgoing migrant-workers had become the main component of the floating population in China, who worked outside the place where the household registrations were located4. The migrant-workers accounting for a large proportion of HIV-1 epidemic in China had caused the diversity of circulating HIV-1 and could further local fuel epidemics5,6. Although several molecular epidemiological investigations conducted in Shanghai, Beijing, Shenzhen, and others indicated that migrant-workers had a significant influence on the HIV-1 epidemics in coastal or metropolis2,7,8, barely researches focused on the condition of rural areas where export labors.
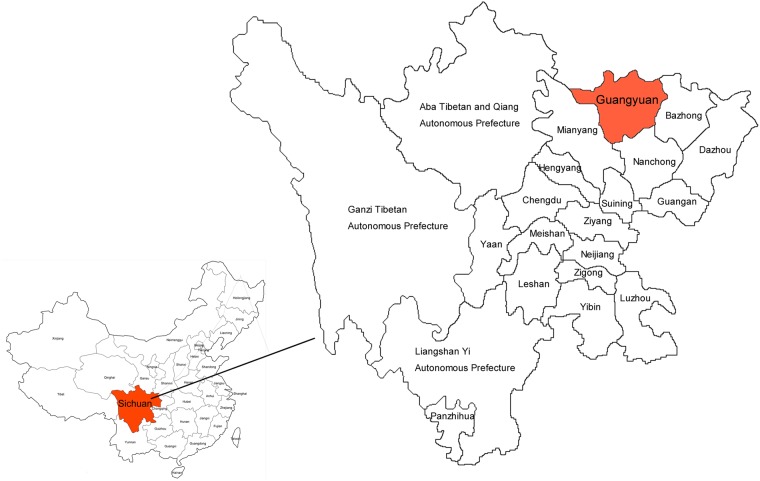
The newly diagnosed cases of HIV-1 in Sichuan province ranked first in China in 2017, and the prevalence of HIV-1 varied widely in regions1. The presence of relatively poor and developing towns and counties had made Sichuan become an important labor-exporting province, with a rapid increase in the prevalence of HIV-1. Guangyuan city, located in northern Sichuan province in western China (Fig. 1), was a mountainous agricultural city with 3.05 million registered populations currently. It was also renowned for its large output of labors in Sichuan. Every year, approximately one million migrant-workers were far away from their homes to seek better employment opportunities, including 21% inside and 54% outside their home province. Above 50% of them had become major migrant labors in Yangtze (mainly including Jiangsu and Shanghai), Zhujiang River delta areas (mainly located in the southeast of Guangdong), and the Bohai Rim (mainly including Beijing and Tianjin)9,10. Since the first HIV-1 case was identified in 1996 in Guangyuan city, the cumulative number of reported HIV-1-infected persons had reached 978 in 2017 (from a report of Guanyuan Municipal Center for Disease Control and Prevention[CDC]). In recent six years, the number of newly diagnosed HIV-1 infections increased from 81 in 2012 to 196 in 2017, showing a serious situation in HIV-1 prevalence. Therefore, we characterized HIV-1 genetic diversity and transmission network in this labor-exporting representative city, Guangyuan city, and tried to explore a possible mechanism for controlling the spread of HIV-1 in this kind of areas.
Figure 1.
The geographical location of Guangyuan in China.
Methods
Study participants
From all local voluntary counseling and testing sites (VCT), sentinel surveillance sites, and medical institutions, a total of 651 HIV-1 patients were newly diagnosed between January 1, 2012 and February 28, 2017 in Guangyuan city. Among them, 66.7% (434) were recruited by the staffs of CDC for participating in the study within the first year after HIV diagnosis. The socio-demographic characteristic indicators included age, gender, level of education, marital status, and risk group were collected by the staffs of CDC simultaneously. All individuals read the content of the study and signed written informed consent. The other individuals could not be recruited for loss of following up (26, 4.0%) or refusal to participate (191,29.3%).
Sequence data collection
A total of 10 mL whole blood samples were collected from the 434 studied participants. None of the individuals was exposed to antiretroviral treatment (ART) at the time of blood specimen collection. Plasma was separated from the whole blood within two hours after collection and stored at −80 °C until use. Blood plasma samples were subjected to viral RNA extraction and cDNA synthesis as previously described11. HIV-1 pol sequences (protease 1–99 and reverse transcriptase 1–250 amino acids) was amplified and sequenced. Eventually, a total of 315 HIV-1 pol sequences covering 1,060 base pairs (HXB2: 2,253–3,312) were successfully obtained. The sampling rate of all the diagnosed patients in Guangyuan city was 48.4% (315/651). (Supplementary Material 1).
Migration condition data collection
The 315 individuals with pol sequences were further conducted a questionnaire survey after sequence data collection. Migration condition data were collected through face-to-face or telephone interviews conducted by the staffs of CDC. These indicators included whether the subjects had gone out as migrant worker before diagnosed, age of the first going out as migrant worker, occupation of going out as migrant worker, and place of migrant working. 294 questionnaires were collected.
Identification of HIV-1 subtypes and CRFs
The HIV-1 pol sequences of studied samples were aligned with reference sequences of subtypes and circulating recombinant forms (CRFs) (Los Alamos HIV sequence database [LANL], http://www.hiv.lanl.gov/) using the Mega version 7.0 with minor manual adjustments. FastTree 2.3 was used to construct an approximately-maximum-likelihood phylogenetic tree (ML tree) using the GTR + G + I nucleotide substitution model12. The phylogenetic tree’s reliability was determined with local support values based on the Shimodaira-Hasegawa (SH) test13 and presented using FigTree v1.3.1 (http://beast.bio.ed.ac.uk).
Identification of HIV-1 epidemic lineages
For further analysis of HIV-1 epidemic lineages of predominant variants circulating in Guangyuan city, a BLAST-based search tool (https://www.hiv.lanl.gov/content/sequence/BASIC_BLAST/basic_blast.html) was used to search against the closely related sequences from locals and nationwide in Sichuan province CDC drug resistance database and LANL database. Two sets of databases, databaseCRF07_BC with 664 CRF07_BC pol sequences and databaseCRF01_AE with 584 CRF01_AE pol sequences were built for both phylogenetic and molecular transmission network analyses. A monophyletic group in ML phylogenetic tree(built as mentioned above) with bootstrap support ≥0.9 was considered as an epidemic lineage.
Analysis of HIV-1 molecular transmission network
The flow chart of transmission network analysis included four steps: construction of phylogenetic tree, extraction of transmission cluster, identification of minimum patristic genetic distance and visualization of the network3. We used Cluster Picker14 to extract transmission clusters from the phylogenetic tree, with the intra-cluster maximum pairwise distance <3.0% nucleotide substitutions per site and bootstrap support value ≥95%. The patristic genetic distances of all sequences within the available clusters were calculated in Patristic software (http://www.bioinformatics.org/patristic/manual.html) (Supplementary Material 2). Among all distances, one that minimizes the sum of edge weights (patristic genetic distances) was selected to define the linkages within a cluster3. Lastly, the network data were visualized and analyzed using the network software Cytoscape 3.515.
Statistical analysis
Chi-square test was used to calculate the distributions of demographic information between CRF01_AE and CRF07_BC, and compare the difference of linkages between migrant-history workers and non-migrant-history individuals in transmission networks. A p-value less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS v.20.0 software (IBM Company, New York, USA).
Ethics statement
The study protocol was reviewed and approved by the Institutional Review Board at the Human Medical Research Ethics Committee of the Sichuan CDC. The objectives and the procedure of the study, and potential risks and benefits of participating in the study were given to potential participants during the recruitment of study subjects. Verbal and written consent procedures were given to the study participants and they had the right to discontinue the survey at any time. All research methods in this study were carried out by the approved guidelines.
Results
The mean age of the 315 participants was 39.4 ± 14.0 years (range 18–78) and male-to-female ratio was 3.5:1. Of these, 132 were single (41.9%), and 182 (57.8%) received primary education or below. The transmission routes of these subjects included 141 (44.8%) male heterosexuals, 86 (27.3%) men who have sex with men (MSM), 65 (20.6%) female heterosexuals, and 23 (7.3%) other transmission routes. The median CD4+ T cell count was 272.0 (IQR: 138.3~377.5) cells/μl (Table 1).
Table 1.
Socio-demographic characteristics for subjects from Guangyuan.
| Demographic characteristics | Number (%) |
|---|---|
| Age (years) | |
| ≤30 | 99 (31.4) |
| 31–40 | 82 (26.0) |
| 41–50 | 65 (20.7) |
| 51–60 | 36 (11.4) |
| ≥61 | 33 (10.5) |
| Sex | |
| Male | 245 (77.8) |
| Female | 70 (22.2) |
| Marital Status | |
| Single | 132 (41.9) |
| Married | 162 (51.4) |
| Unknown | 21 (6.7) |
| Years of Education | |
| 0–6 | 56 (17.8) |
| 7–9 | 126 (40.0) |
| ≥10 | 114 (36.2) |
| Unknown | 19 (6.0) |
| Risk group a | |
| M-HET | 141 (44.8) |
| F-HET | 65 (20.6) |
| MSM | 86 (27.3) |
| PWID/SU | 23 (7.3) |
| Sampling year | |
| 2012 | 49 (15.6) |
| 2013 | 49 (15.6) |
| 2014 | 79 (25.1) |
| 2015 | 66 (20.9) |
| 2016 | 54 (17.1) |
| 2017 | 18 (5.7) |
| CD4+ T cell count (cells/μl) | |
| <200 | 103 (32.7) |
| 200–349 | 107 (34.0) |
| 350–500 | 65 (20.6) |
| ≥500 | 35 (11.1) |
| Unknown | 5 (1.6) |
| Gone out as migrant worker before diagnosed b | |
| Yes | 211 (67.0) |
| No | 83 (26.3) |
| Unknown | 21 (6.7) |
| Age of the first going out as migrant worker (years) c | |
| ≤20 | 63 (29.8) |
| 21–30 | 48 (22.8) |
| 31–40 | 19 (9.0) |
| ≥40 | 21 (9.9) |
| Unknown | 60 (28.5) |
| Place of migrant working c | |
| Inside Guangyuan but outside the domicile | 6 (2.8) |
| Inside the home province but outside Guangyuan | 33 (15.7) |
| Outside the home province | 115 (54.5) |
| Unknown | 57 (27.0) |
| Occupation of going out as migrant worker c | |
| Worker | 78 (37.0) |
| Waiter | 33 (15.6) |
| Company employee | 16 (7.6) |
| Salesman | 14 (6.6) |
| Driver | 4 (1.9) |
| Others | 4 (1.9) |
| Unknown | 62 (29.4) |
aM-HET, male heterosexuals; F-HET, female heterosexuals; MSM, men who have sex with men; PWID, persons who inject drugs; SU, sexual transmission, unspecified type.
bThe time of going out as migrant worker above 30 days before diagnosed.
cThe total number was 211.
High proportion of the migration in Guangyuan city
A total of 67.0% participants reported that they had the experience of being migrant workers before diagnosed, and the mean age of the first going out as migrant workers was 26.9 ± 11.0 years (rang 15.0–70.0). Most of the subjects who ever went out as migrant workers (migrant-history workers) were outside the home province (54.5%), whereas 15.7% and 2.8% stated “inside the home province but outside Guangyuan city” and “inside Guangyuan city but outside the domicile”. The main occupation of these migrant-history workers was worker (37.0%), followed by waiter (15.6%), company employee (7.6%), salesman (6.6%), driver (1.9%), and others (1.9%) (Table 1).
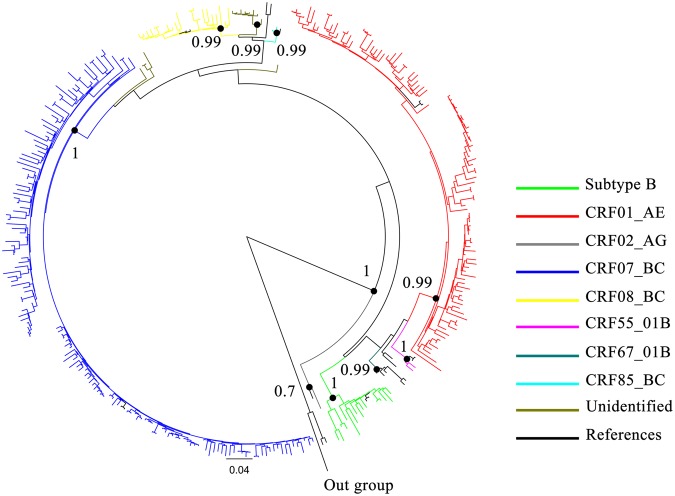
Extensive diversity of HIV-1 subtypes and CRFs in Guangyuan city
Phylogenetic analysis based on 315 pol sequences revealed the presence of one subtype and seven CRFs in Guangyuan city (Fig. 2). Two predominant strains were found to be CRF07_BC (48.3%, n = 152) and CRF01_AE (33.3%, n = 105), followed by CRF08_BC (7.0%, n = 22), subtype B (5.1%, n = 16), CRF55_01B (0.6%, n = 2), CRF85_BC (0.6%, n = 2), CRF02_AG (0.3%, n = 1) and CRF67_01B (0.3%, n = 1). In addition, unique recombinant forms (URFs) were responsible for 4.4% (n = 14) infections.
Figure 2.
Phylogenetic analysis of pol sequences from Guangyuan. The phylogenetic tree was constructed using the approximately-maximum-likelihood method based on the pol region (HXB2: 2, 253 to 3, 312 nt) in FastTree 2.3. The nucleotide substitution mode was GTR + G + I. The subtypes and circulating recombinant forms are marked in different colors. The bootstrap valueswere indicated at relevant nodes. HIV-1 group O was chosen as an out-group in the rooted tree. The reference sequences were from the Los Alamos HIV sequence database (http://hiv-web.lanl.gov/content/index).
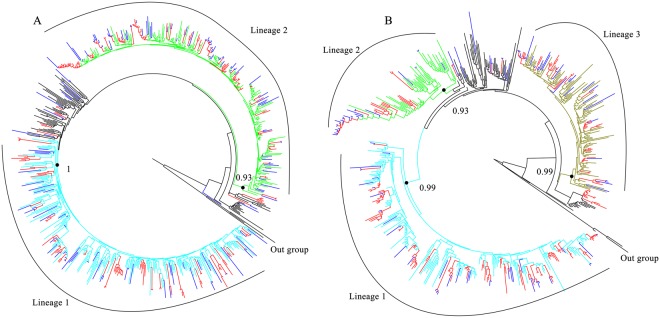
Complicated epidemic characteristics of CRF07_BC and CRF01_AE
When compared with the demographic information between CRF07_BC and CRF01_AE infections, we found that CRF07_BC infections had a higher proportion of MSM (32.9% versus 23.8%), lower age (36.2 ± 13.3 years versus 42.8 ± 13.8 years), and higher of CD4+ T cell count (306.0, IQR: 201.0~402.0 cells/μl versus 254.0, IQR: 77.5~378.5 cells/μl) (Table 2). Phylogenetic analysis evidently identified two major distinct lineages (lineage 1–2) of CRF07_BC (Fig. 3A), involving in 90.1% (137/152) of Guangyuan city-related sequences. Three major distinct lineages (lineage 1–3) of CRF01_AE were identified (Fig. 3B), involving in 90.5% (95/105) Guangyuan city-related sequences. Notably, each lineage presented various epidemic characteristics implying a complexity of HIV-1 transmission among the subjects who ever went out as migrant workers in Guangyuan city (Supplementary Material 3).
Table 2.
Distribution of the demographic information in various subtypes.
| Variable | CRF07_BC n = 152 (%) | CRF01_AE n = 105 (%) | P |
|---|---|---|---|
| Sex | 0.938 | ||
| Male | 121 (79.6) | 84 (80.0) | |
| Female | 31 (20.4) | 21 (20.0) | |
| Risk group a | 0.032 | ||
| M-HET | 57 (37.5) | 54 (51.4) | |
| F-HET | 26 (17.1) | 21 (20.0) | |
| MSM | 50 (32.9) | 25 (23.8) | |
| PWID/SU | 19 (12.5) | 5 (4.8) | |
| Age ( ± s, years) | 36.2 ± 13.3 | 42.8±13.8 | <0.001 |
| Marital Status | 0.771 | ||
| Singlehood | 66 (43.4) | 45 (42.9) | |
| Married | 74 (48.7) | 54 (51.4) | |
| Unknown | 12 (7.9) | 6 (5.7) | |
| Years of Education | 0.561 | ||
| 0–9 | 81 (53.3) | 62 (59.0) | |
| ≥10 | 60 (39.5) | 38 (36.2) | |
| Unknown | 11 (7.2) | 5 (4.8) | |
| CD4+ T cell count (Median and IQR, cells/μl) | 306.0 (201.0~402.0) | 254.0 (77.5~378.5) | 0.019 |
| Gone out as migrant worker before diagnosed b | 0.667 | ||
| Yes | 103 (67.8) | 67 (63.8) | |
| No | 40 (26.3) | 29 (27.6) | |
| Unknown | 9 (5.9) | 9 (8.6) |
aM-HET, male heterosexuals; F-HET, female heterosexuals; MSM, men who have sex with men; PWID, persons who inject drugs; SU, sexual transmission, unspecified type.
bThe time of going out as migrant worker above 90 days before diagnosed.
Figure 3.
Phylogenetic trees of sequences with CRF07_BC (A) and CRF01_AE (B) infection. The phylogenetic tree was constructed using the approximately-maximum-likelihood method based on the pol region (HXB2: 2, 253 to 3, 312 nt) in FastTree 2.3. The nucleotide substitution mode was GTR + G + I. Bootstrap values ≥0.9 were used to identify lineages and were indicated at all relevant nodes. Genetic transmission clusters were defined by node support thresholds ≥95% and intra-cluster maximum pairwise genetic distances <3.0% nucleotide substitutions per site. Transmission clusters were depicted in red. Blue branches represented the sequences from Guangyuan. HIV-1 subtype J (A) and C (B) were chosen as an out-group in the rooted tree.
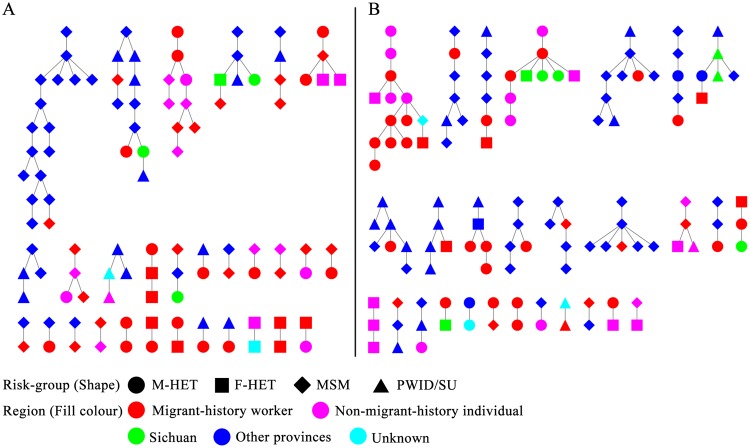
Identification of molecular transmission networks of HIV-1 in Guangyuan city
We focused on observing two major transmission networks, CRF07_BC and CRF01_AE. A total of 75 transmission clusters in the CRF07_BC networks were detected based on databaseCRF07_BC, where 59 Guangyuan city sequences were distributed in 29 Guangyuan city-related clusters (Fig. 4A). The clusters consisted of different sizes covering from 2 to 17 individuals, including 18 (62.1%), 7 (24.1%) and 4 (13.5%) for cluster size 2, 3–5 and >5 individuals, respectively. Of note, based on databaseCRF01_AE, a higher percentage of numbers in Guangyuan city-related sequences in the latter two cluster sizes were found in CRF01_AEnetwork than that in CRF07_BC (P = 0.024),where 9 (32.1%), 11 (39.3%), and 8 (28.6%) for cluster sizes 2, 3–5 and >5 individuals were respectively observed in 28 Guangyuan city-related clusters, (Fig. 4B). Interestingly, a large cluster existed in both CRF07_BC and CRF01_AE networks, with only Guangyuan city-related sequences (Fig. 4A,B). Both clusters had low mean genetic distance (0.00524 ± 0.00109 and 0.00421 ± 0.00062 nucleotide substitutions per sit), inferring a recent transmission of these two strains. The localCRF07_BC cluster included 9 male individuals, consisting of 6 MSM and 3 heterosexuals, among which 2 were diagnosed in 2012, 4 in 2014, 1 in 2015, and 2 in 2016, while theCRF01_AE cluster included 12 male and 2 female individuals, consisting of 1 MSM and 13 heterosexuals, among which each 6 were diagnosed in 2014 and 2015, respectively, and 2 in 2016.
Figure 4.
The transmission networks of CRF07_BC (A) and CRF01_AE (B) infected individuals. M-HET, male heterosexuals; F-HET, female heterosexuals; MSM, men who have sex with men; PWID, persons who inject drugs; SU, sexual transmission, unspecified type.
Migrant-history workers fueled HIV-1 transmission in Guangyuan city
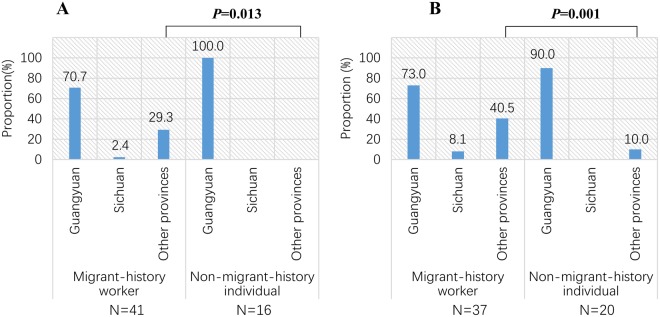
Among all Guangyuan city sequence in CRF07_BC and CRF01_AE networks, the migrant-history workers were dominant. In CRF07_BC networks, there were 59 Guangyuan city sequence including 41 (69.5%) migrant-history workers and 16 (27.1%)non-migrant-history individuals. In CRF01_AE networks, there were 60 Guangyuan city sequence including 37 (61.7%) migrant-history workers and 20 (33.3%) subjects with no migrant history (non-migrant-history individuals). Interestingly, migrant-history workers linked more sequences from other provinces in both CRF07_BC and CRF01_AE networks (Fig. 5). Of 41 migrant-history workers in CRF07_BC networks, 29.3% (12) were linked to other provinces’ sequences. However, of 16 non-migrant-history individuals in CRF07_BC networks, no sequence was linked to other provinces’ sequence (P = 0.013, Fig. 5A). Similarly, of 37 migrant-history workers in CRF01_AE networks, 40.5% (15) were linked to other provinces’ sequences. But, only 2 (10%) subjects with no migrant history were linked to other provinces’ sequences in CRF01_AE networks (P = 0.001, Fig. 5B). While, by contrast, only 1 (2.4%) and 3 (8.1%) migrant-history workers linked with sequences from Sichuan in CRF07_BC and CRF01_AE networks, respectively.
Figure 5.
Links between Guangyuan city and other cities or provinces when stratified by migrant-history workers and non-migrant-history individuals in CRF07_BC (A) and CRF01_AE (B) networks. The column represented the proportion of migrant-history workers or non-migrant-history individuals linked with the Guangyuan, Sichuan and other provinces’ sequences, respectively, in networks.
Regarding to the HIV-1 transmission clusters between Guangyuan city and other provinces, over one fifth (20.3%, 12 of 59) of individuals were found within CFR07_BC network including Beijing (5.1%), Shanghai (5.1%), Guangdong (3.4%), Yunnan (3.4%), Xinjiang (1.7%) and Zhejiang (1.7%). Similarly, in CRF01_AE network, we found 28.3% (17 of 60) of individuals were involved the transmission between Guangyuan city and other provinces including Guangdong (10.0%), Shanghai (6.7%), Beijing (5%), as well as Fujian(1.7%), Hainan(1.7%), Henan(1.7%), Hunan(1.7%), and Shannxi(1.7%). (Table 3).
Table 3.
Links between Guangyuan and other cities or provinces in the transmission networks.
| Subtype | n | BJ | FJ | GD | HAN | HEN | HUN | SAX | SH | XJ | YN | ZJ | O/N |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CRF07_BC | 12 | 3 (5.1) | 2 (3.4) | 3 (5.1) | 1 (1.7) | 2 (3.4) | 1 (1.7) | 2 (3.4) | |||||
| CRF01_AE | 17 | 3 (5.0) | 1 (1.7) | 6 (10.0) | 1 (1.7) | 1 (1.7) | 1 (1.7) | 1 (1.7) | 4 (6.7) |
GY, Guangyuan; SC, Sichuan (not including Guangyuan); BJ, Beijing; FJ, Fujian; GD, Guangdong; HAN, Hainan; HEN, Henan; HUN, Hunan; SAX, Shaanxi; SH, Shanghai; XJ, Xinjiang; YN, Yunnan; ZJ, Zhejiang; O/N, other/not available.
The Guangyuan city local linkages between different risk groups in the transmission networks were shown in Table 4. Of 26 Guangyuan city MSM in CRF07_BC networks, 80.8% (n = 21) were linked to other MSM, 26.9% (n = 7) to male heterosexuals, and 7.7% (n = 2) to female heterosexuals. Unexpectedly, of 20 Guangyuan city male heterosexuals, only 20.0% (n = 4) were linked to female heterosexuals, and on the contrary, a vast majority of them were linked to MSM and other male heterosexuals (75.0%, n = 15). Of 11 Guangyuan city female heterosexuals, 36.4% (n = 4) were linked to male heterosexuals, while 18.2% (n = 2) and 54.5% (n = 6) to MSM and other female heterosexuals, respectively. In CRF01_AE networks of 9 Guangyuan city MSM, 66.7% (n = 6) were linked to other MSM, 22.2% (n = 2) to male heterosexuals, and 33.3% (n = 3) to female heterosexuals. Unexpectedly, among the 35 Guangyuan city male heterosexuals, more than half of individuals (62.9%, n = 22) shared links with other male heterosexuals, while 25.7% (n = 9) were found to link to MSM and 22.9% (n = 8) to female heterosexuals. Of 13 Guangyuan city female heterosexuals, 46.2% (n = 6) were linked to male heterosexuals; however, 23.1% (n = 3) were linked to MSM and other female heterosexuals, respectively.
Table 4.
Links between different risk groups in the transmission networks.
| n | MSM | Male HET | Female HET | O/N | ||
|---|---|---|---|---|---|---|
| CRF07_BC | MSM | 26 | 21 (80.8) | 7 (26.9) | 2 (7.7) | 2 (7.7) |
| M-HET | 20 | 10 (50.0) | 5 (25.0) | 4 (20.0) | 3 (15.0) | |
| F-HET | 11 | 2 (18.2) | 4 (36.4) | 6 (54.5) | ||
| PWID/SU | 2 | 2 (100.0) | ||||
| CRF01_AE | MSM | 9 | 6 (66.7) | 2 (22.2) | 3 (33.3) | 1 (11.1) |
| M-HET | 35 | 9 (25.7) | 22 (62.9) | 8 (22.9) | 2 (5.7) | |
| F-HET | 13 | 3 (23.1) | 6 (46.2) | 3 (23.1) | 1 (7.7) | |
| PWID/SU | 3 | 1 (33.3) | 2 (66.7) |
M-HET, male heterosexuals; F-HET, female heterosexuals; MSM, men who have sex with men; PWID, persons who inject drugs; SU, sexual transmission, unspecified type.
Discussion
As the uneven economic development in China, massive migrant-workers traveled from the rural areas to urban centers to seek better employment opportunities and to improve their living conditions. By the end of 2017, the size of outgoing migrant-workers had reached 171.9 million nationwide, and the majority of them were living in some international metropolis, such as Beijing, Shanghai, Guangzhou, et al.10. The strong association between HIV-1 infection and migrant-workers was well-established16–18. Engaging in high-risk behaviors5 made them more vulnerable to HIV-1 than the general population19. In addition, the high mobility of migrant-workers makes it difficult to monitor HIV-1 infection and manage care20. Guangyuan city in Sichuan was well-known as a labor-exporting city with approximately one million migrant-workers every year21. Overall, we elucidated the characteristics of HIV-1 genetic diversity, viral evolutional lineages, and transmission networks in this city. Two distinguishing features of HIV-1 epidemics in Guangyuan city included: 1) there were close transmission linkages between Guangyuan city and other provinces or municipalities, especially some international metropolis, for which people who ever went out as migrant-workers probably played a crucial role; 2) the vast majority of male heterosexuals were observed being shared links with other male heterosexuals and MSM, implying that some MSM might hide their real sexual orientation.
In this study, we found a remarkably high portion of a migrant-history HIV reported cases in Guangyuan city, and most of the migrant-history workers were outside the home province. The studies in some single towns (e.g., Unite Kingdom and Uganda), showed that only small amount of the transmission events occurred locally22–24. To further identify the reliable linkages between HIV reported cases in Guangyuan city and other areas, a wide range of reference sequences were included for both phylogenetic analysis and transmission network analysis. As expected, our results revealed that Guangyuan city sequences had a close link with sequences form other cities. Furthermore, a much higher proportion of links were found with sequences derived from the Yangtze, Zhujiang River delta areas and the Bohai Rim than that from other cities of Sichuan. Based on the statistical data, an approximately above 50% migrant-workers of Guangyuan city constantly flow to the cities of these areas, such as Guangdong (106.9 thousand), Zhejiang (86.3 thousand), Shanghai and Jiangsu (62.7 thousand), as well as Beijing and Tianjin (61.1 thousand)9. Thus we inferred that the migrant-workers flow between their work place and home with not only money but also HIV-1, for their higher levels of sexual risk including unprotected sex25. And they might serve as a bridge and facilitated viral transmission from other provinces/cities to home regions.
Although heterosexual contact remained the domination of acquiring the HIV-1 infection in Guangyuan city, the proportions of MSM in newly diagnosed HIV-1 infections posed a persistent increase in recent years. Usually, urban areas had more attraction to MSM, since large cities had relatively open culture and convenient sexual venues (bars, saunas, parks, sex clubs, et al.)18. These MSM migrants were more at highest risk for HIV-1 than other individuals in the migrant-workers26–28. More disturbing, a number of MSM might hide their real sexual orientation in China, because of the traditional cultural, historical reasons, as well as societal stigma and discrimination29, which could be wildly underestimating the role of the MSM in the HIV-1 transmission networks. Especially, the frequent high-risk bisexuality and unprotected behaviors of these MSM make their female partners more vulnerable to HIV-130,31. This also suggested that the real infected routes of these male heterosexuals in the large cluster deserved further investigation. Importantly, the low mean genetic distance in two lager clusters with recently diagnosed individuals in both CRF07_BC and CRF01_AE networks illustrated that the dynamic networks would probably continue to expand in the future if not intervened.
However, the incomplete coverage of sequences might make our results subject to selection/sampling bias. We anticipated being able to make even stronger inferences about the transmission network characteristic through improving the completeness of molecular surveillance data in the future.
Conclusions
We, for the first time, revealed the current HIV-1 epidemic in a hotspot area of Sichuan province that exported labors through analysis of viral diversity and transmission networks, and further underscored the value of molecular sequences survey combined with epidemiologic and demographic data in guiding precautionary intervention at the local level.
Electronic supplementary material
Acknowledgements
This study was supported by the Sichuan Science and Technology Project (2017JY0302). The authors would like to thank staffs in Division of Virology and Immunology, National Center for AIDS/STD Control and Prevention (NCAIDS), China CDC for technical assistance. The opinions expressed herein show the collective views of the coauthors and do not necessarily represent the official position of the Sichuan Provincial Center for Disease Control and Prevention, Center for AIDS/STD Control and Prevention, nor the Guangyuan Provincial Center for Disease Control and Prevention, Center for AIDS/STD Control and Prevention.
Author Contributions
Ling Su, Xiaoshan Li and Linglin Zhang conceived and designed the experiments. Xueqin Hou, Dongbin Wei, Yu Fu, Li Ye, Li Xiong,Ying Hu and Hong Yang prepared the data. Shu Liang, Yali Zeng and Bo Wu analyzed the data. Ling Su, Xiaoshan Li and Ping Zhong wrote the paper. All authors read and approved the final manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Linglin Zhang, Email: zhangllsccdc@163.com.
Xiaoshan Li, Email: sclxs87@163.com.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-33996-6.
References
- 1.NCAIDS N, China CDC Update on AIDS/STD epidemic in china in December, 2017. Chinese Journal of AIDS & STD. 2018;02:111–112. [Google Scholar]
- 2.Liu X, Erasmus V, Wu Q, Richardus JH. Behavioral and Psychosocial Interventions for HIV Prevention in Floating Populations in China over the Past Decade: A Systematic Literature Review and Meta-Analysis. Plos One. 2014;9:e101006. doi: 10.1371/journal.pone.0101006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li X, et al. Genetic transmission networks reveal the transmission patterns of HIV-1 CRF01_AE in China. Sexually Transmitted Infections. 2017;94:111–116. doi: 10.1136/sextrans-2016-053085. [DOI] [PubMed] [Google Scholar]
- 4.National Bureau of Statistics of China. Statistical Communiqué of the People’s Republic of China on the 2017 National Economic and Social Development. Available from: http://www.stats.gov.cn/english/PressRelease/201802/t20180228_1585666.html (2018).
- 5.Zhang L, Chow EP, Jahn HJ, Kraemer A, Wilson DP. High HIV prevalence and risk of infection among rural-to-urban migrants in various migration stages in China: a systematic review and meta-analysis. Sexually Transmitted Diseases. 2013;40:136–147. doi: 10.1097/OLQ.0b013e318281134f. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, et al. Prevalence of HIV-1 subtypes among men who have sex with men in China: a systematic review. International Journal of Std & Aids. 2015;26:291–305. doi: 10.1177/0956462414543841. [DOI] [PubMed] [Google Scholar]
- 7.Zhao J, et al. The dynamics of the HIV epidemic among men who have sex with men (MSM) from 2005 to 2012 in Shenzhen. China. Scientific Reports. 2016;6:28703. doi: 10.1038/srep28703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dai W, et al. Sexual behavior of migrant workers in Shanghai, China. BMC Public Health. 2015;15:1067. doi: 10.1186/s12889-015-2385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Municipal people’s government of Guangyuan. Investigation report on the situation of rural labor in Guangyuan. Available from, http://www.cngy.gov.cn/govop/show/20170725144836-36460-00-000.html (2017).
- 10.National Health and Family Planning Commission of the People’s Republic of China. 2016 China Floating Population Development Report. Available from, http://www.moh.gov.cn/ldrks/s7847/201610/d17304b7b9024be38facb5524da48e78.shtml (2016).
- 11.Liao L, et al. Genotypic analysis of the protease and reverse transcriptase of HIV type 1 isolates from recently infected injecting drug users in western China. Aids Research & Human Retroviruses. 2007;23:1062–1065. doi: 10.1089/aid.2007.0050. [DOI] [PubMed] [Google Scholar]
- 12.Price MN, Dehal PS, Arkin AP. FastTree 2 – Approximately Maximum-Likelihood Trees for Large Alignments. Plos One. 2010;5:e9490. doi: 10.1371/journal.pone.0009490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu K, Linder CR, Warnow T. RAxML and FastTree: Comparing Two Methods for Large-Scale Maximum Likelihood Phylogeny Estimation. Plos One. 2011;6:e27731. doi: 10.1371/journal.pone.0027731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ragonnet-Cronin M, et al. Automated analysis of phylogenetic clusters. BMC Bioinformatics. 2013;14:317–317. doi: 10.1186/1471-2105-14-317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Su G, Morris JH, Demchak B, Bader GD. Biological Network Exploration with Cytoscape 3. Current Protocols in Bioinformatics. 2014;47:8.13.11–18.13.24. doi: 10.1002/0471250953.bi0813s47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson AF, Qingsi Z, Hua X, Jianfeng B. China’s floating population and the potential for HIV transmission: a social-behavioural perspective. Aids Care. 2003;15:177–185. doi: 10.1080/0954012031000068326. [DOI] [PubMed] [Google Scholar]
- 17.Anglewicz P, Vanlandingham M, Manda-Taylor L, Kohler HP. Migration and HIV infection in malawi: A population-based longitudinal study. Aids. 2016;30:2099–2105. doi: 10.1097/QAD.0000000000001150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hesketh T, Ye XJ, Li L, Wang HM. Health status and access to health care of migrant workers in China. Public Health Reports. 2008;123:189–197. doi: 10.1177/003335490812300211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xia Z, et al. Rural-to-urban migrants are at high risk of sexually transmitted and viral hepatitis infections in China: a systematic review and meta-analysis. BMC Infectious Diseases. 2014;14:490. doi: 10.1186/1471-2334-14-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meng X, et al. Estimation and projection of the HIV epidemic trend among the migrant population in China. Biomedical and Environmental Sciences. 2011;24:343–348. doi: 10.3967/0895-3988.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Li X, Zhang LB, Fang X, Xiong Q, Lin D. HIV/AIDS-related sexual risk behaviors among rural residents in China: potential role of rural-to-urban migration. Aids Educ Prev. 2007;19:396–407. doi: 10.1521/aeap.2007.19.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher M, et al. Determinants of HIV-1 transmission in men who have sex with men: a combined clinical, epidemiological and phylogenetic approach. Aids. 2010;24:1739–1747. doi: 10.1097/QAD.0b013e32833ac9e6. [DOI] [PubMed] [Google Scholar]
- 23.Yirrell DL, et al. Molecular epidemiological analysis of HIV in sexual networks in Uganda. Aids. 1998;12:285–290. doi: 10.1097/00002030-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Wertheim JO, et al. The global transmission network of HIV-1. Journal of Infectious Diseases. 2014;209:304–313. doi: 10.1093/infdis/jit524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang R, Sun B, Zeng H, Li T, Wang Y. The epidemic dynamics of four major lineages of HIV-1 CRF01_AE strains after their introductions into China. Aids Research & Human Retroviruses. 2016;32:420–426. doi: 10.1089/aid.2016.0031. [DOI] [PubMed] [Google Scholar]
- 26.Shi TX, et al. Study on the high risk behaviors related to AIDS among men who having sex with men in the floating population. Zhonghua liuxingbingxue zazhi(in Chinese). 2009;30:668–671. [PubMed] [Google Scholar]
- 27.Wang K, et al. Increasing prevalence of HIV and syphilis but decreasing rate of self-reported unprotected anal intercourse among men who had sex with men in Harbin, China: results of five consecutive surveys from 2006 to 2010. International Journal of Epidemiology. 2012;41:423–432. doi: 10.1093/ije/dyr182. [DOI] [PubMed] [Google Scholar]
- 28.Zhong F, et al. Increasing HIV and Decreasing Syphilis Prevalence in a Context of Persistently High Unprotected Anal Intercourse, Six Consecutive Annual Surveys among Men Who Have Sex with Men in Guangzhou, China, 2008 to 2013. Plos One. 2014;9:e103136. doi: 10.1371/journal.pone.0103136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Report on the living consumption of LGBT group in China. Available from, https://www.danlan.org/disparticle_55025.htm (2018).
- 30.Lau JT, et al. Prevalence of bisexual behaviors among men who have sex with men (MSM) in China and associations between condom use in MSM and heterosexual behaviors. Sexually Transmitted Diseases. 2008;35:406–413. doi: 10.1097/OLQ.0b013e318164467f. [DOI] [PubMed] [Google Scholar]
- 31.Chow EPF, Wilson DP, Zhang L. What is the potential for bisexual men in China to act as a bridge of HIV transmission to the female population? Behavioral evidence from a systematic review and meta-analysis. BMC Infectious Diseases. 2011;11:242–242. doi: 10.1186/1471-2334-11-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.