Abstract
We aimed to investigate the potential of preoperative mammographic breast density (MBD) as a prognostic factor in breast cancer. Data of 969 patients with primary breast cancer were analyzed. We defined low MBD as fatty or fibroglandular breast, and high MBD as heterogeneously dense or extremely dense breast, respectively. The high MBD group demonstrated a superior overall survival rate compared to the low MBD group (p < 0.001). Favorable prognostic effects of high MBD were observed in subgroups aged >50 years (p < 0.001) and with positive hormone receptor (HRc) and negative human epidermal growth factor receptor 2 (HER2) (p < 0.001). The high MBD group had a higher proportion of patients aged ≤50 years (p < 0.001) and patients with body mass index (BMI) ≤25 kg/m2 (p < 0.001), and a higher proportion of patients who received chemotherapy (p < 0.001). MBD was a significant independent prognostic factor by multivariable analysis (hazard ratio, 0.382; 95% confidence interval, 0.206–0.708). The high MBD group was associated with superior overall survival rates. Preoperative MBD was a strong independent prognostic factor in operable primary invasive female breast cancer, especially in patients with age >50 years and the HRc(+)/HER2(−) subtype. Favorable clinicopathologic features, active treatments, and other factors could contribute to this causality.
Introduction
Mammographic breast density (MBD) depends on the relative composition of radio-dense fibroglandular tissue relative to radiolucent fat tissue in the breast. In 1976, Wolfe first proposed a four category-based classification system of MBD1 and reported the risk of MBD in breast cancer development2. Currently, Breast Imaging-Reporting and Data System (BI-RADS) proposed by the American College of Radiology recommends a succinct description of overall breast composition3.
Several aspects of the clinical significance of MBD in breast cancer have been investigated. First, the association between MBD and breast cancer development has been extensively studied, and MBD has been reported to be one of the strongest risk factors associated with breast cancer4,5. Risk of breast cancer development was reported to be four to six times greater in women with dense breasts compared to women with fatty breasts6,7. Second, the question of whether reductions in MBD, (noted after tamoxifen treatment of estrogen receptor-positive breast cancer), are associated with breast cancer prognosis, has been investigated. Both premenopausal8 and postmenopausal patients9 with estrogen receptor-positive breast cancer, who experience a large reduction in MBD following initiation of tamoxifen treatment, have been reported to have a better prognosis. Third, the association between MBD and breast cancer prognosis has also been investigated, but the results have not been consistent and overall, remain controversial. Some papers reported that fatty breast was associated with worse prognosis10,11, but others reported completely opposite results suggesting a favorable prognostic effect of fatty breast12,13. Still other studies reported no association between MBD and breast cancer prognosis14–16.
As previous studies have focused on the role of MBD as an etiologic factor rather than a prognostic factor in breast cancer, the prognostic value of MBD remains largely unknown. In this study, we aimed to investigate the role of preoperative MBD as a prognostic factor in breast cancer using our institution’s breast cancer database.
Methods
Patients
The subjects of this study were consecutive, operable, primary invasive female breast cancer patients, who underwent curative surgery at the Seoul Metropolitan Government Seoul National University Boramae Medical Center from August 1992 to December 2016. All primary breast cancer patients who received treatment at Seoul Metropolitan Government Seoul National University Boramae Medical Center had been registered in the Boramae Hospital Breast Cancer Registry. The number of patients in the registry was 1,456 at the time of this study. We excluded 57 patients who were diagnosed after December 31, 2016. We also excluded 162 patients diagnosed as having stage 0 breast cancer, 39 patients initially diagnosed as having stage IV breast cancer, and 35 patients with no information on their stage. We further excluded 159 patients with no data on MBD, 6 patients diagnosed as having malignant phyllodes tumor, 27 patients who received neoadjuvant chemotherapy, 2 male patients, and 2 patients with age less than 20 or more than 90 years. Finally, we analyzed data of 967 female patients with operable primary invasive breast cancer.
Clinicopathologic Parameters
We defined patient age as the age at time of diagnosis of primary breast cancer, and described the TNM staging according to the 7th edition of the American Joint Committee on Cancer. Hormone receptor (HRc) status was defined as positive when immunohistochemistry test for either estrogen receptor or progesterone receptor was positive. HRc was defined as negative when both estrogen receptor and progesterone receptor were negative. Human epidermal growth factor receptor 2 (HER2) was defined as negative when immunohistochemistry results were negative or 1+. HER2 was defined as positive when immunohistochemistry results were 3+. When immunohistochemistry results were 2+, positivity of HER2 was defined according to the results of in situ hybridization. Histologic grade was defined according to the modified Scarff-Bloom-Richardson grading system. Lymphovascular invasion was defined as positive when either lymphatic invasion or vascular invasion was present. It was defined as negative when both were absent. Body mass index (BMI) was defined as the ratio of body weight (in kilograms) to height (in square meters). All operations with curative intent for breast cancer patients were classified into lumpectomy or mastectomy according to the extent of surgery.
Mammographic Breast Density
Preoperative MBD was classified according to BI-RADS Atlas 2013 (5th edition)3. BI-RADS Atlas for mammography recommends the following four categories of MBD as defined by the visually estimated content of fibroglandular-density tissue within the breast; the breasts are almost entirely fatty (a), there are scattered areas of fibroglandular density (b), the breasts are heterogeneously dense, which may obscure small masses (c), and the breasts are extremely dense, which lowers the sensitivity of mammography (d). In this study, we have described these four categories as fatty, fibroglandular, heterogeneously dense, and extremely dense, respectively. We further defined fatty or fibroglandular as low MBD, and heterogeneously dense or extremely dense as high MBD, respectively. We obtained data for preoperative MBD from the database of the Boramae Hospital Breast Cancer Registry. For this database, MBD data were obtained from the final and formal interpretation report on the preoperative mammography of each subject. In our institute, a mammogram report is made by single radiologist with no consensus. Seven experienced radiologists had been involved in interpretation of mammograms which were utilized in this study at the start time of this study. All radiologists were or are, faculty members of our hospital as professors in the Department of Radiology. All of them graduated from a four year course of resident training in the Department of Radiology and then, finished a two year course of fellowship training for subspecialty in the area of breast cancer. All of them worked or have been working in the Breast Center of our institute as professors in the Department of Radiology. The mean experience period of MBD interpretation is approximately 5 years. All of the mammograms were obtained before pathologic diagnosis of primary breast cancer. Average time between mammography and diagnosis was approximately 2 weeks (median, 13 days; range, 4~89 days).
Statistical Analyses
Two-sample t-test was used to determine differences in expression levels of biological parameters, while Pearson’s χ2 test was used to determine differences in clinicopathologic characteristics between groups. The p for trend value was calculated using the linear by linear association test in a Pearson’s χ2 test. We analyzed overall survival and disease-free survival, defining the time intervals for each as the time from operation to death from any cause, and the time from operation to recurrence of any type, respectively. Breast cancer recurrence types included local recurrence, regional recurrence and distant recurrence. Contralateral breast cancer development was not included in breast cancer recurrence types but it was also analyzed in this study. The Kaplan-Meier estimator was used to analyze survival rates and log-rank test was used to determine the significance of differences between two or more survival curves. Cox proportional hazards model was used for multivariable analysis. MBD was adjusted with all 14 factors including 9 clinicopathologic factors (tumor size, nodal positivity, estrogen receptor, progesterone receptor, HER2, histologic grade, lymphovascular invasion, age, and BMI) and 5 treatment factors (operation, radiation therapy, chemotherapy, Herceptin therapy, and endocrine therapy) by multivariate analysis.
Hazard ratio (HR) and 95% confidence interval (CI) were calculated. All statistical analyses were carried out using IBM SPSS Statistics, version 20.0 (IBM Corp., Armonk, NY, USA). All tests were two-tailed. Statistical significance was considered achieved when p value was less than 0.05.
Results
Clinicopathologic Characteristics
The total number of subjects was 967 and their mean age was 54.3 ± 12.3 years (median, 52.0 years; range, 25–87 years). Operation dates were between August 1992 and December 2016, and the mean follow-up period for overall survival was 70.8 ± 54.1 months (median, 56.0 months; range, 1~298 months). The total number of deaths and recurrences during this period was 94 (9.7%) and 101 (10.4%), respectively. Among 873 subjects who survived, 652 patients had no evidence of disease, 68 patients had breast cancer recurrence, and 153 patients were missed to follow-up at the reference time of final follow-up (December 2016). The clinicopathologic characteristics of all subjects according to MBD are summarized in Table 1. The proportions of fatty, fibroglandular, heterogeneously dense, and extremely dense breasts were 15.3%, 29.1%, 36.9%, and 18.7%, respectively. Low and high MBD accounted for 44.4% and 55.6% of all subjects, respectively. The mean age of patients with high MBD was significantly lower than that of patients with low MBD. The high MBD group showed a higher proportion of patients with age ≤50 years, BMI ≤ 25 kg/m2, and positive HRc compared to the low MBD group. The high MBD group was also associated with a higher proportion of patients who received chemotherapy or radiation therapy.
Table 1.
Clinicopathologic characteristics of all subjects according to mammographic breast density.
| Characteristics | Mammographic Breast Densitya | Mammographic Breast Densityb | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fatty | Fibroglandular | Heterogeneously dense | Extremely dense | Sum | p for Trend | Low | High | p c | ||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |||
| All | 148 | 15.3% | 281 | 29.1% | 357 | 36.9% | 181 | 18.7% | 967 | 100.0% | 429 | 44.4% | 538 | 55.6% | ||
| Mean age (years) | 66.8 ± 10.0 | 59.1 ± 10.8 | 50.2 ± 9.6 | 44.7 ± 8.8 | 54.3 ± 12.3 | 61.7 ± 11.1 | 48.3 ± 9.7 | <0.001 | ||||||||
| Tumor size (cm) | 0.699 | 0.378 | ||||||||||||||
| ≤2 | 75 | 50.7% | 126 | 178 | 49.9% | 90 | 49.7% | 469 | 48.6% | 201 | 47.0% | 268 | 49.8% | |||
| >2 | 73 | 49.3% | 154 | 55.0% | 179 | 50.1% | 91 | 50.3% | 497 | 51.4% | 227 | 53.0% | 270 | 50.2% | ||
| Nodal positivity | 0.464 | 0.818 | ||||||||||||||
| Negative | 108 | 73.0% | 165 | 58.9% | 230 | 64.4% | 117 | 64.6% | 620 | 64.2% | 273 | 63.8% | 347 | 64.5% | ||
| Positive | 40 | 27.0% | 115 | 41.1% | 127 | 35.6% | 64 | 35.4% | 346 | 35.8% | 155 | 36.2% | 191 | 35.5% | ||
| Stage | 0.924 | 0.477 | ||||||||||||||
| Stage I | 66 | 44.6% | 97 | 34.6% | 142 | 39.8% | 75 | 41.4% | 380 | 39.3% | 163 | 38.1% | 217 | 40.3% | ||
| Stage II, III | 82 | 55.4% | 183 | 65.4% | 215 | 60.2% | 106 | 58.6% | 586 | 60.7% | 265 | 61.9% | 321 | 59.7% | ||
| Hormonal receptor | 0.049 | 0.024 | ||||||||||||||
| Negative | 39 | 26.5% | 77 | 28.1% | 76 | 21.7% | 37 | 20.4% | 229 | 24.0% | 116 | 27.6% | 113 | 21.2% | ||
| Positive | 108 | 73.5% | 197 | 71.9% | 275 | 78.3% | 144 | 79.6% | 724 | 76.0% | 305 | 72.4% | 419 | 78.8% | ||
| Estrogen receptor | 0.049 | 0.067 | ||||||||||||||
| Negative | 48 | 32.7% | 87 | 31.8% | 98 | 27.8% | 44 | 24.3% | 277 | 29.0% | 135 | 32.1% | 142 | 26.6% | ||
| Positive | 99 | 67.3% | 187 | 68.2% | 254 | 72.2% | 137 | 75.7% | 677 | 71.0% | 286 | 67.9% | 391 | 73.4% | ||
| Progesterone receptor | 0.011 | 0.003 | ||||||||||||||
| Negative | 58 | 39.5% | 117 | 42.7% | 115 | 32.8% | 56 | 30.9% | 346 | 36.3% | 175 | 41.6% | 171 | 32.1% | ||
| Positive | 89 | 60.5% | 157 | 57.3% | 236 | 67.2% | 125 | 69.1% | 607 | 63.7% | 246 | 58.4% | 361 | 67.9% | ||
| HER2 | 0.054 | 0.280 | ||||||||||||||
| Negative | 112 | 81.2% | 194 | 76.4% | 252 | 77.3% | 113 | 70.2% | 671 | 76.3% | 306 | 78.1% | 365 | 74.9% | ||
| Positive | 26 | 18.8% | 60 | 23.6% | 74 | 22.7% | 48 | 29.8% | 208 | 23.7% | 86 | 21.9% | 122 | 25.1% | ||
| Histologic grade | 0.330 | 0.198 | ||||||||||||||
| 1,2 | 80 | 58.4% | 157 | 60.2% | 219 | 64.8% | 106 | 61.6% | 562 | 61.9% | 237 | 59.5% | 325 | 63.7% | ||
| 3 | 57 | 41.6% | 104 | 39.8% | 119 | 35.2% | 66 | 38.4% | 346 | 38.1% | 161 | 40.5% | 185 | 36.3% | ||
| Negative | 95 | 71.4% | 162 | 63.8% | 197 | 62.7% | 104 | 63.8% | 558 | 64.6% | 257 | 66.4% | 301 | 63.1% | ||
| Positive | 38 | 28.6% | 92 | 36.2% | 117 | 37.3% | 59 | 36.2% | 306 | 35.4% | 130 | 33.6% | 176 | 36.9% | ||
| Age (years) | <0.001 | <0.001 | ||||||||||||||
| ≤50 | 9 | 6.1% | 64 | 22.8% | 197 | 55.2% | 144 | 79.6% | 414 | 42.8% | 73 | 17.0% | 341 | 63.4% | ||
| >50 | 139 | 93.9% | 217 | 77.2% | 160 | 44.8% | 37 | 20.4% | 553 | 57.2% | 356 | 83.0% | 197 | 36.6% | ||
| BMI (kg/m2) | <0.001 | <0.001 | ||||||||||||||
| ≤25 | 68 | 45.9% | 131 | 46.6% | 238 | 66.9% | 159 | 87.8% | 596 | 61.7% | 199 | 46.4% | 397 | 73.9% | ||
| >25 | 80 | 54.1% | 150 | 53.4% | 118 | 33.1% | 22 | 12.2% | 370 | 38.3% | 230 | 53.6% | 140 | 26.1% | ||
| Operation | 0.063 | 0.062 | ||||||||||||||
| Lumpectomy | 62 | 41.9% | 103 | 36.7% | 150 | 42.0% | 89 | 49.2% | 404 | 41.8% | 165 | 38.5% | 239 | 44.4% | ||
| Mastectomy | 86 | 58.1% | 178 | 63.3% | 207 | 58.0% | 92 | 50.8% | 563 | 58.2% | 264 | 61.5% | 299 | 55.6% | ||
| Radiation therapy | 0.008 | 0.028 | ||||||||||||||
| No | 86 | 58.1% | 151 | 53.7% | 179 | 50.1% | 80 | 44.2% | 496 | 51.3% | 237 | 55.2% | 259 | 48.1% | ||
| Yes | 62 | 41.9% | 130 | 46.3% | 178 | 49.9% | 101 | 55.8% | 471 | 48.7% | 192 | 44.8% | 279 | 51.9% | ||
| Chemotherapy | <0.001 | <0.001 | ||||||||||||||
| No | 69 | 46.6% | 80 | 28.5% | 84 | 23.5% | 41 | 22.7% | 274 | 28.3% | 149 | 34.7% | 125 | 23.2% | ||
| Yes | 79 | 53.4% | 201 | 71.5% | 273 | 76.5% | 140 | 77.3% | 693 | 71.7% | 280 | 65.3% | 413 | 76.8% | ||
| Herceptin therapy | 0.952 | 0.986 | ||||||||||||||
| No | 134 | 90.5% | 251 | 89.3% | 320 | 89.6% | 163 | 90.1% | 868 | 89.8% | 385 | 89.7% | 483 | 89.8% | ||
| Yes | 14 | 9.5% | 30 | 10.7% | 37 | 10.4% | 18 | 9.9% | 99 | 10.2% | 44 | 10.3% | 55 | 10.2% | ||
| Endocrine therapy | 0.175 | 0.072 | ||||||||||||||
| No | 34 | 23.0% | 90 | 32.0% | 91 | 25.5% | 37 | 20.4% | 252 | 26.1% | 124 | 28.9% | 128 | 23.8% | ||
| Yes | 114 | 77.0% | 191 | 68.0% | 266 | 74.5% | 144 | 79.6% | 715 | 73.9% | 305 | 71.1% | 410 | 76.2% | ||
Abbreviations: BMI, body mass index; HER2; human epidermal growth factor receptor 2.
aMammographic breast density was classified to 4 categories as fatty, fibroglandular, heterogeneously dense, and extremely dense according to BI-RADS Atlas 2013 (5th edition).
bFatty and fibroglandular categories were defined as low mammographic breast density. Heterogeneously dense and extremely dense categories were defined as high mammographic breast density.
cP value for mean age was calculated by t-test and all the other p values were calculated by χ2 test.
Survival Analysis
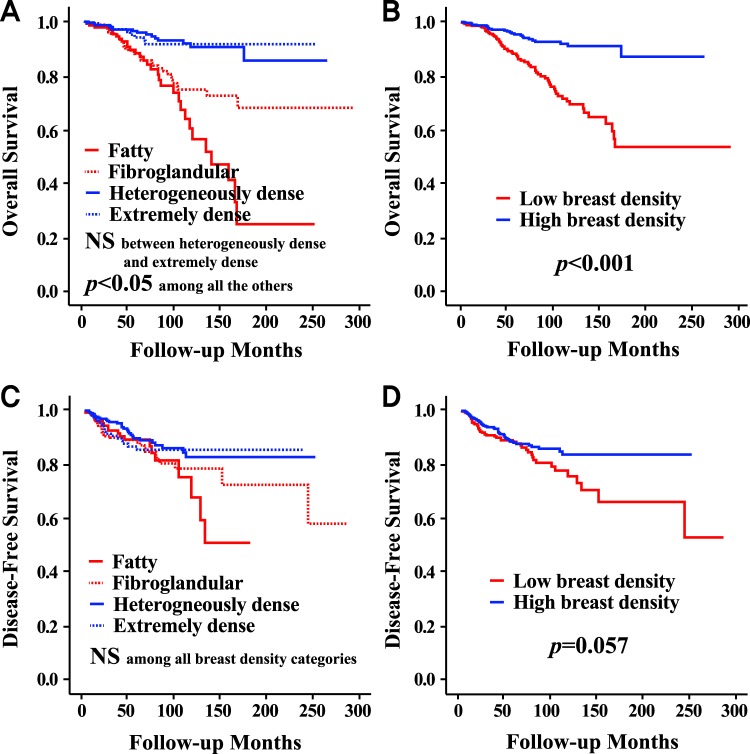
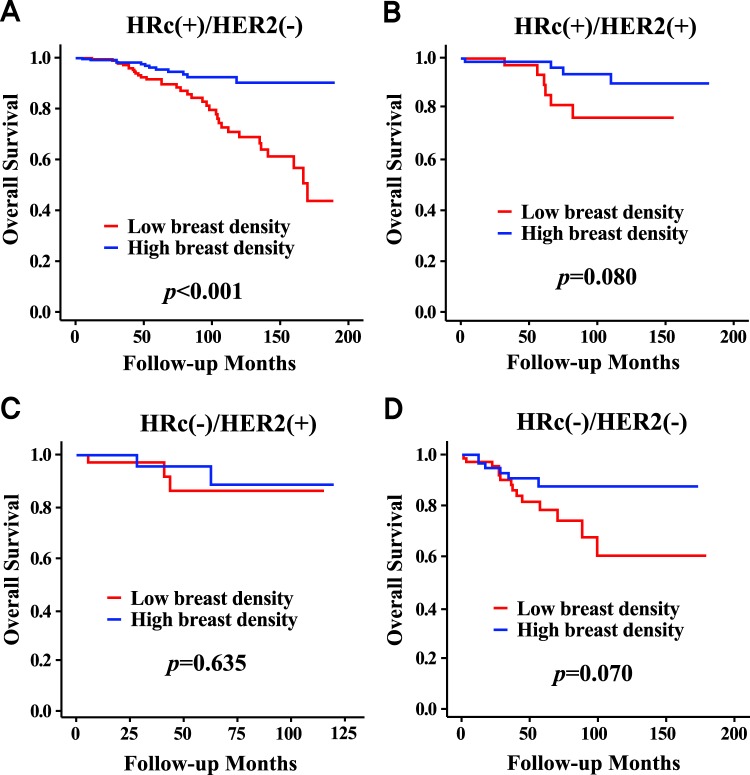
The high MBD group showed a superior overall survival rate compared to the low MBD group (p < 0.001), but there was no significant difference between the two groups in terms of the disease-free survival rate (Fig. 1). When MBD was classified into four categories, the p values by log-rank test were significant among all categories, except between heterogeneously dense, and extremely dense, with respect to overall survival. The p values were not significant among any breast density categories with respect to disease-free survival. The high MBD group showed a higher overall survival rate compared to the low MBD group only in the HRc(+)/HER2(−) subgroup (p < 0.001), and there were no survival differences between the two groups in the other subgroups of HRc(+)/HER2(+), HRc(−)/HER2(+), and HRc(−)/HER2(−) (Fig. 2). There were no differences between the high and low MBD groups in terms of local recurrence or distant recurrence (Fig. S1). The low MBD group showed a higher regional recurrence rate compared to the high MBD group (p = 0.013), but the contralateral breast cancer development rate was higher in the high MBD group (p = 0.034). Detailed regional recurrence rates and incidence rates of contralateral breast cancer according to mammographic breast density are described in Table S3.
Figure 1.
Survival curves according to mammographic breast density in all subjects. Overall survival curves according to 4 categories of mammographic breast density (A) and according to high or low mammographic breast density (B). Disease-free survival curves according to 4 categories of mammographic breast density (C) and according to high or low mammographic breast density (D). Abbreviations: NS, not significant.
Figure 2.
Overall survival curves according to mammographic breast density in patients with each breast cancer subtype. HRc(+)/HER2(−) (A), HRc(+)/HER2(+) (B), HRc(−)/HER2(+) (C), and HRc(−)/HER2(−) (D). Abbreviations: HER2, human epidermal growth factor receptor 2; HRc, hormonal receptor.
Subgroup Analysis
Subgroup analyses with a forest plot revealed that prognoses in the high MBD group were better than those in the low MBD group in subgroups, regardless of tumor size, nodal positivity, stage, estrogen receptor, progesterone receptor, histologic grade, lymphovascular invasion, BMI, operation, radiation therapy, and chemotherapy (Table 2). Although the high MBD group showed superior prognosis in the subgroup with negative HER2 and in patients who received endocrine therapy, there were no differences in the subgroup with positive HER2 and in patients who did not receive endocrine therapy. Notably, the high MBD group showed better prognosis in the subgroup aged >50 years, but no difference was observed in the subgroup aged ≤50 years. In all subjects, the high MBD group showed superior prognosis compared to the low MBD group (HR, 0.282; 95% CI, 0.179–0.443).
Table 2.
Subgroup analysis of hazard ratios according to mammographic breast density regarding overall survival in all subjects.
| Characteristics | Subject Number | Low MBD | High MBD | HRa | CI (95%) | p | Forest Plotb | ||
|---|---|---|---|---|---|---|---|---|---|
| Total | 907 | 414 | 493 | 0.282 | 0.179 | 0.443 | <0.001 |
|
|
| Tumor size (cm) | ≤2 | 440 | 194 | 246 | 0.214 | 0.085 | 0.536 | 0.001 | |
| >2 | 466 | 219 | 247 | 0.330 | 0.196 | 0.556 | <0.001 | ||
| Nodal positivity | Negative | 579 | 264 | 315 | 0.217 | 0.107 | 0.440 | <0.001 | |
| Positive | 327 | 149 | 178 | 0.357 | 0.197 | 0.645 | 0.001 | ||
| Stage | Stage I | 353 | 157 | 196 | 0.178 | 0.050 | 0.632 | 0.008 | |
| Stage II, III | 553 | 256 | 297 | 0.319 | 0.196 | 0.519 | <0.001 | ||
| Hormonal receptor | Negative | 215 | 113 | 102 | 0.363 | 0.160 | 0.820 | 0.015 | |
| Positive | 681 | 295 | 386 | 0.256 | 0.149 | 0.442 | <0.001 | ||
| Estrogen receptor | Negative | 262 | 131 | 131 | 0.428 | 0.212 | 0.861 | 0.017 | |
| Positive | 635 | 277 | 358 | 0.218 | 0.120 | 0.398 | <0.001 | ||
| Progesterone receptor | Negative | 327 | 170 | 157 | 0.317 | 0.159 | 0.629 | 0.001 | |
| Positive | 569 | 238 | 331 | 0.257 | 0.141 | 0.471 | <0.001 | ||
| HER2 | Negative | 638 | 298 | 340 | 0.312 | 0.182 | 0.537 | <0.001 | |
| Positive | 190 | 82 | 108 | 0.410 | 0.146 | 1.157 | 0.092 | ||
| Histologic grade | 1,2 | 529 | 230 | 299 | 0.204 | 0.103 | 0.405 | <0.001 | |
| 3 | 321 | 155 | 166 | 0.333 | 0.174 | 0.637 | 0.001 | ||
| Lymphovascular invasion | Negative | 527 | 251 | 276 | 0.161 | 0.062 | 0.420 | <0.001 | |
| Positive | 285 | 122 | 163 | 0.315 | 0.172 | 0.577 | <0.001 | ||
| Age (years) | ≤50 | 379 | 69 | 310 | 0.495 | 0.220 | 1.118 | 0.091 | |
| >50 | 528 | 345 | 183 | 0.254 | 0.126 | 0.513 | <0.001 | ||
| BMI (kg/m2) | ≤25 | 550 | 189 | 361 | 0.213 | 0.118 | 0.384 | <0.001 | |
| >25 | 356 | 225 | 131 | 0.430 | 0.211 | 0.877 | 0.020 | ||
| Operation | Lumpectomy | 383 | 160 | 223 | 0.148 | 0.032 | 0.686 | 0.015 | |
| Mastectomy | 524 | 254 | 270 | 0.325 | 0.202 | 0.522 | <0.001 | ||
| Radiation therapy | No | 468 | 230 | 238 | 0.347 | 0.203 | 0.591 | <0.001 | |
| Yes | 439 | 184 | 255 | 0.188 | 0.080 | 0.445 | <0.001 | ||
| Chemotherapy | No | 260 | 144 | 116 | 0.185 | 0.072 | 0.474 | <0.001 | |
| Yes | 647 | 270 | 377 | 0.382 | 0.221 | 0.658 | 0.001 | ||
| Endocrine therapy | No | 237 | 120 | 117 | 0.485 | 0.232 | 1.013 | 0.054 | |
| Yes | 670 | 294 | 376 | 0.221 | 0.124 | 0.396 | <0.001 | ||
|
|||||||||
Abbreviations: BMI, body mass index; CI, confidence interval; HER2, human epidermal growth factor receptor 2; HR, hazard ratio.
aHRs are the relative risks of the high mammographic breast density group with reference of the low mammographic breast density group regarding overall survival by Cox proportional hazards model.
bIn the forest plot, a HR value of less than 1 favors the high mammographic breast density group against the low mammographic breast density group regarding overall survival. The red circles mean statistical significance and the blue squares mean no statistical significance. The green diamond means the result of total subjects.
Multivariable Analysis
MBD was a significant independent prognostic factor (HR, 0.382; 95% CI, 0.206–0.708) after being adjusted with 14 factors including nine clinicopathologic factors and five treatment factors (Table 3).
Table 3.
Multivariable analysis in all subjects regarding mammographic breast density in terms of overall survival.
| Characteristics | HR | 95% CI | p | |
|---|---|---|---|---|
| Mammographic breast density, high vs low | 0.382 | 0.206 | 0.708 | 0.002 |
| Tumor size (cm), >2 vs ≤2 | 2.132 | 1.084 | 4.194 | 0.028 |
| Nodal positivity, positive vs negative | 1.103 | 0.605 | 2.013 | 0.749 |
| Estrogen receptor, positive vs negative | 0.757 | 0.391 | 1.469 | 0.411 |
| Progesterone receptor, positive vs negative | 0.612 | 0.313 | 1.196 | 0.151 |
| HER2, positive vs negative | 0.978 | 0.507 | 1.885 | 0.946 |
| Histologic grade, 3 vs 1,2 | 1.406 | 0.793 | 2.492 | 0.243 |
| Lymphovascular invasion, positive vs negative | 2.525 | 1.315 | 4.851 | 0.005 |
| Age (years), >50 vs ≤50 | 1.150 | 0.599 | 2.210 | 0.674 |
| BMI (kg/m2), >25 vs ≤25 | 0.826 | 0.493 | 1.384 | 0.468 |
| Operation, mastectomy vs lumpectomy | 2.566 | 1.152 | 5.715 | 0.021 |
| Radiation therapy, yes vs no | 1.096 | 0.574 | 2.092 | 0.782 |
| Chemotherapy, yes vs no | 0.250 | 0.140 | 0.444 | <0.001 |
| Herceptin therapy, yes vs no | 0.438 | 0.093 | 2.064 | 0.297 |
| Endocrine therapy, yes vs no | 1.227 | 0.563 | 2.673 | 0.607 |
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio.
Mammographic Breast Density in Patients with Age >50 Years
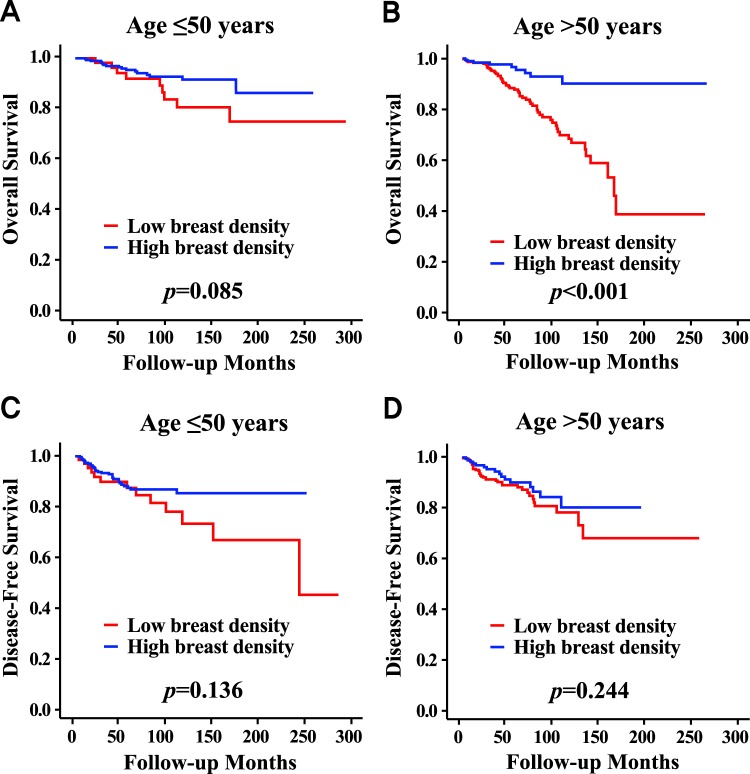
The high MBD group showed a higher overall survival than the low MBD group only in the subgroup aged >50 years (p < 0.001), while a survival difference was not observed between the two groups in the subgroup aged ≤50 years (Fig. 3). There were no survival differences between the two groups regardless of age subgroups in terms of disease-free survival. In the subgroup aged >50 years, the mean age of patients in the high MBD group was significantly lower than that of patients in the low MBD group (Table S1). The high MBD group showed a higher proportion of patients with BMI ≤ 25 kg/m2. In the subgroup aged >50 years, MBD was a significant independent prognostic factor by multivariable analysis (HR, 0.399; 95% CI, 0.181–0.881; Table S2).
Figure 3.
Survival curves according to mammographic breast density in patients with age ≤50 years and in patients with age >50 years. Overall survival curves according to mammographic breast density in patients with ≤50 years (A) and in patients with >50 years (B). Disease-free survival curves according to mammographic breast density in patients with ≤50 years (C) and in patients with >50 years (D).
Mammographic Breast Density and Age
In all subjects, MBD was closely related to age; as higher MBD was associated with lower mean age in terms of the four categories (two-sample t-test; all p < 0.001; Fig. S2A) and the two MBD groups (two-sample t-test; p < 0.001; Fig. S2B). Although the relationship between MBD and mean age was weak in the subgroup aged ≤50 years, it was strong in the subgroup aged >50 years (Fig. S2).
Discussion
In this study, we have shown that high MBD is associated with a superior prognosis compared to low MBD, and that MBD is a strong independent prognostic factor in operable primary invasive female breast cancer, especially in patients older than 50 years and with the HRc(+)/HER2(−) subtype. Among prior studies reporting on results regarding the relationship between MBD and breast cancer, most studies focused on the role of MBD as an etiologic factor. Only a limited number of published studies have reported on the role of MBD as a prognostic factor, but the results were inconsistent and controversial. Some papers have reported adverse effects of low MBD on breast cancer prognosis with results similar to the findings of this study. One study reported that patients with low MBD (<25%) showed worse prognosis compared to those with mixed breast density (>25%), and patients with very low MBD (<10%) showed the strongest significance compared to the remaining patients (HR, 3.275; 95% CI, 1.750–6.127)10. The authors also reported that patients with very low MBD (<10%) had a clinically worse disease-free survival compared to those with mixed MBD (>10%) by multivariable analysis (HR, 2.790; 95% CI, 1.724–4.516)11. Other papers reported the favorable prognostic effect of low MBD on breast cancer. One study reported that median progression-free survival in patients with low breast density (18.4 months; 95% CI, 14.9–22.2) was significantly better than that in patients with high breast density (9.3 months, 95% CI 8.5–13.6) with a p value of 0.00212. Another study reported that dense breast was significantly associated with an increased breast cancer-specific mortality (HR, 1.91; 95% CI, 1.26–2.91) compared to nondense breast13. However, another paper reported that there was no association between MBD and breast cancer prognosis. A study using data of Breast Cancer Surveillance Consortium (BCSC) reported that high MBD (BI-RADS 4) was not associated with breast cancer-specific survival (HR, 0.92; 95% CI, 0.71–1.19) or overall survival (HR, 0.83; 95% CI, 0.68–1.02) compared to low MBD (BI-RADS 2) by multivariable analysis14. A further study reported that MBD was not associated with breast cancer-specific survival (HR, 0.95; 95% CI, 0.79–1.15) or overall survival (HR, 1.08; 95% CI, 0.98–1.20)15. Eriksson et al. also reported that MBD was not associated with breast cancer-specific survival or overall survival in postmenopausal breast cancer patients16. However, the results of our study strongly support a favorable prognostic role of high MBD in terms of overall survival in breast cancer compared to low MBD.
The proposed mechanisms underlying the prognostic value of MBD could be explained by three factors, including clinicopathologic factors, treatment factors, and other factors. First, the high MBD group was associated with favorable factors such as younger age, lower BMI, and a higher proportion of patients with positive HRc or progesterone receptor. Second, the high MBD group could be associated with more active treatments. Although there were no differences in terms of tumor size, nodal positivity, and stage between the high MBD group and the low MBD group, the proportion of patients receiving adjuvant chemotherapy was higher in the high MBD group. Third, other factors could be associated with these results. After adjusting MBD with both clinicopathologic and treatment factors, MBD still remained a significant independent prognostic factor by multivariable analysis in terms of overall survival. This implies that factors other than clinicopathologic and treatment, could be significant effectors explaining this relationship. Socioeconomic status, exercise, dietary habit, health insurance, life style, for example, could be relevant contributors, but further studies would be needed in order to validate roles for these.
As all of the subjects in this study were Asian, racial differences should be considered. According to data from 3,865,070 screening mammography examinations interpreted by radiologists who participated in the BCSC, the proportions of fatty, fibroglandular, heterogeneously dense, and extremely dense breasts were about 10%, 40%, 40%, and 10%, respectively3. The majority of the study population in the BCSC were white (http://www.bcsc-research.org/). In our study, the proportions of fatty, fibroglandular, heterogeneously dense, and extremely dense breasts were approximately 15%, 30%, 35%, and 20%, respectively. BCSC data showed that high and low MBD accounted for 50% and 50%, respectively, but our data indicated that the proportions were approximately 45% and 55%, respectively. Asian women have been reported to have more dense breasts compared to white women. A previous study reported that the proportions of patients having extremely dense breasts were 27.1% and 12.5% in Asian and White women respectively, using data of 15,292 women without a history of breast cancer17. Another study also reported that HR for having dense breasts versus fatty breasts, comparing Asian to white women was 1.3 (95% CI, 1.2–1.5) after full adjustment using data of 28,501 women without a history of breast cancer18.
Although there is considerable variation, MBD changes inversely with age; younger women tend to have denser breasts compared to older women. A previous study reported that there was a significant inverse relationship between age and MBD (p < 0.001), and proportions of dense breast were 74%, 57%, 44%, and 36% for women in their 40 s, 50 s, 60 s, and 70 s, respectively19. Age is also closely related to breast cancer prognosis. Chen et al. analyzed 133,057 female breast cancer patients from 2004 to 2008 using the Surveillance, Epidemiology, and End Results database20. In our study, high MBD was strongly associated with younger age. The strong association between MBD and the age factor could be one of the major causalities behind better prognosis with high MBD.
Obesity has been reported to be a poor prognostic factor in breast cancer. Obesity increases the risk of breast cancer recurrence and death by approximately 35–40% and this is most clearly established for estrogen receptor-positive breast cancer21. A previous study reported that high BMI was an independent prognostic factor in breast cancer for worse outcomes with respect to overall survival (p = 0.03)22. Chan et al. reported the most recent and extensive meta-analysis results using 213,075 patients from 82 studies. They reported that the summary relative risks for total mortality and breast cancer–specific mortality for obese versus normal-weight patients at baseline were 1.41 (95% CI, 1.29–1.53) and 1.35 (95% CI, 1.24–1.47), respectively23. In this study, low MBD was strongly associated with high BMI and it could partly explain the worse prognosis found in the low MBD group.
In this study, high MBD showed higher overall survival rates in all subjects, but this was found only in patients older than 50 years on subgroup analyses. This finding could be one of the main reasons for the prognostic effect of MBD only in patients with age >50 years in this study. Multivariable analysis revealed similar findings, showing that MBD was a significant independent prognostic factor in both unselected breast cancer patients and breast cancer patients with age >50 years, but not in patients with age ≤50 years. According to breast cancer subtypes, MBD was a significant prognostic factor only in the HRc(+)/HER2(−) subtype. Subgroup analyses revealed that the prognostic impact of MBD was more prominent in the subgroup with positive estrogen receptor, positive progesterone receptor, or negative HER2 compared to negative estrogen receptor, negative progesterone receptor, or positive HER2, respectively. The prognostic influence of MBD was different across subtypes of breast cancer, and it was observed only in the HRc(+)/HER2(−) subtype.
Low MBD was significantly associated with higher regional recurrence and lower contralateral breast cancer development, but was not associated with local recurrence or distant recurrence. As a whole, MBD was not a significant factor with respect to disease-free survival, and breast cancer recurrence and therefore MBD is considered to be a minor prognostic factor in our study. Previous papers have reported that high MBD was closely associated with increased locoregional recurrence, but not with distant recurrence24–26. Eriksson et al. reported that in postmenopausal patients, breast cancer originating in dense breasts (≥25%) was associated with higher local recurrence (HR, 1.92; p = 0.039) and locoregional recurrence (HR, 1.67; p = 0.033) compared to patients with less dense breasts (25% density), but it was not associated with distant recurrence16. A previous study reported that dense breast was associated with an increased risk of contralateral breast cancer development (HR, 1.80; 95% CI, 1.22–2.64) compared to nondense breast27.
This study has limitations. First, this was a retrospective cohort study including a relatively small number of subjects, and therefore limited statistical power particularly for subgroup analysis. Second, the main concern of this study was the prognostic influence of preoperative mammographic breast density in operable invasive female breast cancer and we selected the subjects accordingly. Selection bias could be a limitation of this study which can occur as a result of excluding relatively large numbers of subjects. We excluded patients with stage 0 or stage IV as initial diagnosis, patients who received neoadjuvant chemotherapy, patients diagnosed as malignant phyllodes tumor, male patients, patients less than 20 or more than 90 years old, and patients with insufficient information for this study. Third, MBD data has limitations. All data for MBD were obtained from the Boramae Hospital Breast Cancer Registry database based on the mammogram report which was made by single radiologist with no consensus. Although all radiologists who had been involved in interpretation of MBD were, or are, faculty members of our hospital as professors in the Department of Radiology specializing in breast cancer, MBD data were not reviewed independently by radiologist(s) in a controlled manner. Interpretation of MBD in this study was based on visual qualitative analysis which is considered less accurate than quantitative or automated measurements. There was no adjustment between analog mammography films and digital mammography. Fourth, the results of breast cancer-specific survival were not presented in this study, as data for this analysis were not available. Fifth, the change in the prognostic effect of MBD according to different time points was not evaluated in this study and further study is needed to investigate this parameter. Sixth, the recruitment period is relatively long, and there could be biases associated with this variable. There have been chronologic changes in basic clinicopathologic features, diagnostic methods, treatment modalities, and other factors associated with prognosis. Lastly, as this study was based on the Boramae Hospital Breast Cancer Registry database which had limited clinicopathologic information, some important factors could not be analyzed directly. For example, as the registry had no information regarding menopausal status, we analyzed age subgroups with arbitrary cut-off value of 50 years which surrogates for the menopausal status of the subjects. Additionally, although MBD was adjusted with 14 factors including 9 clinicopathologic factors and 5 treatment factors, there could be still other possible confounding factors which were not analyzed in this study.
In conclusion, the high MBD group was associated with superior overall survival rates. Preoperative MBD was a strong independent prognostic factor in operable primary invasive female breast cancer, especially in patients with age >50 years and the HRc(+)/HER2(−) subtype. Favorable clinicopathologic features, active treatments, and other factors could contribute to this causality. Large scale, well designed studies are needed in the near future to validate the relationship between MBD and breast cancer prognosis.
Ethical Statement
The institutional review boards approved this study (Seoul Metropolitan Government Seoul National University Boramae Medical Center, 16-2017-70) and performed in accordance with the principles of the Declaration of Helsinki. The informed consent of this study was waived.
Electronic supplementary material
Acknowledgements
We appreciate valuable discussion from the members of the Boramae hospital Breast cancer Study group (BBS).
Ki-Tae Hwang, MD, PhD1, Bo Kyung Koo, MD, PhD2, Young A Kim, MD, PhD3, Jongjin Kim, MD1, Eun Youn Roh, MD, PhD4, Sung Bae Park, MD5, Jin Hyun Park, MD, MS2, Han Mo Sung, RN1, Bumjo Oh, MD6, So Won Oh, MD, PhD7, Sohee Oh, PhD8, Jong Yoon Lee, MD, MS9, Ji Hyun Chang, MD, PhD10, Se Hee Jung, MD, PhD11, Young Jun Chai, MD, MS1, In Sil Choi, MD, PhD2, A Jung Chu, MD9, Kyu Ri Hwang, MD, PhD12, Seong-Hye Hwang, PhD1.
1Department of Surgery; 2Department of Internal Medicine; 3Department of Pathology; 4Department of Laboratory Medicine; 5Department of Neurosurgery; 6Department of Family Medicine; 7Department of Nuclear Medicine; 7Department of Biostatistics; 7Department of Radiology; 10Department of Radiation Oncology; 11Department of Rehabilitation Medicine; 12Department of Obstetrics and Gynecology.
All BBS members are from Seoul Metropolitan Government Seoul National University Boramae Medical Center (39, Boramae-Gil, Dongjak-gu, Seoul, 156–707, Republic of Korea). We would like to thank Young Wook Ju and Jung Hyun Park for data collection for this study
Author Contributions
K.T.H. conceived, designed, and supervised the study. A.J.C., J.K., J.Y.L. and Y.A.K. collected and assembled data. K.T.H., A.J.C., J.H.C., S.O., J.J. and B.O. analyzed data and interpreted the results. K.T.H. and A.J.C. wrote the manuscript. All authors reviewed and approved the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ki-Tae Hwang and A. Jung Chu contributed equally.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-34297-8.
References
- 1.Wolfe JN. Breast patterns as an index of risk for developing breast cancer. AJR Am J Roentgenol. 1976;126:1130–7. doi: 10.2214/ajr.126.6.1130. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe JN. Risk for breast cancer development determined by mammographic parenchymal pattern. Cancer. 1976;37:2486–92. doi: 10.1002/1097-0142(197605)37:5<2486::AID-CNCR2820370542>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 3.Sickles E. A. et al. ACR BI-RADS Mammography. In: D’Orsi, C.J., Sickles, E.A., Mendelson, E.B., Morris, E.A., et al. ACR BI-RADS Atlas, Breast Imaging Reporting and Data System. Reston, VA: American College of Radiology (2013).
- 4.Thurfjell E. Breast density and the risk of breast cancer. N Engl J Med. 2002;347:866. doi: 10.1056/NEJMp020093. [DOI] [PubMed] [Google Scholar]
- 5.McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1159–69. doi: 10.1158/1055-9965.EPI-06-0034. [DOI] [PubMed] [Google Scholar]
- 6.Boyd NF, et al. Mammographic breast density as an intermediate phenotype for breast cancer. Lancet Oncol. 2005;6:798–808. doi: 10.1016/S1470-2045(05)70390-9. [DOI] [PubMed] [Google Scholar]
- 7.Boyd NF, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356:227–36. doi: 10.1056/NEJMoa062790. [DOI] [PubMed] [Google Scholar]
- 8.Nyante SJ, et al. Prognostic significance of mammographic density change after initiation of tamoxifen for ER-positive breast cancer. J Natl Cancer Inst. 2015;107:dju425. doi: 10.1093/jnci/dju425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li J, et al. Mammographic density reduction is a prognostic marker of response to adjuvant tamoxifen therapy in postmenopausal patients with breast cancer. J Clin Oncol. 2013;31:2249–56. doi: 10.1200/JCO.2012.44.5015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Masarwah A, et al. Very low mammographic breast density predicts poorer outcome in patients with invasive breast cancer. Eur Radiol. 2015;25:1875–82. doi: 10.1007/s00330-015-3626-2. [DOI] [PubMed] [Google Scholar]
- 11.Masarwah A, et al. Prognostic contribution of mammographic breast density and HER2 overexpression to the Nottingham Prognostic Index in patients with invasive breast cancer. BMC Cancer. 2016;16:833. doi: 10.1186/s12885-016-2892-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elsamany S, et al. Prognostic value of mammographic breast density in patients with metastatic breast cancer. Med Oncol. 2014;31:96. doi: 10.1007/s12032-014-0096-3. [DOI] [PubMed] [Google Scholar]
- 13.Chiu SY, et al. Effect of baseline breast density on breast cancer incidence, stage, mortality, and screening parameters: 25-year follow-up of a Swedish mammographic screening. Cancer Epidemiol Biomarkers Prev. 2010;19:1219–28. doi: 10.1158/1055-9965.EPI-09-1028. [DOI] [PubMed] [Google Scholar]
- 14.Gierach GL, et al. Relationship between mammographic density and breast cancer death in the Breast Cancer Surveillance Consortium. J Natl Cancer Inst. 2012;104:1218–27. doi: 10.1093/jnci/djs327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maskarinec G, et al. Mammographic density as a predictor of breast cancer survival: the Multiethnic Cohort. Breast Cancer Res. 2013;15:R7. doi: 10.1186/bcr3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eriksson L, Czene K, Rosenberg L, Humphreys K, Hall P. Possible influence of mammographic density on local and locoregional recurrence of breast cancer. Breast Cancer Res. 2013;15:R56. doi: 10.1186/bcr3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.del Carmen MG, et al. Mammographic breast density and race. AJR Am J Roentgenol. 2007;188:1147–50. doi: 10.2214/AJR.06.0619. [DOI] [PubMed] [Google Scholar]
- 18.El-Bastawissi AY, White E, Mandelson MT, Taplin S. Variation in mammographic breast density by race. Ann Epidemiol. 2001;11:257–63. doi: 10.1016/S1047-2797(00)00225-8. [DOI] [PubMed] [Google Scholar]
- 19.Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. AJR Am J Roentgenol. 2012;198:W292–5. doi: 10.2214/AJR.10.6049. [DOI] [PubMed] [Google Scholar]
- 20.Chen HL, Zhou MQ, Tian W, Meng KX, He HF. Effect of Age on Breast Cancer Patient Prognoses: A Population-Based Study Using the SEER 18 Database. PLoS One. 2016;11:e0165409. doi: 10.1371/journal.pone.0165409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiralerspong S, Goodwin PJ. Obesity and Breast Cancer Prognosis: Evidence, Challenges, and Opportunities. J Clin Oncol. 2016;34:4203–16. doi: 10.1200/JCO.2016.68.4480. [DOI] [PubMed] [Google Scholar]
- 22.Berclaz G, et al. Body mass index as a prognostic feature in operable breast cancer: the International Breast Cancer Study Group experience. Ann Oncol. 2004;15:875–84. doi: 10.1093/annonc/mdh222. [DOI] [PubMed] [Google Scholar]
- 23.Chan DS, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25:1901–14. doi: 10.1093/annonc/mdu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cil T, et al. Mammographic density and the risk of breast cancer recurrence after breast-conserving surgery. Cancer. 2009;115:5780–7. doi: 10.1002/cncr.24638. [DOI] [PubMed] [Google Scholar]
- 25.Park CC, Rembert J, Chew K, Moore D, Kerlikowske K. High mammographic breast density is independent predictor of local but not distant recurrence after lumpectomy and radiotherapy for invasive breast cancer. Int J Radiat Oncol Biol Phys. 2009;73:75–9. doi: 10.1016/j.ijrobp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Huang YS, et al. High mammographic breast density predicts locoregional recurrence after modified radical mastectomy for invasive breast cancer: a case-control study. Breast Cancer Res. 2016;18:120. doi: 10.1186/s13058-016-0784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raghavendra A, et al. Mammographic breast density is associated with the development of contralateral breast cancer. Cancer. 2017;123:1935–40. doi: 10.1002/cncr.30573. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.