Abstract
Purpose
We investigated correlations between the findings of oral examinations and panoramic radiography in order to determine the efficacy of using panoramic radiographs in screening examinations.
Methods
This study included patients who visited dental clinics at National Health Insurance Service (NHIS) Ilsan Hospital for checkups during 2009–2015 and underwent panoramic radiographic examinations within 1 year prior to the oral examinations. Among the 48,006 patients who received checkups, 1,091 were included in this study. The data were evaluated using the Cohen kappa and interrater agreement coefficients. Accuracy, sensitivity, and specificity were calculated using data from the panoramic radiographs as true positive diagnoses.
Results
The interrater agreement coefficient for occlusal caries was 28.8%, and the Cohen kappa coefficient was 0.043 between the oral and panoramic radiographic examinations. Root caries and subgingival calculus were only found on the radiographs, while gingival inflammation was found only by the oral examinations. The oral examinations had a specificity for detecting occlusal dental caries of 100%, while their sensitivity for proximal dental caries and supragingival calculus was extremely low (14.0% and 18.3%, respectively) compared to the panoramic radiographic examinations. The oral examinations showed a relatively low sensitivity of 66.2% and a specificity of 43.7% in detecting tooth loss compared with panoramic radiography.
Conclusions
Panoramic radiography can provide information that is difficult to obtain in oral examinations, such as root caries, furcation involvement, and subgingival calculus, which are factors that can directly affect the survival rate of teeth. It therefore seems reasonable and necessary to add panoramic radiography to large-scale health checkup programs such as that provided by the NHIS.
Keywords: Dental radiography, Diagnosis, National Health Program, Panoramic radiography
Graphical Abstract
INTRODUCTION
Many people are not aware of the condition of their oral cavity because they do not receive regular dental checkups, which can be due to a busy working life or, in some cases, dental phobia. This situation can result in periodontal or other dental diseases worsening with time [1,2,3].
The Korean National Health Insurance Service (NHIS) provides health checkups with the aim of disease prevention and early detection in order to prevent its further advancement. The NHIS was initiated to improve public health and promote social security by paying insurance benefits in 1963, and implemented medical insurance for workplaces with at least 500 workers in 1977. The national health checkups consist of general checkups, lifetime transition period health checkups, cancer checkups, and baby and infant health checkups. A general checkup is provided biannually to employee subscribers and their dependents, as well as regional insurance subscribers and their dependents, and it is fully paid for by corporations. The checkup includes an interview examination and posture test, a chest X-ray, a blood test, a urine test, and an oral checkup. The oral examination is performed through a visual inspection and questionnaires. However, a radiographic examination is not included, which can prevent precise diagnoses. In particular, detecting certain dental issues, such as bone resorption and secondary caries, is very difficult through an oral examination.
Dental panoramic radiography was developed by Y.V. Paatero in 1945 and remains in widespread use for dental diagnoses [4]. The Food and Drug Administration published guidelines in 2012 for radiological examinations in dentistry [5]. Given the desirability of low doses of dental irradiation, panoramic radiography is suitable for general oral examinations [6]. Early panoramic radiographs were not sufficiently accurate to replace standard X-rays, but the spatial resolution of panoramic radiographs has improved recently, making them effective for detecting various dental diseases such as periodontitis, dental caries, and temporomandibular joint disorder [7,8,9]. It is now recommended that panoramic radiographs be obtained every 18 to 36 months in patients who visit dental clinics for regular checkups [10].
Shin et al. [11] reported that panoramic radiographs increased the diagnosis rates of dental caries and periodontal disease by 23.1% and 31.9%, respectively. In addition, Ha et al. [12] reported that panoramic radiography was cost-effective for periodontal disease screening in adults aged 40 years in Korea. Nonetheless, there is still insufficient evidence and reports on the efficacy of using panoramic radiography in large-scale oral examination programs.
The aim of this study was to compare panoramic radiography with oral examinations and to determine the efficacy of combining panoramic radiographs with the oral examinations performed for NHIS health checkups.
MATERIALS AND METHODS
Setting and the study group
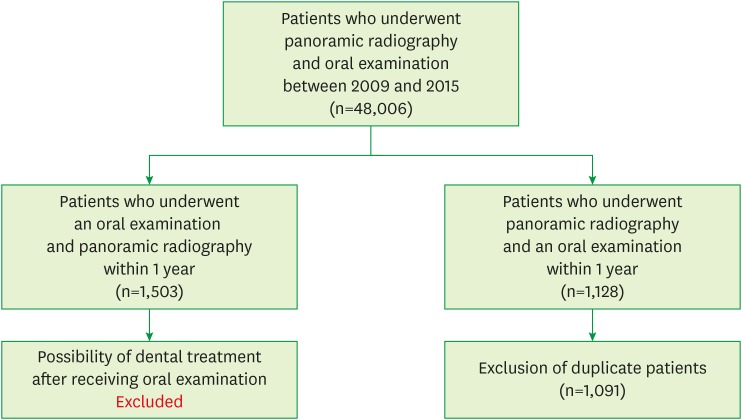
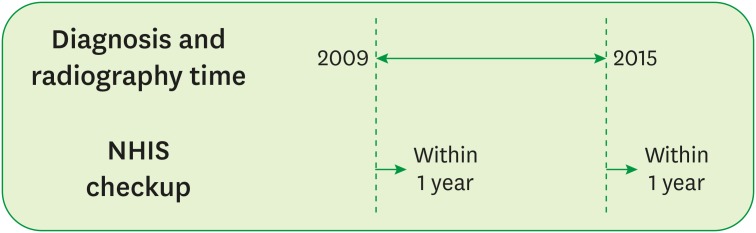
Among 48,006 patients who underwent an oral examination as part of the NHIS checkups at NHIS Ilsan Hospital between 2009 and 2015, preceded by panoramic radiography within 1 year (Figure 1), 1,091 were included in this study after excluding redundancy (Figure 2).
Figure 1. Study flow diagram of patient inclusion.
Figure 2. Relationship between the timing of NHIS health checkups and panoramic radiography.
NHIS: National Health Insurance Service.
Research data – measurements
Oral examinations were carried out randomly by dentists who had graduated from dental colleges and had become licensed within the previous 1 year. These examinations formed part of their routine national examinations. Dental caries (including proximal caries and caries-associated conditions such as tooth restoration and lost teeth), the presence of gingival inflammation, and the presence of calculus were detected in the examinations.
Panoramic radiographs were obtained by a radiologist (Orthopantomograph® OP100 D, General Electric Company, Helsinki, Finland) and interpreted by dentists who had graduated from dental colleges and had become licensed within the previous 1 year. Dental caries (divided into root, proximal, and occlusal), the presence or absence of calculus (divided into supragingival and subgingival), loss of teeth, furcation involvement, and maximum bone loss height were examined. This study was approved by the ethics committee of NHIS Ilsan Hospital (IRB No. 2016-03-010).
Statistical analysis
Data were evaluated using SAS software (SAS version 9.2, SAS Institute Inc., Cary, NC, USA). Interrater reliability was evaluated using the interrater agreement coefficient and the Cohen kappa coefficient. The interrater agreement coefficient was calculated using the intra-class correlation coefficient between data obtained by oral examinations and by radiographic analysis. The Cohen kappa coefficient accounts for the random-chance occurrence of interrater agreement and was calculated using the following equation:
Where PA is the relative observed agreement between measurements obtained by oral examinations and by radiographic analysis and PC is the hypothetical probability of chance agreement.
Accuracy, sensitivity, and specificity were calculated using the data from the panoramic radiographs as true positive diagnoses. Several additional concepts are commonly used as part of the description of sensitivity, specificity, and accuracy: true positive (TP), true negative (TN), false negative (FN), and false positive (FP).
Sensitivity, specificity and accuracy are described in terms of TP, TN, FN, and FP.
| Sensitivity = TP/(TP + FN) = (Number of true positive assessments)/(Number of all positive assessments) |
| Specificity = TN/(TN + FP) = (Number of true negative assessments)/(Number of all negative assessments) |
| Accuracy = (TN + TP)/(TN+TP+FN+FP) = (Number of correct assessments)/(Number of all assessments) |
RESULTS
Composition of the study group
The patients included in this study comprised 449 (41.2%) males and 642 (58.8%) females. Their mean age was 56.8 years (range, 23–94 years), and those aged in their 60s constituted the largest proportion by decade (28.6%). (Table 1).
Table 1. Characteristics of the patient population.
| Characteristic | Value | |
|---|---|---|
| Total | 1,091 | |
| Sex | ||
| Male | 449 (41.2) | |
| Female | 642 (58.8) | |
| Age, mean (range) (yr) | 56.8 (23–94) | |
| 20–29 | 20 (1.4) | |
| 30–39 | 115 (8.6) | |
| 40–49 | 202 (17.1) | |
| 50–59 | 304 (23.7) | |
| 60–69 | 211 (28.6) | |
| 70–79 | 179 (7.1) | |
| ≥80 | 57 (5.8) | |
Data are number (%) values except where indicated otherwise.
Results of oral examination via panoramic radiography
The findings of the oral examinations and panoramic radiography are presented in Table 2. Occlusal caries were detected in 14.4% of oral examinations, but only on 7.6% of the panoramic radiographs. The coefficient for the interrater agreement between these 2 types of examination was only 28.8%, and the Cohen kappa coefficient was 0.043. Proximal caries were found in 12.4% of oral examinations, but only on 9.2% of the radiographs. The interrater agreement coefficient was higher in this case, at 31.9%. However, the Cohen kappa coefficient was negative (−0.34), indicating the absence of any correlation. Root caries were found in 14.1% of the subjects on the panoramic radiographs, but were not found in the oral examinations. Gingival inflammation was found in 21.3% of the oral examinations, but the degree of gingival inflammation could not be detected radiographically. The Cohen kappa coefficient was negative (−0.026), also indicating the absence of any correlation. Supragingival calculus was evident in 19.7% of oral examinations and on 16.6% of the radiographs. The concordance rate was high (63.7%), but the kappa value indicated only slight agreement (0.022). However, subgingival calculus was not found in the oral examinations, while it was found on 18.4% of the panoramic radiographs, which was higher than the rate of supragingival calculus. Panoramic radiography revealed that 59.2% of the study group had lost teeth, while the oral examinations showed that 39.0% of the study group had lost teeth. The agreement rate was low, at 25%. Finally, the marginal bone loss rate was 64.1% and the furcation involvement rate was 38.4%.
Table 2. Comparison between the findings of oral examinations and panoramic radiography.
| Variable | Oral examination (%) | Panoramic radiography (%) | Interrater agreement coefficient (%) | Cohen kappa coefficient | ||
|---|---|---|---|---|---|---|
| Caries | ||||||
| Occlusal | 14.4 | 7.6 | 28.8 | 0.043 | ||
| Proximal | 12.4 | 9.2 | 31.9 | −0.342 | ||
| Root | - | 14.1 | ||||
| Gingival disease | ||||||
| Inflammation | 21.3 | - | 39.8 | −0.026 | ||
| Calculus | ||||||
| Supragingival | 19.7 | 16.6 | 63.7 | 0.022 | ||
| Subgingival | - | 18.4 | ||||
| Marginal bone loss | - | 64.1 | ||||
| Furcation involvement | - | 38.4 | ||||
| Missing tooth | 39.0 | 59.2 | 25.0 | 0.089 | ||
Accuracy, sensitivity, and specificity of oral examinations based on panoramic radiography
The accuracy, sensitivity, and specificity of oral examinations were evaluated based on the findings of panoramic radiography (Table 3). The probability of finding occlusal dental caries in an oral examination was only 48.2%. If no dental caries were found, the probability of there actually being no caries at the time of the oral examination was 100%. However, in the case of suspected proximal dental caries, the probability of finding the caries in the presence of actual dental caries was only 14.0%, and the probability of having no caries was 89.2%. This suggests that the probability of diagnosing dental caries suspected in an oral examination is actually very low. The accuracy was 84.4% for occlusal dental caries and 82.5% for proximal dental caries. The probability of discriminating the presence of calculus was only 18.3%, while the specificity was 83.7%. The sensitivity for periodontal disease was very low, while the specificity was very high.
Table 3. Accuracy, sensitivity, and specificity of oral examinations using panoramic radiography as the reference.
| Variable | Accuracy (%) | Sensitivity (%) | Specificity (%) | ||
|---|---|---|---|---|---|
| Caries | |||||
| Occlusal | 84.4 | 48.2 | 100 | ||
| Proximal | 82.5 | 14.0 | 89.2 | ||
| Gingival disease | |||||
| Calculus | |||||
| Supragingival | 63.7 | 18.3 | 83.7 | ||
| Missing tooth | 52.2 | 66.2 | 43.7 | ||
DISCUSSION
The oral examinations included in NHIS health checkups consist of questionnaires and visual inspections by dentists. However, some parts of the oral anatomy are covered with soft tissue, and it is easy to underestimate oral diseases such as periodontal disease [13] in their early stages. This means that visual inspections are insufficient for detecting various oral diseases that affect the subgingival tissue and are obscured by tooth enamel. It may therefore be helpful to obtain additional information using other diagnostic methods or tools.
The panoramic radiographs obtained in the present study provided information on periodontal disease, such as marginal bone loss and furcation involvement, that cannot be detected in visual inspections. The prevalence rates of marginal bone loss and furcation involvement were 62.0% and 37.1%, respectively, meaning that a large proportion of the subjects had a history of periodontitis or were currently affected by periodontitis.
Periodontal disease is defined as an inflammatory chronic disease caused by bacteria. The bacteria present in teeth and calculus irritate the gingiva, further destroying periodontal tissue and potentially progressing to periodontitis [14]. Therefore, plaque and dental calculus are the most common causes of periodontal disease as local factors. In particular, subgingival calculus in populations with poor hygiene can act as a bacterial reservoir and is associated with the loss of periodontal attachments [15]. In the present oral examinations, subgingival calculus was seen in 16.8% of patients, and panoramic radiographs showed it in 16.0%. However, the interrater-agreement coefficient was only 63.7%. Visual inspections have limitations in detecting subgingival calculus, which represents a critical drawback of the NHIS health checkups.
The number of patients diagnosed and treated for periodontitis in Korea is increasing by 16.7% annually, and 22% of the Korean population was treated for periodontitis covered by the NHIS in 2013 [16]. It is reasonable to assume that more patients may have undetected periodontal disease. Detecting subgingival calculus appears to help to reduce the prevalence of periodontal disease. However, supragingival dental calculus is mainly observed in oral examinations, whereas subgingival dental calculus is only detected on panoramic radiography; this difference means that the 2 methods can be used synergistically.
Gingival inflammation is easily detected in oral examinations, and it requires additional periodontal treatment. Therefore, the sensitivity and specificity are low compared with cases of periodontal disease that are suspected to involve alveolar bone resorption. If the inflammation is not evident on a panoramic radiograph, it can be expected to be gingivitis or mild periodontitis without any alveolar bone resorption. In other words, the presence of alveolar bone resorption on a panoramic radiograph needs to be followed up with further dental surveillance.
The prevalence rates of occlusal dental caries and proximal dental caries were 14.5% and 11.1% in the oral examinations performed in this study, while the corresponding rates on panoramic radiography were 7.4% and 8.9%. This difference occurred because occlusal dental caries are not evident on panoramic radiographs. However, the presence of proximal dental caries cannot be confirmed in a short oral examination. Proximal dental caries were present on panoramic radiographs in 9.2% of patients, and Table 2 indicates that the coefficient for the interrater agreement between the 2 methods was 0%. This means that the reliability of detecting proximal dental caries is very low. Dental caries appearing on panoramic radiographs can only be confirmed through visual inspection once significant deterioration is present [17], which means that visual inspections miss a large proportion of cases of proximal caries.
The prevalence of root caries was 13.7% in the present study, which is similar to previously reported rates ranging from 11.9% to 28.0% [18]. Root caries are a major cause of tooth loss in older adults [19] and so the detection of root caries is important for maintaining oral health. The sensitivity of detecting dental caries via panoramic radiography is about 60%. Although oral examinations may be more effective for the early treatment of dental caries, panoramic radiography is more effective if the aim is to prevent tooth loss, since occlusal dental caries, proximal dental caries, and root caries can be detected.
This study also investigated the accuracy of oral examinations, using panoramic radiography with objective criteria as the reference. Some parts of panoramic radiographs can serve as appropriate criteria. Since panoramic radiography has low sensitivity but high specificity, a detected lesion will certainly exist, and in some cases the disease will show significant progression.
The oral examinations revealed that 37.8% of patients had missing teeth, compared to the finding of 60.0% when using panoramic radiography, and the interrater agreement coefficient was only 25.0%. It is challenging for a dentist to confirm clinical conditions such as molar impaction through a quick visual inspection [20], and it is often difficult to make a precise diagnosis because of variables such as the third molar and supernumerary teeth [21]. Panoramic radiographs could be used as a reference in cases of missing teeth. The accuracy (52.2%), sensitivity (66.2%), and specificity (43.7%) of the oral examinations were all low, which confirms the difficulty of identifying missing teeth in an oral examination. In addition, because these statistics were based on the number of patients, sensitivity and specificity are expected to be lower when tested at the tooth level. Diagnosing tooth loss is the most important factor in oral reconstruction, and accurate information should be obtained. Panoramic radiographs act as a key reference for detecting tooth loss. Despite the limitations of this study (as described below), we were able to identify that oral examinations had insufficient sources of information, which could be a critical drawback of NHIS checkups. Since most oral examinations are performed in adults, prosthetic restorations for lost teeth must be accompanied by aesthetic and functional recovery. This situation provides a strong rationale for inspecting panoramic radiographs in health checkups.
Various types of information can be obtained through oral examinations, including determining whether patients are performing good oral hygiene management and whether they have had regular dental checkups. However, this information is used only to determine the most basic aspects of treatment. In contrast, panoramic radiography can detect lesions that may be directly related to tooth loss by detecting ongoing dental caries, subgingival dental calculus, and alveolar bone resorption [17,22,23,24], and it can also be used for prosthodontic planning. Thus, beyond the current level of determining the basic treatment needed, including panoramic radiography in the screening program may make it possible to increase the tooth survival rate in the short term and to reduce the cost of restorations or reconstruction of teeth such as implants and dentures in the long term [25].
The first limitation of this study was its retrospective design. In addition, the study was conducted during 2009–2015 in dental clinics at NHIS Ilsan Hospital, and so the distribution of the study cohort may have been limited to a small region. Another potential limitation is that the period between the panoramic radiography and oral examinations was up to 1 year, making it likely that the patients were also treated at other dental clinics; it is possible that diseases had progressed over this 1-year period. Finally, the quality of diagnoses performed by dentists using panoramic radiographs may have varied.
In conclusion, panoramic radiographs can provide information that is difficult to obtain from oral examinations, such as information about subgingival calculus, root caries, and furcation involvement, which are key factors for the tooth survival rate. Panoramic radiography can therefore be helpful for improving the screening of oral disease in NHIS health checkups.
Footnotes
Funding: This work was supported by National Health Insurance Service (NHIS) in Korea.
Author Contributions: Conceptualization: Young-Taek Kim; Data curation: Tae-mi Youk, Yong-Taek Kim, Helen Hyein Kweon; Formal analysis: Helen Hyein Kweon, Bo-Ah Lee; Investigation: Young-Taek Kim, Helen Hyein Kweon, Bo-Ah Lee; Methodology: Young-Taek Kim, Tae-mi Youk, Helen Hyein Kweon, Bo-Ah Lee; Project administration: Young-Taek Kim; Writing - original draft: Helen Hyein Kweon, Bo-Ah Lee, Tae-mi Youk; Writing - review & editing: Helen Hyein Kweon, Bo-Ah Lee, Young-Taek Kim.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Armfield JM, Spencer AJ, Stewart JF. Dental fear in Australia: who's afraid of the dentist? Aust Dent J. 2006;51(1):78–85. doi: 10.1111/j.1834-7819.2006.tb00405.x. [DOI] [PubMed] [Google Scholar]
- 2.Schuller AA, Willumsen T, Holst D. Are there differences in oral health and oral health behavior between individuals with high and low dental fear? Community Dent Oral Epidemiol. 2003;31(2):116–121. doi: 10.1034/j.1600-0528.2003.00026.x. [DOI] [PubMed] [Google Scholar]
- 3.Armfield J. The avoidance and delaying of dental visits in Australia. Aust Dent J. 2012;57(2):243–247. doi: 10.1111/j.1834-7819.2012.01697.x. [DOI] [PubMed] [Google Scholar]
- 4.Hallikainen D. History of panoramic radiography. Acta Radiol. 1996;37(3 Pt 2):441–445. doi: 10.1177/02841851960373P207. [DOI] [PubMed] [Google Scholar]
- 5.American Dental Association. Dental radiographic examinations: recommendations for patient selection and limiting radiation exposure [Internet] Chicago, IL: American Dental Association; 2012. [cited 2016 Aug 26]. Available from: https://www.ada.org/~/media/ADA/Member%20Center/FIles/Dental_Radiographic_Examinations_2012.pdf. [Google Scholar]
- 6.Cohnen M, Kemper J, Möbes O, Pawelzik J, Mödder U. Radiation dose in dental radiology. Eur Radiol. 2002;12(3):634–637. doi: 10.1007/s003300100928. [DOI] [PubMed] [Google Scholar]
- 7.Farman AG, Horner K. There are good reasons for selecting panoramic radiography to replace the intraoral full-mouth series. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):653–654. doi: 10.1067/moe.2002.129766. [DOI] [PubMed] [Google Scholar]
- 8.Rushton VE, Horner K, Worthington HV. Aspects of panoramic radiography in general dental practice. Br Dent J. 1999;186(7):342–344. doi: 10.1038/sj.bdj.4800098. [DOI] [PubMed] [Google Scholar]
- 9.Rushton VE, Horner K, Worthington HV. Routine panoramic radiography of new adult patients in general dental practice: relevance of diagnostic yield to treatment and identification of radiographic selection criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(4):488–495. doi: 10.1067/moe.2002.121994. [DOI] [PubMed] [Google Scholar]
- 10.American Dental Association Council on Scientific Affairs. The use of dental radiographs: update and recommendations. J Am Dent Assoc. 2006;137(9):1304–1312. doi: 10.14219/jada.archive.2006.0393. [DOI] [PubMed] [Google Scholar]
- 11.Shin MJ, Choi BR, Huh KH, Yi WJ, Heo MS, Lee SS, et al. Usefullness of panoramic radiograph for the improvement of periodic oral examination. Korean Journal of Oral and Maxillofacial Radiology. 2010;40:25–32. [Google Scholar]
- 12.Ha JE, Jin BH, Kim TI, Lee SS, Paik DI, Bae KH. A cost-benefit analysis of dental panoramic radiography for periodontal disease screening. J Korean Acad Oral Health. 2011;35:466–473. [Google Scholar]
- 13.Hirschmann PN. Radiographic interpretation of chronic periodontitis. Int Dent J. 1987;37(1):3–9. [PubMed] [Google Scholar]
- 14.Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4(1):1–6. doi: 10.1902/annals.1999.4.1.1. [DOI] [PubMed] [Google Scholar]
- 15.White DJ. Dental calculus: recent insights into occurrence, formation, prevention, removal and oral health effects of supragingival and subgingival deposits. Eur J Oral Sci. 1997;105(5 Pt 2):508–522. doi: 10.1111/j.1600-0722.1997.tb00238.x. [DOI] [PubMed] [Google Scholar]
- 16.Kim J, Son M. National Health Insurance Statistical Yearbook. Seoul, Korea. National Health Insurance Service. 2014;2011:5–34. [Google Scholar]
- 17.Douglass CW, Valachovic RW, Wijesinha A, Chauncey HH, Kapur KK, McNeil BJ. Clinical efficacy of dental radiography in the detection of dental caries and periodontal diseases. Oral Surg Oral Med Oral Pathol. 1986;62(3):330–339. doi: 10.1016/0030-4220(86)90017-4. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigues JA, Lussi A, Seemann R, Neuhaus KW. Prevention of crown and root caries in adults. Periodontol 2000. 2011;55(1):231–249. doi: 10.1111/j.1600-0757.2010.00381.x. [DOI] [PubMed] [Google Scholar]
- 19.Gregory D, Hyde S. Root caries in older adults. J Calif Dent Assoc. 2015;43(8):439–445. [PubMed] [Google Scholar]
- 20.Rushton VE, Horner K, Worthington HV. Screening panoramic radiology of adults in general dental practice: radiological findings. Br Dent J. 2001;190(9):495–501. doi: 10.1038/sj.bdj.4801014. [DOI] [PubMed] [Google Scholar]
- 21.Brook AH. Dental anomalies of number, form and size: their prevalence in British schoolchildren. J Int Assoc Dent Child. 1974;5(2):37–53. [PubMed] [Google Scholar]
- 22.Updegrave WJ. The role of panoramic radiography in diagnosis. Oral Surg Oral Med Oral Pathol. 1966;22(1):49–57. doi: 10.1016/0030-4220(66)90141-1. [DOI] [PubMed] [Google Scholar]
- 23.Tugnait A, Clerehugh V, Hirschmann PN. The usefulness of radiographs in diagnosis and management of periodontal diseases: a review. J Dent. 2000;28(4):219–226. doi: 10.1016/s0300-5712(99)00062-7. [DOI] [PubMed] [Google Scholar]
- 24.Feldens CA, Tovo MF, Kramer PF, Feldens EG, Ferreira SH, Finkler M. An in vitro study of the correlation between clinical and radiographic examinations of proximal carious lesions in primary molars. J Clin Pediatr Dent. 2003;27(2):143–147. doi: 10.17796/jcpd.27.2.858m05m461q2k613. [DOI] [PubMed] [Google Scholar]
- 25.Svenson B, Eriksson T, Kronström M, Palmqvist S. Image quality of intraoral radiographs used by general practitioners in prosthodontic treatment planning. Dentomaxillofac Radiol. 1994;23(1):46–48. doi: 10.1259/dmfr.23.1.8181659. [DOI] [PubMed] [Google Scholar]